Immunizations Billing Manual
- Covered Services
- Pharmacy Administration of Vaccines
- Pharmacist Billing Guidelines
- Non-Covered Services and General Limitations
- General Billing Information
- Vaccine Administration Codes and Reimbursement Rates
- Using Pediatric Immunization Codes 90460 and 90461
- Using Vaccine Administration Codes 90471-90474
- Using Vaccine Administration Codes 96380 and 96381
- Preventive Medicine Counseling Codes
- Billing Instructions for Specific Providers
- Self-Administered Vaccines
- Medicare Crossover Claims (Medicare/Health First Colorado Claims)
- Immunization Billing Codes
- National Correct Coding Initiative (NCCI) Impacts on Immunization and Evaluation and Management (E&M) Codes
- COVID-19 Vaccines
- Synagis® (Palivizumab) Vaccine
- Nirsevimab and Clesrovimab
- Seasonal Influenza Vaccine
- CDPHE VFC Program
- CMS 1500 Paper Claim Reference Table
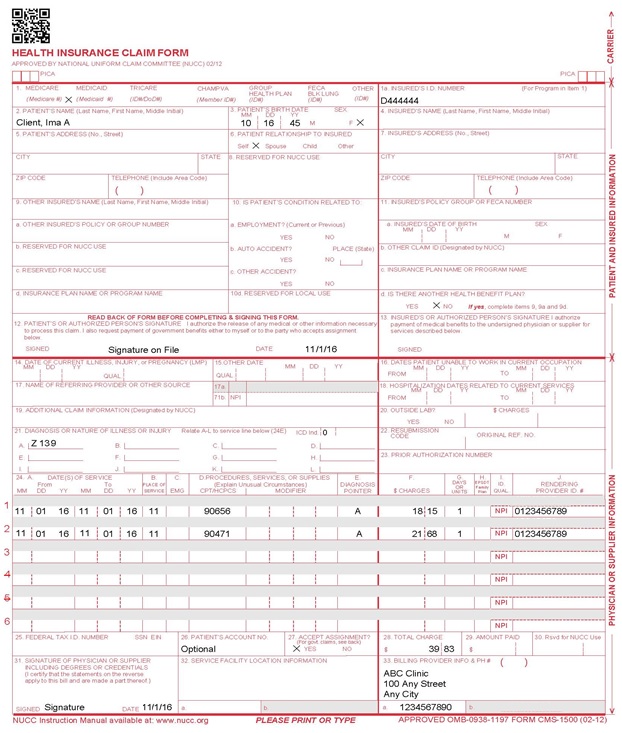
- CMS 1500 Immunization Claim Example
- Timely Filing
- Appendices
- Immunization Manual Revisions Log
Return to Billing Manuals Web Page
This Immunization Billing Manual provides a summary of benefits and billing guidelines for Health First Colorado (Colorado's Medicaid program) providers who administer vaccines to adults and children. The Department of Health Care Policy & Financing (the Department) periodically reviews and modifies immunization benefits and services. Therefore, the information in this manual is subject to change, and the manual is updated as new policies are implemented.
Visit the Provider Rates and Fee Schedules web page to access the most recent fee schedule.
The immunization benefit works to promote and facilitate the prevention of vaccine-preventable diseases. Health First Colorado maintains an inter-agency agreement with the Colorado Department of Public Health and Environment (CDPHE) to implement immunization recommendations by the Advisory Committee on Immunization Practices (ACIP) of the U.S. Department of Health and Human Services.
Covered Services
Immunizations for all Health First Colorado members are a benefit when recommended by the Advisory Committee on Immunization Practices (ACIP). This includes vaccines approved through an Emergency Use Authorization (EUA).
Health First Colorado members under 19 years of age are eligible to receive all immunizations available from the federal Vaccines for Children (VFC) Program at VFC-enrolled provider offices, as well as any other vaccine distributed by the federal government, at no cost, to Health First Colorado providers. Effective September 11, 2023, COVID-19 vaccines are included in the VFC Program.
