Inpatient/Outpatient (IP/OP) Billing Manual
- General Billing Information
- General Prior Authorization Requirements
- Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
- Gender-Affirming Care Services
- Emergency Medicaid Services (EMS)
- Inpatient Hospital Transitions (IHT)
- Co-Pay
- Out-of-State Hospital Services
- Hospital Specialty Drug Policy
- Inpatient/Outpatient (IP/OP) Hospital Billing Information
- Inpatient Hospital Billing Information
- Date of Discharge
- Interim Payments for Diagnosis Related Group (DRG) Hospitals with Long-Term Inpatient Stays
- Billing for Services Rendered in a Distinct Part Unit
- Birthing Parent and Newborn Billing
- Special Instructions for Labor and Delivery Claims
- Newborn Hearing and Metabolic Screenings
- Billing for Immediate Post-Partum Long-Acting Reversible Contraceptives (IPP-LARCs)
- Billing for Take-Home Naloxone (Opioid Antagonist) for an Inpatient Stay
- Billing for Transplants
- Billing for Non-Covered Days
- Medicare Part B Only/Part A Exhaust Coverage
- Professional Fees
- Health First Colorado and Criminal Justice Involved Populations
- Billing for Combined Stays Under the 48-Hour Readmission Policy
- Late Charges
- Long-Term Acute Care (LTAC) and Rehabilitation Services
- Behavioral Health Services
- Hospital Service Payments - Inpatient Reimbursement
- Swing Bed Services
- Inpatient Subacute Care During the COVID-19 Public Health Emergency
- Outpatient and Community Clinic (CC)/Free Standing Emergency Departments (FSED)
- Outpatient Service Limitations
- Enhanced Ambulatory Patient Grouping System (EAPG)
- Bundling
- Recurring Visits and Emergency Department/Observation Billing for Outpatient Claims
- Enhanced Ambulatory Patient Grouping System (EAPG) Consolidation and Distinct Procedures
- Additional Medical Visits
- Bilateral Procedures
- 340B Drug Billing
- Discarded Portion of Drug Modifier
- Never Event Billing
- Terminated Procedure Reporting
- CPT/HCPCS Multiple Units
- Billing for Take-Home Naloxone (Opioid Antagonist) for an Outpatient Visit
- Outpatient Hospital Unbundled Durable Medical Equipment (DME) Billing
- Inpatient-Only Procedures
- Observation Billing for Outpatient Claims
- Billing for Services on Outpatient Claims with a Behavioral Health-Covered Primary Diagnosis Code
- Partial Hospitalizations
- Span Billing
- Split Bills
- Third-Party Payment Prorate
- Transportation
- Procedure/Healthcare Common Procedure Coding System (HCPCS) Codes Overview
- UB-04 Revenue Codes
- UB-04 Paper Claim Reference Table
- Timely Filing
- Sterilization, Hysterectomies and Abortions
- Institutional Provider Certification
- Inpatient Hospital Claim Example
- Inpatient for Combined Stay Under 48-Hour Readmission Policy Claim Example
- Outpatient Hospital Medicare Claim Example
- Outpatient Hospital Lab and X-Ray Claim Example
- Outpatient Hospital Crossover Claim Example
- Inpatient Hospital Medicare Part A Claim Example
- Outpatient Hospital with National Drug Code (NDC) Claim Example
- State Mental Hospital Claim Example
- Inpatient/Outpatient Revisions Log
Return to Billing Manuals Web Page
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page for general billing information.
General Prior Authorization Requirements
Prior Authorization Requests (PARs) must be submitted via the ColoradoPAR Program. Refer to the General Provider Information Manual on the Billing Manuals web page for information about prior authorization requirements. More information can be found on the Provider Contacts web page.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
Refer to 8.280.4.E Other EPSDT Benefits.
Gender-Affirming Care Services
Refer to the Gender-Affirming Care Billing Manual for gender-affirming care services.
Emergency Medicaid Services (EMS)
Refer to the Emergency Medicaid Services Billing Manual.
Inpatient Hospital Transitions (IHT)
Refer to the Inpatient Hospital Transitions (IHT) web page for information about this program.
Co-Pay
For cost sharing to be imposed on a member seeking Non-Emergency Services in a hospital emergency department, the hospital must first provide the appropriate medical screening examination as required by the Emergency Medical Treatment and Labor Act (EMTALA) and ancillary services such as laboratory and radiology, in accordance with 42 CFR 489.24 subpart G, to determine that the medical condition does not meet the Emergency Care Services definition found in 10 CCR 2505-10 8.300.1. The definition is as follows:
“Emergency Care Services, for the purposes of this rule, means services for a medical condition, including active labor and delivery, manifested by acute symptoms of sufficient severity, including severe pain, that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical attention to result in: (1) placing the member’s health in serious jeopardy, (2) serious impairment to bodily functions or (3) serious dysfunction of any bodily organ or part.”
If the provider determines that the condition does not meet the Emergency Care Services definition, the hospital staff is instructed to inform the member that the condition does not require emergency care services. The hospital staff is instructed to assist the member in finding an appropriate provider by using the following tools:
- Find a Doctor web page
- PEAK Health app
- Care Coordinator within the assigned Regional Accountable Entity (RAE)
Prior to imposing a Non-Emergency Services cost share, the provider must adhere to the following requirements of 42 CFR 447.54(d)(2):
- Inform the member of the cost sharing obligation amount for Non-Emergency Services provided in the emergency department.
- Provide the member with the name and location of an available and accessible alternative Non-Emergency Services provider.
- Determine that the alternative provider can provide services to the member in a timely manner with the imposition of a lesser cost sharing amount or no cost sharing if the individual is otherwise exempt from cost sharing.
- Provide a referral to coordinate scheduling for treatment by the alternative provider.
Members are responsible for an $8 cost share if choosing to receive Non-Emergency Services in the hospital emergency department after being informed of all options.
Hospitals may not assess the $8 cost share without following the above protocol before providing Non-Emergency Services for a member in the hospital emergency department.
Refer to the Co-Pay section in the General Provider Information Manual for more information.
Out-of-State Hospital Services
Out-of-state hospitals are classified as urban or rural. A base rate of 90% of the Colorado urban or rural base rate is used for the purpose of reimbursement calculation under the Health First Colorado (Colorado's Medicaid program) All-Patient Refined Diagnosis Related Group (APR-DRG) and Enhanced Ambulatory Patient Grouping (EAPG) payment methodologies.
Visit the Inpatient Hospital Payment web page for further inpatient base rate information.
Visit the Outpatient Hospital Payment web page for further outpatient base rate information.
Non-emergent out-of-state inpatient services must be prior authorized. Inpatient Prior Authorization Requests (PARs) must be submitted via the ColoradoPAR Program. Refer to the General Prior Authorization Requirements section above.
To qualify for a Single Case Agreement (SCA), the following requirements must be met:
- The services must be hospital services.
- The services must not be available in Colorado.
- The services must be prior authorized.
Requests for prior authorization solely to meet the criteria above are not granted. The service or stay must require prior authorization.
Hospital Specialty Drug Policy
Payments for certain Hospital Specialty Drugs are carved out of the Enhanced Ambulatory Patient Group (EAPG) methodology for Outpatient Hospital claims with the first date of service on or after August 11, 2018.
Effective January 1, 2024, certain Hospital Specialty Drugs may be administered in the Inpatient setting and be reimbursed outside of the All-Patient Refined Diagnosis Related Group (APR-DRG) methodology when billed on an Outpatient Hospital claim. Reimbursement is based on a percentage of acquisition cost.
Refer to Appendix Z located on the Billing Manuals web page under the Appendices drop-down for the codes for these drugs and the effective dates for their carveout.
An approved member specific prior authorization is required prior to administration of the Physician-Administered Drug (PAD).
The following processes must be completed prior to administration of the Hospital Specialty Drug:
- A member-specific prior authorization (PA) is required
- All Hospital Specialty Drugs requiring a PA are listed on Appendix Z
- Hospital Specialty Drug policy and procedures can be found on the Physician-Administered Drugs web page
- An approved PA must be on file prior to the administration of the Hospital Specialty Drug
- Retroactive authorization is not usually considered
- An approved PA on file does not guarantee payment
The following billing processes must be completed after administration:
- Outpatient Hospital Administration
- Outpatient claim is billed
- Amount billed
- Acquisition cost
- Cost per NDC unit multiplied by the number of NDC units administered to the member
- Claim will be denied if the amount billed does not equal the number of NDC units billed on the claim multiplied by the invoice dollar amount per NDC unit administered
- Acquisition cost
- NDC
- The NDC of the Hospital Specialty Drug administered to the member must be billed on the line
- Units billed
- The amount of drug administered to the member must be billed on the claim line in both HCPCS and NDC units
- Invoice attached
- Claim will be denied if no invoice is attached
All PAD, 340B and IP/OP policies apply
- Inpatient Hospital Administration
- Inpatient hospital claim is billed and paid
- The OP claim must be submitted after the affiliated IP claim is paid
- Outpatient hospital claim is billed
- All requirements from above apply
- Modifier “SE” must be billed on the claim line
- No additional revenue or procedure codes may be billed on the claim
- Outpatient claim date of service must be the date of administration and within the affiliated inpatient claim From Date of Service (FDOS) and To Date of Service (TDOS)
- Amount billed
- Acquisition cost
- Cost per NDC unit multiplied by the number of NDC units administered to the member
- Claim will be denied if amount billed does not equal the number of NDC units billed on the claim multiplied by the invoice dollar amount per NDC unit administered
- Acquisition cost
- NDC
- The NDC of the Hospital Specialty Drug administered to the member must be billed on the line
- Units billed
- The amount of drug administered to the member must be billed on the claim line in both HCPCS and NDC units
- Invoice attached
- Claim will be denied if no invoice is attached
- All PAD and IP/OP policies apply
- 340B exception
- 340B inventory cannot be used when a Hospital Specialty Drug is administered in an Inpatient setting and billed on an Outpatient claim.
- 340B exception
- All requirements from above apply
- Inpatient hospital claim is billed and paid
Refer to the Physician-Administered Drugs (PAD) web page for policy and procedures.
Inpatient/Outpatient (IP/OP) Hospital Billing Information
Both inpatient and outpatient hospital services are a benefit of Health First Colorado when medically necessary and supervised by a physician. Non-emergency outpatient services are subject to Primary Care Physician Program guidelines. The Department of Health Care Policy and Financing (the Department) periodically modifies billing information. Therefore, the information in this manual is subject to change, and the manual is updated as new billing information is implemented. Providers should refer to the Code of Colorado Regulations, Program Rules (10 C.C.R. 2505-10), for specific information when providing hospital care.
Ordering, Prescribing and Referring (OPR) Providers
42 CFR § 455.440 requires that claims certain types of services contain the National Provider Identifier (NPI) of the provider who ordered the service and that the NPI is actively enrolled with Health First Colorado.
Providers are required to enter the NPI of the ordering provider into the following locations for claim submission.
Institutional claims
- The Attending Provider field (#76) or the Other ID fields (#78 or #79) for both paper and electronic claims
- Providers should refer to their applicable UB-04 billing manuals for guidance on how each field is used.
Refer to the OPR Claim Identifier Project web page for further information on this project.
Inpatient Hospital Billing Information
Inpatient Hospital Services means services that are furnished by a Hospital for the care and treatment of an Inpatient and are provided in the Hospital by or under the direction of a physician.
Inpatient is a person who has been admitted to a Hospital for the purposes of receiving Inpatient Hospital Services.
Inpatient Hospital Services are reimbursed by Health First Colorado on a prospective basis using the All Patient Refined (APR) Diagnosis Related Group (DRG) method. Inpatient APR-DRG hospital claims utilize the last date of service to assign which inpatient hospital base rate and APR-DRG Weight Table will be used for payment. Please visit our Inpatient Hospital Payment web page for more information on APR-DRG Weight Tables and Inpatient Hospital Base Rates throughout the years.
Date of Discharge
The date of discharge or death is not counted as a covered day unless discharge or death occur on the day of admission. If admission and discharge or death occur on the same day, the day is considered a day of admission and counts as a full day unit. This includes if a patient is discharged or dies after admission but before assignment to a room. Charges for ancillary services on the day of discharge or death are covered.
Refer to the Bundling section of this manual.
Interim Payments for Diagnosis Related Group (DRG) Hospitals with Long-Term Inpatient Stays
The Health First Colorado All-Patient Refined Diagnosis Related Group (APR-DRG) payment system requires that claims for inpatient stays in DRG Hospitals be submitted after discharge. To accommodate the financial needs of DRG Hospitals when long-term stays create large account receivables, DRG Hospitals may bill interim claims using adjusted claims.
Criteria
The following criteria must be met in order to receive an interim payment:
- Health First Colorado must be the primary payer. Interim payment is not permitted when the member has other medical resources such as Medicare or commercial health insurance coverage.
- Patient status for interim claims must be "30: Still a patient." A final interim claim can only be filed after patient discharge.
After the first interim payment, additional requests should be submitted when Health First Colorado reimbursement reaches or exceeds an additional $100,000 from original interim claim.
Billing Process
Submit the first interim claim and submit adjustments to the first interim claim until discharge. All interim claims should be submitted directly to the Department's fiscal agent.
First interim claim (type of bill 112 - First Interim Claim) should be billed by the hospital for the services performed from the admission date through the billing date with patient status.
Additional interim adjustment claims (type of bill 117 - Hospital Inpatient [Including Medicare Part A]- Replacement of Prior Claim) should be billed by the hospital when the total Health First Colorado payment is at least $100,000 more than the previous interim payment. Interim adjustment claims must cover the entire stay from the first date of service through the billing date.
Final interim claim (type of bill 117 - Hospital Inpatient [Including Medicare Part A]- Replacement of Prior Claim) should be billed after the member has been discharged and should cover the entire stay from the first date of service through the discharge date.
If a hospital chooses to interim bill using type of bill 113-114, then the provider must void previous interim claims prior to submitting additional interim claims or the final interim claim.
Billing for Services Rendered in a Distinct Part Unit (DPU)
Health First Colorado does not currently recognize Distinct Part Units (DPUs) as separate from the General Hospital under which they are licensed and does not enroll DPUs separately. Admissions to DPUs are for psychiatric care or rehabilitation care in the General Hospital. The Medical Assistance Program payment to the General Hospital for these cases is designed to cover the cost of these services.
Since Health First Colorado does not recognize DPUs, hospitals may not submit two (2) claims for a member who is admitted to a General Hospital and then transferred to the hospital's DPU. A single claim should be submitted for this scenario covering the dates of service from the admission to the general acute facility through the discharge from the DPU. The DPU National Provider Identifier (NPI) should be represented as a service location on the claim.
Birthing Parent and Newborn Billing
For claims in which the birthing parent's discharge date occurs on or after July 1, 2020:
Services for the birthing parent and baby must be billed on separate claims under the identification number of each member per 10 CCR 2505-10 8.300.3.A.
