Outpatient Imaging and Radiology Billing Manual
- General Benefit Policies
- Payment for Covered Services/Procedures
- Covered Imaging and Radiology Procedures
- Benefit Limitations
- Coding Guidelines
- Prior Authorization Requirements and Information
- Billing Information
- Procedure/HCPCS Codes Overview
- CMS 1500 Paper Claim Reference Table
- Timely Filing
- Outpatient Imaging and Radiology Revisions Log
Return to Billing Manuals Web Page
General Benefit Policies
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid program) provider in order to:
- Treat a Health First Colorado member, and
- Submit claims for payment to Health First Colorado.
Imaging and radiology services are a benefit under the following conditions:
- Services must be authorized and supervised by a licensed physician.
- The services are performed to diagnose conditions and illnesses with specific symptoms.
- The services are performed to prevent or treat conditions that are Health First Colorado covered benefits.
- The services are not routine diagnostic tests performed without apparent relationship to treatment or diagnosis for a specific illness, symptom, complaint, or injury.
- Radiology services are performed by a provider with equipment certified by the Colorado Department of Public Health and Environment (CDPHE) and enrolled as a Health First Colorado Provider.
The Department of Health Care Policy & Financing (the Department) periodically modifies billing information. Therefore, the information in this manual is subject to change, and the manual is updated as new billing information is implemented.
Payment for Covered Services/Procedures
Regardless of whether Health First Colorado has actually reimbursed the provider, billing members for covered procedures is strictly prohibited. Balance billing is prohibited. If reimbursement is made, providers must accept this payment as payment in full. Refer to Program Rule 8.012. The provider may only bill the member for procedures not covered by Health First Colorado.
- Members may be billed for non-covered procedures in accordance with C.R.S. 25.5-4-301(1)(a)(I).
- (1) (a) (I) Except as provided in section 25.5-4-302 and subparagraph (III) of this paragraph (a), no recipient or estate of the recipient shall be liable for the cost or the cost remaining after payment by Medicaid, Medicare, or a private insurer of medical benefits authorized by Title XIX of the social security act, by this title, or by rules promulgated by the state board, which benefits are rendered to the recipient by a provider of medical services authorized to render such service in the state of Colorado, except those contributions required pursuant to section 25.5-4-209 (1). However, a recipient may enter into a documented agreement with a provider under which the recipient agrees to pay for items or services that are nonreimbursable under the medical assistance program. Under these circumstances, a recipient is liable for the cost of such services and items.
- If a PAR for procedures are required, the following policy applies:
- Technical/lack of information (LOI) denial does not mean those procedures are not covered. Members may not be billed for procedures denied for LOI.
- Procedures partially approved are still considered covered procedures. Members may not be billed for the denied portion of the request.
- Procedures totally denied for not meeting medical necessity criteria are considered non-covered services.
Covered Imaging and Radiology Procedures
Health First Colorado covers procedures including but not limited to: angiograms, computed tomography (CT scans), electrocardiograms (ECG), magnetic resonance imaging (MRI scans), mammograms, positron emission tomography (PET scans), radiation treatment, ultrasounds, and X-rays.
An exhaustive list of covered procedures may be found on the Department's Fee Schedule located on the Provider Rates and Fee Schedule web page.
Benefit Limitations
- Procedures for cosmetic treatment or infertility treatment (ICD-10 N97) are not covered.
- Procedures considered experimental or not approved by the Food and Drug Administration (FDA) are not covered.
- Procedures not ordered by the member's attending or treating physician are not covered.
- Procedures which are part of a clinical study are not covered.
Computed Tomography
- CT of sinuses for acute, uncomplicated rhinosinusitis (ICD-10 J01) is not covered.
- Virtual Colonoscopy (CPTs 74261, 74262, 75263) is covered at a frequency of once every five (5) years.
Magnetic Resonance Imaging
- Imaging of cortical bone and calcifications, and procedures involving spatial resolution of bone and calcifications are not covered.
- Imaging of the same anatomic area to address patient positional changes, additional sequences, or equipment failure is not allowed. These variations or extra sequences are included within the original imaging authorization request.
Preventive Lung Cancer Low Dose Computed Tomography (LDCT) Screening
Health First Colorado covers annual screening for lung cancer in accordance with the U.S. Preventive Services Task Force (USPSTF) recommendation.
The following policies are effective as of January 1, 2021:
HCPCS code G0297 has been replaced with CPT code 71271.
- CPT code 71271 must be used and always requires Prior Authorization.
- ICD-10 diagnosis code Z12.2 must be reported on the claim.
- Benefit is limited to one (1) screening (one [1] billed unit of service) per state fiscal year (July 1 - June 30).