- Refer to the Appendix B - Vaccines for Children Program section of this manual for more information about the VFC Program.
- Immunizations may be given during an Early Periodic Screening, Diagnosis and Treatment (EPSDT) periodic screening visit, an EPSDT inter-periodic visit or any other medical appointment.
- Health First Colorado-enrolled providers will be reimbursed for administering vaccines distributed to eligible providers by the federal government, at no cost, outside of the VFC Program.
- VCP vaccines cannot be used for anyone 19 and older.
- All vaccines that are part of the VFC Program are only reimbursable when administered to members under 19 years of age and when administered by a VFC-enrolled provider using VFC vaccine products.
- The influenza vaccine is covered for all members. All ACIP-recommended vaccines are covered for all Health First Colorado Members without cost-sharing.
Members enrolled in a Health First Colorado Managed Care Organization (MCO) must receive immunization services through a provider in the MCO's network.
Vaccines available from the VFC Program are updated annually and listed on the Immunization Rate Schedle located on the Provider Rates and Fee Schedule web page.
Refer to the Center for Disease Control and Prevention (CDC) Immunization Schedules for the current ACIP recommended schedules for children, teens and adults.
A vaccine product code, as well as an administration code, must always be included on any claims for vaccination.
Prior Authorization (PA)
There are no prior authorization (PA) requirements for any vaccine recommended by the ACIP. Refer to the Synagis® (Palivizumab) Vaccine section of this manual for more information about PA of Synagis®.
Pharmacy Administration of Vaccines
Enrolled pharmacists at Health First Colorado-enrolled pharmacies may counsel for and administer all covered vaccinations to Health First Colorado members aged 19 and older. Members enrolled in a Health First Colorado Managed Care Organization (MCO) must receive immunization services through a provider in the MCO's network.
Pharmacist Billing Guidelines
To submit vaccine claims, use these guidelines:
- The pharmacy's National Provider Identifier (NPI) is the billing provider.
- The pharmacist's NPI is the rendering provider.
- A product code must always be included in any claims for vaccination.
Pharmacists must follow the Board of Pharmacy Rules outlined in 3CCR 719-1, 19.00.00.
Visit the Quick Guides web page for additional information related to provider enrollment or claim submission.
Non-Covered Services and General Limitations
Health First Colorado will not reimburse providers for the cost of vaccines that are available through the VFC Program or for the cost of vaccines that the provider receives at no cost from the federal government. A product code, as well as an administration code, must always be included on any claims for vaccination. Providers must enroll with VFC, as well as Health First Colorado, and use VFC vaccines to receive reimbursement for vaccines administered to members under 19 years of age.
Immunizations for the sole purpose of international travel are not a benefit for Health First Colorado members.
Effective May 3, 2024, place of service 03 is an allowed place of service for all FFS benefits. In order for community providers to bill FFS to children in a school setting, the provider must follow school district policy. Please reference the Community Providers in a School Setting Policy memo. However, school district providers participating in the School Health Services (SHS) Program may not bill for immunizations.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page or general billing information.
Vaccine Administration Codes and Reimbursement Rates
The following codes should be used for all vaccine administration, including VFC vaccine administrations for members under 19 years of age. Report these codes in addition to the vaccine and toxoid code(s).
| Current Procedural Terminology (CPT) Code | |
|---|---|
| Use the following codes for VFC vaccine administration to members under 19 years of age with face-to-face counseling of the member/family during the vaccine administration: | |
| 90460 | 90461 (used to indicate multi-component vaccinations when listed in addition to 90460) |
| Use the following codes for vaccine administration to members of any age when the administration is not accompanied by any face-to-face counseling, or for administration to members over 18 years of age with or without counseling: | |
| 90471 | + 90472 (List separately in addition to 90471, 90473) |
| + 90472 | + 90474 (List separately in addition to 90471, 90473) |
| Use the following codes for nirsevimab administration | |
| 96380 or 96381 | Use 96380 when the administration is accompanied by provider counseling. Use 96381 when the administration is not accompanied by provider counseling. Code selection is based on whether a provider provided counseling on the same date as the administration of nirsevimab or clesrovimab. |
| Use the following code for vaccine administration to members of any age when administering COVID-19 vaccines | |
| 90480 | |
Refer to the Immunization Fee Schedule located on the Provider Rates and Fee Schedules web page for the most up-to-date rate information.