- Baby requires its own Health First Colorado ID number.
- The Colorado interChange claims processing system cannot accept a baby's birth weight. The weight must be coded using an ICD-10 diagnosis code. Include newborn/live (Z38, Z38X OR Z38XX) as a primary diagnosis on the baby's claim.
- The admission date on the baby's hospital claim is the baby's date of birth.
- If the baby is transferred to a different hospital, Health First Colorado benefits are still applicable. The baby's charges (procedure and diagnosis codes) must be billed separately by the receiving hospital.
- If the birthing parent is not eligible for benefits and third-party insurance pays for any portion of the well-baby care, the payment must be included on the claim as a third-party payment. Health First Colorado is always the payer of last resort.
Visit the Hospital Stakeholder Engagement Meetings web page and the Inpatient Hospital Payment web page for information regarding the impact this billing process may have on payment.
Unless otherwise medically necessary, charges for a well newborn remaining in the hospital after the birthing parent’s discharge are not a Health First Colorado benefit (e.g., placement).
For claims in which the birthing parent's discharge date occurs prior to July 1, 2020:
The birthing parent's and baby's charges (procedure and diagnosis codes) are billed on one (1) claim as one (1) stay while the birthing parent is in the hospital. The Colorado interChange claims processing system cannot accept a baby's birth weight; the weight must be coded using an ICD-10 diagnosis code.
Do not show nursery days in form locator 6. Nursery days are entered as units on a detail line but are not covered days that represent additional payment. There is no additional inpatient benefit for routine newborn hospitalization. Charges for a well newborn remaining in the hospital after the birthing parent's discharge are not a benefit (e.g., placement).
When the birthing parent is not eligible for benefits, the baby's well-baby care charges may be billed under the following conditions:
- The baby is eligible for benefits.
- The baby has its own Health First Colorado ID number.
- If the birthing parent's insurance pays for any portion of the well-baby care, the payment must be included on the claim as a third-party payment. Health First Colorado is always the payer of last resort.
Services may be billed on the birthing parent's claim until the time the birthing parent is discharged. Baby's charges, procedure and diagnosis codes related to the baby's extended stay, beginning with the birthing parent's date of discharge through the baby's discharge, are billed separately from the birthing parent's charges.
The baby requires its own Health First Colorado ID number. The admission date on the baby's hospital claim is the date of birthing parent's discharge. Including a newborn/live (Z38, Z38X OR Z38XX) as a primary diagnosis on the baby's independent claim may cause the claim to be ungroupable and result in an appropriate denial. The primary diagnosis should reflect the reasons why the child remains in the hospital after the birthing parent leaves.
If the baby is transferred to a different hospital, the Health First Colorado benefits are still applicable. The baby's charges (procedure and diagnosis codes) must be billed separately by the receiving hospital.
Special Instructions for Labor and Delivery Claims
Delivery is a benefit for recipients of Emergency Medicaid Services (EMS).
Refer to the Emergency Medicaid Services Billing Manual for more information.
Newborn Hearing and Metabolic Screenings
Costs associated with the Newborn Hearing Screening and the initial Newborn Metabolic Screening are included in the delivery Diagnosis Related Group (DRG) calculation or the birthing center facility payment. They may not be billed separately. Current Procedural Terminology (CPT)/ Healthcare Common Procedure Coding System (HCPCS) codes for the Newborn Hearing Screening cannot be billed for dates on or during the date span of the delivery stay. Refer to the Audiology Benefit Billing and Policy Manual and the Laboratory Services Billing Manual for more information.
Billing for Immediate Post-Partum Long-Acting Reversible Contraceptives (IPP-LARCs)
Effective January 1, 2020, Immediate Post-Partum-Long-Acting Reversible Contraceptive (IPP-LARC) devices inserted in a Diagnosis Related Group (DRG) Hospital may be reimbursed at the fee schedule rate or the amount billed, whichever is less. Delivery DRG weights (540, 542 and 560) were reduced by .004 to allow for this separate payment.
Prior to January 1, 2020, the cost of the IPP-LARC device was included in the All Patient Refined-Diagnosis Related Group (APR-DRG) calculation for the delivery claim.
Reimbursement for IPP-LARCs requires submission of both:
- An Inpatient claim - for the DRG payment
- An Outpatient claim - for the IPP-LARC fee schedule payment
The Inpatient Hospital Claim must group to APR-DRG 540, 542 or 560, and include:
- ICD-10 Diagnosis Code for LARC insertion: Z30.430 or Z30.018
- ICD-10 Surgical Procedure Code for either:
- An IUD insertion: 0UH90HZ, 0UH97HZ or 0UH98HZ
- A Contraceptive Implant insertion: 0JHD0HZ, 0JHD3HZ, 0JHF0HZ or 0JHF3HZ
The Outpatient Hospital Claim:
- Must include:
- The HCPCS for the LARC device: J7296, J7297, J7298, J7300, J7301 or J7307
- The LARC device's affiliated NDC
- Both the FP and SE modifiers
- No additional revenue or procedure codes can be present on the claim.
- Outpatient claim must be submitted after the affiliated inpatient claim is paid.
- Outpatient claim's date of service must be the date of insertion and within the affiliated inpatient claim's From Date of Service (FDOS) and To Date of Service (TDOS).
Billing for Take-Home Naloxone (Opioid Antagonist) for an Inpatient Stay
Prior to January 1, 2023, the cost of take-home Naloxone was included in the All Patient Refined-Diagnosis Related Group (APR-DRG) calculation for the inpatient claim.
Effective January 1, 2023, payment for take-home Naloxone (opioid antagonist) dispensed by a hospital upon discharge to members deemed at risk of opioid-related overdoses are excluded from the DRG relative weight calculation and will be paid according to the physician administered drugs payment methodology.
Reimbursement for take-home Naloxone requires submission of both:
- An Inpatient claim - for the DRG payment
- An Outpatient claim - for the take-home Naloxone fee schedule payment
The Outpatient Hospital Claim must include:
- One of the HCPCS for take-home Naloxone: G2215 and G1028
- The NDC of the medication dispensed
- Modifier SE
- The attached invoice if G2215 is billed on the claim
- No additional revenue or procedure codes can be present on the claim
Additional information:
- Outpatient claim must be submitted after the affiliated Inpatient claim is paid, and
- Outpatient claim's date of service must be the dispense date affiliated with the Inpatient claim's FDOS-TDOS.
Billing for Transplants
Donor acquisition costs are included in both the All-Patient Refined Diagnosis Related Group (APR-DRG) and Enhanced Ambulatory Patient Group (EAPG) payment methodologies for transplants.
Transplants and related services are not a covered benefit for Emergency Medicaid Services (EMS) members.
Refer to the Medical-Surgical Billing Manual for the professional component of these Medical-Surgical Services.
Billing for Non-Covered Days
Total days are the total number of days billed on the claim. These days are calculated as the days between admission and To Date of Service (TDOS). A day on which a patient begins a leave of absence is not counted as a covered day.
Value codes 80 and 81 should be used to indicate the quantity of covered and non-covered days during an inpatient stay. The sum of these days should equal the total days on the claim, less the day of discharge.
Occurrence Span Code 74 should be used to report the from and through dates at a non-covered level of care or leave of absence during an otherwise covered stay.
Medicare Part B Only/Part A Exhaust Coverage
Providers should submit a claim to Medicare for any services covered by Medicare.
Health First Colorado pays the Health First Colorado inpatient allowable amount less the Medicare Part B payment, any commercial insurance payment (if applicable) and any Health First Colorado co-payment.
Billing Instructions
The crossover claim Type of Bill (TOB) 12X will be automatically denied and post Explanation of Benefit (EOB) 1290 (“Invalid Type of Bill for the Claim Type”).
For the inpatient crossover claim TOB 11X, providers must manually enter the Medicare Part B Only and Medicare Part A Exhaust payments. Final claim payment should equal the Health First Colorado inpatient allowable amount less the Medicare payment, commercial insurance payment (if applicable) and any co-payment.
The Provider Web Portal allows providers to use a Part B only/Part A checkbox when billing inpatient crossover claims for members that have Title XIX (19) benefits and Medicare Part A benefits are exhausted prior to or during the stay.
Claims can be submitted via paper, interactively via the Provider Web Portal or by batch via Electronic Data Interchange (EDI). Refer to the instructions below for each submission type:
- Paper: In the Payer Name field (form locator 50), enter the payment source code H - Medicare Part B/A Exhaust, followed by name of each payer organization from which the provider might expect payment. At least one (1) line must indicate Health First Colorado. Electronic claims format shall be required unless hard copy claims submittals are specifically approved by the Department. Refer to the General Provider Information Manual located on the Billing Manuals web page for further details.
- Provider Web Portal: Refer to the Entering Other Insurance or Medicare Crossover Information Quick Guider located on the Quick Guides web page.
- EDI: Refer to the Companion Guides located on the EDI Support web page.
Professional Fees
Costs associated with professional services by salaried physicians are included in the hospital's rate structure and cannot be billed separately to Health First Colorado. Do not bill professional fees (Revenue Codes 0960-0989) for emergency and outpatient services on an institutional claim (UB-04).
Professional fees for services provided in the emergency room by contract physicians must be billed by the physician as a professional claim (CMS 1500) using the appropriate Healthcare Common Procedure Coding System (HCPCS) codes. The Health First Colorado payment is made to the physician or physician clinic.
Health First Colorado and Criminal Justice Involved Populations
For criminal justice involved populations, Health First Colorado will only cover medically necessary inpatient services rendered in a hospital setting. This policy is based on federal regulation in section 1905(a) of the Social Security Act which excludes Federal Financial Participation (FFP) for medical services for inmates with exception to inpatient care.
Inpatient services for incarcerated individuals are covered when they meet all of the following conditions:
- Occur in an inpatient hospital outside of the correctional facility
- Require inpatient hospitalization for at least 24 hours
- Are provided between the time of inpatient admission and time of inpatient discharge
Health First Colorado cannot cover services for incarcerated individuals that are provided:
- In an outpatient setting
- In an inpatient setting for a stay that lasts less than 24 hours
- On the premises of the prison, jail or detention center
The From Date of Service (FDOS) must match the Admission Date and be reflected in Colorado interChange, the claims processing system, to ensure that only the services provided during the covered inpatient stay are included in the claim.
Example 1:
A member is admitted to inpatient care on October 2, 2021, and discharged on October 5, 2021.
- The claim can be submitted to Health First Colorado.
Example 2:
A member is admitted to inpatient care on October 2, 2021, at 6:00 p.m. and discharged on October 3, 2021, at 8:00 a.m.
- The stay is under 24 hours and is therefore not eligible to be submitted to Health First Colorado.
Example 3:
A member is taken to the emergency room on October 2, 2021, but then is admitted as an inpatient on October 3, 2021, and discharged on October 5, 2021.
- The hospital can only submit a claim to Health First Colorado for the inpatient days.
- On the claim, the From Date of Service (FDOS) and Admit Date will both be October 3, 2021.
Visit the Health First Colorado and Criminal Justice Involved Populations web page for further information on eligibility and billing for criminal justice involved populations.
Billing for Combined Stays Under the 48-Hour Readmission Policy
Effective for dates of service on or after July 1, 2011, a hospital must bill admissions as a single hospital stay if a member is discharged and then readmitted to the same hospital within 48 hours for symptoms related to, or for evaluation and management of, the prior stay's medical condition. The hospital will receive only one (1) payment for what is considered one (1) episode of care.
All claims for hospital readmissions in which a member is readmitted to the same hospital within 48 hours of discharge will be denied unless the readmission is completely unrelated to the first admission. The 48 hours is calculated from Discharge Hour (form locator 16 on the first claim) to Admission Hour (form locator 13 on the second claim). This will apply to all claims for second admissions dated July 1, 2011, or later.
Example 1:
A member is admitted January 19, 2012, and is discharged January 23, 2012, at 2:00 a.m. The member is readmitted with related symptoms on January 25, 2012, at 1:00 a.m. and is discharged January 28, 2012.
- The hospital bills one (1) claim from Date of Service (DOS) January 19, 2012, through DOS January 28, 2012. The number of covered days is seven (7). The number of non-covered days is two (2).
- Covered days must be reported using Value Code 80.
- Non-covered days must be reported using Value Code 81.
- Claim details need to include leave of absence Revenue Code 0180. The units should equal the non-covered days and charges equal to a non-zero (0) amount.
Example 2:
A member is admitted January 19, 2012, and is discharged January 23, 2012, at 2:00 a.m. The member is readmitted for an unrelated reason on January 25, 2012, at 1:00 a.m. and is discharged on January 28, 2012.
- The hospital bills two (2) separate claims for each stay because they are unrelated. The first stay is from DOS January 19, 2012, through DOS January 23, 2012. The second stay is from DOS January 25, 2012, through DOS January 28, 2012.
- The second claim must include condition code B4.
Example 3:
A member is admitted January 19, 2012, and is discharged January 23, 2012, at 2:00 a.m. The member is readmitted with related symptoms on January 25, 2012, at 4:00 a.m. and is discharged January 28, 2012.
- The hospital bills two (2) separate claims for each stay because the time between first discharge and second admission is greater than 48 hours. The first stay is from DOS January 19, 2012, through DOS January 23, 2012. The second stay is from DOS January 25, 2012, through DOS January 28, 2012.
The Colorado interChange claims processing system will automatically deny subsequent claims for readmission to the same hospital within 48 hours. Providers will have to submit an adjustment claim to correctly reflect the dates of service for the full episode of care. A claim may be coded with condition code B4 to indicate that a readmission is completely unrelated to the first admission and allow the separate episode of care.
The Department's audit team will continue to retrospectively review all readmissions within 48 hours which are paid with use of condition code B4. The Department will recoup payment if it is determined that the readmission is related to the first admission.
Health First Colorado does not currently recognize Distinct Part Units (DPUs) or any other units of a hospital as separate from the General Acute Care Hospital under which they are licensed. General Acute Care Hospitals may not submit two (2) claims for a member who is transferred between units of a hospital. A single claim should be submitted covering the dates of service from the admission to the General Acute Care Hospital through the discharge from the DPU. When the Department's audit team identifies claims for such transfers, the second admission will be denied.
Stays at Transitional Care Units or any other location that is not part of the General Acute Care Hospital are not billable under the hospital's Health First Colorado provider number and will be denied if billed as such.
Late Charges
Late charges for claims may be submitted as an adjustment to the Department’s fiscal agent at any time during the initial timely filing period.
When claims are adjusted, for any reason, outside of the timely filing period, the claim will deny for being outside of timely filing, and the entire original payment for the claim will be recouped.
Adjustments for Overpayments
Under Section 1128J(d) of the Social Security Act, any provider who receives an overpayment needs to report and return the overpayment to the Department within 60 days of identification. There are two (2) different ways this can be completed, including through the Provider Web Portal or by making a self-disclosure.
