Medical-Surgical Billing Manual
- Benefits Overview
- General Billing Information
- Anesthesia Services
- Medical Services
- Vaccines/Immunization
- Non-Benefit Medical Services
- Psychiatric Services
- Radiology Services
- Skin Substitutes
- Surgical Services
- General Benefits
- Cosmetic Surgery
- Abortion
- Assistant Surgeon
- Bariatric Surgery
- Breast Reconstruction
- Hysterectomy
- Reconstructive Surgery
- Sterilization
- Transplantation
- Multiple Surgeries
- Bilateral Procedures - Modifier 50
- Two (2) Surgeons - Modifier 62
- Endoscopic Procedures
- Global Surgery
- Unlisted CPT Codes
- Vision Care Services
- CMS Paper Claim Reference Table
- Sterilizations, Hysterectomies and Abortions
- Timely Filing
- Medical-Surgical Services Revisions Log
Return to Billing Manuals Web Page
Benefits Overview
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid program) provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
Health First Colorado reimburses providers for medically necessary medical and surgical services furnished to eligible members.
Providers should refer to the Code of Colorado Regulations, Program Rules (10 CCR 2505-10 8.2.3.D.2), for specific information when providing audiology care.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page for general billing information.
Anesthesia Services
General Benefits
Anesthesia benefits are provided for medical, surgical and radiological procedures. Anesthesia reimbursement is based on actual anesthesia time. Providers should bill the exact number of minutes during which services were provided. One (1) unit of service equals fifteen minutes of anesthesia time. Anesthesia time begins when the anesthetist starts member preparation for induction in the operating room or an equivalent area and ends when the member may be safely placed under post-operative care. No additional benefits are provided for emergency conditions or the member's physical status.
Reimbursement for anesthesia includes all of the following:
|
|
Nerve blocks for anesthetic purposes are processed as general anesthesia. Nerve blocks for diagnostic or therapeutic purposes are processed as surgical procedures.
Anesthesia services rendered by a CRNA who is supervised by an anesthesiologist may be billed by either the CRNA or the supervising anesthesiologist but not both. If the services are billed by both the CRNA and the anesthesiologist, the second claim will be denied as a duplicate.
The following services are considered incidental to the anesthesia service and no separate benefit is allowed:
- Total body hypothermia in combination with or in addition to procedure codes described as "open" or "bypass"
- Endotracheal intubation or extubation
Payment
Anesthesia payment is the lesser of the billed amount and the amount calculated as follows:
(Relative Value + ![]() ) x Allowed Amount
) x Allowed Amount
The Relative Value and Allowed Amount for each anesthesia CPT code are found on the Health First Colorado Physician Fee Schedule.
Anesthesia by Surgeon
Local infiltration, digital block, or topical anesthesia administered by the operating surgeon is included in the surgical reimbursement and no additional benefit is available. IV valium or IV pentothal is a benefit when administered by the surgeon. For obstetrical deliveries, local pudendal and paracervical block anesthesia is included in the obstetrical payment and no additional benefits are allowed for the delivering physician.
Obstetrical Anesthesia
Epidural anesthesia by a provider other than the delivering practitioner is a covered benefit. Member contact time must be documented on the claim. Claims for more than 120 minutes (eight [8] or more time units) of direct member contact epidural time require an attached copy of the anesthesia record.
When CPT codes 01967 and 01968 are performed across two (2) dates of service, both procedures should be reported with a date span that includes both dates of service.
Standby Anesthesia
Standby anesthesia is a benefit in conjunction with obstetrical deliveries, subdural hematomas, femoral or brachial artery embolectomies, members with a physical status of four (4) or five (5), insertion of a cardiac pacemaker, cataract extraction and/or lens implant, percutaneous transluminal angioplasty, and corneal transplant. Unusual circumstances or exceptions to allow a benefit for standby anesthesia for other procedures must be fully documented. Documentation must be submitted with claim.
Family Planning Services
Family planning services including intrauterine devices, implants, diaphragms, and contraceptive drugs are benefits of Health First Colorado.