Using Pediatric Immunization Codes 90460 and 90461
The following chart identifies the number of components in some of the common pediatric vaccines and how to report the pediatric immunization administration codes for each vaccine.
Table 1
| Vaccine | # of Components | Which Administration Codes to Report? |
|---|---|---|
| HPV | 1 | 90460 |
| Influenza | 1 | 90460 |
| Meningococcal | 1 | 90460 |
| Pneumococcal | 1 | 90460 |
| Td | 2 | 90460, 90461 |
| DTaP or Tdap | 3 | 90460, 90461, 90461 |
| MMR | 3 | 90460, 90461, 90461 |
| DTaP-Hib-IPV | 5 | 90460, 90461, 90461, 90461, 90461 |
| DTaP-HepB-IPV | 5 | 90460, 90461, 90461, 90461, 90461 |
| DTaP-IPV | 4 | 90460, 90461, 90461, 90461 |
| MMRV | 4 | 90460, 90461, 90461, 90461 |
| DTaP-Hib | 4 | 90460, 90461, 90461, 90461 |
| HepB-Hib | 2 | 90460, 90461 |
| Rotavirus | 1 | 90473 |
| IPV | 1 | 90460 |
| Hib | 1 | 90460 |
Source: American Academy of Pediatrics
To submit claims for immunization services, providers must "roll up/bundle" the total unit count of the immunization administration codes.
- If an immunization administration code is billed for each vaccine that was given during the visit as its own line item, each subsequent line item billed using 90460 after the initial 90460 line item will be denied as a duplicate claim.
Example 1:
The following example demonstrates how to bill for the administration of Hep A, DTaP-HIB-IPV and MMR vaccines.
Component Calculation and which codes to report using Table 1
Table 2
| Vaccine | # of Components | Which Codes to Report? |
|---|---|---|
| Hep A | 1 | 90460 |
| DTaP-HIB-IPV | 5 | 90460, 90461, 90461, 90461, 90461 |
| MMR | 3 | 90460, 90461, 90461 |
How to Bill
Table 3
| Line # | CPT Descriptor | CPT Code | Units |
|---|---|---|---|
| Line 1 | First Vaccine Component | 90460 | 3 |
| Line 2 | Additional Vaccine Component | 90461 | 6 |
| Line 3 | Hep A | 90633 | 1 |
| Line 4 | DTaP-HIB-IPV | 90698 | 1 |
| Line 5 | MMR | 90707 | 1 |
- Current Procedural Terminology (CPT) code 90460 is billed for three (3) units because it was reported once for each vaccine that was administered.
- CPT code 90461 is billed for six (6) units because it was reported six (6) times, four (4) times for the DTaP-HIB-IPV vaccine and two (2) times the MMR vaccine).
Visit the American Academy of Pediatrics (AAP) Child Health Finance & Payment Strategy web page for further clarification on billing pediatric immunization codes.
Contact the Provider Services Call Center for billing questions.
Using Vaccine Administration Codes 90471-90474
The immunization administration codes 90471-90474 need to be billed as one (1) line item, and the vaccine product should be billed as a separate line item. In order for an immunization claim to be reimbursed, both an administration code and the vaccine product must be billed. If immunization is the only service rendered, providers may not submit charges for an Evaluation and Management (E&M) service.
Adult immunizations are reimbursed at the lower of billed charges or the Health First Colorado fee schedule amount for each immunization.
Note: Providers are not to bill CPT codes 90471-90474 for children ages 0 through 18 for whom counseling was given. Refer to the Using Pediatric Immunization Codes 90460 and 90461 section in this manual. CPT Codes 90471-90474 must only be billed for members aged 19 and older or members aged 18 and under for whom no counseling was given.