The following policies were effective prior to January 1, 2021:
- HCPCS code G0297 must be used. G0297 always requires Prior Authorization.
- ICD-10 diagnosis code Z12.2 must be reported on the claim.
- Benefit is limited to one (1) screening (one [1] billed unit of service) per state fiscal year (July 1 - June 30).
Coding Guidelines
- Regardless of billing provider type, component modifiers must be indicated on the claim if reimbursement for the procedure is split between the professional and technical components.
- Professional component - modifier 26
- Technical component - modifier TC
- Claims lacking a component modifier are understood to be inclusive of both components and will be reimbursed as payment in full for the entire procedure. Any separate claim for the same procedure, billed on the same date of service, will be considered an overpayment and may be subject to recovery.
- Outpatient Hospital claims for Imaging and Radiology must be billed via an 837I (UB-04 paper claim), Practitioner procedure claims must be billed via an 837P (CMS1500 paper claim)
- National Correct Coding Initiative (NCCI) billing edits affect this benefit. Providers should be familiar with the information on the National Correct Coding Initiative in Medicaid web page on the Centers for Medicare & Medicaid Services (CMS) website, including the NCCI Policy Manual found there.
- All claims must include the National Provider Identification (NPI) number of the enrolled provider who rendered the service.
- All claims must include the NPI number of the enrolled provider who ordered the service.
Unlisted Procedure Codes
Unlisted radiology procedure codes are used when there is no CPT or HCPCS code that accurately identifies the services performed. Unlisted procedure codes will be priced by a clinical reviewer with the Department's fiscal agent.
Claims with unlisted codes must include as attachments the operating report from the procedure and the Unlisted Procedure Code Form located on the Provider Forms web page under the Claim Forms and Attachments drop-down. All lines on the Unlisted Procedure Code Form must be completed. The Department will deny claims lacking the required attachments. Claims denied for incomplete information will have to be resubmitted with the correct information for reimbursement.
Billing Modifiers for Bilateral Radiology Procedures
Bilateral radiology procedures should be reported using modifiers RT and LT. When using both modifiers for an appropriate radiology code on the same claim, each code should be billed on a separate line of the claim: one (1) with modifier RT indicating the right side, and one (1) with modifier LT indicating the left side. If bilateral radiology procedures are reported using modifier 50, claims may be denied.
Prior Authorization Requirements and Information
Health First Colorado requires all outpatient hospitals and free-standing radiology/X-ray facility centers to obtain a prior authorization (prior authorization request, PAR) for most non-emergent CT, non-emergent MRI, and all PET scans. A PAR precedes the submission of a claim and must be approved in advance of the claim. Procedures which require a PAR cannot be claimed for without an approved PAR on record. Refer to the Department's Fee Schedule located on the Provider Rates and Fee Schedule web page for a list of all procedure codes which require a PAR.
All Imaging and Radiology PARs and revisions are processed by the ColoradoPAR Program and must be submitted using Atrezzo, the Acentra portal. PARs submitted via fax or mail will not be processed. These PARs will be returned to providers via mail. This requirement only impacts PARs submitted to the ColoradoPAR Program.
To ensure claims are quickly and accurately processed, all claims for procedures which require a PAR must:
- Contain the correct Billing Provider ID number.
- Contain procedure codes which match the corresponding PAR on record.
- Contain modifier codes which match the corresponding PAR on record.
Contact the ColoradoPAR Program or visit the Department's ColoradoPAR Program web page for more information.
PAR Revisions
If a procedure is prior authorized but the desired test was changed just prior to the time of the service, the provider is responsible for submitting a PAR revision with adequate documentation within 48 hours of the date of service for the PAR to be processed by the ColoradoPAR Program. PAR revisions can only be submitted using Atrezzo. Contact the ColoradoPAR Program with questions regarding how to process PAR revisions.
PAR Exceptions
To request a PAR exception, contact the ColoradoPAR Program or visit the Department's ColoradoPAR Program web page.
- Emergency outpatient imaging and radiology procedures are exempt from PAR requirements. To mark a claim as emergency, check the emergency indicator field.
- All PET and SPECT scan procedures require prior authorization regardless of whether emergency is indicated.
- A PAR is not required when Medicare, Medicare Advantage plans, or private insurance has made primary payment on the claim. If third party liability (TPL) carriers have not made payment on the claim, the service must be prior authorized to ensure it meets medical necessity standards of the Health First Colorado program.
- PARs are not required of any Imaging and Radiology procedure for the professional component if the procedure billing is split between components. The technical component still requires prior authorization.
