Vision Care and Eyewear Billing Manual
- Benefits
- Services Delivered to Children in a School Setting
- Post Eligibility Treatment of Income (PETI)
- Ordering, Prescribing, and Referring Claim Requirements
- Aspheric Lenses- Medical Necessity Requirements
- General Billing Information
- Temporary Service Sites and Mobile Units
- Prior Authorization Requests (PARs) for Vision Services
- CMS 1500 Paper claim Reference Table
- Procedure/HCPCS Codes Overview
- Timely Filing
- Vision and Eyewear Revisions Log
Return to Billing Manuals Web Page
Benefits
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid program) provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to the Health First Colorado
Health First Colorado reimburses providers for medically necessary medical and surgical services furnished to eligible members.
Providers should refer to the Code of Colorado Regulations, Program Rules (10 CCR 2505-10), for specific information when providing medical/surgical services.
Members Ages 21 and Older
- Annual eye examinations and medically necessary follow-up appointments are a benefit.
- Eyeglasses and contact lenses are benefits following eye surgery only. The surgery may have been performed at any time during the member's life. The modifier -55 must be used with eyewear codes to identify surgery-related eyewear (one [1] unit per lens).
- Eyeglasses, following eye surgery, include one (1) or two (2) single or multifocal vision clear plastic or polycarbonate lenses with one (1) frame. Health First Colorado provides payment for one (1) frame.
- Adult members who have undergone eye surgery are eligible for new eyeglasses once every 24 months.
- Contact lenses are only covered if glasses cannot achieve correction.
- Glasses dispensed by an optician are a benefit when ordered by a physician, ophthalmologist or optometrist.
- Eyeglasses or contacts must have a valid prescription from a qualifying provider.
- Ocular prosthetics.
- Providers must maintain prescriptions and other client records in accordance with 10 CCR 2505-10 8.130.2 Maintenance of Records.
Members Ages 20 and Younger
The Early Periodic Screening Diagnosis and Treatment (EPSDT) Program provides the following vision benefits for members ages 20 and under:
- Annual eye examinations and medically necessary follow-up appointments are a benefit.
- Eyeglasses (one [1] or two [2] single or multifocal vision clear plastic or polycarbonate lenses with one [1] frame). Health First Colorado provides payment for one (1) frame.
- Glasses dispensed by an optician are a benefit when ordered by a physician, ophthalmologist or optometrist.
- Replacement or repair of frames or lenses, not to exceed the cost of replacement.
- Contact lenses must be medically necessary. Contact lenses are only covered if glasses cannot achieve correction. Contact lens supplies and contact lens insurance are not benefits.
- Eyeglasses or contacts must have a valid prescription from a qualifying provider.
- Orthoptic and Pleoptic Vision Therapy.
- Ocular prosthetics.
- There is no yearly maximum for eye exams or eyeglasses.
- Providers must maintain prescriptions and other client records in accordance with 10 CCR 2505-10 8.130.2 Maintenance of Records.
Services Delivered to Children in a School Setting
Effective May 3, 2024, place of service 03 is an allowed place of service for all fee-for-service benefits. In order for community providers to bill fee-for-service to children in a school setting, the provider must follow school district policy. Please reference the Community Providers in a School Setting Policy memo.
Post Eligibility Treatment of Income (PETI)
Post Eligibility Treatment of Income (PETI) is the amount of an individual’s income that is paid to the nursing facility for the cost of care provided. Mandated by the federal government, this income is used for incurred medical expenses not covered by Health First Colorado or third-party insurance. These types of incurred medical expenses include health insurance premiums, hearing, acupuncture, dental, and vision services. PETI coverage and billing requirements for vision services may differ from the benefits and billing requirements included in this manual. PETI-specific regulations can be found in the Code of Colorado Regulations.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Ordering, Prescribing, and Referring Claim Requirements
Effective July 1, 2022, the Department of Health Care Policy & Financing (the Department) started soft enforcement of the federal requirement 42 CFR § 455.440 that claims for certain types of services contain the National Provider Identifier (NPI) of the provider who ordered the service, and that the NPI is actively enrolled with Health First Colorado.
All claims for Vision Care and Eyewear services must have the NPI number of the provider who ordered the items to be indicated on the claim. In the Provider Web Portal, this field is labeled "Referring Provider".
The provider types that may order these services are: physician (05, 65), optometrist, (07), and osteopath (26).
The following providers are eligible to render vision services when enrolled with Colorado Medicaid and licensed by the Colorado Department of Regulatory Agencies, or the licensing agency of the state in which they do business: optometrists (07), physicians (05, 65), and opticians. Services rendered by an optician should be billed with the NPI of the managing provider.
If a physician, optometrist or osteopath renders a service under their own ordering authority, that rendering physician’s NPI number should be placed in the applicable OPR field on the claim.
Providers are required to enter the NPI of the ordering provider into the following locations for claim submission. In the Provider Web Portal, this field may be labeled as "Referring Provider."