The provider can adjust the claim through the Provider Web Portal. A new Internal Control Number (ICN) is generated and will be processed against the edits in the claims processing system. One (1) of these edits is the timely filing edit, which will deny any claim where timely filing has not been preserved. If the adjustment occurs outside of the timely filing, the claim will deny, and the amount paid on the original claim will be recouped. The Department does not issue waivers of timely filing in order to reverse these recoupments.
The correct way to address an overpayment outside of timely filing is to submit a self-disclosure. The self-disclosure process requires the provider to identify the claims at issue and the reason for the overpayment. In order to return money to the Department, the provider may either direct the Department to set up an accounts receivable in the Colorado interChange claims processing system so that the amount can be deducted from future payments or submit a check to:
Department of Health Care Policy & Financing
ATTN: Audits and Compliance Division
303 E. 17th Avenue, Suite 1100
Denver, CO 80203
Visit the Provider Self-Disclosure Information web page for more information on the self-disclosure process.
Long-Term Acute Care (LTAC) and Rehabilitation Services
As of July 1, 2019, all Long-Term Acute Care (LTAC) Hospitals, Rehabilitation Hospitals and Spine/Brain Injury Treatment Specialty Hospitals as defined in Hospital Services Rule 8.300.1 will be reimbursed under a per diem.
Refer to the Billing for Services Rendered in a Distinct Part Unit section in this manual for Distinct Part Unit (DPU) information.
Long-Term Acute Care (LTAC) Hospitals
Inpatient services provided to Health First Colorado members in Long-Term Acute Care (LTACs) Hospitals are reimbursed on a per diem basis. The per diem rates follow a step-down methodology based on length of stay.
Tier 1: day 1 through day 21
Tier 2: day 22 through day 35
Tier 3: day 36 through day 56
Tier 4: day 57 through remainder of care
Rehabilitation Hospitals
Inpatient services provided to Health First Colorado members in Rehabilitation Hospitals are reimbursed on a per diem basis. The per diem rates follow a step-down methodology based on length of stay.
Tier1: day 1 through day 6
Tier 2: day 7 through day 10
Tier 3: day 11 through day 14
Tier 4: day 15 through remainder of care
Spine/Brain Injury Treatment Specialty Hospital
Inpatient services provided to Health First Colorado members in Spine/Brain Injury Treatment Specialty Hospitals are reimbursed on a per diem basis. The per diem rates follow a step-down methodology based on length of stay.
Tier 1: day 1 through day 28
Tier 2: day 29 through day 49
Tier 3: day 50 through day 77
Tier 4: day 78 through remainder of care
Billing for Dates of Service that Span the Fiscal Year for LTAC Hospitals, Rehabilitation Hospitals and Spine/Brain Injury Treatment Specialty Hospital
This billing is only allowed for claims that span the Per Diem Implementation Date of July 1, 2019.
To accommodate the change in Inpatient Reimbursement Methodology, the following criteria must be met in order to bill for dates of service that span the fiscal year.
- From Date of Service (FDOS) must be on June 30, 2019, or prior.
- To Date of Service (TDOS) must be on July 1, 2019, or later.
- Must be a Long-Term Acute Care (LTAC) Hospital, Rehabilitation Hospital (Rehab) or Spine/Brain Injury Treatment Specialty Hospital. Distinct Part Units (DPUs) are not included.
Billing Process
- Void claim if it meets criteria outlined above.
- Bill claims with FDOS prior to or on June 30, 2019, with Type of Bill (TOB) 112. Utilize discharge code 30: still a patient.
- Bill claims with TDOS July 1, 2019, or later with TOB 111 and appropriate discharge code.
Behavioral Health Services
Non-Psychiatric Hospitals
Outpatient Psychiatric Services:
Psychiatric services, including prevention, diagnosis and treatment of emotional or mental disorders, are Health First Colorado benefits at Non-Psychiatric Hospitals as noted in the Hospital Services Rule at 8.300.3.B.2.
Psychiatric Hospitals
Inpatient Psychiatric Hospital Services:
Inpatient Hospital Psychiatric Services are a Health First Colorado benefit for individuals aged 20 and under when provided as a service of an In-State Hospital as noted in the Hospital Services Rule at 8.300.3.A.5.
Inpatient Psychiatric Hospital Services are a benefit only when:
- Services involve active treatment which a team has determined is necessary on an inpatient basis, and services can reasonably be expected to improve the condition or prevent further regression so that the services shall no longer be needed. The team must consist of physicians and other personnel qualified to make determinations with respect to mental health conditions and the treatment thereof.
- Services are provided prior to the date the individual attains age 21 or, in the case of an individual who was receiving such services in the period immediately preceding this date, the date such individual no longer requires services or, if earlier, the date such individual attains age 22.
Outpatient Psychiatric Hospital Services:
Outpatient services are not a Health First Colorado benefit in Psychiatric Hospitals.
Billing for Inpatient Psychiatric Hospital Services - Non-Substance Use Disorder
Inpatient services provided to Health First Colorado members in Psychiatric Hospitals are reimbursed on a per diem basis. The per diem rates follow a step-down methodology based on revenue codes. Refer to Appendix Q located on the Billing Manuals web page under the Appendices drop-down for the revenue codes.
Step 1 (Revenue Code 114): day 1 through day 7
Step 2 (Revenue Codes 124 and 134): day 8 through remainder of care at acute level
Interim Billing Instructions for Inpatient Psychiatric Hospital Services
Psychiatric Hospitals may bill on an interim basis for services.
A new claim should be submitted for each span of time billed with the Admit date representing the original date of admission, From Date of Service (FDOS) representing the first date of service on the claim being submitted and the To Date of Service (TDOS) representing the last date of service on the claim.
Example:
If a provider bills on a monthly basis and the member's admission was on February 1, 2019, the first claim should have the following:
Admit date: February 1, 2019
FDOS: February 1, 2019
TDOS: February 28, 2019
Revenue code 114 should be used for days 1-7
Revenue code 124/134 should be used for days 8-28
The second claim submission for the following month should have the following:
Admit date: February 1, 2019
FDOS: March 1, 2019
TDOS: March 31, 2019
Revenue code 124/134 should be used for all days on this claim.
Obtaining Authorization for Behavioral Health Services
All Health First Colorado members are assigned to a Regional Accountable Entity (RAE) which is responsible for approval and reimbursement of behavioral health services. Services rendered prior to a member's assignment to a RAE should be billed Fee-for-Service (FFS) to the Department’s fiscal agent and are subject to Fee-for Service policies. A RAE may refer a member to a hospital for either inpatient or outpatient services. At the time of referral, the RAE will provide the hospital prior authorization and personal health information for the member as necessary.
If a member is referred to a hospital by a RAE, all information necessary for billing will be provided. The hospital will need to submit an eligibility inquiry to verify the member's RAE if a member presents at a hospital requesting services. The hospital will then contact the RAE in order to obtain prior authorization for treatment.
When a member presents at a hospital requesting emergency behavioral health services, the hospital provider will be reimbursed by the RAE for medical stabilization of the member but must contact the RAE to coordinate any further services.
Refer to the Health First Colorado UB-04 Revenue Code Table (Appendix Q) for a complete listing of services and the corresponding valid revenue codes.
Refer to Appendix Q located on the Billing Manuals web page under the Appendices drop-down.
Providers may appeal the decision if the claim has been denied by the RAE for non-included services. Appeal information is listed on the denial letter from the RAE.
Billing for Substance Use Disorder (SUD) Services
For claims in which the discharge date is prior to January 1, 2021: Inpatient Substance Use Disorder (SUD) services are not a Health First Colorado covered benefit.
Individuals aged 20 and under may access these services through Early and Periodic Screening, Diagnostic and Treatment (EPSDT). Services must be provided by facilities that attest to having in place rehabilitation components required by the Department. These facilities must be approved by the Department to receive reimbursement. The Department will review the claims submitted under All-Patient Refined Diagnosis Related Group (APR-DRG) 772 regularly to ensure only providers that have an attestation with the Department are being reimbursed for these services.
For claims in which the discharge date occurs on or after January 1, 2021:
Inpatient SUD services are a Health First Colorado covered benefit for members with a primary SUD diagnosis when medically necessary as determined by the American Society for Addiction Medicine (ASAM) Criteria. Inpatient SUD services are billed using the following accommodation revenue codes:
Revenue code 1000 - ASAM Level 3.7: Medically Monitored Intensive Inpatient Treatment
Revenue code 1002 - ASAM Level 3.7WM: Medically Monitored Inpatient Withdrawal Management
Reimbursement for Inpatient SUD services include behavioral health treatment, medical treatment and room and board. Refer to the Provider Manual for Resident and Inpatient Substance Use Disorder (SUD) Services located on the Ensuring Full Continuum SUD Benefits - Providers web page under the Provider Resources section for coding pages and information about residential and inpatient SUD services.
Hospitals must maintain an accurate count of all beds in their facility in the Colorado interChange claims processing system. Bed counts should include all beds in a facility regardless of whether they are utilized for psychiatric or SUD stays.
Non-Psychiatric Hospitals
Substance Use Disorder (SUD) services are covered in non-psychiatric hospitals for members of all ages.
Inpatient SUD services provided to Health First Colorado members in non-psychiatric hospitals are reimbursed using the methodology assigned to them (APR-DRG, Per Diem, etc.). The following accommodation revenue codes should be used for claims in which the member's primary diagnosis is a SUD. Using these accommodation codes allows for the services to be identified as SUD services.
Revenue code 1000 - ASAM Level 3.7: Medically Monitored Intensive Inpatient Treatment
Revenue code 1002 - ASAM Level 3.7WM: Medically Monitored Inpatient Withdrawal Management
Psychiatric Hospitals
SUD services are covered in Psychiatric Hospitals for members aged 21-64.
Inpatient SUD services provided to Health First Colorado members in Psychiatric Hospitals are reimbursed on a per diem basis. The per diem rates are identified based on revenue code. Refer to Appendix Q located on the Billing Manuals web page under the Appendices drop-down for the revenue codes.
Revenue code 1000 - ASAM Level 3.7: Medically Monitored Intensive Inpatient Treatment
Revenue code 1002 - ASAM Level 3.7WM: Medically Monitored Inpatient Withdrawal Management
Individuals aged 20 and under may access these services through Early and Periodic Screening, Diagnostic and Treatment (EPSDT). Services must be provided by facilities which attest to having in place rehabilitation components required by the Department. These facilities must be approved by the Department to receive reimbursement. The Department will review the claims submitted under All-Patient Refined Diagnosis Related Group (APR-DRG) 772 regularly to ensure only providers that have an attestation with the Department are being reimbursed for these services.
Hospital Service Payments - Inpatient Reimbursement
Hospitals designated as Prospective Payment System (PPS) Hospitals and Pediatric Specialty Hospitals are paid using the Diagnosis Related Group (DRG) methodology. Each hospital is assigned a base reimbursement rate which is calculated to represent the average cost per discharge for Health First Colorado members. New hospitals, critical access hospitals or low-discharge hospitals are assigned the peer group average base rate according to their in-state/out-of-state and urban/rural designations. Each DRG is assigned a relative weight.
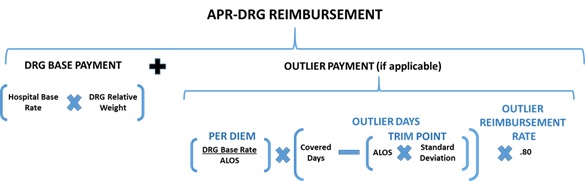
DRG Base payment is calculated as the hospital base rate multiplied by the DRG relative weight.
Outlier payments: If a hospital stay exceeds the DRG trim point, outlier days are calculated for additional payment at 80% of the established DRG per diem.
Outlier Payment Logic:
- Outlier Days = Covered Days beyond DRG Trim Point
- Outlier Payment = Outlier Days * Per Diem * 80%
Transfers: If the member is transferred from one (1) hospital to another, both facilities are paid a DRG per diem rate up to the maximum reimbursement under the appropriate DRG, based on the length of stay. Both hospitals receive outlier day payments, if applicable. See more specific information below for coding used to identify transfers and calculations for payment.
Cutback Payment for Uncovered Days During Stay: If there are days during the inpatient stay where the member does not have coverage under Health First Colorado, the hospital will be paid a DRG per diem rate up to the maximum reimbursement under the appropriate DRG, based on the length of stay. The hospital will also receive outlier day payments, if applicable.
Cutback Payment Logic:
- IF Covered Days < DRG Average Length of Stay, THEN pay Per Diem * Covered Days
- IF Covered Days > or = DRG Average Length of Stay, THEN pay DRG Base Payment
Psychiatric Hospitals: Hospitals designated as Non-Prospective Payment System (NPPS) Hospitals are reimbursed at an established per diem rate.
Out of State Hospitals: Urban or Rural Out-of-State Hospitals are paid using the DRG methodology. Reimbursement is made using a base rate of 90% of the average Colorado urban or rural base rate.
Medicare Crossover Claims: Medicare crossover claims are reimbursed by Health First Colorado based on whichever of the following two (2) formulas results in a lesser amount:
- The sum of the reported Medicare coinsurance and deductible
- The Health First Colorado-allowed amount minus the Medicare payment
Transfer Payment Logic
In situations where an inpatient member is transferred to or from a General Hospital (patient discharge status codes 02, 05, 62, 63, 66, 69, 82, 85, 90, 91, or 94 OR admit source 4), the General Hospital will be reimbursed on a per diem basis if the member's covered days are less than the DRG Average Length of Stay (ALOS). The General Hospital is also eligible to receive outlier payments if the member's covered days exceeds the DRG Trim Point. Refer to the outlier calculation above. Otherwise, the DRG Base payment is paid for covered days equal to or greater than the ALOS and less than or equal to the DRG Trim Point.
Per Diem Calculation:
- Per Diem = DRG Base Payment √ DRG Average Length of Stay
Transfer Payment Logic:
- IF Covered Days < DRG Average Length of Stay, THEN pay Per Diem * Covered Days
- IF Covered Days > or = DRG Average Length of Stay, THEN pay DRG Base Payment
When transfer services are billed, complete the following form locators for correct reimbursement calculation:
Form Locator 15, Source of Admission (04)
Form Locator 17, Patient Status (02, 05, 62, 63, 66, 69, 82, 85, 90, 91, or 94)
Refer to the instructions for each form locator in this provider manual.
"Lower of" Pricing
The Department has the obligation to pay "lower of" pricing based on providers' customary charges, also known as the providers' submitted charges, on the claim. Federal regulations require that payment for Inpatient Hospital Services not exceed providers' customary charges. Refer to 42 CFR § 447.271. Likewise, Colorado's State Plan includes an attestation that the Department "meets the requirements of 42 CFR Part 447, Subpart C, and sections 1902(a)(13) and 1923 of the [Social Security] Act with respect to payment for Inpatient Hospital Services." Refer to § 4.19(a) Payment for Services.