The Department will allow retroactive authorizations when a member's eligibility is determined after the date that the service is performed. When a member's eligibility is determined after the date of service, the member is issued a Load Letter. The Load Letter must be submitted with the supporting clinical documentation for the PAR for a retroactive request to be processed by ColoradoPAR.
PAR Denials
If the PAR is denied, contact the ColoradoPAR Program or visit the Department's ColoradoPAR Program web page.
Other PAR Policies
- It is the provider's responsibility to maintain clinical documentation to support procedures provided in the member's file in the event of an audit or retroactive review. Submitted PARs without minimally required information or with missing or inadequate clinical information will result in a lack of information (LOI) denial.
- All accepted PARs are reviewed by the authorizing agency. The authorizing agency approves or denies, by individual line item, each requested service or supply listed on the PAR.
- Paper PAR forms and completion instructions are located on the Provider Forms web page. They must be completed and signed by the member's physician and submitted to the authorizing agency for approval.
- Providers should not render procedures or submit claims for procedures that require prior authorization before the PAR is approved. After the authorizing agency has reviewed the request, the PAR status is transmitted to the fiscal agent's prior approval system.
- The status of the requested procedures is available through the Provider Web Portal. In addition, after a PAR has been reviewed, both the provider and the member receive a PAR response letter detailing the status of the requested procedures. Some procedures may be approved and others denied. Check the PAR response carefully as some line items may be approved and others denied.
- Approval of a PAR does not guarantee Health First Colorado reimbursement and does not serve as a timely filing waiver. Authorization only assures that the approved service is a medical necessity and is considered a Health First Colorado covered benefit.
Billing Information
Ordering, Prescribing and Referring (OPR) Providers
Health First Colorado complies with Federal Medicaid Regulations in 42 CFR 455.410(b) which provide that Medicaid must require all ordering or referring physicians or other professionals providing services be enrolled as providers, and 42 CFR 455.440, which provides that Health First Colorado must require all claims for the payment of items and services that were ordered, referred, and prescribed to include the National Provider Identifier (NPI) of the ordering, referring or prescribing physician or other professional.
Effective July 1, 2022, the Department will enforce the federal requirement 42 CFR § 455.440 that claims for all Imaging and Radiology services, rendered by any type of provider, contain the NPI of the provider who ordered the services, and that the NPI is actively enrolled with Health First Colorado. The ordering NPI may be that of the qualified provider overseeing the member’s care, for example as is the case with maternity services.
Providers are instructed to place the NPI of the ordering provider into the following locations for claim submission:
Professional Claims
- Paper claims use field 17.b
- Electronic submissions use loop 2420e with qualifier DK.
Imaging and Radiology services can be ordered by either a physician, physician assistant, advanced practice nurse or podiatrist. The ordering provider must also be actively enrolled with Health First Colorado. If these conditions are not met the claim will be denied.
Visit the OPR Claim Identifier Project web page for further information on this project.
Refer to the General Provider Information Manual located on the Billing Manuals web page for general billing information.
Billing Edits
The provider's adherence to the application of policies in this manual is monitored through either post-payment review of claims by the Department, or computer audits or edits of claims. When computer audits or edits fail to function properly, the application of policies in this manual remain in effect. Therefore, all claims shall be subject to review by the Department.
Procedure/HCPCS Codes Overview
All outpatient radiology procedures must be billed using HCPCS codes.
When submitting claims for radiology to the Health First Colorado, observe the following guidelines:
- Always use the most current CPT revision. The Health First Colorado adds and deletes codes as they are published in annual revisions of the CPT.
- Use CMS codes only when CPT codes are not available or are not as specific as the CMS codes.
Not all codes listed in the annual Health First Colorado HCPCS code publications are benefits of the Health First Colorado. Read the entire entry to determine the benefit status of the item.
The CPT Manual can be purchased at local university bookstores and from the American Medical Association at the following address:
Book & Pamphlet Fulfillment: OP 341/9
American Medical Association
P.O. Box 10946
Chicago, Illinois 60610
Refer to the General Provider Information Manual for more information on the procedure/HCPCS codes.
