Nursing Facility Billing Manual
- Nursing Facility
- Timely Filing
- Change of Ownership (CHOW) or Change in Tax Identification Number
- Medicare Crossover Claims
- General Member Eligibility Requirements
- Medical and Non-Medical Leave Days
- Revenue Coding
- UB-04 Paper Claim Reference Table
- Nursing Facility Claim Examples
- Prior Authorization - PETI/IME
- Create Prior Authorization in the Provider Web Portal
- Nursing Facility Manual Revisions Log
Return to Billing Manuals Web Page
Nursing Facility
Nursing Facility Overview
The Nursing Facility program provides skilled and maintenance services to members meeting long-term care guidelines. Long-term guidelines are based on a member's functional needs assessment in several areas.
Providers should refer to the Code of Colorado Regulations, Program Rules (10 C.C.R. 2505-10), for specific information when providing nursing facility care. Refer to Section 8.
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Change of Ownership (CHOW) or Change in Tax Identification Number
Nursing facilities are required to notify the Nursing Facility Operations Specialist at HCPF_LTC_Facilities@state.co.us when there is a change of ownership or a change of tax ID number. Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for other CHOW requirements.
Refer to Department rule 10 C.C.R. 2505-10, section 8.443 for further CHOW requirements.
- Notice must be given to the Department of Health Care Policy & Financing's (the Department) Nursing Facility Operations Specialist at least 45 days before the change is to occur.
- The new owner is encouraged to obtain a new NPI.
- New owner must have their own Health First Colorado (Colorado's Medicaid program) billing number before they can bill Health First Colorado.
Medicare Crossover Claims
When the member is dually eligible (both Medicare/Health First Colorado eligible, most claims for nursing facility services are automatically, electronically transferred from Medicare to Health First Colorado. This is known as a "crossover."
If a crossover claim does not appear on the Medical Assistance Program Remittance Advice (RA) within 30 days after the Medicare processing date, a provider must submit the crossover either electronically through the Provider Web Portal or on paper.
Nursing facility services are a Medicare Part A benefit if the member is discharged after a hospital stay of at least three (3) days and qualifies for skilled nursing care as defined by Medicare. Some services for nursing facility residents may qualify for Medicare Part B coverage.
Medicare Part A Crossover Claims
Medicare Part A reimburses the first through the 20th day of the Nursing Facility stay at 100% of the Medicare allowed rate. The 21st through the 100th day are subject to a coinsurance amount per day.
Health First Colorado uses the "lower of" pricing formula to process the coinsurance amount.
Please note the proper completion of the following UB-04 form locators (FL) when submitting a Medicare Part A paper-based crossover claim:
| Form Locator | Instructions |
| 39-41 | Value Codes/Amount - Enter the appropriate value code and related dollar amount that identifies Medicare Coinsurance and Medicare payment amount. A2 is the amount billed to Medicare Coinsurance, A3 is the amount Medicare paid |
| 42 | Revenue Code - Enter appropriate revenue code. |
| 44 | Rates - Enter Nursing Facility's Health First Colorado per diem rate. |
| 50 | Payer Name - Enter Health First Colorado on the appropriate payer line. |
| 51 | Health Plan ID - Enter the Nursing Facility's NPI number |
| 60 | Insured's Unique ID - Enter the Member's Health First Colorado State ID number |
Medicare Part B Crossover Claims
Some dually eligible members do not qualify for comprehensive skilled nursing care as defined by Medicare but do quality for certain nursing facility ancillary services (e.g., physical therapy). Medicare Part B processes benefit ancillary services. Part B services are subject to the Medicare annual deductible and reimbursed at 80% by Medicare.
Note the proper completion of the following UB-04 form locators (FL) when submitting a Medicare Part B paper-based crossover claim:
| Form Locator | Instructions |
| 39-41 | Value Codes/Amount - Enter the appropriate value code and related dollar amount that identifies Medicare Coinsurance and Medicare payment amount. A2 is the amount billed to Medicare Coinsurance, A3 is the amount Medicare paid |
| 42 | Revenue Code - Enter appropriate revenue code. |
| 50 | Payer Name - Enter Health First Colorado on the appropriate payer line. |
| 51 | Health Plan ID - Enter the Nursing Facility's NPI number |
| 60 | Insured's Unique ID - Enter the Member's Health First Colorado State ID number |
General Member Eligibility Requirements
ULTC 100.2 and 5615 Forms
The Uniform Long-term Care (ULTC) 100.2 form must include medical information from the medical provider. Forms are filed by the SEP via the "Bridge" which directly interfaces with the Colorado interChange System. Access to the Bridge is accomplished via the Medicaid Enterprise User Provisioning System (MEUPS).
The nursing facility (or hospital) completes only the Initial Screening and Intake and Professional Medical Information portions and submits these two (2) portions of the form to the Single-Entry Point (SEP). When the SEP completes the ULTC 100.2 and approves the care, a confirmation number is assigned and the approval is faxed to the nursing facility.
Approval of a ULTC 100.2 does not guarantee Health First Colorado payment and does not serve as a timely filing waiver. Authorization only assures that the approved service is a medical necessity and is considered a benefit of the Health First Colorado.