Professional claims
- Paper claims use field 17.b
- Electronic submissions use loop 2420 with qualifier DK (Ordering), DN (Referring), or DQ (Supervising)
Institutional claims
- The Attending Provider field (#76) or the Other ID fields (#78 or #79) for both paper and electronic claims
Providers should refer to their applicable UB-04 billing manuals for guidance on how each field is used.
Contact the Provider Services Call Center for assistance with claim submission.
Aspheric Lenses- Medical Necessity Requirements
All services rendered to Health First Colorado members must meet medical necessity requirements defined at 10 CCR 2505-10 8.076.1.8.
Aspheric single vision and multifocal lenses are only covered when medically necessary and when the spherical equivalent of the prescription is equal to or greater than +/- 6.0 diopters.
Back to Top
Temporary Service Sites and Mobile Units
Mobile units and temporary service sites are not required to be separately enrolled with Health First Colorado. Temporary sites and mobile units can bill from the location where the staff or unit is based.
Per C.R.S. 25.5-4-420, which can be found on the Colorado Revised Statues web page on the Colorado General Assembly website, service sites that become permanent locations are required to obtain and use a unique National Provider Identifier (NPI) for each service location and to enroll with Health First Colorado.
Services provided in a temporary location do not require enrollment of the temporary location.
Prior Authorization Requests (PARs) for Vision Services
Prior authorization is not required for vision services.
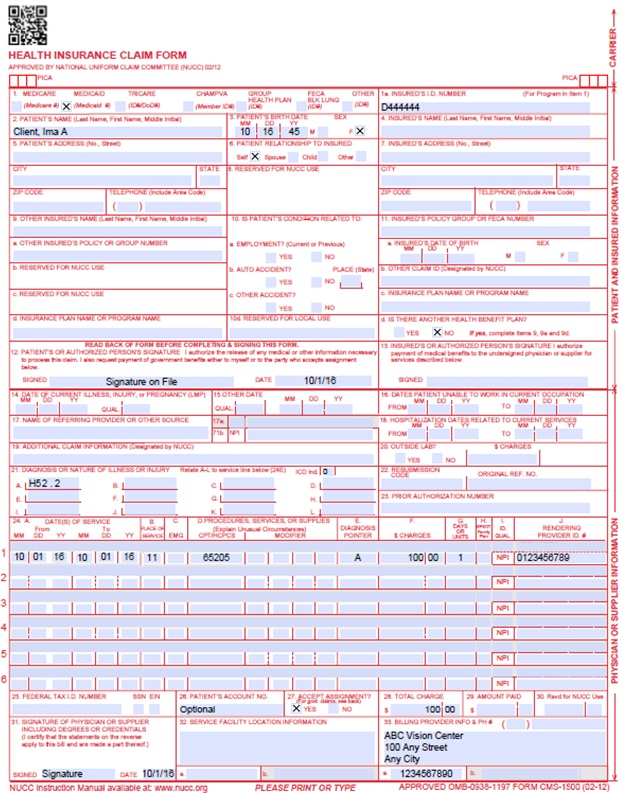
CMS 1500 Paper Claim Reference Table
The following paper form reference table describes required fields for the paper CMS 1500 claim form for Early Intervention claims:
| CMS Field Number & Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11d is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070118 for July 1, 2018. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Other Date | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070118 for July 1, 2018. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | Enter the six (6)-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010124 for January 1, 2024.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. The Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one (1) that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. 24 Unrelated Evaluation/Management (E/M) service by the same physician during a postoperative period Use with E/M codes to report unrelated services by the same physician during the postoperative period. Claim diagnosis code(s) must identify a condition unrelated to the surgical procedure. 26 Professional component Use with diagnostic codes to report professional component services (reading and interpretation) billed separately from technical component services. Report separate professional and technical component services only if different providers perform the professional and technical portions of the procedure. Read CPT descriptors carefully. Do not use modifiers if the descriptor specifies professional or technical components. 51 Multiple Procedures Use to identify additional procedures that are performed on the same day or at the same session by the same provider. Do not use to designate "add-on" codes. 55 Postoperative Management only Surgery related eyewear Use with eyewear codes (lenses, lens dispensing, frames, etc.) to identify eyewear provided after eye surgery. Benefit for eyewear, including contact lenses, for members over age 20 must be related to surgery. Modifier -55 takes the place of the required claim comment that identifies the type and date of eye surgery. The provider must retain and, upon request, furnish records that identify the type and date of surgery. 59 Distinct Procedural Service Use to indicate a service that is distinct or independent from other services that are performed on the same day. These services are not usually reported together but are appropriate under the circumstances. This may represent a different session or member encounter, different procedure or surgery, different site or organ system or separate lesion or injury. 62 Two (2) surgeons Use when two (2) surgeons work together as primary surgeons performing distinct part(s) of a procedure, each surgeon should report his/her distinct operative work by adding modifier 62 to the procedure code and any associated add-on code(s) for that procedure as long as both surgeons continue to work together as primary surgeons 76 Repeat procedure or service by the same physician/provider/other qualified health care professional Use to identify subsequent occurrences of the same service on the same day by the same provider. Not valid with E/M codes. 77 Repeat procedure by another physician/provider/other qualified health care professional Use to identify subsequent occurrences of the same service on the same day by different rendering providers. 79 Unrelated procedure or service by the same surgeon during the postoperative period Unrelated procedures or services (other than E/M services) by the surgeon during the postoperative period. Use to identify unrelated services by the operating surgeon during the postoperative period. Claim diagnosis code(s) must identify a condition unrelated to the surgical procedure. 