Using Vaccine Administration Codes 96380 and 96381
The nirsevimab and clesrovimab administration codes 96380 or 96381 must be billed as one (1) line item, and the immunization product should be billed as a separate line item. For an immunization claim to be reimbursed, both an administration code and the immunization product code must be billed. If immunization is the only service rendered, providers may not submit charges for an E&M service.
Preventive Medicine Counseling Codes
Health First Colorado covers vaccine counseling visits in which healthcare providers talk to families about the importance of vaccination.
Health First Colorado also covers and will reimburse for stand-alone vaccine counseling visits as part of vaccine administration required for all routine vaccines. Providers should bill CPT G0310, G0311, G0312, G0313, G0314, or G0315 for visits in which healthcare providers give counseling about the importance of vaccination. Providers should include modifier CR for all COVID-19 vaccine counseling-only visits.
Providers should not bill for the vaccine counseling code and the vaccine administration code on the same date of service when vaccine administration codes are inclusive of counseling.
CPT G0310, G0311, G0312, G0313, G0314 or G0315 can be billed at only one (1) visit for each member per day, but there are no quantity limits for the number of times this education is provided to an individual member.
Keep documentation in the member's chart that shows the duration of counseling and a list of the prevention topics covered during counseling.
If there is a separately identifiable E&M service performed outside of vaccine counseling and immunization administration, a separate E&M visit code may be reported along with modifier 25.
When using a modifier is appropriate, refer to the Medicaid National Correct Coding Initiative (NCCI) web page of the Centers for Medicare & Medicaid Services (CMS) website for specific guidance on the proper use of modifiers.
Billing Instructions for Specific Providers
Pharmacists
Pharmacists must bill for vaccinations on a professional claim (CMS 1500) either via batch through a vendor or through the Provider Web Portal using the pharmacy's NPI as the billing provider, the pharmacist's NPI as the rendering provider and the physician on the standing order as the ordering provider.
- Pharmacies must have a Provider Web Portal account because the pharmacists do not bill. They are strictly the renderer on the claims.
- Pharmacies can add a pharmacist to their Provider Web Portal account as a delegate for the purpose of submitting claims on their behalf. Refer to the Delegates - Provider Web Portal Quick Guide for instructions.
- Pharmacies can submit FFS claims via the Provider Web Portal or batch claims via the 837P.
- If the member is enrolled in Denver Health Medicaid Choice or Rocky Mountain Health Plans Prime, providers must submit the claim to the MCO.
Health First Colorado members enrolled in an MCO must receive immunization services from the MCO, and providers may not bill Health First Colorado directly for vaccines provided to these members.
Outpatient, Emergency Room or Inpatient Hospital
Immunization administration may be billed as part of an outpatient or emergency room visit when the visit is for medical reasons.
Outpatient or emergency room visits cannot be billed for the sole purpose of immunization administration. Administration of immunization at the time of an inpatient stay is included in the All Patients Refined Diagnosis Related Group (APR-DRG).
Federally Qualified Health Centers (FQHCs) and Rural Health Centers (RHCs)
Federally Qualified Health Centers (FQHCs) and Rural Health Centers (RHCs) may bill an encounter fee even if the only service provided is immunization administration by a billable provider, so long as the visit otherwise qualifies as a billable encounter per 10 CCR 2505-10 8.700 FQHC and 8.740 RHC. If immunization is administered in addition to a routine office visit, then an additional encounter fee may not be billed.
Nursing facility residents may receive immunizations if ordered by their physician. The skilled nursing component for immunization administration is included in the facility's rate. The vaccine itself may be billed directly to Health First Colorado by a Health First Colorado enrolled pharmacy. The pharmacy must bill the appropriate National Drug Code (NDC) for the individual vaccine dose under the member's Health First Colorado ID.
Home Health
A member receiving home health services may receive immunizations if the administration is part of a normally scheduled home health visit. A home health visit for the sole purpose of immunization administration is not a benefit.
The pharmacy bills the vaccine as an individual dose under the member's Colorado Health First Colorado ID. The home health agency may not bill for the vaccine.