"Present on Admission" Indicator on Hospital Claims
Inclusion of "Present on Admission" (POA) indicator responses are required for inpatient hospital claims submitted through the Provider Web Portal. The Department's policy follows that of the Medicare program for hospitals paid through prospective payment.
The POA response is required for Principal Diagnosis and all Other Diagnoses. It is not required for the Admitting Diagnosis. The POA response is to be documented in the gray area to the right of Form Locator 67 (Principal Diagnosis) and 67A -67Q (Other Diagnoses). Allowed responses are limited to:
✓ Y = Yes - Present at the time of inpatient admission
✓ N = No - Not present at the time of inpatient admission
✓ U = Unknown - The documentation is insufficient to determine if the condition was present at the time of inpatient admission
✓ W = Clinically Undetermined - The provider is unable to clinically determine if the condition was present at the time of inpatient admission
✓ "Blank" or "1" = Diagnosis is exempt for POA reporting or is not submitted ("Blank" to be used on electronics submissions, "1" for paper submissions)
The POA indicator is used to identify claims with Health Care Acquired Conditions (HCAC) and Other Provider Preventable Conditions (OPPC). Specific codes associated with HCAC and OPPC are provided below. These are events which, if occurred while in the hospital (POA = N or U), can complicate care and member outcomes. Because these events can be deemed preventable, the Centers for Medicare & Medicaid Services (CMS) does not allow the Department to pay additional costs of a higher All-Patient Refined Diagnosis Related Group (APR-DRG) assignment arising from HCACs or must deny payment altogether for OPPCs.
Hospital-Acquired Conditions (HAC)/Healthcare-Acquired Conditions (HCAC)
Refer to the latest CMS Medicare Hospital Acquired Conditions List for the latest ICD-10-CM Diagnosis Codes.
Other Provider Preventable Conditions (OPPC)
Other Provider Preventable Conditions (OPPC) include:
- Surgery performed on the wrong body part
- Surgery performed on the wrong member
- Wrong surgical procedure performed on the member
Hospitals are required to submit claims when any of these HCAC or OPPC events occur in an inpatient hospital setting and when an OPPC event occurs in an outpatient healthcare setting. Members may not be billed or balance-billed for services related to these HCACs or OPPCs. The Department will collaborate with hospitals to assure appropriate reimbursement for cases in which a member receives subsequent care for an HCAC or OPPC in a hospital other than the original site in which the event occurred.
Swing Bed Services
Hospitals certified to provide Skilled Nursing Facility (SNF) services and/or Intermediate Care Facility (ICF) services to members in swing beds must furnish the services, supplies and equipment required for SNFs and ICFs within the approved per diem rate. Services must be certified as medically necessary.
Swing Bed services should be billed using a Swing Bed enrollment (Provider Type 20 Specialty Code 396). Refer to the Nursing Facility Billing Manual located on the Billing Manuals web page for details on billing and reimbursement for these services.
Inpatient Subacute Care During the COVID-19 Public Health Emergency
Inpatient Subacute Care - Hospital
The Department passed an emergency rule on April 23, 2020, to allow hospitals enrolled as General Hospitals (Provider Type 01) to provide Inpatient Subacute Care, and Colorado Department of Public Health and Environment (CDPHE)-approved alternate care sites during the COVID-19 Public Health Emergency (PHE). On May 20, 2020, the Department received approval from the Centers for Medicare & Medicaid Services (CMS) for a corresponding State Plan Amendment (SPA) #20-0012 allowing Inpatient Subacute Care.
What is Inpatient Subacute Care?
Inpatient Subacute Care is equivalent to the medically necessary level of care administered by a Skilled Nursing Facility (SNF) for skilled nursing and intermediate care services as defined in 10 CCR 2505-10, Sections 8.406 and 8.409.
When can a hospital provide Inpatient Subacute Care?
- If the member requires the level of care that would normally be provided by an SNF, but they cannot or should not be transferred to an SNF
- The hospital may provide Inpatient Subacute Care
- If the member requires the level of care that would normally be provided by an SNF, but they cannot or should not be transferred to an SNF and the hospital does not have capacity, the member may be transferred to a
- CDPHE approved alternate care site, or,
- Another hospital that can provide Inpatient Subacute Care.
- Members may be admitted to Inpatient Subacute Care,
- After an inpatient admission,
- From an emergency department,
- From observation status, or,
- By primary care referral to the administering hospital.
When can't a hospital provide Inpatient Subacute Care?
- If the member's principal diagnosis is a RAE-covered mental health diagnosis
- If the hospital is a Psychiatric Hospital (Provider Type 02)
- If the PHE has ended
Where can Inpatient Subacute Care be provided?
Inpatient Subacute Care can be provided in the following locations:
- A hospital
- A hospital's CDPHE approved Alternate Care Sites (ACS)
What payment methodology is used for Inpatient Subacute Care?
Inpatient Subacute Care is paid at a per diem rate of $235.
If a hospital has designated swing beds, the hospital should continue to provide services as swing beds and will be paid under their existing per diem rate.
How does a hospital bill for Inpatient Subacute Care?
Claims for Inpatient Subacute Care with dates of service on or after April 24, 2020, through the end of the federal Public Health Emergency, may be submitted to the Department for reimbursement.
Hospitals must submit a separate inpatient or inpatient crossover claim for covered Inpatient Subacute Care days using Revenue Code 190 (Subacute Care). No other revenue codes should be present on the claim. If the member was moved from an inpatient hospital stay to Inpatient Subacute Care, then Patient Status 70 (discharged/transferred to another type of health care institution not defined elsewhere in this code list) should be used as the patient status on the claim for the inpatient hospital stay. The claim for the inpatient hospital stay will be paid using the hospital's current inpatient payment methodology. If a different patient status code is used, transfer pricing may apply.
If the patient receives services at a CDPHE approved alternate care site, then the location of the ACS should be submitted as the service facility provider on the claim. If the ACS is not an enrolled Health First Colorado provider, the claims will need to be submitted through batch as an 837I standard x12 HIPAA transaction.
Inpatient Subacute Care services billed with any revenue code other than 190 or a RAE-covered mental health principal diagnosis will be denied for Explanation of Benefits (EOB) 3255 (“Inpatient lower level of care service billed with conflicting services”).
Outpatient and Community Clinics (CC)/Free-Standing Emergency Departments (FSED)
Outpatient Hospital Services means services that are furnished to Outpatients and are furnished by or under the direction of a physician or dentist.
Outpatient means a person who is receiving professional services at a Hospital or an off-campus location of a Hospital but is not admitted as an Inpatient.
Outpatient Service Limitations
Visit the Colorado Medicaid State Plan web page for more information.
Routine and annual physical examinations are not provided unless determined to be medically necessary based upon a medical diagnosis, complaint or symptom.
Enhanced Ambulatory Patient Grouping (EAPG) System
The Department reimburses hospitals for institutional outpatient claims with all service dates on or after October 31, 2016, using the Enhanced Ambulatory Patient Grouping (EAPG) methodology. As such, periodic updates to cost-to-charge ratios are no longer required. Payment calculation is performed on the claim detail as the lower of redistributed charges or hospital-specific base rate multiplied by the detail's assigned EAPG's Adjusted Relative Weight.
The Colorado interChange claims processing system relies on the 3M EAPG Grouper module to price outpatient hospital claims. In its pricing calculations, billed amounts are determined as reimbursable or non-reimbursable based on whether the revenue code is covered. Refer to Appendix Q located on the Billing Manuals web page under the Appendices drop-down. Reimbursable billed amounts are aggregated by visit and then distributed to each line based on the proportion of that line's EAPG Adjusted Relative Weight to the sum of that line's visit's EAPG Adjusted Relative Weights. The redistributed billed amounts are utilized for the purpose of performing a "lower of" calculation, which will compare that line's redistributed billed amount to its EAPG Payment amount.
Outpatient hospital claims should be billed using Type of Bill 013X (Hospital Outpatient). The EAPG methodology relies on both revenue and Current Procedural Terminology (CPT)/Healthcare Common Procedure Coding System (HCPCS) codes to price claim details. As such, CPT/HCPCS should be billed whenever possible as appropriate for the services delivered. Please note that this is an update from the requirements of the preceding outpatient hospital payment methodology which required claim details billed with certain revenue codes (036X [Operating Room Services], 045X [Emergency Room], etc.) to have their charges aggregated into a single line without a CPT/HCPCS code.
The Department is currently reimbursing using version 3.16 of EAPG methodology.
| Effective Date Range | EAPG Version |
|---|---|
| October 30, 2016, and prior | N/A |
| October 31, 2016, to December 31, 2021 | EAPG version 3.10 |
| January 1, 2022 to June 30, 2025 | EAPG version 3.16 |
| July 1, 2025 to current | EAPG version 3.18 |
Visit the Outpatient Hospital Payment web page for further information on the Department's implementation of the EAPG methodology, including information on Colorado's EAPG Relative Weights and how to obtain the EAPG Definitions Manual from 3M.
Prior to October 31, 2016, reimbursement for Outpatient Hospital Services was calculated by multiplying the submitted charges by the Medicare Part B cost-to-charge ratio of the submitting hospital and then by the Health First Colorado cost ratio (subject to change). Outpatient laboratory, occupational therapy, physical therapy and hospital-based transportation claims were reimbursed based on the lower of submitted charges or Health First Colorado fee schedule.
In-State Billing Providers:
- Reimbursement Amount = Line Item Submitted Charges * Hospital Cost-to-Charge Ratio * Health First Colorado Cost Ratio
Out-of-State Billing Providers:
- Reimbursement Amount = Line Item Submitted Charges * Hospital Cost-to-Charge Ratio* Health First Colorado Cost Ratio
Bundling
"Bundling" describes a single reimbursement package for related services. Health First Colorado reimbursement for inpatient hospital care includes associated outpatient, laboratory and supply services provided immediately prior to the hospital admission and during the hospital stay when billed by the same provider. Refer to the 48-hour Readmission Policy above for circumstances when a member is readmitted to the same hospital within 48 hours after a previous inpatient stay.
Prenatal services such as observation stays and same location emergency department visits provided immediately prior to an inpatient admission are related and are included in the reimbursement for the inpatient claim.
Example:
A member is seen in the emergency department on February 11, 2018. The member is admitted as an inpatient on February 12, 2018. The member is discharged on February 20, 2018.
From Date: February 11, 2018
Admit Date: February 12, 2018
Covered (Inpatient) Days: 8 days (February 12, 2018 - February 20, 2018)
Revenue line items and surgical procedure performed on an outpatient day should be reported (From Date) but should not be reported for the accommodation units and inpatient covered days.
Recurring Visits and Emergency Department/Observation Billing for Outpatient Claims
Emergency Department visits should not be included on outpatient claims describing recurring visits (e.g., regularly scheduled visits for ongoing treatment, such as physical therapy or oncology treatment). Emergency Department visits should be billed separately for the Enhanced Ambulatory Patient Group (EAPG) grouper to calculate payment appropriately per claim and visit. These types of visits are identified by outpatient claims which are billed with Revenue Codes 045X (Emergency Services) or 076X (Specialty Services).
Recurring visits which may include Observation Services should have each visit billed on separate claims to avoid unintended bundling during payment calculation.
Enhanced Ambulatory Patient Group (EAPG) Consolidation and Distinct Procedures
The EAPG reimbursement methodology is utilized to group payment for similar significant procedures when billed on an outpatient hospital claim, such that only the most resource-intensive significant procedure will be payable per visit as determined by the EAPG algorithm. For payment to be calculated appropriately for separate and distinct significant procedures occurring during the same visit, claim details may be billed with modifier 59 to indicate that they are distinct procedural services. Effective for institutional outpatient claims with a first date of service on or after January 1, 2018, modifiers XE, XP, XS and XU may also be used to indicate distinct procedural services.
Additional Medical Visits
Modifier 27 may be reported for multiple outpatient hospital evaluation and management encounters on the same date for an institutional outpatient claim. Line items billed in this way may be assigned ancillary EAPG 449 (Additional Undifferentiated Medical Visits/Services) and are only payable during visits where no significant procedure has taken place.
Bilateral Procedures
Modifier 50 may be reported on institutional outpatient hospital claim details for bilateral procedures performed during the same operative session. Such procedures must be billed on a single claim detail for reimbursement to be calculated appropriately.
340B Drug Billing
Drugs purchased through the 340B Drug Discount Program must be billed with the UD modifier, which will allow the drug to be priced appropriately by the EAPG software. Drugs purchased in this way must be billed at acquisition cost.
| OUTPATIENT CLAIM FIRST DATE OF SERVICE | 340B DISCOUNT |
| October 31, 2016 to March 10, 2018 | 50% |
| March 11, 2018 to June 30, 2025 | 80% |
| July 1, 2025 to current | 65% |
Discarded Portion of Drug Modifier
Discarded portions of drugs provided during an outpatient hospital stay must be billed on a separate line with the JW modifier. These details are not considered payable on an outpatient hospital claim.
Never Event Billing
Modifiers for never events PA (surgery, wrong body part), PB (surgery, wrong patient) and PC (wrong surgery on patient) must be reported when appropriate. These services are not considered payable on an outpatient hospital claim.
Terminated Procedure Reporting
Terminated procedures must be reported with modifiers 52 (reduced services) or 73 (discontinued services prior to anesthesia administration). Reporting with the proper modifier will allow the procedure to be priced appropriately by the EAPG software.
CPT/HCPCS Multiple Units
Billed units should be summed into a single line for each CPT/HCPCs code and date of service. The only exceptions are for required modifiers (e.g., billing two (2) lines for a drug where the discarded portion of the drug must be billed on a separate line with the JW modifier) or when billing drugs with different National Drug Codes (NDCs) but the same HCPCS. On the lines with the repeated drug HCPCS code, a different NDC must be billed for correct processing.
Observation stays that span multiple DOS must have all units summed and billed on a single line.
Billing for Take-Home Naloxone (Opioid Antagonist) for an Outpatient Visit
Effective July 8, 2022, take-home Naloxone will be reimbursed at the fee schedule rate when billed on an outpatient hospital claim with HCPCS G1028 and/or G2215. The outpatient claim must contain the NDC of the drug dispensed. If G2215 is billed on the outpatient claim, it must also include the invoice of the drug dispensed.
Outpatient Hospital Unbundled Durable Medical Equipment (DME) Billing
Since the implementation of EAPGs, the Department has carved out the payment for unbundled DME from its outpatient claims and requests that such line items are billed on the CMS-1500 professional claim. Such line items are subject to the billing rules and payment methodology in place for DME Suppliers. Refer to Appendix G located on the Billing Manual web page under the Appendices drop-down for a listing of the CPT/HCPCS codes which are unbundled from the EAPG methodology.
A CMS 1500 should be used to bill DME only when the procedure code is listed on the Department's Appendix G: Outpatient Hospital Unbundled Durable Medical Equipment Codes. Otherwise, payment for DME is assumed to be a part of EAPG, and the procedure code should go on a UB-04.