Foot Care Services
Foot care services are benefits of Health First Colorado whether provided by a physician or licensed podiatrist. Claims for services provided to dually eligible (i.e., Health First Colorado and Medicare-eligible) members are submitted directly to the fiscal agent.
If the billed service is routine foot care and is identified by the Medicare program as non-reimbursable, use the GY modifier to identify routine podiatric foot care services that are not covered by Medicare. The Medicare non-covered services field on the claim record must also be completed.
Medical Services
Consultation
Effective April 1, 2010, CPT consultation codes (ranges 99241-99245 for office/outpatient consultations and 99251-99255 for inpatient consultations) will no longer be recognized for payment. This change was implemented to be consistent with Medicare policy.
Please submit claims for consultation services using another Evaluation and Management (E/M) code that most appropriately represents where the visit occurred and that identifies the complexity of the visit performed.
Annual Physical
Adults may receive one (1) physical examination per year. Sports physicals are not covered.
Vaccines/Immunizations
Refer to the Immunization Benefits Billing Manual located on the Billing Manuals web page.
Medical Care and Surgery on the Same Day
Both medical care and surgery are allowed when performed on the same day by the physician when the surgical procedure is minor in nature. Follow-up care requirements are determined by the Department of Health Care Policy & Financing (the Department) and are related to those assigned by Medicare and other sources.
New Member Services
New member medical care visits are limited to one (1) per member per provider. A medical records administrative fee is included in Health First Colorado reimbursement.
Nursing Facility Visits
Nursing facility visits are limited to one (1) visit per day per member by the same provider for the same diagnosis or condition.
Office Visits
Office visits are limited to one (1) visit per day per member by the same provider for the same diagnosis or condition.
Supplies Provided by a Physician
Providers may bill for non-routine supplies following the instructions in the current CMS bulletin for practitioners.
Billable non-routine supplies are listed in the CMS publication under separate categories. Providers should always refer to the most current publications when billing Health First Colorado as some supplies are considered inclusive in the medical or surgical service.
Non-Benefit Medical Services
Services for which Health First Colorado assistance is not available include, but are not limited to:
|
|
Psychiatric Services
General Benefits
Psychiatric services refer to services described in CPT under the heading "Psychiatry". Health First Colorado benefits are available for face-to-face member contact services only. Benefits are not available for report preparation, telephone consultation, case presentations, or staff consultation.
Non-Benefit Psychiatric Services
Psychotherapy services provided for the following specific primary diagnoses are not benefits of Health First Colorado.
| F03.90 | Unspecified dementia without behavioral disturbance |
| F05 | Delirium due to known physiological condition |
| 290.4 | Vascular dementia |
| F01.50 | Vascular dementia without behavioral disturbance |
| F01.51 | Vascular dementia with behavioral disturbance |
| 310 | Specific nonpsychotic mental disorders due to brain damage |
| F07.0 | Personality change due to known physiological condition |
| F07.81 | Postconcussional syndrome |
| F48.2 | Pseudobulbar affect |
| 310.8 | Other specified nonpsychotic mental disorders following organic brain damage |
| F07.89 | Other personality and behavioral disorders due to known physiological condition |
| F07.9 | Unspecified personality and behavioral disorder due to known physiological condition |
| F09 | Unspecified mental disorder due to known physiological condition |
| F70 | Mild intellectual disabilities |
| 318 | Other specified mental retardation |
| F71 | Moderate intellectual disabilities |
| F72 | Severe intellectual disabilities |
| F73 | Profound intellectual disabilities |
| F78 | Other intellectual disabilities |
| F79 | Unspecified intellectual disabilities |
| R41.81 | Age-related cognitive decline |
| R54 | Age-related physical debility |
The following psychiatric services are not benefits:
|
|
Unusual circumstances or exceptions to allow benefits for these services must be fully documented, reviewed and prior authorized.
Regional Accountable Entities (RAEs)
Regional Accountable Entities (RAEs) provide all mental health care to members in their geographical area. Non-network practitioners who render emergency mental health services must bill the RAE for payment. The RAE will not pay for non-emergency services provided without RAE prior authorization.