The County Income Maintenance Technician reviews and determines the financial eligibility of the member. The county updates CBMS with the member's financial information and sends the completed 5615 form to the nursing facility. The facility verifies member eligibility using the Provider Web Portal and bills for dates of service.
All claims, including those for prior authorized services, must meet eligibility and claim submission requirements before payment can be made (e.g., timely filing, Primary Care Physician information completed appropriately, third party resources payment(s) pursued, required attachments included, etc.).
Prior to March 1, 2017, a Nursing Facility Prior Authorization was created by the ULTC 100.2 and the 5615 form. After March 1, 2017, this prior authorization was discontinued as the ULTC 100.2 and 5615 form information is systematically matched. However, the ULTC 100.2 and 5615 forms are still provided to the nursing facility. Additionally, the member's program aid code should be "MJ", indicating the applicable level of care.
Member Liability Amount
The Member Liability Amount is payment made by the member for nursing facility care, after the personal needs allowance and other approved expenses are deducted from the member's income.
The County Income Maintenance Technician determines the member liability amount by identifying the personal needs allowance amount and other approved deductions. The 5615 form is used to communicate the calculated amount to the facility.
Refer to program rules for more details on the 5615 form, facility responsibilities and county responsibilities. Section 8.400-8.499.
When reporting the member liability amount for the entire month, the full member liability amount must be applied to the member's care at the beginning of each month as Health First Colorado is the payer of last resort.
How to calculate member liability amount for a partial month
- Calculate the Health First Colorado amount by multiplying the number of days in the facility (excluding the date of discharge) times the per diem rate.
- If the Health First Colorado amount exceeds the member liability amount, the partial month's member liability amount remains the same as the regular member liability amount.
- If the member liability amount is more than the Health First Colorado amount, the partial month's member liability amount is considered the same as the Health First Colorado amount. The excess of the member liability amount over the partial month's member liability amount belongs to the member and, if it has already been paid to the facility, shall be refunded to the member.
Medical and Non-Medical Leave Days
Medical Leave Days
Medical leave days are days that the member is absent from the nursing facility due to an inpatient hospital stay or admittance to another institution (e.g., skilled bed payable by Medicare). Medical leave days must be ordered by a physician and documented in the member's medical record. Medical leave days must be tracked on the facility's daily census report.
Nursing facility medical leave days are not a Health First Colorado benefit.
Non-Medical Leave Days
Non-medical leave days are leave days from the nursing facility for non-medical reasons (e.g., visits to the homes of family or friends or absences for therapeutic and/or rehabilitative reasons.) The attending physician must approve the leave and certify that the leave is not contrary to the member's plan of care. Approval must be documented in the member's medical record. Non-medical leave days must be tracked on the facility's daily census report.
Excessive Non-Medical Leave Days
Health First Colorado pays for a total of 42 non-medical leave days per calendar year. With physician approval, members may pay for room reservations in excess of the combined total of 42 non-medical leave days per calendar year. Approval must be documented in the member's medical record. Non-medical leave days must be tracked on the facility's daily census report.
Revenue Coding
The following tables identify the only valid revenue codes for billing nursing facility services to Health First Colorado. Claims submitted with revenue codes that are not listed below will be denied.
Type of Bill Codes
Type of Bill (TOB) code is based on the type of provider account established within the MMIS interChange system. Use the following information to determine which TOB code to use when billing inpatient, Medicare Part B and outpatient claims.
For nursing facilities - provider type 20
| Specialty Code | Type of Bill |
|---|---|
| 382 - Hospital Backup Unit (HBU) | 21x, 22x, 23x |
| 392 - Nursing Facility Regular (NF/SNF) | |
| 392 - Nursing Facility Regular (QMB Only) | |
| 396 - SNF Swing Bed | 28x, 22x, 23x |
For intermediate care facilities - provider type 21
| Specialty Code | Type of Bill |
|---|---|
| 383 - ICF Level I - Privately owned | 65x, 22x, 23x |
| 394 - ICF Level II - State owned | 66x, 22x, 23x |
Nursing Facility Revenue Codes
| Revenue Code | Description |
| 0119 | Private Room * (valid with TOB 21x, 28x, 65x, 66x) |
| 0129 | Semi-Private Room (valid with TOB 21x, 28, 65x, 66x) |
| 0182 | Non-Medical Leave Days (member convenience) |
| 0183 | Non-Medical Leave Days (therapeutic) |
| 0185 | Medical Leave Days (Hospitalization) |
| 042X | Physical Therapy |
| 043X | Occupational Therapy |
| 044X | Speech Therapy |
* Health First Colorado reimburses the facility for a member in a private room at the semi-private per diem rate. There is no additional reimbursement for a member in a private room.
Post Eligibility Treatment of Income/Incurred Medical Expenses (PETI/IME)
In addition to the above codes, seven (7) state-specific revenue codes for PETI/IME can be billed on nursing facility claims. PETI/IME services include services that are medically necessary but are not covered by Health First Colorado (e.g., hearing aids, eyeglasses).
