Obstetrical Care Billing Manual
- Presumptive Eligibility (PE)
- Diagnosis Coding
- Billing for Obstetrical (OB) Care
- Global Obstetrics Billing
- Partial Global Obstetric CPT codes - Labor and Delivery and Postpartum Care
- Exceptions to Global or Partial Global Billing Guidelines
- Prenatal Care Only
- Labor and Delivery (L&D) Only
- Postpartum Care Only
- Prenatal Care and Delivery
- Early "Interim" Claim Submission for Prenatal Care and Delivery Services
- Global, Partial/Bundled and Individual Service Procedure Codes
- Services Not Included In Global Reimbursement
- Separate Procedures
- Special Provider Considerations
- Billing for Obstetrical (OB) Care
- Freestanding Birth Centers
- Fetal Anomalies Incompatible with Life Outside the Womb
- Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
- CMS 1500 Paper Claim Reference Table
- Billing Information
- Gender-Specific Procedures
- Timely Filing
- Obstetrical Care Revision Log
Return to Billing Manuals Web Page
Presumptive Eligibility (PE)
Presumptive Eligibility (PE) provides medical assistance benefits to low-income pregnant women and their children prior to receiving approval for full Health First Colorado (Colorado's Medicaid program) benefits. This program improves benefit accessibility for pregnant women through the process known as PE.
PE allows a woman temporary Health First Colorado coverage for 60 days. PE members receive a PE card that identifies them as eligible for ambulatory medical services. Inpatient hospital (e.g., delivery) services are not a PE benefit. After the full eligibility determination process, Health First Colorado eligible members receive a Medical Identification Card (MIC). Refer to the General Information Manual for more information on presumptive eligibility.
Diagnosis Coding
Health First Colorado recognizes the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-10-CM) diagnostic coding reference. The following diagnoses are for reference only. Refer to the ICD-10-CM for a full list of diagnosis codes. When required, use additional digits as indicated.
| Diagnosis Code | Description | Diagnosis Code | Description |
|---|---|---|---|
| Z32.00-Z32.02 | Encounter for pregnancy test | O00.0-O00.9 | Ectopic pregnancies |
| Z34.00-Z34.93 | Encounter for supervision of normal pregnancy | O01.0-O02.0 | Hydatidiform mole and other abnormal products of conception |
| O09.00-O09.93 | Supervision of high-risk pregnancy | O02.1 | Missed abortion (incomplete miscarriage) |
| O30.00-O30.93 | Multiple gestation | O03.0-O03.9 | Spontaneous abortion (miscarriage) |
| Z37.0 - Z37.9 | Outcome of delivery | Z39.0 - Z39.2 | Encounter for care and examination of mother immediately after delivery |
Billing for Obstetrical (OB) Care
Health First Colorado uses global obstetric codes for professional services provided during the perinatal period, including prenatal care, labor and delivery, and postpartum care. Pregnancies, excluding high-risk pregnancies, are reimbursed through a global payment rate. There are certain circumstances where providers may bill partial payment.
Global Obstetrics Billing
The global obstetrics (OB) code must be billed whenever one (1) practitioner or practitioners of the same group provide all three (3) components of the member's obstetrical care, including prenatal care (four [4] or more visits), labor and delivery and postpartum care. The number of prenatal visits may vary from member to member. However, if more than four (4) prenatal visits, labor and delivery and postpartum care are provided, ALL pregnancy-related visits (excluding inpatient hospital visits for complications of pregnancy) must be billed under the global OB code.
The date of delivery must be reported when billing these global OB codes.