Inpatient-Only Procedures
The Department uses both Centers for Medicare & Medicaid Services (CMS) and 3M Enhanced Ambulatory Patient Group (EAPG) Inpatient Only lists. Refer to Appendix O located on the Billing Manual web page under the Appendices drop-down for the 3M EAPG Inpatient Only List. Inpatient-only procedures performed in the outpatient setting are denied.
Observation Billing for Outpatient Claims
Effective for claims with dates of service on or after October 30, 2023
Observation stays are a covered Health First Colorado benefit when provided by or under the direction of a physician for as many days as determined Medically Necessary. The billed line for observation must have an observation time of eight (8) or more hours. With appropriate documentation, members may stay in observation for more than 24 hours and only rarely shall the stay exceed 48 hours in length per 10 CCR 2505-10 8.300.3.B.1.
Observation Stays end when a physician orders either Inpatient admission or discharge from the hospital. An Inpatient admission cannot be converted to an Outpatient Observation Stay after the member is discharged unless for purposes of rebilling after an audit finding as specified in 10 CCR 2505-10 8.043.
The assignment of separate ancillary Observation EAPG is dependent upon specific criteria. This logic is displayed within the Ancillary Observation Processing Logic within the 3M Definitions Manual for 3M Enhanced APG (EAPG) System.
Example 1: HCPCS G0378 is billed with eight plus (8+) billed units on a claim along with a Type 2 Significant Procedure EAPG. Regardless of services billed on the claim, G0378 will be assigned EAPG code 450 and will package.
Example 2: HCPCS G0378 is billed with eight plus (8+) billed units on a claim along with a medical visit and Type 21-25 Significant Procedure EAPG. G0378 will be assigned EAPG code 450 and not be packaged.
Example 3: HCPCS G0378 is billed and no Type 2 Significant Procedure and no medical visit are present. G0378 will be assigned EAPG 999.
Example 4: HCPCS G0378 is billed and no Significant Procedure and no medical visit are present, but a Type 21-25 Significant Procedure is present. G0378 will be assigned EAPG 450 and will package.
Example 5: HCPCS G0378 is billed with eight plus (8+) billed units on a claim along with a medical visit and no Significant Procedure EAPG of any type. G0378 will be assigned EAPG code 450 and not be packaged.
For claims with dates of service prior to October 30, 2023
Observation stays are a covered benefit as follows. Members may be admitted as Outpatients to Observation Stay status. The billed line for observation must have an observation time between eight (8) and 48 hours. With appropriate documentation, members may stay in Observation for more than 24 hours, but an Observation Stay shall not exceed 48 hours in length per 10 CCR 2505-10 8.300.3.B.1. A physician orders either Inpatient admission or discharge from observation. An Inpatient admission cannot be converted to an Outpatient Observation Stay after the member is discharged.
The assignment of separate ancillary Observation EAPG is dependent upon specific criteria. This logic is displayed within the Ancillary Observation Processing Logic within the 3M Definitions Manual for 3M Enhanced APG (EAPG) System.
Example 1: HCPCS G0378 is billed with eight (8)-48 billed units on a claim along with a Type 2 Significant Procedure EAPG. Regardless of services billed on the claim, G0378 will be assigned EAPG code 450 and will package.
Example 2: HCPCS G0378 is billed with eight (8)-48 billed units on a claim along with a medical visit and Type 21-25 Significant Procedure EAPG. G0378 will be assigned EAPG code 450 and not be packaged.
Example 3: HCPCS G0378 is billed and no Type 2 Significant Procedure and no medical visit are present. G0378 will be assigned EAPG 999.
Example 4: HCPCS G0378 is billed and no Significant Procedure and no medical visit are present, but a Type 21-25 Significant Procedure is present. G0378 will be assigned EAPG 450 and will package.
Example 5: HCPCS G0378 is billed with eight (8)-48 billed units on a claim along with a medical visit and no Significant Procedure EAPG of any type. G0378 will be assigned EAPG code 450 and not be packaged.
Billing for Services on Outpatient Claims with a Behavioral Health-Covered Primary Diagnosis Code
The primary diagnosis code on the claim determines when outpatient institutional claims are submitted Fee-for-Service (FFS) or to the Regional Accountable Entity (RAE) that the member is attributed to. Refer to the State Behavioral Health Services (SBHS) Billing Manual for a list of behavioral health diagnosis codes that are covered under the Medicaid Capitated Behavioral Health Benefit and reimbursed by the RAEs.
For Institutional Outpatient Claims:
- If the claim’s primary diagnosis code is a listed RAE-covered diagnosis, the claim should be submitted to the member’s RAE.
- If the claim’s primary diagnosis code is not a listed RAE-covered diagnosis code, the claim should be submitted FFS.
- If the member is not attributed to a RAE, the claim will need to be submitted FFS.
Split billing for behavioral health services provided in a Hospital is not permitted.
Providers may appeal the decision if the claim has been denied by the RAE. Appeal information is listed on the denial letter from the RAE.
Contact HCPF_BHCoding@state.co.us for behavioral health billing questions.
Partial Hospitalizations
When Partial Hospitalization services are delivered by a General Acute Care Hospital, and the principal diagnosis is not a Regional Accountable Entity (RAE)-covered mental health diagnosis, the services may be billed fee-for-service using revenue codes 912 and/or 913. A RAE denial is not necessary to process these claims. These revenue codes have been payable through EAPG since November 20, 2019, and the codes were retroactively opened for billing back to July 1, 2018.
Span Billing
Span billing is allowed for outpatient hospitals, rural health clinics and dialysis centers. Enter the beginning and ending dates of service in form locator 6. Form locator 45 must be completed with the correct date of service using MMDDYY format for each line item submitted. Each date of service must be shown on a separate detail line with a revenue code, procedure code, unit(s) and charge.
Split Bills
For any specified date or date span, billed services must appear on a single UB-04 institutional claim. A paper claim cannot be submitted as a two (20 or more-part claim. Multiple page claim should be submitted through the Provider Web Portal or electronically.
Outpatient claims that span the end of one (1) calendar year and the beginning of the following year should be split billed by year.
Providers reimbursed an encounter rate or per diem must split bill to accommodate the date of the rate change.
Third-Party Payment Prorate
When a provider receives a third-party lump sum payment for multiple services billed to Health First Colorado on separate claim forms (e.g., hospital stay and transportation), the provider should prorate the third-party payment to the multiple services/claims.
Each claim must include a copy of the insurance company's Explanation of Benefits (EOB) or check with a notation that the payment has been applied to multiple claims.
Example (for outpatient and transportation services):
Services incurred were:
Outpatient $800
Transportation $200
Total Billed to Third-Party Payer $1000Lump-sum payment received from Third-Party Payer $700
To prorate third-party payment for multiple Health First Colorado UB-04 institutional claims, determine what percentage of the total charge is represented by each claim amount. Divide each individual claim charge by the total charge.
Outpatient Services $800 ÷ $1,000 = 80%
Transportation Services $200 ÷ $1,000 = 20%
To determine the correct third-party payment amount to enter on each claim, multiply each percentage from the previous calculation times the total amount received from the third-party payer.
These amounts should be entered on the Third-Party Payer line in form locator 54 (Prior Payments).
80% x $700 = $560 on the Outpatient claim
20% x $700 = $140 on the Transportation claim
The amount for the Health First Colorado line in form locator 55 (Estimated Amount Due) is the difference between the total claim charge and the third-party payer prorate amount.
Outpatient $800 - $560 = $ 240
Transportation $200 - $140 = $ 60
Transportation
Effective October 31, 2016, transportation services can no longer be billed on a UB-04 institutional claim by the hospital. Hospitals providing transportation must also enroll as a transportation provider. Such services should be billed on a professional CMS 1500 claim. Refer to the Emergency Medical Transportation (EMT) Billing Manual and the Non-Emergent Medical Transportation (NEMT) Billing Manual for details.
To provide NEMT and/or EMT services, hospitals must complete enrollment to become a Health First Colorado transportation provider.
Visit the Enrollment Types web page to access the application.
Contact Information
Contact NEMT@state.co.us for questions about transportation policy.
Contact the Providers Services Call Center with questions about enrollment or claims.
Procedure/Healthcare Common Procedure Coding System (HCPCS) Codes Overview
The codes used for submitting claims for services provided to Health First Colorado members represent services that are approved by the Centers for Medicare & Medicaid Services (CMS) and services that may be provided by an enrolled Health First Colorado provider.
The Healthcare Common Procedure Coding System (HCPCS) is divided into two (2) principal subsystems, referred to as level I and level II of the HCPCS. Level I of the HCPCS is comprised of Current Procedural Terminology (CPT), a numeric coding system maintained by the American Medical Association (AMA). The CPT is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other health care professionals. Level II of the HCPCS is a standardized coding system that is used primarily to identify products, supplies and services not included in the CPT codes, such as ambulance services and durable medical equipment, prosthetics, orthotics and supplies (DMEPOS) when used outside a physician's office.
Level II codes are also referred to as alpha-numeric codes because they consist of a single alphabetical letter followed by four (4) numeric digits, while CPT codes are identified using five (5) numeric digits.
The Health Insurance Portability and Accountability Act (HIPAA) requires providers to comply with the coding guidelines of the AMA CPT Procedure Codes and the International Classification of Disease (ICD), Clinical Modification Diagnosis Codes. If there is no time designated in the official descriptor, the code represents one (1) unit or session.
The Department updates and revises HCPCS code listings through the billing manuals and bulletins. Providers should regularly consult the billing manuals and monthly bulletins on the Billing Manuals web page and Bulletins web page of the Department's website.
To receive electronic provider bulletin notifications, an email address can be entered into the Provider Web Portal in the Provider Data Maintenance area. Bulletins include updates on approved codes as well as the maximum allowable units billed per procedure.
All outpatient laboratory, occupational therapy, physical therapy, x-ray and hospital-based transportation claims must be billed using both HCPCS and revenue codes. Outpatient laboratory, occupational therapy, physical therapy, and hospital-based transportation claims are reimbursed based on the Health First Colorado fee schedule. Outpatient hospital radiology and diagnostic imaging claims are reimbursed based on the hospital cost-to-charge ratio. Refer to the Outpatient Imaging and Radiology Billing Manual located on the Billing Manuals web page for complete policy and requirements for diagnostic imaging and radiology.
When submitting claims for transportation, outpatient laboratory, occupational therapy, physical therapy and radiology to Health First Colorado, observe the following guidelines:
- Always use the most current CPT revision. Health First Colorado adds and deletes codes as they are published in annual revisions of the CPT.
- Use CMS codes only when CPT codes are not available or are not as specific as the CMS codes.
- Not all codes listed in the annual Health First Colorado HCPCS code publications are benefits of Health First Colorado. Read the entire entry to determine the benefit status of the item.
The CPT code book can be purchased at local university bookstores and from the American Medical Association at the following address:
Book & Pamphlet Fulfillment: OP-341/9
American Medical Association
P.O. Box 10946
Chicago, IL 60610
UB-04 Revenue Codes
The Health First Colorado Revenue Code Table in Appendix Q, located on the Billing Manuals web page under the Appendices drop-down, contains revenue codes for billing services to Health First Colorado. Not all of the revenue codes listed are Health First Colorado benefits. When non-benefit revenue codes are used, the claim must be completed according to the billing instructions for non-covered charges. Claims submitted with revenue codes that are not listed are denied.
UB-04 Paper Claim Reference Table
The information in the following table provides instructions for completing form locators (FL) as they appear on the paper UB-04 institutional claim form. Instructions for completing the UB-04 institutional claim form are based on the current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data form locators on the UB-04 have the same attributes (specifications) for Health First Colorado as those indicated in the NUBC_UB-04 Reference Manual.
All code values listed in the NUBC UB-04 Reference Manual for each form locator may not be used for submitting paper claims to Health First Colorado. The appropriate code values listed in this manual must be used when billing Health First Colorado.
The UB-04 Institutional Certification Form, located on the Provider Forms web page under the Claim Forms and Attachments drop-down menu, must be completed and attached to all claims submitted on the paper UB-04. Completed UB-04 paper claims, including hardcopy Medicare claims, should be mailed to the correct fiscal agent address located in Appendix A, located on the Billing Manuals web page under the Appendices drop-down.
Each claim form has a set number of billing lines available for completion. Do not crowd more lines on the form. Billing lines in excess of the designated number are not processed or acknowledged. Claims with more than one (1) page may be submitted through the Provider Web Portal or batch. The following Paper Claim Reference Table lists the required, optional and conditional form locators for submitting the UB-04 institutional paper claim form to Health First Colorado for Inpatient and Outpatient Hospital Services.
| Form Locator and Labels | Completion Format | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Billing Provider Name, Address, Telephone Number | Text | Inpatient/Outpatient - Required
Abbreviate the state using standard post office abbreviations. Enter the telephone number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Pay-to Name, Address, City, State | Text | Inpatient/ Outpatient - Required if different from form locator 1.
Abbreviate the state using standard post office abbreviations. Enter the telephone number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3a. Patient Control Number | Up to 20 characters: Letters, numbers or hyphens | Inpatient/Outpatient - Optional Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3b. Medical Record Number | 17 digits | Inpatient/Outpatient - Optional Enter the number assigned to the member to assist in retrieval of medical records. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Type of Bill | 3 digits | Inpatient/ Outpatient - Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Federal Tax Number | None | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Statement covers period - From/Through | From:6 digits MMDDYY Through: 6 digits MMDDYY | Inpatient/ Outpatient - Required Inpatient "From" date is the earliest date of service on the bill, or first date of an interim bill. Interim charges may be submitted for All-Patient Refined Diagnosis Related Group (APR-DRG) claims but must meet specific billing requirements. Refer to the Interim Billing section. Outpatient This form locator must reflect the beginning and ending dates of service. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8a. Patient Identifier | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8b. Patient Name | Up to 25 characters, letters and spaces | Inpatient/Outpatient - Required Enter the member's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Patient Address - Street | Characters Letters and numbers | Inpatient/Outpatient - Required Enter the member's street/post office box as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Patient Address - City | Text | Inpatient/Outpatient - Required Enter the member's city as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Patient Address - State | Text | Inpatient/Outpatient - Required Enter the member's state as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Patient Address - ZIP | Digits | Inpatient/Outpatient - Required Enter the member's zip code as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10. Birthdate | 8 digits (MMDDYYYY) | Inpatient/Outpatient - Required Enter the member's birthdate using two (2) digits for the month, two (2) digits for the date and four (4) digits for the year (MMDDYYYY format). Example: 01012025 for January 1, 2025. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Patient Sex | 1 letter | Inpatient/ Outpatient - Required Enter an M (male) or F (female) to indicate the member's sex. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Admission Date | 6 digits | Inpatient - Required Outpatient - Conditional Inpatient Enter the date member was admitted to the hospital. Use MMDDYY format for inpatient hospital claims. Outpatient Required for observation holding beds only. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Admission Hour | 6 digits | Inpatient - Required
Outpatient | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Admission Type | 1 digit | Inpatient/Outpatient - Required Enter the following to identify the admission priority: 1 - Emergency Member requires immediate intervention as a result of severe, life-threatening or potentially disabling conditions. Deliveries should be reported as emergencies. Exempts inpatient hospital and clinic claims from co-pay and PCP referral. Exempts outpatient hospital claims from co-payment and PCP referral only if Revenue Code 0450 or 0459 is present. If span billing, emergency services cannot be included in the span bill and must be billed separately from other outpatient services. 2 - Urgent The member requires immediate attention for the care and treatment of a physical or mental disorder. 3 - Elective The member's condition permits adequate time to schedule the availability of accommodations. 4 - Newborn Required for inpatient and outpatient hospital. 5 - Trauma Center Visit to a trauma center/hospital as licensed or designated by the state or local government authority authorized to do so, or as verified by the American College of Surgeons and involving trauma activation. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Source of Admission | 1 digit | Inpatient/ Outpatient - Required
✓ Triggers Transfer Pricing (LTACs and Rehab Hospitals are exempt). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Discharge Hour | 2 digits | Inpatient - Required Enter the hour the member was discharged from inpatient hospital care. Use the same coding used in FL 13 (Admission Hour.) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Patient Discharge Status | 2 digits | Inpatient/Outpatient Required Inpatient/Outpatient
✓ Triggers Transfer Pricing (LTAC and Rehab Hospitals are exempt) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18-28. Codes and Conditions | 2 digits | Inpatient/Outpatient -- Conditional Complete with as many codes as necessary to identify conditions related to this bill that may affect payer processing.