PETI/IME services can only be billed on claims that have an accommodation line item revenue code and a member liability amount greater than zero.
As of March 1, 2017, all PETI/IME services must be prior authorized (PA) by the Department.
All PETI/IME services must be submitted through the Provider Web Portal for Department review and determination. All required documents must be attached to the request. A PA confirmation number is provided for tracking the status of the request. Once PA is approved by the Department, the provider can bill the PETI/IME service on the next claim containing a member liability amount greater than zero.
Refer to the Prior Authorization - PETI/IME section below for further information.
PETI/IME Revenue Codes
| Revenue Code | Description |
| 0259 | Non-covered Prescription Drugs |
| 0479 | Hearing and Ear Care |
| 0949 | Acupuncture |
| 0962 | Vision and Eye Care |
| 0969 | Dental Services * |
| 0982 | Other Outpatient Services |
| 0999 | Health Insurance Premiums and Other Approved Services |
*Dental Services only applicable after the $1,000 State Benefit has been exhausted or Health First Colorado has denied the service.
UB-04 Paper Claim Reference Table
The information in the following table provides instructions for completing form locators (FL) as they appear on the paper UB-04 claim form. Instructions for completing the UB-04 claim form are based on the current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data form locators on the UB-04 have the same attributes (specifications) for Health First Colorado as those indicated in the NUBC UB-04 Reference Manual.
All code values listed in the NUBC UB-04 Reference Manual for each form locator may not be used for submitting paper claims to Health First Colorado. The appropriate code values listed in this manual must be used when billing Health First Colorado.
The UB-04 Certification document must be completed and attached to all claims submitted on the paper UB-04. Completed UB-04 paper Health First Colorado claims, including hardcopy Medicare claims, should be mailed to the correct fiscal agent address listed in Appendix A located on the Billing Manuals web page under the Appendices drop-down.
Do not submit "continuation" claims. Each claim form has a set number of billing lines available for completion. Do not crowd more lines on the form.
Billing lines in excess of the designated number are not processed or acknowledged. Claims with more than one (1) page may be submitted through the Provider Web Portal.
Bill with a date span (From and To dates of service) only if the service was provided every consecutive day within the span. The From and To dates must be in the same month.
The Paper Claim Reference Table below lists the required, optional and/or conditional form locators for submitting the paper UB-04 claim form to Health First Colorado for nursing facility services.
| Form Locator and Labels | Completion Format | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Billing Provider Name, Address, Telephone Number | Text | Required
Abbreviate the state using standard post office abbreviations. Enter the telephone number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Pay-to Name, Address, City, State | Text | Required only if different from FL 1.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3a. Patient Control Number | Up to 20 characters: Letters, numbers or hyphens | Optional Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3b. Medical Record Number | 17 digits | Optional Enter the number assigned to the member to assist in retrieval of medical records. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Type of Bill | 3 digits | Required Note: NF/SNF, HBU, QMB Only facilities use: 21x, 22x, 23x Swing Bed facilities use: 28x, 22x, 23x Private ICFs use: 65x, 22x, 23x State ICFs use: 66x, 22x, 23x First two (2) digits, use 21 for SNF Inpatient (IP) includes Medicare A 22* for SNF Inpatient (OP) Medicare B only 23 for SNF Outpatient (OP) 28 for SNF Swing Bed (IP) 65 for ICF Level I (IP) - Privately owned 66 for ICF Level II (IP) - State owned Third digit must be one (1) of the following: Frequency 1 - Admit thru Discharge Claim 2 - Interim - First Claim 3 - Interim - Continuing Claim 4 - Interim - Last Claim 7 - Adjust 8 - Void Revenue Codes 0129 and 0119 should be billed under 21x, 28x, 65x or 66x. *22 should only be used for Medicare Part B claims after Medicare Part A has been exhausted. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Federal Tax Number | None | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Statement covers period From/Through | From: 6 digits MMDDYY Through: 6 digits MMDDYY | Required "From" date is the actual start date of services. "From" date cannot be prior to the start date reported on the initial prior authorization, if applicable, or is the first date of an interim bill. "Through" date is the actual discharge date, or final date of an interim bill. "From" and "Through" dates cannot exceed a calendar month (e.g., bill 01/15/18 thru 01/31/18 and 02/01/18 thru 02/15/18, not 01/15/18 thru 02/15/18). The end date of one (1) eligibility period and the begin date of the following eligibility period cannot be billed on the same claim. If the member is admitted and discharged on the same date, that date appears in both form locators. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8a. Patient Identifier | Text | Required Enter the Health First Colorado ID number for the member. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8b. Patient Name | Up to 25 characters, letters and spaces | Required Enter the member's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Patient Address - Street | Characters Letters and numbers | Required Enter the member's street/post office box as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Patient Address - City | Text | Required Enter the member's city as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Patient Address - State | Text | Required Enter the member's state as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Patient Address - ZIP | Digits | Required Enter the member's zip code as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9e. Patient Address - Country Code | Digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10. Birthdate | 8 digits (MMDDCCYY) | Required Enter the member's birthdate using two (2) digits for the month, two (2) digits for the date, and four (4) digits for the year (MMDDCCYY format). Example: 01012010 for January 1, 2010. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Patient Sex | 1 letter | Required Enter an M (male) or F (female) to indicate the member's sex. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Admission Date | 6 digits | Required Enter the date the member was admitted to the nursing facility using MMDDYY format. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Admission Hour | 6 digits | Optional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Admission Type | 1 digit | Required 1 - Emergency 2 - Urgent 3 - Elective 9 - Information Not Available | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Source of Admission | 1 digit | Required Complete if the member has been admitted or readmitted during the billing period. Use one (1) of the following codes: 1 - Non-Health Care Facility Point of Origin 2 - Clinic or Physician Office 4 - Transfer from a Hospital/Different Facility 5* - Transfer from a SNF/ICF or ACF 6 - Transfer from another Health Care Facility 8 - Court/Law Enforcement 9 - Information Not Available F - Transfer from Hospice or enrolled in Hospice *Use code 5 if the member is a nursing facility resident transfer or is changing from private pay to Health First Colorado pay. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Discharge Hour | 2 digits | Optional Refer to FL 13 for valid codes. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Patient Discharge Status | 2 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18-28. Conditions Codes | 2 digits | Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Accident State | 2 digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31 - 34. Occurrence Code/Date | 2 digits and 6 digits | Conditional
*Other Payer occurrence codes 24 and 25 must be used when applicable. The claim must be submitted with the third-party information. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35-36. Occurrence Span Code From/ Through | Digits | Conditional Complete if nursing facility bills PETI service code(s) on the claim. Enter occurrence span code 76. Enter the "From" and "Through" dates for the PETI services in MMDDYY format. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38. Responsible Party Name/Address | None | Leave blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39 - 41. Value Codes and Amounts | 2 characters and up to 9 digits | Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 42. Revenue Code | 4 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 43. Revenue code Description | Text | Required Enter the revenue code description or abbreviated description. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 44. HCPCS/Rates/ HIPPS Rate Codes | 5 digits | Required Enter the rates (dollar amounts) for the per diem or the PETI/IME. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 45. Service Date | 6 digits | Conditional Enter the first date of service for PETI/IME service code(s). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 46. Service Units | 3 digits | Required Enter the number of covered days. Do not enter fractions or decimals and do not show a decimal point followed by a 0 to designate whole numbers. Enter the number of Non-Medical Leave days. Do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 47. Total Charges | 9 digits | Required Enter the total charge for each revenue code. For Medicare Part B claims, enter the total ancillary charges billed to Medicare. A grand total on line 23 is required for all charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 48. Non-covered Charges | Up to 9 digits | Leave Blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 50. Payer Name | 1 letter and text | Enter the payment source code followed by name of each payer organization from which the provider might expect payment.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 51. Health Plan ID | 8 digits | Required Enter the provider's Health Plan ID for each payer name. Enter the NPI number assigned to the billing provider. Payment is made to the enrolled provider or agency that is assigned this number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 52. Release of Information | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 53. Assignment of Benefits | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 54. Prior Payments | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter third-party and/or Medicare payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 55. Estimated Amount Due | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter the net amount due from Health First Colorado after the provider has received other third party, Medicare or member liability amount. Medicare Crossovers Enter the sum of the Medicare coinsurance plus Medicare deductible less third-party payments and member payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 56. National Provider Identifier (NPI) | 10 digits | Required Enter the billing provider's 10-digit National Provider Identifier (NPI). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 57. Other Provider ID | Optional Enter the eight (8)-digit Health First Colorado provider number assigned to the billing provider. Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 58. Insured's Name | Up to 30 characters | Required Enter the member's name on the Health First Colorado line. Other Insurance/Medicare Complete additional lines when there is third party coverage. Enter the policyholder's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 60. Insured's Unique ID | Up to 20 characters | Required Enter the insured's unique identification number assigned by the payer organization exactly as it appears on the health insurance card. Include letter prefixes or suffixes shown on the card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 61. Insurance Group Name | 14 letters | Conditional Complete when there is third party coverage. Enter the name of the group or plan providing the insurance to the insured exactly as it appears on the health insurance card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 62. Insurance Group Number | 17 digits | Conditional Complete when there is third party coverage. Enter the identification number, control number, or code assigned by the carrier or fund administrator identifying the group under which the individual is carried. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 63. Treatment Authorization Code | Up to 18 characters | Conditional Complete when the service requires a PAR. Enter the authorization number in this FL if a PAR is required and has been approved for services. As of March 1, 2017, PETI/IMEs require a PAR. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 64. Document Control Number | None | Conditional | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 65. Employer Name | Text | Conditional Complete when there is third party coverage. Enter the name of the employer that provides health care coverage for the individual identified in FL 58 (Insured Name). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 66. Diagnosis Version Qualifier | Submitted information is not entered into the claim processing system. Enter applicable ICD indicator to identify which version of ICD codes is being reported. 0ICD-10-CM (DOS 10/1/15 and after) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67. Principal Diagnosis Code | Up to 6 digits | Required Enter the exact ICD-10-CM diagnosis code describing the principal diagnosis that exists at the time of admission or develops subsequently and affects the length of stay. Do not add extra zeros to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67A. - 67Q. - Other Diagnosis | 6 digits | Optional Complete when there are additional conditions that affect treatment. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 69. Admitting Diagnosis Code | 6 digits | Required Enter the ICD-10-CM diagnosis code as stated by the physician at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 70. Patient Reason Diagnosis | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 71. PPS Code | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 72. External Cause of Injury code (E-Code) | 6 digits | Optional Enter the ICD-10-CM diagnosis code for the external cause of an injury, poisoning, or adverse effect. This code must begin with an "E". | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74. Principal Procedure Code/Date | 7 characters and 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74A. Other Procedure Code/Date | 7 characters and 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 76. Attending NPI - Required Attending Last/First Name | NPI - 10 digits Text | Health First Colorado ID Required NPI - Enter the 10-digit NPI number assigned to the physician having primary responsibility for the member's medical care and treatment. This number is obtained from the physician and cannot be a clinic or group number. (If the attending physician is not enrolled in the Health First Colorado or if the member leaves the ER before being seen by a physician, the hospital may enter their individual numbers.) Hospitals and FQHCs may enter the member's regular physician's 10- digit NPI in the Attending Physician ID form locator if the locum tenens physician is not enrolled in the Health First Colorado. QUAL - Enter "1D" for Health First Colorado Enter the attending physician's last and first name. This form locator must be completed for all services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 77. Operating NPI | Optional Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 78 - 79. Other ID NPI - Conditional | NPI - 10 digits | Conditional Complete when attending physician is not the PCP or to identify additional physicians. Ordering, Prescribing, or Referring NPI - when applicable NPI - Enter up to two (2) 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attending physician is not the PCP or if a clinic is a PCP agent, enter the PCP NPI number as the referring physician. The name of the Health First Colorado member's PCP appears on the eligibility verification. Review either for eligibility or PCP. Health First Colorado does not require that the PCP number appear more than once on each claim submitted. The attending physician's last and first name are optional. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 80. Remarks | Text | Enter specific additional information necessary to process the claim or fulfill reporting requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 81. Code - QUAL/CODE/VALUE (a-d) | Qualifier: 2 digits Taxonomy Code: 10 digits | Optional Complete both the qualifier and the taxonomy code for the billing provider in field 81CC-a. Field 81CC-a must be billed with qualifier B3 for the taxonomy code to be captured in the claims processing system. If B3 is missing, no taxonomy code will be captured in the claims processing system. Only one (1) taxonomy code can be captured from field 81CC. If more than one (1) taxonomy code is provided, only the first instance of B3 and taxonomy code will be captured in the claims processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
Nursing Facility Claim Examples
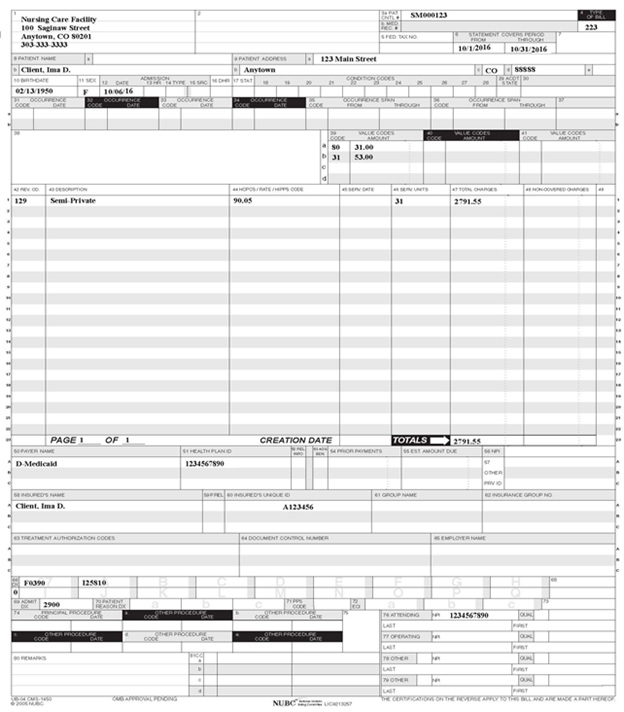
General Nursing Facility Claim Example
TYPE OF BILL: 21X - LTC INPATIENT, Revenue Code 0119 and 0129
Nursing Facility - Medicare Part A Crossover Claim Example
TYPE OF BILL: 21X - LTC INPATIENT. Use Occurrence Code 24 or 25 with date, if applicable.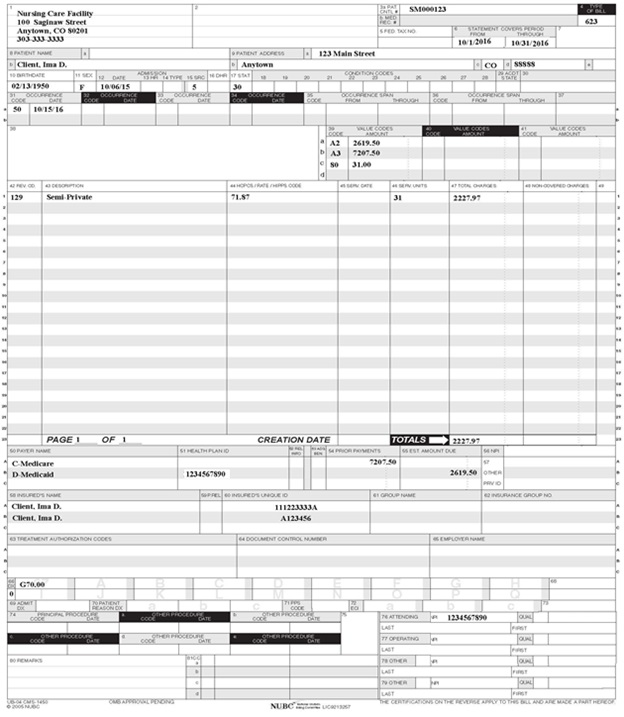
Nursing Facility - Medicare Part B Crossover Claim Example
TYPE OF BILL: 22X - ONLY USE AFTER RESIDENT HAS EXHAUSTED MEDICARE PART A BENEFITS. Use Occurrence Code 24 or 25 with date, if applicable.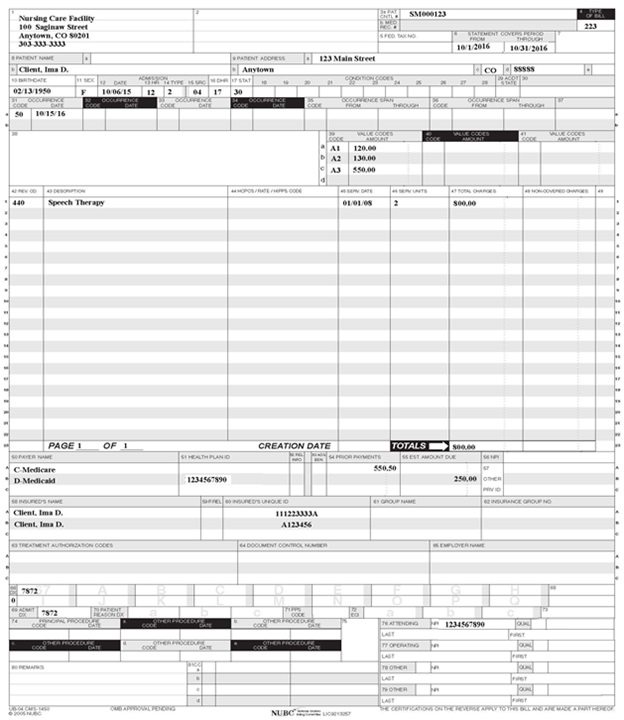
Nursing Facility with PETI Codes and Member Liability Amount Claim Example
TYPE OF BILL: 21X - LTC INPATIENT. Use Occurrence Code 76 and PETI date range.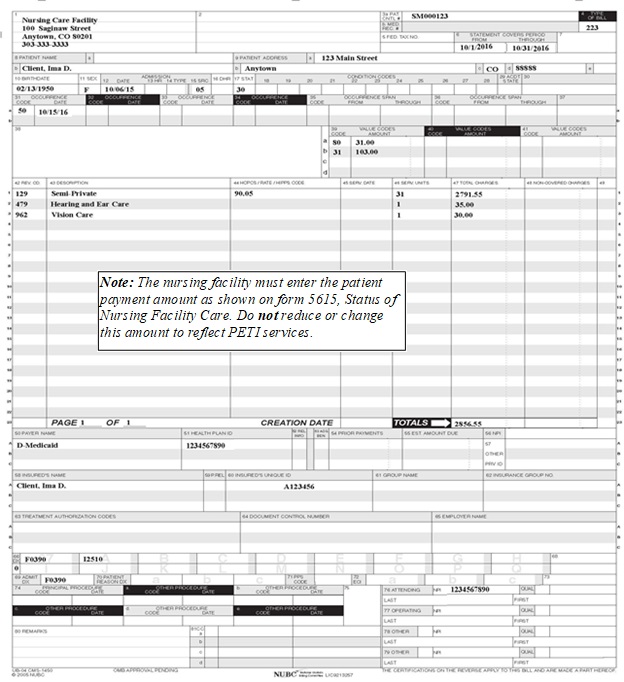
Nursing Facility with Medical Leave Days Claim Example
TYPE OF BILL: 21X - LTC INPATIENT.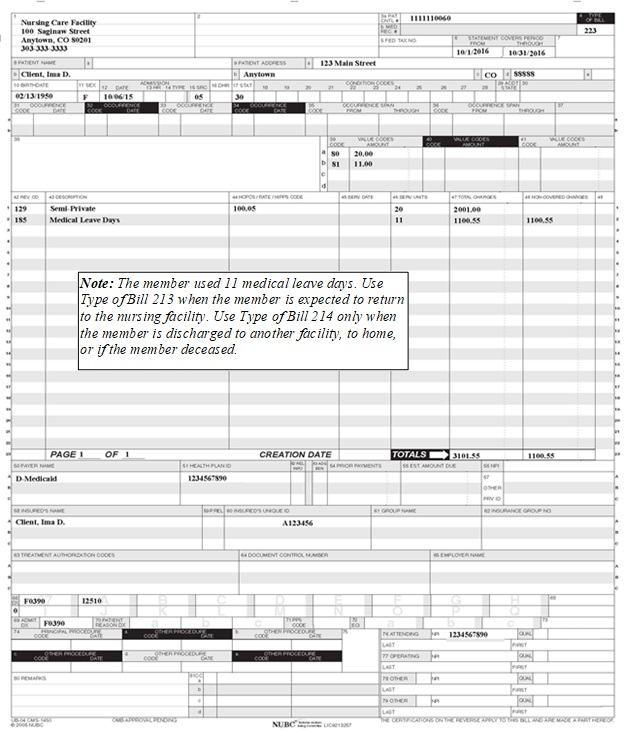
Prior Authorization - PETI/IME
Implemented March 1, 2017
Overview
Post Eligibility Treatment of Income (PETI) is the amount of an individual's income that must be paid to the nursing facility for the cost of care provided to the individual after certain deductions have been applied.