Alternative Health Care Facilities (ACFs)/Group Homes
Residents of an Alternative Health Care Facility (ACF) may receive immunizations from their own physicians. They may also receive vaccines under home health as stated above in the home health guideline.
Health First Colorado does not pay for home health agencies, physicians or other non-physician practitioners to go to nursing facilities, group homes or residential treatment centers to administer immunizations (e.g., flu vaccines) to groups of members.
Medicare Crossover Claims (Medicare/Health First Colorado Claims)
For Medicare crossover claims, Health First Colorado pays the Medicare deductible and coinsurance or Health First Colorado allowable reimbursement minus the Medicare payment, whichever amount is less. If Medicare's payment for immunization services is the same or greater than the Health First Colorado allowable benefit, no additional payment is made.
If Medicare pays 100% of the Medicare allowable, Health First Colorado makes no additional payment.
Self-Administered Vaccines
Vaccines approved for self-administration are a covered benefit. When administered by a healthcare provider, the claim must include the Current Procedural Terminology (CPT) code for the vaccine product, as well as the corresponding administration CPT code. When self-administered, or administered by the member’s caregiver, the claim should contain only a vaccine product CPT code.
Immunization Billing Codes
Refer to the Appendix B - Vaccines for Children (VFC) Program section of this manual.
National Correct Coding Initiative (NCCI) Impacts on Immunization and Evaluation and Management (E&M) Codes
Effective April 1, 2014, the Department will no longer reimburse NCCI Procedure-to-Procedure (PTP) edits when immunization administration procedure codes (CPT 90460-90474) are paired with preventive medicine E&M service procedure codes (CPT 99381-99397).
If a significant separately identifiable E&M service (e.g., new or established member office or other outpatient services [99201-99215], office or other outpatient consultation [99241-99245], emergency department service [99281-99285], preventive medicine service [99381-99429] is performed), the appropriate E&M service code should be reported in addition to the vaccine and toxoid administration codes.
Each NCCI PTP edit has an assigned modifier indicator. A modifier indicator of 0" indicates that NCCI PTP-associated modifiers cannot be used to bypass the edit. A modifier indicator of 1" indicates that NCCI PTP-associated modifiers may be used to bypass an edit under appropriate circumstances. A modifier indicator of 9" indicates that the edit has been deleted and the modifier indicator is not relevant. The Correct Coding Modifier Indicator can be found in the files containing Health First Colorado NCCI PTP edits on the Medicare NCCI Edits web page of the Centers for Medicare & Medicaid Services (CMS) website.
A modifier should not be added to a Healthcare Common Procedure Coding System (HCPCS)/CPT code solely to bypass an NCCI PTP edit if the clinical circumstances do not justify its use. If the E&M service is significant and separately identifiable and performed on the same day, the E&M code should be billed with the vaccine and toxoid administration codes using PTP associated modifier '25.' Modifier '25' is only valid when appended to the E&M codes. Do not append to the immunization administration procedure codes 90460-90474.
COVID-19 Vaccines
COVID-19 vaccines are used to prevent Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) viral infections and the disease they cause, Coronavirus disease (COVID-19). All FDA-approved COVID-19 vaccines are a covered benefit for all Health First Colorado Members without cost-sharing and without prior authorization. This includes COVID-19 vaccines approved under an Emergency Use Authorization (EUA). If providers receive the vaccine product at no cost, Health First Colorado will reimburse for vaccine administration only. Providers serving adult members (aged 19 and up) may also seek reimbursement for commercially purchased COVID-19 vaccine products in addition to vaccine administration. A product code, as well as an administration code, must always be included in any claims for vaccination. Effective September 11, 2023, pediatric COVID-19 vaccines are part of the VFC Program and must be administered by a VFC-enrolled provider using VFC vaccine products.
Synagis® (Palivizumab) Vaccine
Synagis® (Palivizumab) is used to prevent serious lower respiratory tract disease caused by Respiratory Syncytial Virus (RSV) in certain high-risk pediatric members. The Department uses coverage criteria based on the American Academy of Pediatrics (AAP) 2014 and the Colorado Chapter of the AAP recommendations for RSV prophylactic therapy. Synagis® (Palivizumab) is not provided by the VFC Program.