Complete with as many codes as necessary to identify conditions related to this bill that may affect payer processing.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Accident State | 2 digits | Inpatient/Outpatient - Optional State's abbreviation where accident occurred | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31 - 34. Occurrence Code/Date | 2 digits and 6 digits | Inpatient/Outpatient - Conditional
*Other Payer occurrence codes 24 and 25 must be used when applicable. The claim must be submitted with the third-party information. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35-36. Occurrence Span Code From/ Through | 2 digits |
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38. Responsible Party Name/Address | None | Submitted information is not entered into the claim processing system | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39 - 41. Value Codes and Amounts | 2 digits and 9 digits | Inpatient/Outpatient - Conditional Enter appropriate codes and related dollar amounts to identify monetary data or number of days using whole numbers necessary for the processing of this claim. Never enter negative amounts. If a value code is entered, a dollar amount or numeric value related to the code must always be entered.
For Rancho Coma Score bill with appropriate diagnosis for head injury. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 42. Revenue Code | 4 digits | Inpatient/Outpatient - Required Psychiatric step down | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 43. Revenue code Description | Text | Inpatient/Outpatient - Required
Examples include:
Refer to the claim example included in this billing manual. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 44. HCPCS/Rates/ Health Insurance Prospective Payment System (HIPPS) Rate Codes | 5 digits | Inpatient - Not required Outpatient - Conditional
Enter HCPCS and revenue codes for each radiology line. The only valid modifier for outpatient radiology is TC. Visit the Bulletins web page and locate the most current HCPCS Special Provider Bulletin. With the exception of outpatient lab and hospital-based transportation, outpatient radiology services can be billed with other outpatient services. HCPCS codes must be identified for the following revenue codes:
HCPCS codes cannot be repeated for the same date of service. Combine the units in form locator 46 (Service Units) to report multiple services. Outpatient - Conditional Enter only the HCPCS code for each detail line. The following revenue codes always require a HCPCS code. Refer to Appendix X: HCPCS / NDC Crosswalk for Billing Physician-Administered Drugs for a list of physician-administered drugs that also require an NDC code. When a HCPCS code is repeated more than once per day and billed on separate lines, use modifier 76 to indicate this is a repeat procedure and not a duplicate.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 45. Service Date | 6 digits | Inpatient - Leave blank Outpatient - Required For span bills only | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 46. Service Units | 3 digits | Inpatient/Outpatient - Required Enter a unit value on each line completed. Use whole numbers only. Do not enter fractions or decimals and do not show a decimal point followed by a zero (0) to designate whole numbers (e.g., Do not enter 1.0 to signify one [1] unit) The grand total line (Line 23) does not require a unit value. For span bills, the units of service reflect only those visits, miles or treatments provided on dates of service in form locator 45. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 47. Total Charges | 9 digits | Inpatient/Outpatient - Required Enter the total charge for each line item. Calculate the total charge as the number of units multiplied by the unit charge. Do not subtract Medicare or third-party payments from line charge entries. Do not enter negative amounts. A grand total in line 23 is required for all charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 48. Non-covered Charges | 9 digits | Inpatient/Outpatient - Conditional Enter incurred charges that are not payable by Health First Colorado. Non-covered charges must be entered in both form locator 47 (Total Charges) and form locator 48 (Non-Covered Charges). Each column requires a grand total. Non-covered charges cannot be billed for outpatient hospital laboratory or hospital-based transportation services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 50. Payer Name | 1 letter and text | Enter the payment source code followed by name of each payer organization from which the provider might expect payment.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 51. Health Plan ID | 8 digits | Inpatient/Outpatient - Required Enter the provider's Health Plan ID for each payer name. Enter the eight (8)-digit Health First Colorado provider ID assigned to the billing provider. Payment is made to the enrolled provider or agency that is assigned this number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 52. Release of Information | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 53. Assignment of Benefits | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 54. Prior Payments | Up to 9 digits | Inpatient/Outpatient - Conditional Complete when there are Medicare or third-party payments. Enter third-party and/or Medicare payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 55. Estimated Amount Due | Up to 9 digits | Inpatient/Outpatient - Conditional Complete when there are Medicare or third-party payments. Enter the net amount due from Health First Colorado after provider has received other third-party, Medicare or member liability amounts. Medicare Crossovers Enter the sum of the Medicare coinsurance plus Medicare deductible less third-party payments and member payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 56. National Provider Identifier (NPI) | 10 digits | Inpatient/Outpatient - Required Enter the billing provider's 10-digit National Provider Identifier (NPI). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 57. Other Provider ID | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 58. Insured's Name | Up to 30 characters | Inpatient/Outpatient - Required Enter the member's name on the Health First Colorado line. Other Insurance/Medicare Complete additional lines when there is third-party coverage. Enter the policyholder's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 60. Insured's Unique ID | Up to 20 characters | Inpatient/Outpatient - Required Enter the insured's unique identification number assigned by the payer organization exactly as it appears on the health insurance card. Include letter prefixes or suffixes shown on the card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 61. Insurance Group Name | 14 letters | Inpatient/Outpatient - Conditional Complete when there is third-party coverage. Enter the name of the group or plan providing the insurance to the insured exactly as it appears on the health insurance card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 62. Insurance Group Number | 17 digits | Inpatient/Outpatient - Conditional Complete when there is third-party coverage. Enter the identification number, control number or code assigned by the carrier or fund administrator identifying the group under which the individual is carried. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 63. Treatment Authorization Code | Up to 18 characters | Inpatient/Outpatient - Conditional Complete when the service requires a Prior Authorization Request (PAR). Enter the authorization number in this form locator if a PAR is required and has been approved for services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 64. Document Control Number | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 65. Employer Name | Text | Inpatient/Outpatient - Conditional Complete when there is third-party coverage. Enter the name of the employer that provides health care coverage for the individual identified in form locator 58 (Insured Name). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 66. Diagnosis Version Qualifier | Submitted information is not entered into the claim processing system. Enter applicable ICD indicator to identify which version of ICD codes is being reported. 0ICD-10-CM (DOS 10/1/15 and after) 9ICD-10-CM (DOS 9/30/15 and before) Outpatient Hospital Laboratory May use diagnosis code Z04.9. Hospital-Based Transportation May use diagnosis code R68.89 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67. Principal Diagnosis Code | Up to 6 digits | Inpatient/Outpatient - Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67A. - 67Q. - Other Diagnosis | Up to 6 digits | Inpatient/Outpatient - Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 69. Admitting Diagnosis Code | Up to 6 digits | Inpatient - Required Outpatient - Optional Enter the diagnosis code as stated by the physician at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 70. Patient Reason Diagnosis | Up to 6 digits | Submitted information is not entered into the claim processing system. Outpatient - Required for all unscheduled outpatient visits. Enter the ICD-CM diagnosis codes describing the member's reason for visit at the time of outpatient registration. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 71. PPS Code | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 72. External Cause of Injury code (E-Code) | Up to 6 digits | Inpatient/Outpatient - Optional Enter the diagnosis code for the external cause of an injury, poisoning or adverse effect. This code must begin with an "E". | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74. Principal Procedure Code/Date | Up to 7 characters or up to 6 digits | Inpatient/Outpatient - Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 75. Unlabeled Field | N/A | N/A | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 76. Attending NPI - Required Attending Last/First Name | NPI - 10 digits Text | Health First Colorado ID Required NPI - Enter the 10-digit NPI number assigned to the physician having primary responsibility for the member's medical care and treatment. This number is obtained from the physician and cannot be a clinic or group number. (If the attending physician is not enrolled in Health First Colorado, or if the member leaves the ER before being seen by a physician, the hospital may enter their individual numbers.) Hospitals may enter the member's regular physician's 10- digit NPI in the Attending Physician ID form locator if the locum tenens physician is not enrolled in Health First Colorado. QUAL - Enter "1D" for Medicaid. Enter the attending physician's last and first name. This form locator must be completed for all services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 77. Operating NPI | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 78 - 79. Other ID NPI - Conditional | NPI - 10 digits | Conditional - Complete when attending physician is not the PCP or to identify additional physicians. Ordering, Prescribing, or Referring NPI - when applicable NPI - Enter up to two (2) 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attending physician is not the PCP, or if a clinic is a PCP agent, enter the PCP NPI number as the referring physician. The name of the Health First Colorado member's PCP appears on the eligibility verification. Review either for eligibility or PCP. Health First Colorado does not require that the PCP number appear more than once on each claim submitted. The attending physician's last and first name are optional. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 80. Remarks | Text | Enter specific additional information necessary to process the claim or fulfill reporting requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 81. Code - QUAL/CODE/VALUE (a-d) | Qualifier: 2 digits Taxonomy Code: 10 digits | Optional Complete both the qualifier and the taxonomy code for the billing provider in field 81CC-a. Field 81CC-a must be billed with qualifier B3 for the taxonomy code to be captured in the claims processing system. If B3 is missing, no taxonomy code will be captured in the claims processing system. Only one (1) taxonomy code can be captured from field 81CC. If more than one (1) taxonomy code is provided, only the first instance of B3 and taxonomy code will be captured in the claims processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Timely Filing
Refer to the General Provider Information Manual available on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Sterilization, Hysterectomies and Abortions
Refer to the Obstetrical Care Billing Manual on the Billing Manuals web page for more information on Sterilization, Hysterectomies and Abortions.
Institutional Provider Certification
The Institutional Provider Certification form is located on the Provider Forms web page under the Claim Forms and Attachments drop-down menu.