It is federally mandated that this income may be used for an incurred medical expense not covered by Health First Colorado or by any other third-party insurance.
Types of Incurred Medical Expenses (IME) include health insurance premiums, hearing aids, dental and eyeglasses. Check with the Department's Office of Community Living, Nursing Facility Operations Specialist to verify if a service or item is covered by PETI/IME.
Eligibility Criteria
The member must meet the following criteria to receive PETI/IME approval.
- Active Health First Colorado member
- Nursing facility resident
- Monthly member liability payment greater than zero
- Documented medical necessity
- Other potential payer sources exhausted
Reasonable Limits
The State Plan Amendment Supplement 3 to Attachment 2.6-A imposes the following reasonable limits:
- Prior authorization for all expenses. (New Colorado interChange requires all PETI/IMEs to be submitted electronically.)
- Verification of medical necessity required by physician.
- Validation expense is not a benefit of Health First Colorado.
- Allowable cost does not exceed the basic Health First Colorado rate.
- Cost will not be allowed for items for cosmetic reasons only.
- Expenses are not a duplication of expenses previously authorized.
Prior Authorization
Prior authorization by the Department is required for all PETI/IME requests, starting March 1, 2017. The Provider Web Portal is utilized to submit the Nursing Facility (NF) PETI Prior Authorization request.
Refer to the Create Prior Authorization in the Provider Web Portal section below for further details.
Adult Health First Colorado Dental Benefit
Historically, Health First Colorado has not covered dental services for adults and PETI/IME had been utilized by many members in nursing facilities in order to obtain oral health services. Lack of preventive dental coverage can contribute to a range of serious health complications and drives Health First Colorado costs for both emergency services and medical services.
In 2013, the state legislature passed Senate Bill 242. This authorized the Department to create a new limited dental benefit for adults in Health First Colorado. It is provided to all Health First Colorado-enrolled adults age 21 years and over, including members using the PETI/IME program. There is an annual dental benefit up to $1,000 in dental services per member per state fiscal year which runs from July 1 to June 30.
As of July 1, 2014, the following is covered.
The following dental benefits are covered by the State Plan $1,000 annual dental benefit.
- Basic dental preventive exam
- Diagnostic and minor restorative dental services (such as x-rays and minor fillings)
- Root canals
- Crowns
- Partial dentures
- Complete dentures
- Periodontal scaling
- Root planning
Requirements for Adult Dental Benefit
- The dental provider must be enrolled in Health First Colorado. This enables the dental provider to bill Health First Colorado directly for reimbursement of services.
- Once the member's $1,000 benefit has been exhausted, then for those PETI/IME eligible members a PETI/IME request can be submitted to the Department for additional services.
- The $1,000 benefit for each member will also be tracked by the Department's Administrative Service Organization (ASO). The ASO duties will include outreach, recruitment and assisting residents in finding a Health First Colorado provider.
Visit the Provider Rates and Fee Schedule web page and the Provider Forms web page under the Post-Eligibility Treatment of Income Forms (PETI) drop-down menu for PETI/IME documents.
Look on the Department's website under Stakeholder for the Rules, 10 CCR 2505-10, Section 8.482.33.
Facility Requirements
Basics
| Hearing | Vision | Health Insurance | Dental |
| Signed medical necessity form | Signed medical necessity form | Signed medical necessity form | Signed medical necessity form |
| Itemized invoice | Itemized invoice | Verification of premium amount | Itemized invoice |
| Audiogram | Insurance card - front and back | Denial from Health First Colorado - if applicable | |
| Explanation of benefits - if applicable | |||
| A new request is required each calendar year | Documentation if 2nd request |
Activity Log
The nursing facility will document all the member's use of the PETI/IME funds on an annual basis. The log should include the following information as it may be asked for during an audit or review performed by the Department or designee to validate all steps of the PETI/IME process were performed. Log should include the $1,000 Dental benefit and PETI/IMEs.