Members who are dually eligible (i.e., Health First Colorado and Medicare-eligible) may obtain services through the RAE or from a non-RAE provider, and the fiscal agent will process submitted Medicare crossover claims. If the mental health service is covered by Health First Colorado only, the member must obtain services from the RAE.
Radiology Services
Refer to the Outpatient Imaging and Radiology Billing Manual located on the Billing Manuals web page.
Skin Substitutes
As of September 1, 2019, skin substitute products are categorized and reimbursed based on their composition. The categories for reimbursement include:
- Allogenic Acellular (product is derived from human cells and does not contain living cells)
- Allogenic Cellular (product is derived from human cells and contains whole and/or living cells)
- Xenogenic (product is derived from a non-human species)
- Injections
Skin substitute products are reimbursed at the same rate as all other products in the same category. The reimbursement rate for each category is based on the average price of the products within that category.
Covered skin substitute products and corresponding rates can be found on the Provider Rates and Fee Schedule web page under the Health First Colorado Fee Schedule drop-down section.
Effective March 1, 2026, providers must only bill for units administered. Discarded units should not be reported on the claim.
Surgical Services
General Benefits
Surgical reimbursement includes payment for the operation, local infiltration, digital block or topical anesthesia when used, and normal, uncomplicated follow-up care. Under most circumstances, the immediate preoperative visit necessary to examine the member is included in the surgical procedure whether provided in the hospital or elsewhere.
Cosmetic Surgery
Procedures intended solely to improve the physical appearance of an individual, but which do not restore bodily function or correct deformity are not benefits of Health First Colorado.
Abortion
Therapeutic legally induced abortions are benefits of Health First Colorado when performed to save the life of the mother. Health First Colorado also reimburses legally induced abortions for pregnancies that are the result of sexual assault (rape) or incest. Refer to the Sterilizations, Hysterectomies and Abortions Billing Instructions section for specific instructions on submitting claims for abortions performed for maternal life-endangering circumstances, sexual assault or incest.
Assistant Surgeon
Assistant surgeon services may be reported by adding the appropriate modifier code 80, 81 or 82 to the surgical procedure code. The only procedures allowable for assistant surgery benefits are procedures listed on the Medicare Physician Fee Schedule Database (MPFSDB) with an assistant surgery indicator of 2.
Payment allowed is up to 20% of the surgeon's maximum allowable reimbursement for the first procedure and 5 percent of the surgeon's maximum allowable reimbursement for second and subsequent procedures. If multiple surgery pricing also applies to services reported with modifier 80, 81 or 82, the assistant surgery pricing will be applied after the multiple surgery discount.
Services rendered by non-physician practitioners should be reported using modifier-AS in addition to 80, 81 or 82.
Surgeries performed by the same rendering provider for the same member on the same date of service must be submitted on a single claim. Each rendering provider's procedures should be submitted on a separate claim, even if the claims are submitted by the same billing provider.
Metabolic and Bariatric Surgery
Health First Colorado covers metabolic and bariatric surgery for members age thirteen years and older when members have clinical obesity and the service is medically necessary. One metabolic and bariatric surgery is covered per member lifetime unless a revision is appropriate based on an identified complication.
Covered primary procedures are indicated by the Health First Colorado Fee Schedule and include:
- Roux-en-Y Gastric Bypass
- Biliopancreatic Diversion with or without Duodenal Switch
- Vertical Sleeve Gastroplasty
Surgeons must be trained and credentialed in metabolic and bariatric surgery procedures and surgeries may only be performed in a hospital.