Inpatient Hospital Claim Example
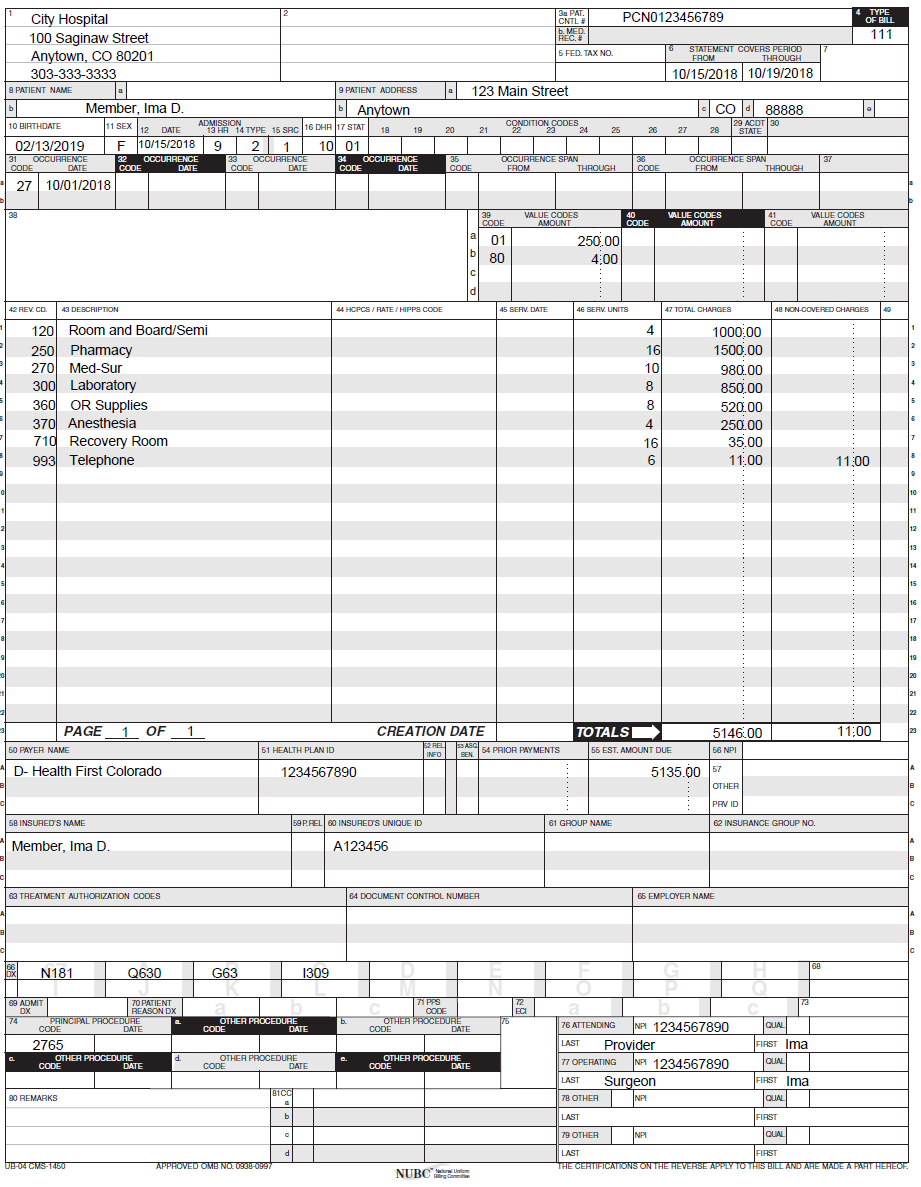
Inpatient for Combined Stay Under 48-Hour Readmission Policy Claim Example
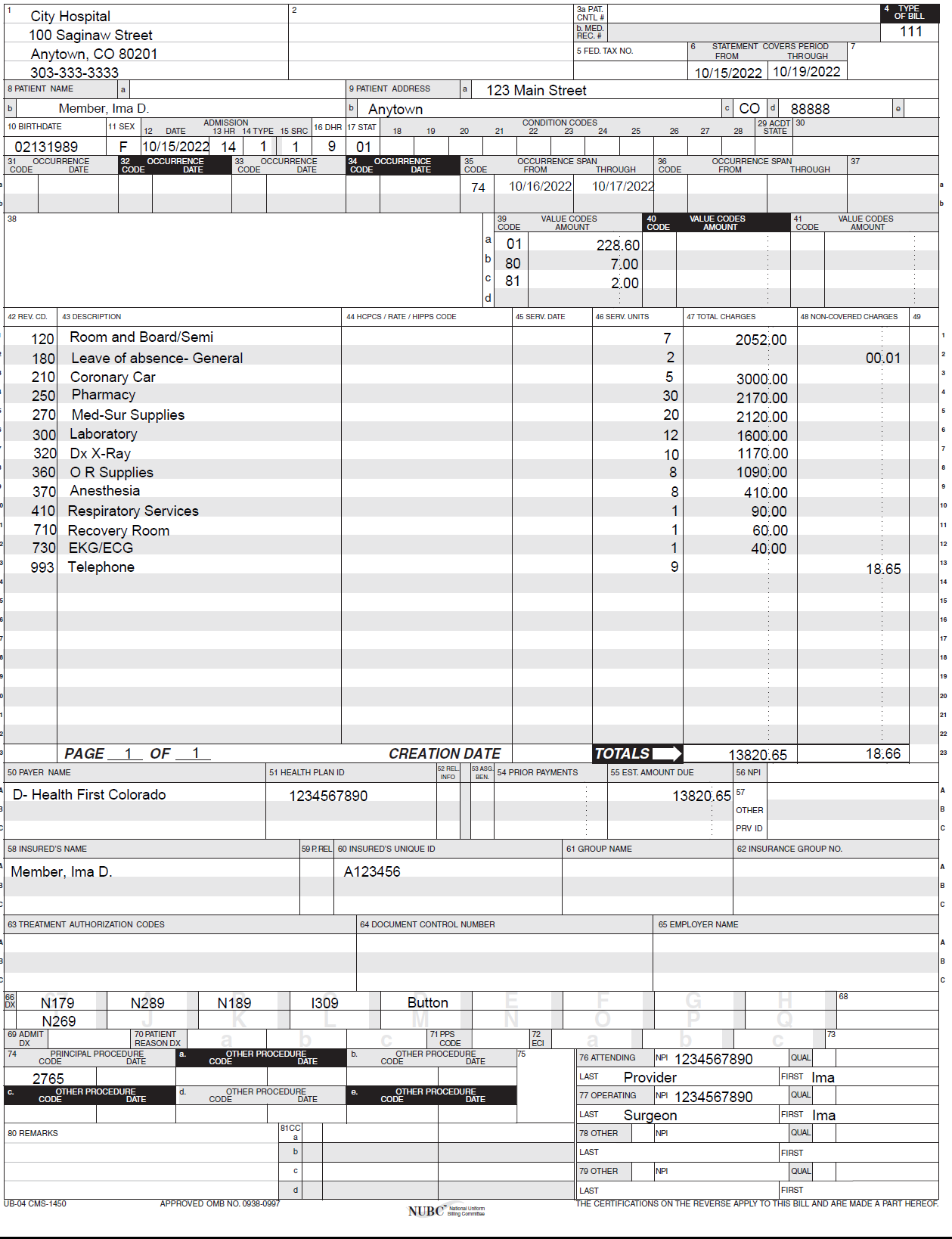
Outpatient Hospital Medicare Claim Example
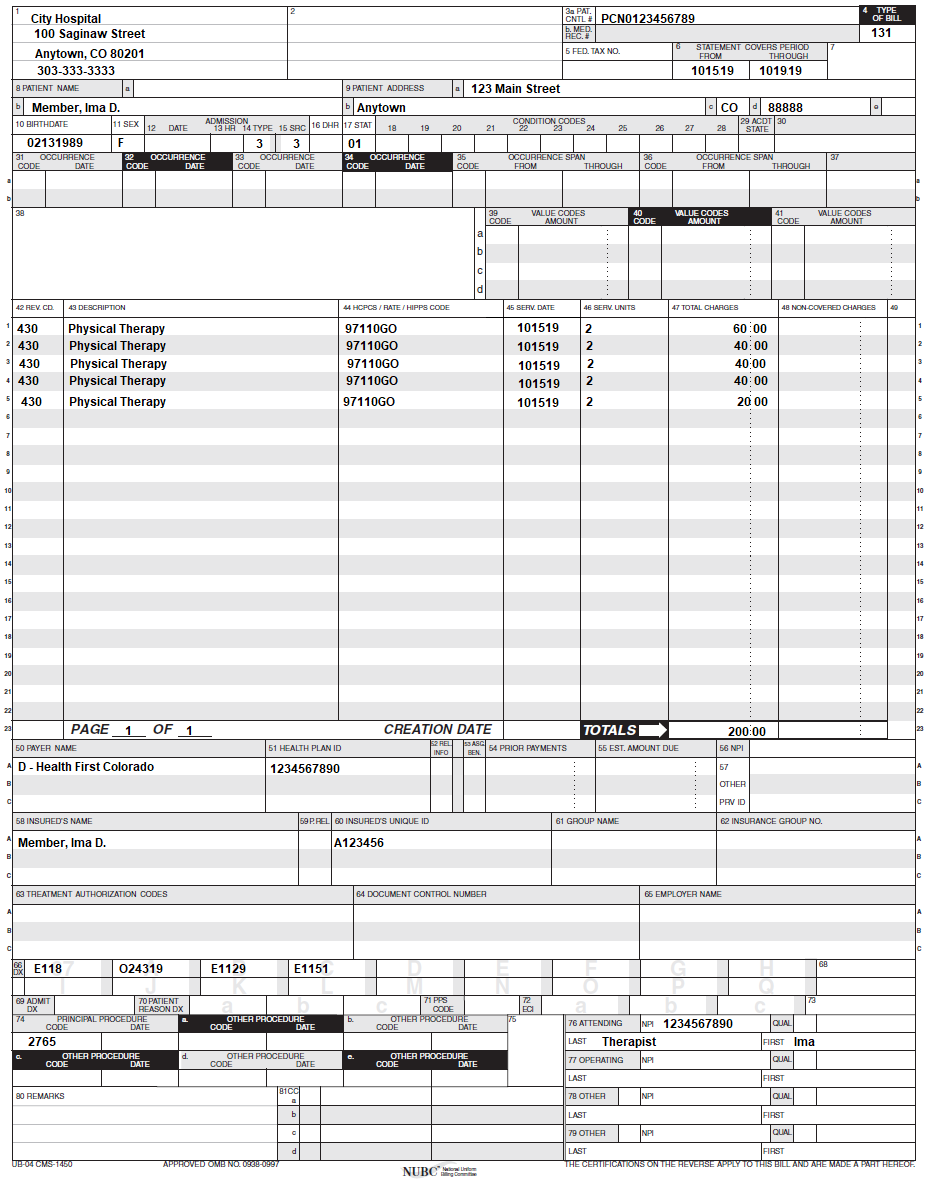
Outpatient Hospital Lab and X-Ray Claim Example
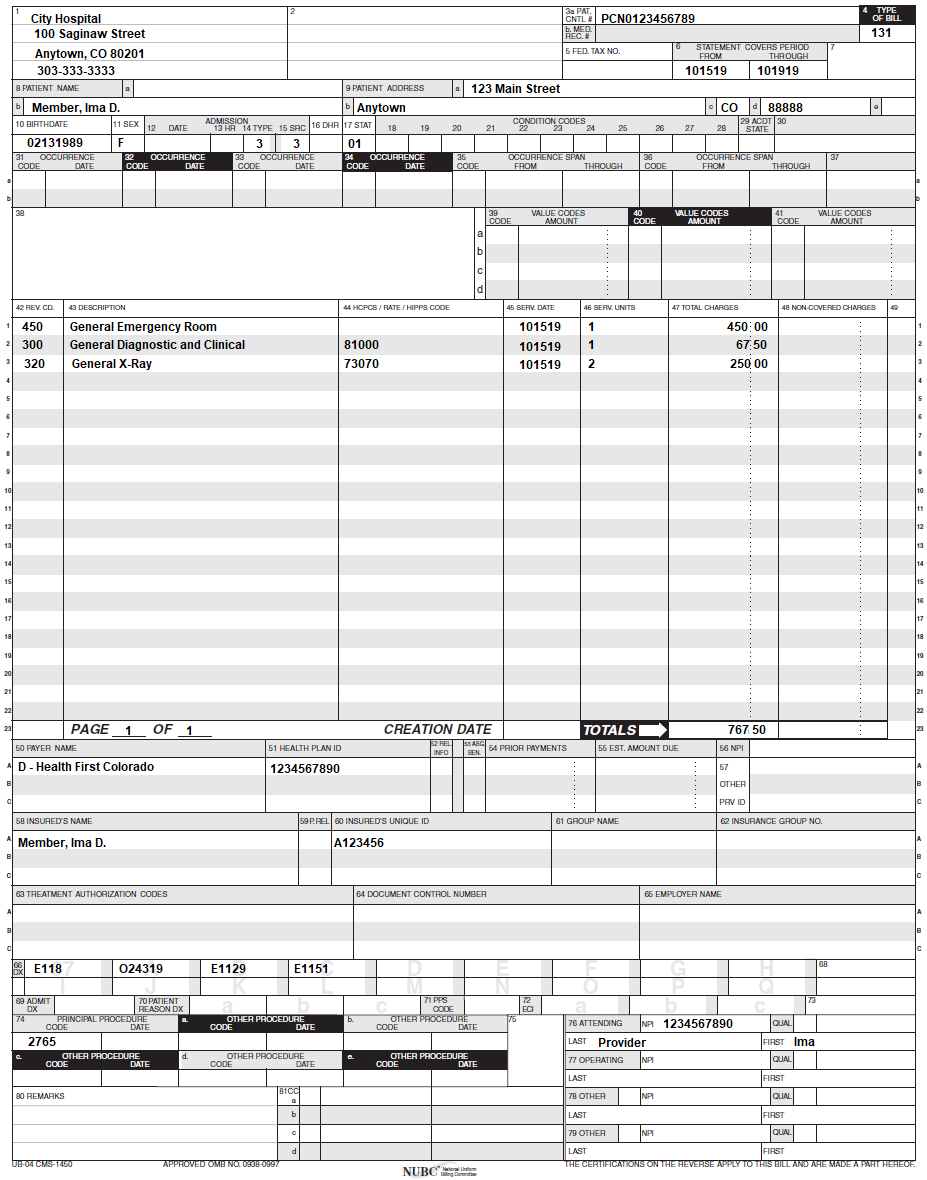
Outpatient Hospital Crossover Claim Example
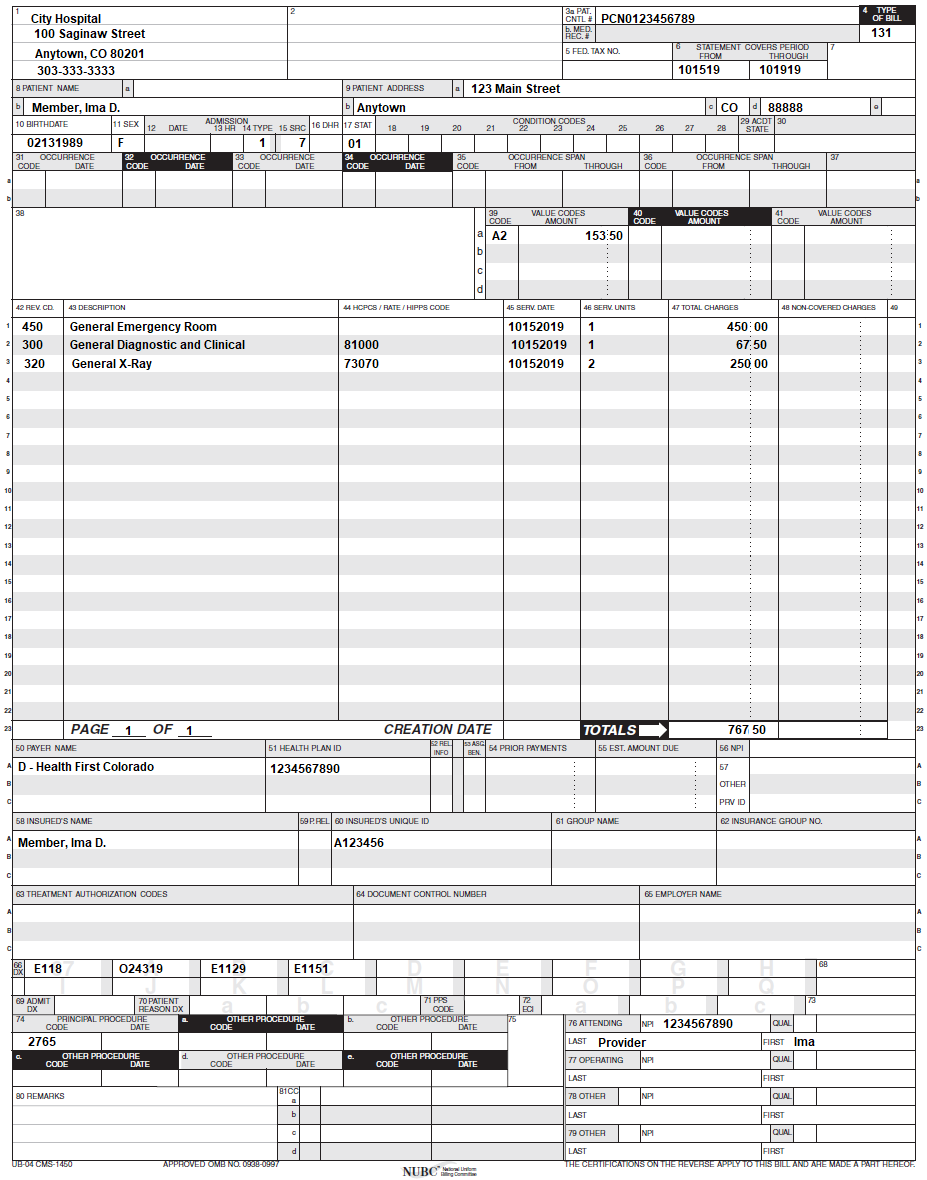
Inpatient Hospital Medicare Part A Claim Example
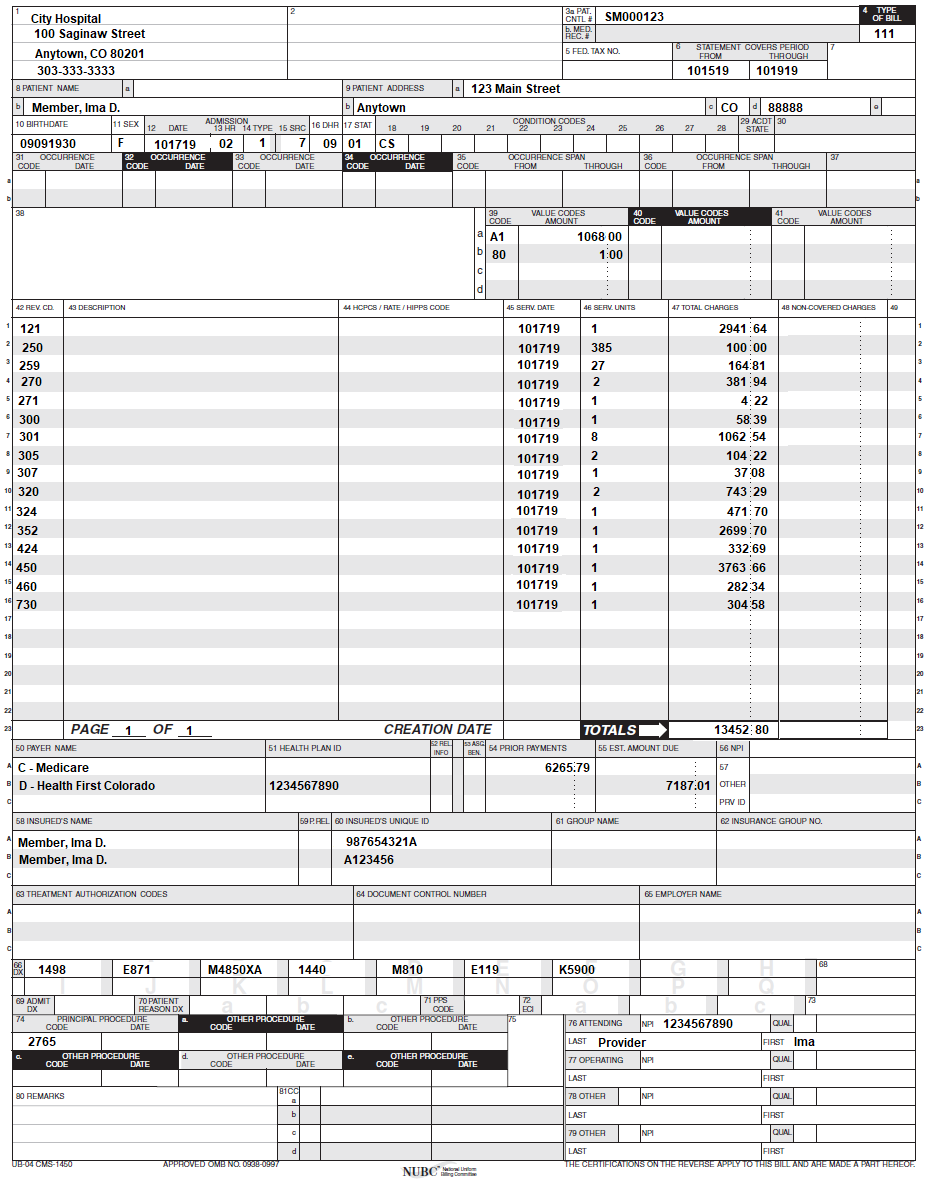
Outpatient Hospital with National Drug Code (NDC) Claim Example
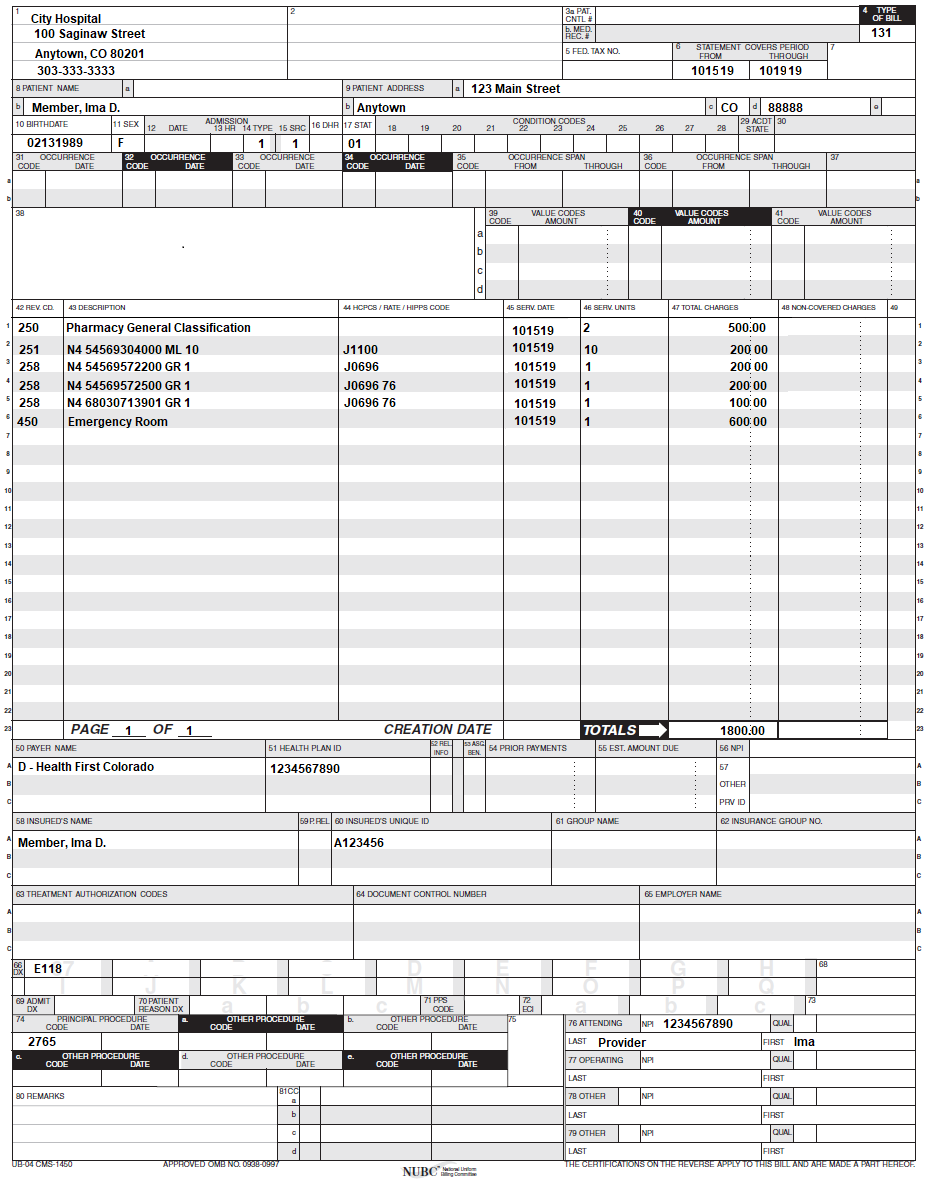
State Mental Hospital Claim Example
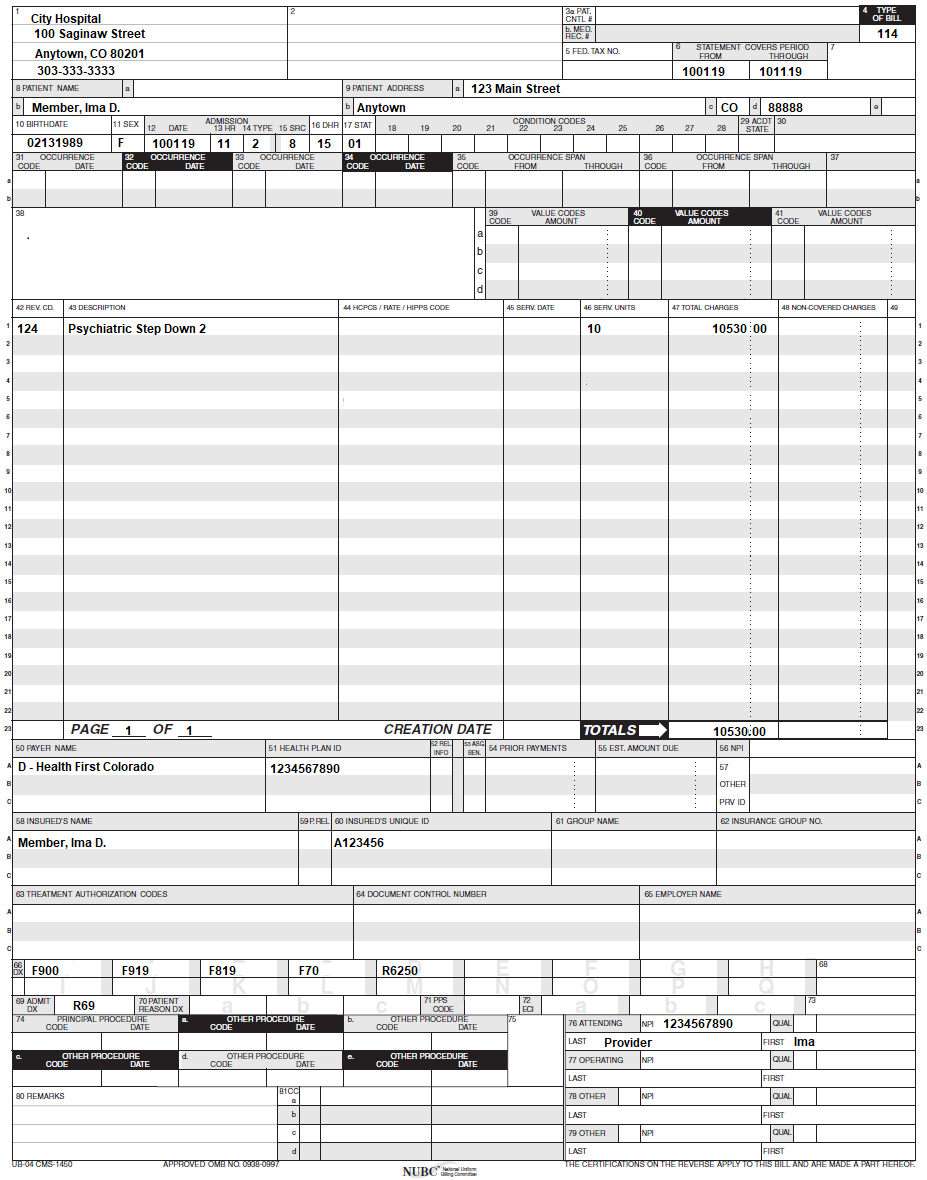
Inpatient/Outpatient Revisions Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 12/01/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx. | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_3.xlsx. | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_4.xlsx. | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 3/13/2017 | Updated the Type of Bill section in the Paper Claims Table to reflect the NUBC manual | RC |
| 5/26/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 4/5/2018 | Updated Inpatient Part B section | AL |
| 6/25/2018 | Updated billing and timely to point to general manual | HCPF |
| 6/28/2018 | Minor Grammatical Updates | HCPF |
| 7/9/2018 | Reduced space on ToC, Removed superscripted "st" from 1 | HCPF |
| 4/29/2019 | Revision of Manual | HCPF |
| 6/26/2019 | Reformatted manual to correct page number issue | HCPF |
| 8/26/2019 | Corrected typo on professional fees | HCPF |
| 9/18/2019 | Added specialty drug carveout section | HCPF |
| 10/31/2019 | Added Source Payment Code H | HCPF |
| 12/02/2019 | Converted to web page | HCPF |
| 01/07/2020 | Updated interim information | DXC |
| 1/28/2020 | Updated Multiple Sections | HCPF |
| 4/23/2020 | Added Split-Bill Instructions for Long Term Acute Care, Rehabilitation and Spine/Brain Injury Treatment Specialty Hospital | HCPF |
| 7/2/2020 | Updated maternity/newborn section | HCPF |
| 8/7/2020 | Updated item 81 of the Paper Claim Reference Table for taxonomy code billing | DXC |
| 8/31/2020 | Added Inpatient Subacute Care Section, updated maternity/newborn billing. | HCPF |
| 12/11/2020 | Added information regarding SUD and IP Only Services | HCPF |
| 5/4/2021 | Added information regarding DPU enrollment | HCPF |
| 7/8/2021 | Added section on Medicaid and Criminal Justice Involved Populations | HCPF |
| 11/5/2021 | Added information in Inpatient Hospital Billing Information section regarding discharge or death on the same day of admission | HCPF |