80 Assistant surgeon Use with surgical procedure codes to identify assistant surgeon services. Note: Assistant surgeon services by non-physician practitioners, physician assistants, perfusionists, etc. are not reimbursable. GY Item or services statutorily excluded or does not meet the Medicare benefit. Use with podiatric procedure codes to identify routine, non-Medicare covered podiatric foot care. Modifier -GY takes the place of the required provider certification that the services are not covered by Medicare. The Medicare non-covered services field on the claim record must also be completed. KX Specific required documentation on file Use with laboratory codes to certify that the laboratory's equipment is not functioning or the laboratory is not certified to perform the ordered test. The -KX modifier takes the place of the provider's certification, "I certify that the necessary laboratory equipment was not functioning to perform the requested test", or "I certify that this laboratory is not certified to perform the requested test." | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | General Instructions | A unit represents the number of times the described procedure or service was rendered. Except as instructed in this manual or in Health First Colorado bulletins, the billed unit must correspond to procedure code descriptions. The following examples show the relationship between the procedure description and the entry of units. Lens materials One (1) lens equals one (1) unit of service. If two (2) lenses of the same strength are provided, complete one (1) billing claim line, entering two (2) units of service and the total charge for both lenses. Lenses of different strengths are billed on separate claim lines. Lens dispensing A dispensing fee is allowed for each lens. For two (2) lenses, complete on claim line with two (2) units of service and charge for both lenses. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area)
Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||||||||||||||||||
CMS 1500 Vision Claim Example
Procedure/HCPCS Codes Overview
The Department accepts procedure codes that are approved by the Centers for Medicare & Medicaid Services (CMS). The codes are used for submitting claims for services provided to Health First Colorado members and represent services that may be provided by enrolled certified Health First Colorado providers.
The Healthcare Common Procedural Coding System (HCPCS) is divided into two (2) principal subsystems, referred to as level I and level II of the HCPCS. Level I of the HCPCS is comprised of Current Procedural Terminology (CPT), a numeric coding system maintained by the American Medical Association (AMA). The CPT is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other health care professionals. Level II of the HCPCS is a standardized coding system that is used primarily to identify products, supplies, and services not included in the CPT codes, such as ambulance services and durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) when used outside a physician's office. Level II codes are also referred to as alpha-numeric codes because they consist of a single alphabetical letter followed by 4 numeric digits, while CPT codes are identified using 5 numeric digits.
HIPAA requires providers to comply with the coding guidelines of the AMA CPT Procedure Codes and the International Classification of Disease, Clinical Modification Diagnosis Codes. If there is no time designated in the official descriptor, the code represents one (1)unit or session. Providers should regularly consult monthly bulletins located on the Bulletins web page. To receive electronic provider bulletin notifications, an email address can be entered in the Provider Data Maintenance area of the Provider Web Portal. Bulletins include updates on approved procedures codes as well as the maximum allowable units billed per procedure.
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
Vision and Eyewear Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/01/2016 | Manual revised for interChange implementation. For manual revisions prior to 11/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 9/30/17 | Updates based on new Vision and Eyewear rule implementation | HCPF |
| 2/28/2018 | Removed NDC supplemental qualifier - not relevant for vision and eyewear providers | DXC |
| 6/25/2018 | Updated billing and timely to point to general manual | HCPF |
| 6/28/2018 | Corrected spelling in header | HCPF |
| 8/13/2018 | Removed dental & menstrual references | HCPF |
| 12/20/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 2/28/2020 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 7/23/2021 | Added PETI Information | HCPF |
| 1/10/2024 | Added Eyeglass billing and record retention requirements | HCPF |
| 3/14/2024 | Added Temporary Site information | HCPF |
| 5/23/2024 | Eyeglasses and Orthoptic vision services | HCPF |
| 8/2/2024 | Corrected Orthoptic and Pleoptic Vision Therapy info POS 3 addition | HCPF |
| 11/21/24 | Ordering, Prescribing, and Referring Claim Requirements | HCPF |
| 4/3/2025 | Clarify Medical Necessity for Aspheric Lenses | HCPF |
| 6/30/2025 | Added language around adult glasses coverage | HCPF |