Synagis® is administered by intramuscular injections, at 15 mg per kg of body weight, once a month during expected periods of RSV frequency in the community. Synagis® administration must be prior authorized. Members who have received nirsevimab or clesrovimab may not receive subsequent Synagis® in the same season.
Synagis® season usually begins in the fall. Refer to the annual Synagis® provider bulletin on the Provider Bulletins web page for more information.
- The Department will provide pricing information during each Synagis® season.
- Providers may not ask members to obtain Synagis® from a pharmacy and bring it to the practitioner's office for administration.
- Synagis® given in a doctor's office, hospital or dialysis unit is to be billed directly by those facilities as a medical benefit. Prior Authorization Requests (PARs) for Synagis® billed as a medical benefit shall be submitted to the fee for service Utilization Management (UM) vendor via their online PAR portal, Atrezzo.
- Synagis® may only be a pharmacy benefit if the medication is administered in the member's home or long-term care facility.
Note: A separate Synagis® PAR process exists for the Child Health Plan Plus (CHP+) State Managed Care Network members. Any questions regarding this process should be directed to Colorado Access at 303-751-9005 or 800-511-5010, or US Bioservices at 303-706-0053.
Nirsevimab and Clesrovimab
Nirsevimab and clesrovimab are monoclonal antibodies for the prevention of Respiratory Syncytial Virus (RSV) lower respiratory tract disease. They are available through the VFC Program for providers enrolled in the program to administer to Health First Colorado enrolled children. It does not require prior approval. Report the administration of nirsevimab or clesrovimab with codes 96380 or 96381. Do not report immunization administration codes 90461–90462 or 90471–90472 for the injection of nirsevimab or clesrovimab. Members who have received nirsevimab or clesrovimab may not receive subsequent Synagis in the same season.
Seasonal Influenza Vaccine
Seasonal influenza vaccine is a benefit for children and adults and is recommended for individuals who are six (6) months of age or older. Influenza vaccine is available through the VFC Program for providers enrolled in the program to administer to Health First Colorado-enrolled children/adolescents (under 19 years of age). Refer to the Appendix B - Vaccines for Children (VFC) Program section in this manual.
Refer to the annual Synagis® and Influenza Vaccines provider bulletin located on the Provider Bulletins web page for more Health First Colorado information on the seasonal influenza vaccine for both children and adults.
CDPHE VFC Program
The VFC Program, administered by CDPHE, partners with Health First Colorado to provide free vaccines for providers to administer to Health First Colorado-enrolled children.
Participation in the VFC Program is strongly encouraged by the Department. VFC participation is required for reimbursement for administration of vaccines to members under 19 years of age. Providers, including but not limited to private practitioners, managed care providers, local public health agencies, RHCs, hospital outpatient clinics, school-based health centers, pharmacies and FQHCs, who wish to participate in the immunization program must enroll with CDPHE. Visit the Vaccines for Children web page or call 303-692-2650 for information on the CDPHE VFC Program.
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 professional claim form.
| CMS Field Number and Label | Field is: | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado identification card. Example: A123456 | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014 Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES," enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES," enter the policy or group number. | ||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES," enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the identification card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014 Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES," complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's Signature | Required | Enter "Signature on File," "SOF," or legal signature. If there is no signature on file, leave blank or enter "No Signature on File." Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury, or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014 Enter the applicable qualifier to identify which date is being reported. | ||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016 If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019
or
Span dates of service
Practitioner claims must be consecutive days.
