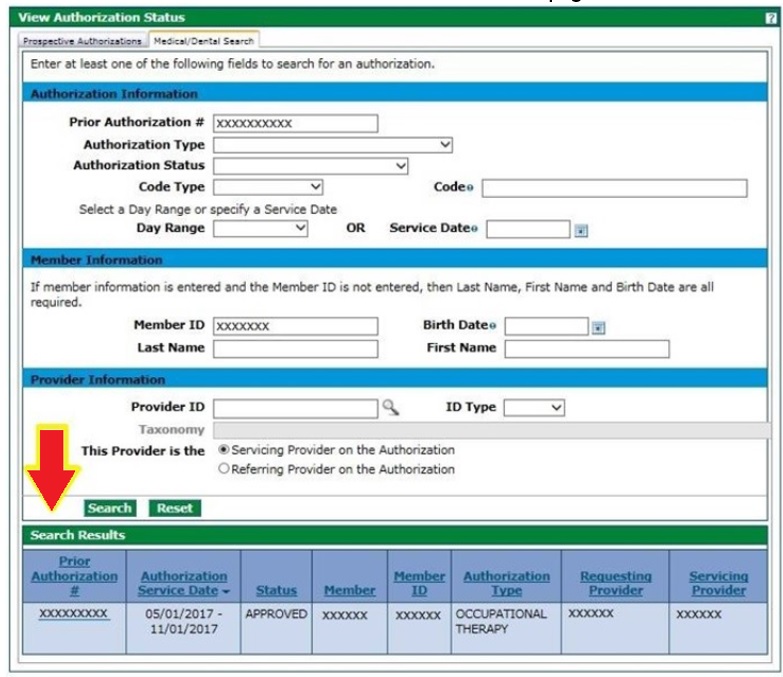
View Prior Authorizations in the Portal
Registered providers and their delegates can view Prior Authorizations (PAs) in the Provider Web Portal even if the provider ID is not listed on the PA. The provider will need to search with the following information:
Prior Authorization Number and Member ID
Or
Prior Authorization Number, Member Last Name and Member First Name
Using any other search criteria will require the provider to be listed as the billing provider or rendering provider on the PA to see the PA on the Provider Web Portal.
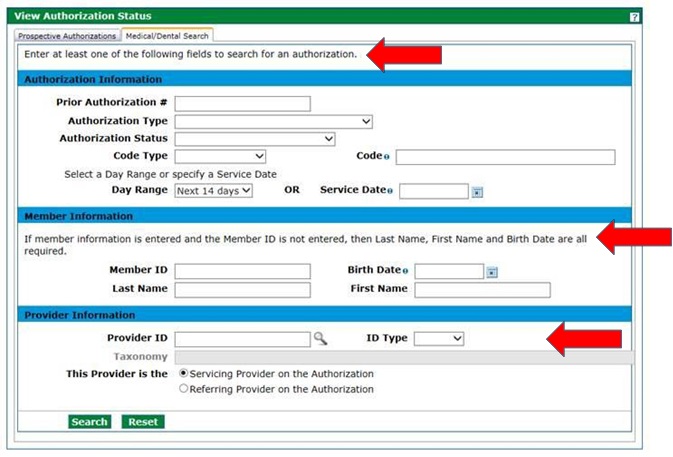
If the provider is listed as the billing or rendering provider on the PA, the Prior Authorization Number is not needed to search. Providers can see all their PAs on the Prospective Authorization tab or they can search for specific PAs on the Medical/Dental tab using any of the following criteria:
At least one (1) field in the Authorization Information section
Or
At least one (1) field in the Provider Information section
Or
Member ID or Last Name, First Name and Birth Date in the Member Information section
NOTE: Prior Authorization Requests (PARs) that are in process in the Bridge cannot be viewed through the Provider Web Portal.
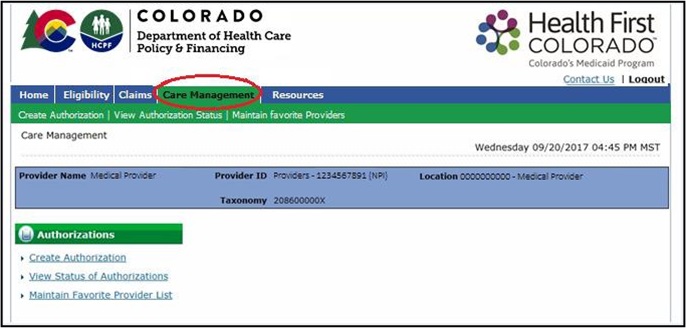
- Select Care Management from the menu.
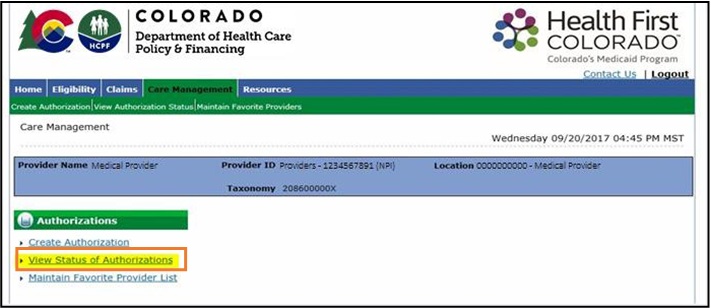
- Select View Status of Authorizations on the Care Management page.
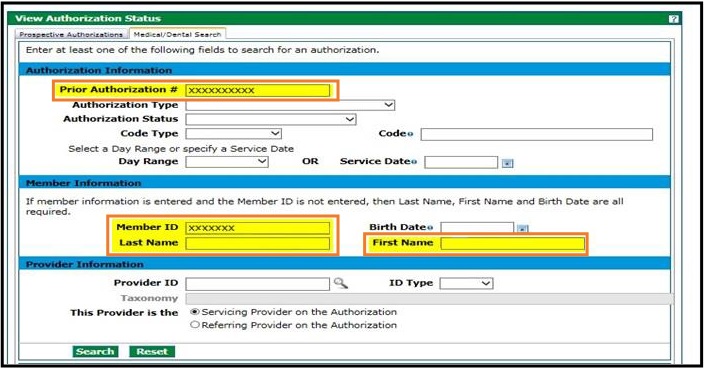
- If the user is not the billing or rendering provider on the PA, enter the Prior Authorization # and Member ID, or the Prior Authorization # and the Member Last Name and First Name.
- If the user is the billing or rendering provider on the PA, enter at least one (1) field in the Authorization Information section, at least one (1) field in the Provider Information section, OR the Member ID or Last Name, First Name and Birth Date in the Member Information section. The Prior Authorization # is not needed.
- Prior Authorization results will show at the bottom of the page.
Need More Help?
Visit the Quick Guides web page to find all the Provider Web Portal Quick Guides.