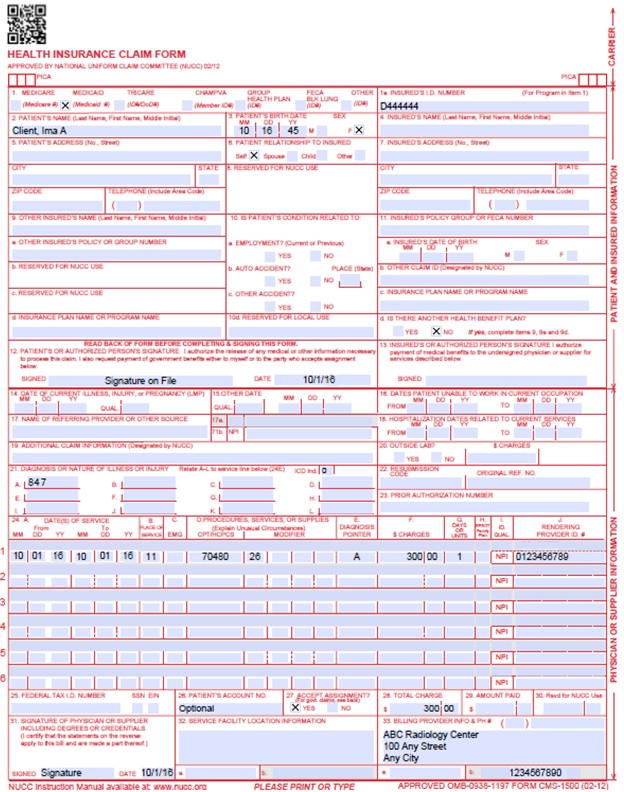
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Required | OPR NPI Number is required in accordance with Program Rule 10 CCR 2505-10 8.125.8.A | ||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070115 for July 1, 2015. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | CLIA When applicable, enter the word "CLIA" followed by the number. | ||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one (1) that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||
| 24D. | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. 26 - Professional component TC - Technical component 76 - Repeat procedure, same physician 77 - Repeat procedure, different physician 50 - Bilateral procedure- Both sides of the body are imaged LT/RT - Left side/Right side- Only one (1) side was imaged 59 - Indicates that two (2) or more procedures are performed at different anatomic sites or different member encounters. Only use if no other modifier more appropriately describes the relationships of the two (2) or more procedure codes. 52 - Reduces services- Under certain circumstances, a services or procedure is reduced or eliminated at the physician's discretion. 53 - Discontinued services- Under certain circumstances, a physician may elect to terminate a diagnostic procedure. 25 - Separate procedure during an evaluation and management visit- If a radiologist performs office visits and/or consultations and performs procedures (not 7xxxx codes) that are separately identifiable on the same date of service. | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. Anesthesia Services Anesthesia services must be reported as minutes. Units may only be reported for anesthesia services when the code description includes a time period. Anesthesia time begins when the anesthetist begins member preparation for induction in the operating room or an equivalent area and ends when the anesthetist is no longer in constant attendance. No additional benefit or additional units are added for emergency conditions or the member's physical status. The fiscal agent converts reported anesthesia time into fifteen minute units. Any fractional unit of service is rounded up to the next fifteen minute increment. Codes that define units as inclusive numbers Some services such as allergy testing define units by the number of services as an inclusive number, not as additional services. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early and Periodic Screening, Diagnosis and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available- Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) Not Required | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. Unacceptable signature alternatives: Claim preparation personnel may not sign the enrolled provider's name. Initials are not acceptable as a signature. Typed or computer printed names are not acceptable as a signature. "Signature on file" notation is not acceptable in place of an authorized signature. | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
CMS 1500 Radiology Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Outpatient Imaging and Radiology Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016 Please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 6/15/2018 | Reorganized some information to improve layout. Clarified ordering/rendering provider NPI requirements. Clarified co-pay policy. Removed out of date LDCT lung cancer screening billing information. Clarified clinical trial coverage. Added specific exclusions for CT and MRI scans. | HCPF |
| 7/9/2018 | Updated co-payment to co-pay per style guide, updated timely filing info and general billing info (removed duplication from general manual & provided links) | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 1/15/2020 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 10/26/2020 | Incorporated August 2019 Provider Bulletin material for Billing Modifiers for Bilateral Radiology Procedures | HCPF |
| 2/1/2021 | Updated LDCT section to note the replacement of HCPCS code G0297 with new HCPCS code 70271. Corrected language in PAR Auth section to better correlate with information found on the Provider Fee Schedule | HCPF |
| 6/28/2021 | Updated LDCT Lung Cancer Screening section with latest guidance from USPSTF | HCPF |
| 7/21/2021 | Removed references to eQSuites, updated URLs for PAR | HCPF |
| 5/11/2022 | Updated lung cancer screening to refer to USPSTF recommendations. | HCPF |
| 7/1/2022 | Added the Unlisted Procedure Code subsection. | HCPF |
| 3/27/2023 | Updated AWS URL Links | HCPF |
| 8/24/2023 | Removed the Copay Language, Updated Field #17 on the claim reference table to required, Added the Ordering, Prescribing, Referring (OPR) Provider Policy | HCPF |
| 3/20/2024 | Removed CPT 75571 as a non-covered service. | HCPF |
| 9/3/2024 | Clarified podiatrist as a provider type that can order Radiology/Imaging Services. | HCPF |