- Member number and name receiving the service
- Type of service requested
- Date service was requested by the member
- Date PAR was added to Provider Web Portal
- Date PAR was approved by the Department
- Date facility received payment from Health First Colorado for service
- Date service provider was paid by the facility
- Date service was rendered to the member
- Were the member's personal needs account funds used?
- Was the member's personal needs account reimbursed?
- Was the member still at the facility when the service was rendered?
10 CCR 2505-10, Section 8.482.33 states:
- All allowable costs must be documented in the resident's record with date of purchase and receipt of payment, whether or not these costs meet the requirements for prior authorization. Lack of documentation shall cause the cost to be disallowed, causing the nursing facility to be overpaid by the Medicaid program.
Create Prior Authorization in the Provider Web Portal
As of March 1, 2017, all PETI/IME requests must be submitted to the Department via the Provider Web Portal. Once submitted, the Nursing Facility Operations Specialist or designee will approve, approve - with revisions or deny the request. The facility can look up the status of any PETI/IME request on the Provider Web Portal.
Prior Authorization Required Steps
Note: This electronic prior authorization form is used by all HCPF divisions, so it is generic in nature and requirements to complete this form are built into the new Colorado interChange system. The various codes used are based on the NUBC (national) codes. Follow the instructions below to navigate through the various sections of the form.
The form must be completed all at once. There is no saving of partial information.
The Prior Authorization form must be approved by the Department before the PETI/IME can be submitted on a claim for payment.
Refer to the Nursing Facility Post Eligibility Treatment of Income (PETI) Prior Authorization Request (PAR) Submission Quick Guide located on the Quick Guides web page.
Refer to the View Prior Authorizations in the Portal Quick Guide located on the Quick Guides web page to view the PAR status.
PETI/IME Determination
The Department's Nursing Facility Operations Specialist or designee will determine if the PETI/IME request meets the requirements necessary to approve the request. The status will change to approved, approved - with revisions or denied. The Provider Web Portal is instantly updated with the determination and a letter is system generated for mailing the next day.
If PETI/IME request is denied. Submit a whole new request and include all required documents. The denied request can't be re-opened.
Billing Health First Colorado for PETI/IME
Once the PAR status has been changed to approved or approved - with revisions, the facility can bill Health First Colorado for the service or item.
There are seven (7) state-specific revenue codes for PETI/IME that can be billed on nursing facility claims.
Bill the approved PETI/IME on the next billing cycle with a patient liability amount. Do not adjust prior paid claims to add the approved PETI amount.
PETI/IME Revenue Codes
| Revenue Code | Description |
| 0259 | Non-covered Prescription Drugs |
| 0479 | Hearing and Ear Care |
| 0949 | Acupuncture |
| 0962 | Vision and Eye Care |
| 0969 | Dental Services * |
| 0982 | Other Outpatient Services |
| 0999 | Health Insurance Premiums and Other Approved Services |
*Dental Services only applicable after the $1,000 State Benefit has been exhausted or Health First Colorado has denied the service.
To View a PETI/IME Letter
- Select Resources on the blue menu bar on the Provider Web Portal home page.

- Click Report Download.
- Select Colorado interChange - PA Letter.
Nursing Facility Manual Revisions Log
| Revision Date | Changes | Made by |
|---|---|---|
| 12/16/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/16/2016 Please refer to Archive. (Replaced Nursing Facility Billing Manual dated 07/2016.) | HCPF |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | DXC (formerly HPE) |
| 1/10/2017 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_3.xlsx | DXC (formerly HPE) |
| 1/19/2017 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_4.xlsx | DXC (formerly HPE) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | DXC (formerly HPE) |
| 2/2/2017 | Changed Type of Bill to 3 digits. Dropped leading 0. | HCPF |
| 2/23/2017 | Updates based on Provider feedback to Policy SME during February 2017 NFAC meeting. | HCPF |
| 7/31/2017 | Updates based on Department and Provider feedback to Policy SME regarding billing codes. | HCPF |
| 11/1/2017 | Updates based on clarification of Type of Bill coding and Revenue Codes. Updates on PETI/IME process. | HCPF |
| 6/25/2018 | Updated timely filing to point to general manual, other edits | HCPF |
| 6/28/2018 | Removed Fraud, Waste, Abuse heading as there wasn't any verbiage | HCPF |
| 7/10/2018 | Updated Change of Ownership, updated Medicare Crossovers and added Frequency codes. All changes specific to NF. | HCPF |
| 6/13/2019 | Updated Appendices links and verbiage | DXC |
| 12/6/2019 | Updated Medicaid to Health First Colorado, removed images for submitting PETI PAR and replaced with link to portal guide, converted to web page. | HCPF |
| 8/7/2020 | Updated item 81 of the Paper Claim Reference Table for taxonomy code billing | DXC |
| 4/3/2023 | Updated AWS URL Links | HCPF |