Criteria for a primary procedure:
BMI
To qualify for metabolic and bariatric surgery members must have either Class III Obesity, or Class II Obesity and documentation of one or more of the following comorbidities:
- Severe cardiac disease
- Type 2 diabetes mellitus
- Obstructive sleep apnea or another respiratory disease
- Pseudo-tumor cerebri
- Hypertension
- Hyperlipidemia
- Severe joint or disc disease that interferes with daily functioning
- Intertriginous soft-tissue infections, nonalcoholic steatohepatitis, stress urinary incontinence, recurrent or persistent venous stasis disease, or significant impairment in activities of daily living
For members eighteen years of age and older:
- Class II Obesity = BMI between 35-39.9
- Class III Obesity = BMI of 40 or higher
For members under the age of eighteen:
- Class II Obesity = BMI greater than 120% of the 95th percentile for age and sex
- Class III Obesity = BMI greater than 140% of the 95th percentile for age and sex
Contraindications
Contraindications are determined based on nationally recognized standards of care.
Contraindications must be ruled out through a complete history and physical and a psychiatric/psychological assessment that has been conducted within the past 12 months prior to the requested prior authorization.
Additional Criteria
Members must have attempted nonsurgical weight loss and weight management without sufficient clinical improvement.
Members must also receive nutritional counseling comprised of at least three visits with a provider with documented expertise in nutrition. The counseling must be individualized for the member’s health related social needs. It can be provided in person or via telemedicine and must include the following:
- Identification of maladaptive eating behaviors and patterns and recommendations for addressing them
- Nutritional and dietary education for postoperative success
- Education on modifying the member’s modifiable risk factors and correcting micronutrient deficiencies
The member’s multidisciplinary team must document that the member understands and is willing to comply with a long-term postoperative care plan created by the team.
Revision Procedures
Revision procedures are covered when medically necessary to correct complications such as slippage of an adjustable gastric band, intestinal obstruction, or stricture following a primary procedure.
Indications for surgical revision include:
- Weight loss to 20% below the ideal body weight
- Esophagitis, unresponsive to nonsurgical treatment
- Hemorrhage or hematoma complicating a procedure
- Excessive bilious vomiting following gastrointestinal surgery
- Complications of the intestinal anastomosis and bypass
- Stomal dilation, documented by endoscopy
- Documented slippage of the adjustable gastric band
- Pouch dilation documented by upper gastrointestinal examination or endoscopy producing weight gain of 20% or more, provided that
- The primary procedure was successful in inducing weight loss prior to the pouch dilation and
- The member has been compliant with a prescribed nutrition and exercise program following the procedure
- Other and unspecified post-surgical non absorption complications
Prior Authorization Requirements
All metabolic and bariatric surgery procedures require prior authorization. Requests for prior authorization must include the following:
- The member’s height, weight, and BMI
- A list of each comorbid condition, with attention to any contraindications which might affect the surgery including all objective measurements
- A detailed account of the member’s nonsurgical weight loss and weight management attempt(s)
- A detailed account of nutritional counseling
- A current psychiatric or psychological assessment regarding contraindications for metabolic and bariatric surgery
- A description of the post-surgical follow-up program
Providers should refer to the Code of Colorado Regulations, Program Rules (10 CCR 2505-10 8.300.3.C), for additional information when providing this service.
Breast Reconstruction
Breast reconstruction is a benefit when:
- Members meet requirements described in the Breast and Cervical Cancer Program;
- Members meet requirements described in the Gender-Affirming Care Billing Manual;
- Performed within five (5) years of a mastectomy; or
- Procedure otherwise meets the definition of medical necessity in Dept. rule at 10 CCR 2505-10 8.076.1.8.
Removal and replacement of breast implants is considered medically necessary when:
- The implant is affected by surgical complications such as recurrent infections
- An implant has ruptured, and the member is experiencing side-effects related to the rupture, such as but not limited to persistent pain
- Including when implants were originally placed for cosmetic reasons
- The implant was originally placed for reconstructive reasons and 10 years or longer has elapsed since original placement
- Procedure otherwise meets the definition of medical necessity in Department rule at 10 CCR 2505-10 8.076.1.8
When replacement of one (1) breast implant is considered medically necessary, replacement of the contralateral implant is also deemed medically necessary when performed at the same time.
All breast reconstruction and revision procedures require prior authorization.
Hysterectomy
A hysterectomy is a benefit of Health First Colorado when performed solely for medical reasons. A hysterectomy is not a benefit when:
- The procedure is performed solely for the purpose of sterilization.