VP - Vendor Product Number | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes. 01 - Pharmacy | ||||||||||||||||||||||||||||||||||||
| 24C. EMG (Emergency) | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services or Supplies | Required | Enter the procedure code that specifically describes the service for which payment is requested. | ||||||||||||||||||||||||||||||||||||
| 24D. | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. Telemedicine For originating provider, use procedure code Q3014. For distant provider, use procedure code + modifier GT. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first and then other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only. Do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early and Periodic Screening, Diagnosis, and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available- Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) If the service is Family Planning, enter "Y" for YES or "N" for NO in the bottom, unshaded area of the field. | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016 Unacceptable signature alternatives: | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Information & Phone Number # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
CMS 1500 Immunization Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Appendices
Appendix A - Immunization Schedules
- Recommended Immunization schedule for persons aged 0 through 18 years.
- Recommended Immunization schedule for adults aged 19 and older.
Appendix B - Vaccines for Children (VFC) Program
Visit the Vaccines for Children web page for updated information about the VFC Program.
Immunization Manual Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manuals Comment Log v0_2.xlsx. | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 2/12/2018 | Removed NDC supplemental qualifier - not relevant for immunization providers | DXC |
| 6/22/2018 | Updated general billing and timely filing | HCPF |
| 10/15/2018 | Added pharmacy-specific billing information | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 1/9/2020 | Converted to web page | HCPF |
| 7/22/2020 | Added pharmacy-specific flu vaccine billing information | HCPF |
| 9/10/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 12/10/2020 | Added 2 codes to pharmacy-specific flu vaccine billing information and added information about COVID-19 vaccines | HCPF |
| 1/14/2021 | MCO, Nursing Facility and ACF policy edits. Co-pay policy clarification | HCPF |
| 2/3/2021 | Clarification of FQHC/RHC reimbursement policy for immunizations and added flu code | HCPF |
| 2/23/2021 | Removed IHS references, clarify need for both product and administration codes, addition of 91303 and 0031A to pharmacy-specific billing information | HCPF |
| 6/7/2021 | MCO billing clarification for COVID-19 vaccines | HCPF |
| 8/16/2021 | Added COVID-19 booster codes and update 2021 Synagis info | HCPF |
| 9/14/2021 | Added 90865 to Pharmacy flu codes | HCPF |
| 11/2/2021 | Added COVID-19 vaccine codes | HCPF |
| 12/8/2021 | Added 90677 | HCPF |
| 1/12/2022 | Added COVID-19 vaccine codes | HCPF |
| 1/12/2022 | Added Vaccine Counseling | HCPF |
| 2/8/2022 | Modify Vaccine Counseling | HCPF |
| 2/8/2022 | Add 90671 to Pharmacy Section | HCPF |
| 5/6/2022 | Add Routine Adult Vaccines to Pharmacy Section | HCPF |
| 6/13/2022 | Vaccine Counseling codes & Covid-19 vaccine codes | HCPF |
| 7/19/2022 | Added COVID-19 Vaccine codes | HCPF |
| 7/19/2022 | Add 90713, 91304 and 90749 to Pharmacy section | HCPF |
| 11/14/2022 | Update Monkeypox and COVID-19 vaccine codes. Pharmacy Section | HCPF |
| 11/14/2022 | Update annual Synagis dates | HCPF |
| 11/14/2022 | Add COVID-19 Vaccine administration CPT codes | HCPF |
| 12/19/2022 | Add COVID-19 pediatric booster codes | HCPF |
| 3/3/2023 | Updated linked to immunization schedules | HCPF |
| 3/27/2023 | Updated AWS URL Links | HCPF |
| 6/9/2023 | Updated Covered Services Language | HCPF |
| 6/9/2023 | Updated COVID-19 Vaccine CPT Codes | HCPF |
| 8/24/2023 | Add RSV vaccine information | HCPF |
| 9/28/2023 | Commercial COVID codes and additional RSV and VFC updates, general edits for consistency and style | HCPF |
| 1/2/2024 | Updated RSV administration codes | HCPF |
| 7/5/2024 | Add place of service 03 information | HCPF |
| 8/15/2024 | Update pharmacy administration information. | HCPF |
| 9/12/2024 | RSV spelling corrections | HCPF |
| 4/28/2025 | Removed expired PHE policies | HCPF |
| 9/25/2025 | Update RSV information. Added self-Administered Vaccines. | HCPF |