The complete global OB Current Procedural Terminology (CPT) codes are identified as:
- 59400
- 59510
- 59610
- 59618
Partial Global Obstetric CPT codes - Labor and Delivery and Postpartum Care
Partial Global OB billing applies when a single provider or group practice bills only for two (2) components of the global obstetric package:
- Labor and Delivery, and
- Postpartum care
These codes do not include the prenatal care component (which requires at least 4 prenatal visits)
If the provider did not perform prenatal care but did perform the delivery and postpartum care, bill the appropriate partial Global OB code as shown below:
| Service Type | CPT Code | F Code | Notes |
|---|---|---|---|
| Vaginal delivery including postpartum care | 59410 | 0503F | Use 0503F to identify the initial date of service (DOS) for postpartum care. |
| Cesarean (C-section) delivery including postpartum care | 59515 | 0503F | Use 0503F to identify the initial DOS for postpartum care. |
| Vaginal birth after cesarean (VBAC) including postpartum care | 59614 | 0503F | Use 0503F to identify the initial DOS for postpartum care. |
| C-section after attempted VBAC including postpartum care | 59622 | 0503F | Use 0503F to identify the initial DOS for postpartum care. |
Exceptions to Global or Partial Global Billing Guidelines
The following examples are additional situations where itemization of OB services may be applicable.
Physicians from different group practice (non-affiliated practitioners) may provide and bill for individual components that are generally included in global or partial global OB billing when:
- The member transfers into or out of a physician or affiliated group practice and services provided do not meet the complete global or partial global OB service criteria.
- The member is referred to another non-group physician during their pregnancy.
- The member has the delivery performed by another physician or other health care professional not associated with their regular physician or affiliated group practice.
- The member terminates or miscarries their pregnancy.
- The member changes insurers during their pregnancy.
Prenatal Care Only
Prenatal care only codes should be billed when the practitioner or practitioners of the same affiliated provider group will NOT be performing all three (3) components of global OB care. Only one (1) prenatal care code is allowed to be billed per pregnancy.
- When fewer than four (4) prenatal visits are performed, bill the appropriate E/M codes for the visits. The appropriate E&M visit code must be billed with the TH modifier added to indicate that the visit is pregnancy-related, but outside of the OB global billing code.
- For four (4)-six (6) prenatal visits, bill CPT code 59425 with the appropriate 0500F or 0501F code identifying the initial date of service (DOS).
- For seven (7) or more prenatal visits, bill CPT code 59426 with appropriate 0500F or 0501F identifying the initial DOS.
The DOS used for billing the prenatal CPT code must be the same DOS reported for the first prenatal visit which is identified by the appropriate Category II CPT “F” code.
Labor and Delivery (L&D) Only
Delivery begins on the date of initial hospitalization for delivery and extends through the date on which the member is released from the hospital. Hospital care related to the delivery is considered part of the delivery charge and is NOT considered part of postpartum care.
- For vaginal delivery only, bill CPT code 59409.
- For C-section delivery only, bill CPT code 59514.
- For vaginal birth after C-section (VBAC), bill code 59612.
- For C-section after attempted VBAC delivery only, bill code 59620.
Postpartum Care Only
Postpartum care begins after the patient is discharged from the hospital stay for delivery and extends throughout the postpartum period. Health First Colorado defines "postpartum period" as 12 months after the pregnancy ends (i.e., through the end of the month in which that 12-month period ends). This 12-month extension became effective July 1, 2022. This extension ensures continuous coverage during that 12-month postpartum period, regardless of changes in income or household (unless the member voluntarily opts out, leaves the state, or eligibility was determined incorrectly). To qualify for the extended 12-month postpartum coverage, the member must have been enrolled in Health First Colorado/Child Health Plan Plus (CHP+) in the pregnancy eligibility category.
- For postpartum care only, bill code 59430 with the appropriate 0503F, identifying the initial DOS.
Prenatal Care and Delivery
There is not a comprehensive CPT code that describes prenatal care and includes delivery. Therefore, when prenatal care and delivery are performed, the provider must bill the appropriate prenatal code with either 0500F or 0501F CPT code and the appropriate delivery-only code. Prenatal and delivery codes should only be billed if postpartum care was NOT provided. Hospital care related to the delivery is considered part of the delivery charge and is NOT considered part of postpartum care.
Early "Interim" Claim Submission for Prenatal Care and Delivery Services
Providers may submit an interim claim for incomplete global OB service payments when Only prenatal and labor and delivery services have been rendered. If a postpartum visit is subsequently provided, the provider must void the interim OB claim and submit a new claim using the appropriate global codes, which includes prenatal, labor and delivery and postpartum services. This claim submission should ONLY be billed after the post-partum visit has been provided. The global OB codes should NOT be billed until the postpartum visit has been provided.