- There is more than one (1) purpose for the procedure, and it would not have been performed except for the purpose of sterilization.
Refer to the Sterilizations, Hysterectomies and Abortions Billing Instructions section for billing requirements.
Reconstructive Surgery
Surgical procedures intended to improve the function and appearance of any body area altered by disease, trauma, congenital or developmental anomalies, or previous surgical processes may be benefits of the program if services are prior authorized. Physician documentation on the PAR form is the basis for determining the benefit for reconstructive surgery.
Sterilization
Voluntary sterilization is a benefit when appropriately documented on the Consent to Sterilization - MED 178 Form. Refer to the Sterilizations, Hysterectomies and Abortions Billing Instructions section for sterilization billing requirements.
Transplantation
Organ procurement and transplantation are benefits only when prior authorized. Corneal and kidney transplants are benefits and do not require prior authorization.
Donor expenses (i.e., organ procurement associated surgical and laboratory costs) for living organ donations are covered for kidney and liver transplants. Living organ donations for liver transplants require the transplant recipient to have received prior authorization for a living organ transplant procedure.
Reimbursement is only allowed for the approved donor. Expenses for donors who are tested and not approved are not covered.
Donor expenses should be billed on the recipient's transplant claim using the recipient's Health First Colorado identification number.
Important: Organ transplants are not a covered benefit for non-citizens.
Multiple Surgeries
Health First Colorado utilizes the general surgical guidelines, subsection instructions, and procedure code modifiers found in each year's CPT codebook published by the AMA. The following information is in addition to the CPT guidelines, and should be utilized for billing Health First Colorado and reimbursement purposes.
The Medicare Physician Fee Schedule Data Base (MPFSDB) designates some procedure codes as subject to multiple surgery criteria. When two (2) or more procedures subject to multiple surgery pricing are reported on a claim, the surgery procedure commanding the greatest allowable payment will be reimbursed at 100 percent of the allowed amount, the surgery procedure with the second greatest allowable payment at 50 percent and subsequent surgery procedures at 25 percent.
Services must be billed on the same claim to receive payment for multiple surgical services rendered on the same date of service, for the same member, by the same rendering provider. If a separate claim is billed for the same rendering provider, the subsequent claim will deny. If multiple surgeons provide services to a member on the same date of service, report each rendering provider's procedures on a separate claim.
Bilateral Procedures - Modifier 50
Unless otherwise identified in the CPT-4 listings, bilateral procedures requiring a separate incision that are performed at the same operative session, should be identified by the appropriate five (5)-digit code describing the procedure with modifier 50 added to the procedure code. Use of this modifier should be limited to procedures for which "bilateral" services are appropriate according to the MPFSDB. See the Unlisted section for information on reporting unlisted procedures performed bilaterally.
Bilateral procedures indicated using modifier 50 will be reimbursed at 180 percent of the maximum allowable for the procedure. If multiple surgery pricing also applies to services reported with modifier 50, the multiple surgery discount will be applied after the bilateral pricing.
Two (2) Surgeons - Modifier 62
When two (2) surgeons work together as primary surgeons performing distinct part(s) of a procedure, each surgeon should report his/her distinct operative work by adding modifier 62 to the procedure code and any associated add-on code(s) for that procedure as long as both surgeons continue to work together as primary surgeons. Each surgeon should report the co-surgery once using the same procedure code. If additional procedure(s) including add-on procedure(s) are performed during the same surgical session, separate code(s) may also be reported with modifier 62 added.
Note: If a co-surgeon acts as an assistant in the performance of additional procedure(s) during the same surgical session, those services may be reported using separate procedure code(s) with modifier 80 or modifier 82 added, as appropriate.
The only procedures allowable for co-surgeon reimbursement are listed on the Medicare Physician Fee Schedule Database with a co-surgery indicator of 2.
Report each rendering provider's procedures on a separate claim, even if the claims are submitted by the same billing provider. Procedures reported with modifier 62 will be priced at 62.5% of the maximum allowed amount. Multiple surgery discounting will be applied to eligible procedures after the 62.5% adjustment.