| 11/5/2021 | Added information in Billing for Non-Covered Days section regarding leave of absence | HCPF |
| 11/5/2021 | Made edits to the incarcerated care section | HCPF |
| 9/14/2022 | Created section for Observation Billing in Outpatient Claims and added information to CPT/HCPCS Multiple Units section | HCPF |
| 11/2/2022 | Updated example images for Inpatient and 48-hour readmission | HCPF |
| 11/22/2022 | Updated DXC reference to “the fiscal agent of the Department” under the Late Charges section | HCPF |
| 11/22/2022 | Added EPSDT, Gender Affirming Care, and Partial Hospitalizations sections. Added information on Outpatient limitations to care. Updated general formatting. Updated information on outpatient specialty carveout drugs. | HCPF |
| 2/23/2023 | Updated IHRP section | HCPF |
| 5/17/2023 | Updated EAPG reimbursement with chart | HCPF |
| 9/19/2023 | Updated Special Instructions for Labor and Delivery Claims, Out-of-State Hospital Services and address under billing info. Added Transplant Billing, OPR guidance, Billing for Take-Home Naloxone and Co-pay section. Made some minor edits for consistency. | HCPF |
| 10/5/2023 | Removed Billing for Take-Home Naloxone section to make updates | HCPF |
| 10/30/2023 | Updated hospital services definitions. Updated observation billing guidance | HCPF |
| 11/8/2023 | Adding Billing for Take-Home Naloxone guidance and updated Outpatient Hospital Specialty Drug Carveout section | HCPF |
| 1/5/2024 | Added DME clarification to Outpatient Hospital Bundling section | HCPF |
| 3/11/2024 | Added billing guidance for Outpatient Hospital claims with RAE covered diagnosis code. Updated language in the birthing parent and newborn billing section. | HCPF |
| 10/10/2024 | Updated Medicaid Member Terminology, Bundling section, transfer logic for LTAC/Rehab hospitals, OPR section. Addition of EMS Billing Manual section and link. Updated IHRP to IHT. | HCPF |
| 11/15/2024 | Added link to the Inpatient Hospital Payment webpage for APR-DRG version updates. | HCPF |
| 2/28/2025 | Update to CPT/HCPCS Multiple Units Section for observation billing guidance. | HCPF |
| 5/2/2025 | Added Hospital Specialty Drug Policy Section. Moved information from Outpatient Hospital Specialty Drug Carveout Section to new Hospital Specialty Drug Policy. | HCPF |
| 10/15/2025 | Added clarifying language for how APR-DRG claims utilize last date of service to determine base rate, APR-DRG version, and APR-DRG weights used to price claims. Added EAPG version 3.18 effective dates and 340B drug discount table. Updated paper claim reference table. | HCPF |