Individual OB service billing refers to maternity care services/components that are not combined and managed by a single provider or group of affiliated practitioners.
Providers must use the appropriate individual OB codes for prenatal-only, postpartum-only, and/or labor and delivery only services when the Global or Partial Global OB service codes are not applicable for use.
Global, Partial/Bundled and Individual Service Procedure Codes
| Complete Global OB Code (prenatal, labor and delivery, and postpartum care) | Units | Prior Authorization Required? |
|---|---|---|
| 59400 (vaginal delivery) 0500F or 0501F with initiating prenatal DOS mandatory with submission of complete global code on claim, 0503F with initiating postpartum DOS mandatory with submission of complete global code on claim. | 1 | No |
| 59510 (C-Section delivery) 0500F or 0501F with initiating prenatal DOS mandatory with submission of complete global code on claim, 0503F with initiating postpartum DOS mandatory with submission of complete global code on claim. | 1 | No |
| 59610 (VBAC- vaginal) 0500F or 0501F with initiating prenatal DOS mandatory with submission of complete global code on claim, 0503F with initiating postpartum DOS mandatory with submission of complete global code on claim. | 1 | No |
| 59618 (VBAC- C-section) 0500F or 0501F with initiating prenatal DOS mandatory with submission of complete global code on claim, 0503F with initiating postpartum DOS mandatory with submission of complete global code on claim. | 1 | No |
| Partial Global OB Codes (Labor and Delivery and Postpartum Care only) | Units | Prior Authorization Request Required? |
|---|---|---|
| 59410 (Vaginal delivery and postpartum care) 0503F with initiating postpartum DOS mandatory with submission of partial global codes | 1 | No |
| 59515 (C-section and postpartum care only) 0503F with initiating postpartum DOS mandatory with submission of partial global codes | 1 | No |
| 59612 (VBAC delivery including postpartum care) 0503F with initiating postpartum DOS mandatory with submission of partial global codes | 1 | No |
| Prenatal Care Only | Visit threshold | Prior Authorization required? |
|---|---|---|
| 59425 Please ensure the initiating 0500F or 0501F is added with the correct DOS when billing this code | 4-6 prenatal visits | No |
| 59426 Please ensure the initiating 0500F or 0501F is added with the correct DOS when billing this code | 7 or more prenatal visits | No |
| Postpartum Care Only | Visit Threshold | Prior Authorization Required? |
|---|---|---|
| 59430 Ensure the initiating 0503F code is added with the correct DOS when billing the 59430 code | 1 | No |
Refer to the information below for the correct billing of multiple infants:
Billing for Multiple Infants:
To avoid claim denials and National Correct Coding Initiative (NCCI) edits on claims involving the delivery of multiple infants, additional information is required.
For Cesarean Deliveries: Bill only one CPT code and only one unit for the complete cesarean delivery, regardless of the number of infants delivered. Whether reporting for a global delivery (59510 or 59618), delivery only (59514 or 59620), or delivery including post-partum care (59515 or 59622), only one cesarean procedure (with one incision) is being performed. Use the most accurate/complete procedure code that describes the prenatal care, delivery history, current delivery type, and any postpartum care provided for the current pregnancy.
For Vaginal Deliveries: bill multiple infants using the guidelines outlined below:
For the first infant (Baby A), use the most accurate and complete vaginal delivery diagnostic and procedure code. Choose the procedure code that best describes all services provided and considers delivery history, current delivery type, prenatal care, and postpartum care.
Bill one unit of service for Baby A.
For the additional infant (Baby B), bill this infant on a separate line using one (1) of the following delivery only codes: 59409 or 59612. Choose the code associated with the delivery history and delivery type you used for Baby A.
Include modifier '59' in the first position for Baby B. Use the delivery date as the date of service.
For Vaginal Deliveries followed by a Cesarean Delivery:
For a Vaginal Delivery of the first infant (Baby A): Use either code 59409 or 59612 for Baby A. Include modifier '59' in the first position for Baby A. Bill only one (1) unit of service.