For surgeries requiring prior authorization, prior authorization requests must include sufficient units for each surgeon. For example, if a procedure will be reported by two (2) surgeons, each with one (1) unit, two (2) total units must be prior authorized. One (1) provider may request prior authorization on behalf of both surgeons.
Endoscopic Procedures
Certain procedure codes are designated as endoscopic and placed into families according to the MPFSDB. A reimbursement reduction is applied to multiple endoscopic procedures within the same family performed by the same physician on the same member on the same day. When a claim contains multiple endoscopy procedures within the same family, the procedure with the highest allowable payment will be reimbursed at 100 percent of that amount, the procedure with the next highest allowable payment will be reimbursed at 80 percent, and subsequent procedures will be reimbursed at 50 percent. Reimbursement for endoscopic procedures within the same family is calculated independently of discounts that might apply to other lines on the claim, including other families of endoscopic procedures, or multiple surgeries.
Global Surgery
Payment for a surgical procedure includes the pre-operative, intra-operative, and post-operative services routinely performed by the surgeon. The post-operative period for each surgical procedure code is determined by the value given in the MPFSDB, and is either 0, 10, or 90 days. Evaluation and management services rendered by the surgeon during this period that are related to recovery from the surgery are included in the payment for the surgery, and not separately reimbursable. This includes any services required of the surgeon during the post-operative period because of complications which do not require additional trips to the operating room.
Services that are considered related to the surgery include but are not limited to:
- For dates of service before 5/1/2022: The two (2) procedures are considered to be related E/M services when the first three (3) digits of the diagnoses associated with the E/Mare the same match the first three (3) digits of the diagnoses associated with the surgery.
- For dates of service 5/1/2022 and after: E/M services when the diagnoses associated with the E/M match exactly any of the diagnoses associated with the surgery.
Modifiers for reporting separately identifiable services during the postoperative period are described at the end of this manual.
The Department will only recognize modifiers 54 and 55 when appended to CPT codes 66821, 66982, 66984 from dates of service June 1, 2022, forward. Providers may use modifier 54 to report performance of surgical care only and modifier 55 to report postoperative management only. The global rate will be split between the two (2) providers. Modifier-specific rates can be found on the Health First Colorado Fee Schedule.
Unlisted CPT Codes
Unlisted surgery CPT codes are used when there is no CPT or HCPCS code that accurately identifies the services performed. Unlisted surgery codes with dates of service on or after November 1, 2018, will be manually priced by a clinical reviewer with the Department's fiscal agent.
Covered unlisted surgery codes can be found on the Health First Colorado Fee Schedule.
Claims with unlisted codes must include as attachments the operating report from the procedure and the Unlisted Procedure Code Form located on the Provider Forms web page under Claim Forms and Attachments. All lines on the Unlisted Procedure Code Form must be completed. The Department will deny claims lacking the required attachments. Claims denied for incomplete information will have to be resubmitted with the correct information for reimbursement.
When unlisted codes are used to report bilateral surgery, the Unlisted Procedure Code Form should list the total time for both sides of the procedure. The standard bilateral modifier (modifier 50) should not be used.
Vision Care Services
Refer to the Vision Care and Eyewear Manual located on the Billing Manuals web page.
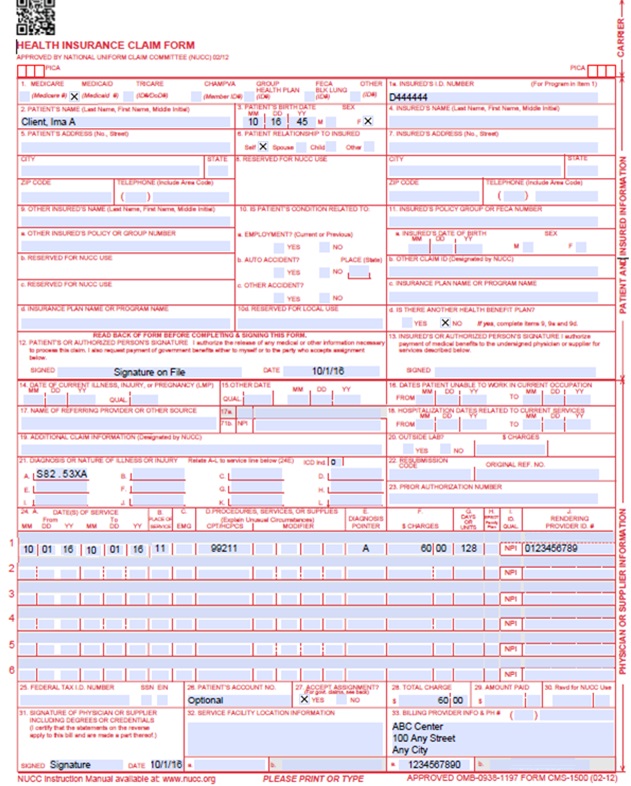
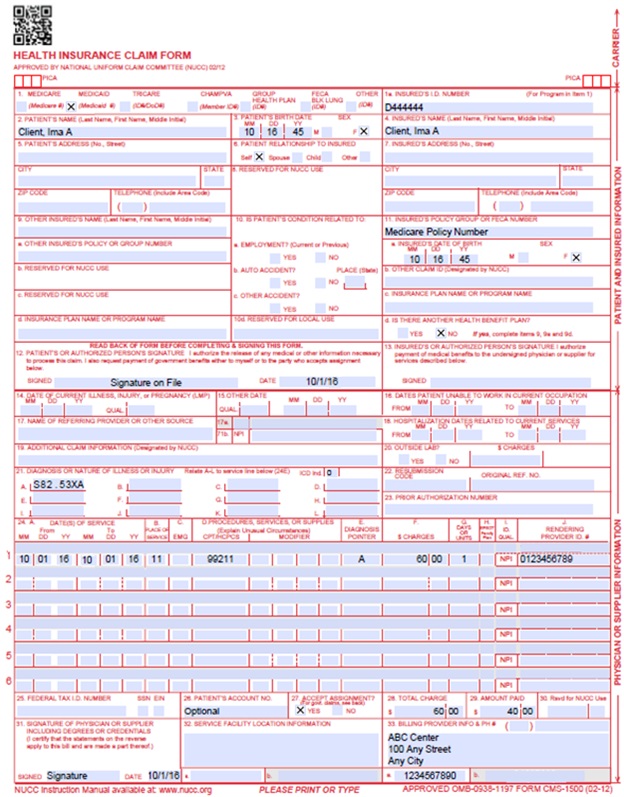
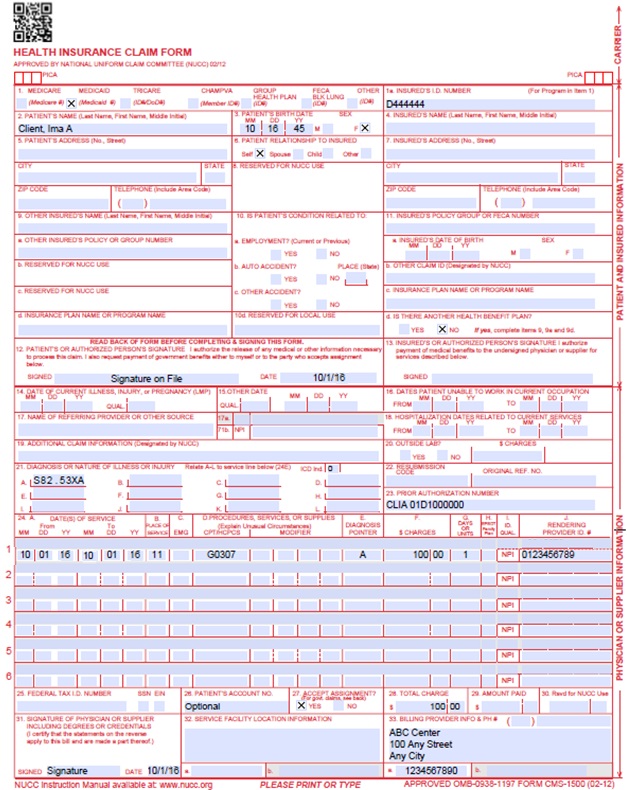
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven (7)-digit ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left-hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | CLIA When applicable, enter the word "CLIA" followed by the number. Prior Authorization Enter the six (6)-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||||||||||||||
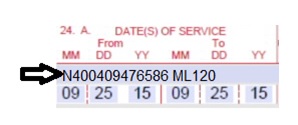
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
VP - Vendor Product Number OZ - Product Number CTR - Contract Rate JP - Universal/National Tooth Designation JO - Dentistry Designation System for Tooth and Areas of Oral Cavity | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form.
| ||||||||||||||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | General Instructions | A unit represents the number of times the described procedure or service was rendered. Except as instructed in this manual or in Health First Colorado bulletins, the billed unit must correspond to procedure code descriptions. The following examples show the relationship between the procedure description and the entry of units. | ||||||||||||||||||||||||||||||||||||||||||||||||
Anesthesia Services
| ||||||||||||||||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area)
Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||||||||||||||
CMS 1500 Medical Claim Example
CMS 1500 Medical Crossover Claim Example
CMS 1500 Medical Claim with CLIA Number Example
Sterilizations, Hysterectomies and Abortions
Refer to the Obstetrical Care Billing Manual located on the Billing Manuals web page for more information on Sterilization, Hysterectomies and Abortions.
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page for more information on timely filing policy, including the resubmission rules for denied claims.
Medical-Surgical Services Revisions Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016 Please refer to Archive. | HPE (now DXC) |
| 2/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_4xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 8/31/2017 | Updates based on DXC Management comments. | DXC |
| 1/2/2018 | Supplemental Qualifier addition - instructions for reporting an NDC | DXC |
| 5/3/2018 | Updated Anesthesia payment policy and billing instructions | HCPF |
| 6/26/2018 | Removed entire Laboratory section, updated timely | HCPF |
| 11/20/2018 | Clarified Multiple Surgery, added Endoscopic and Unlisted sections | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 2/6/2019 | Updated billing instructions for multiple surgery, bilateral, assistant surgeon, and two surgeon sections | HCPF |
| 3/18/2019 | Clarification to signature requirement | HCPF |
| 7/11/2019 | Updated Appendices' links and verbiage | DXC |
| 10/16/2019 | Added modifier 25 and 57 descriptions, removed vaccine, vision, and radiology sections | HCPF |
| 12/16/2019 | Converted to web page | HCPF |
| 2/11/2020 | Added global surgery section, updated assistant surgeon, two surgeons, and unlisted sections | HCPF |
| 9/10/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 2/2/2021 | Updated transplant section | HCPF |
| 4/2/201 | Updated obstetrical anesthesia section | HCPF |
| 5/3/2021 | Updated assistant surgery section | HCPF |
| 11/10/2021 | Added Bariatric Surgery section | HCPF |
| 4/6/2022 | Updated diagnosis criteria in global surgery section, clarified allowable procedures for assistant and co-surgery | HCPF |
| 5/9/2022 | Updated instructions on use of modifiers 54 and 55 | HCPF |
| 7/1/2022 | Added link to Forms page for Unlisted Code form | HCPF |
| 8/29/2022 | Updated global surgery section, added FT modifier | HCPF |
| 12/19/2022 | Updated Unlisted CPT Codes section | HCPF |
| 4/6/2023 | Added Breast Reconstruction section | HCPF |
| 10/12/2023 | Clarified PAR units required for co-surgery | HCPF |
| 5/15/2024 | Added skin substitute section | HCPF |
| 11/14/2024 | Clarified anesthesia billing requirements | HCPF |
| 08/08/2025 | Clarified bilateral requirement for unlisted codes | HCPF |
| 09/30/2025 | Updated metabolic and bariatric surgery section | HCPF |
| 12/12/2025 | Clarified anesthesia supervision policy | HCPF |
| 01/30/2026 | Updated Skin Substitute section with unit discard information. | HCPF |