For Cesarean Delivery of the second infant (Baby B):
Use the most accurate/complete global cesarean procedure code that describes the antenatal and/or postpartum care or delivery only care provided for the current pregnancy. Use one of the following codes for Baby B: global delivery, delivery only, or delivery including post-partum care. Choose the Cesarean code associated with the same delivery history you used for Baby A: (59510 or 59515 with 59409) OR (59618, 59620, or 59622 with 59612). Bill one unit of service for Baby B. Each infant should be listed on a separate line. Use the delivery date as the date of service.
NCCI Edit Requirements: A second modifier 'XU' is required for NCCI edits when the following code combinations are billed: 59410 with 59409, 59610 with 59612, or 59614 with 59612.
NCCI edits do not allow procedure code 59514 to be combined or billed with codes: 59400, 59409, or 50410.
Delivery Procedure Codes:
59400, 59410, 59409, 59610, 59614, 59612, 59510, 59515, 59514, 59618, 59622, 59620.
Services Not Included in Global Reimbursement
- Unusual circumstances
- Conditions that are unrelated to the pregnancy or delivery
- Complications of pregnancy
- Certain adjunctive services
- Medical/Surgical services unrelated to the pregnancy
- Depression screens for pregnant and postpartum women
Separate Procedures
These services should be billed separately from (in addition to) global obstetrical care charges.
| Service | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prenatal testing | Bill only for the testing or the portion of the testing performed by the provider Use modifier -TC for technical component services only Use modifier - 26 for professional services only Use no modifier if professional and technical testing services are performed by the same provider | ||||||||||||||||||||||||||||||||||||||||||||||
| Invasive or non-invasive prenatal testing, including ultrasound | Health First Colorado covers a maximum of two (2) ultrasounds for an uncomplicated or low-risk pregnancy. If the member's medical condition requires additional ultrasonography, medical records must be documented. | ||||||||||||||||||||||||||||||||||||||||||||||
| Clinical laboratory testing | Providers must be CLIA certified. Tests performed by an outside lab must be billed by the lab. A prenatal obstetric panel must include tests for a complete blood count with differential, a hepatitis B surface antigen, a rubella antibody, syphilis and HIV testing, a red blood cell antibody screen, ABO blood typing, and Rh typing. Syphilis testing is a Colorado statutory requirement for the first trimester or at the first OB visit (testing independently or as included in the prenatal obstetric panel). Nationwide and in CO, increased cases of syphilis and congenital syphilis have been reported so additional syphilis monitoring and/or testing for pregnant individuals at higher risk are needed. Effective January 15, 2025, CDPHE revised and added Regulation 12 to their Board of Health Rule 6 CCR 1009-1 (Epidemic & Communicable Disease Control) to address the increased need to expand access and to increase frequency of syphilis testing during pregnancy. Healthcare facilities and medical providers that evaluate and treat pregnant individuals must offer syphilis testing to all pregnant members unless testing has already occurred which meets the needed testing requirement or if the member declines testing. Syphilis testing must be offered:
These new testing requirements must be followed These new testing requirements must be followed as per 6 CCR 1009-1 or until other state guidelines or directives supersede this Rule. For the most recent CO syphilis statistics, data is available through the CDPHE website. Laboratory testing other than routine chemical urinalysis and finger stick hematocrit. Pap smear during pregnancy and a second pap smear during the postpartum period. (This is in addition to the routine annual pap smear.) Note: Lab tests must include the emergency indicator for all Emergency Medicaid Services Members. Refer to the Emergency Medicaid Services Billing Manual for additional information. | ||||||||||||||||||||||||||||||||||||||||||||||
| Adjunctive services | For example, Tracheoplasty/trachelorrhaphy, etc. | ||||||||||||||||||||||||||||||||||||||||||||||
| Initial antepartum visit | Use CPT E and M codes 99202-99215 for initial visit. Initial visit may involve additional time and attention.
| ||||||||||||||||||||||||||||||||||||||||||||||
| Medical or surgical complications | Bill on an ongoing basis using the appropriate procedure code(s). The diagnosis code must identify the complication or condition. | ||||||||||||||||||||||||||||||||||||||||||||||
| Sterilization following Delivery | A voluntary sterilization, performed at the time of a vaginal or cesarean delivery, is available and requires accurate completion and attachment of the federal compliance informed consent documentation (Med 178 Form), located on the Provider Forms web page, under the sterilization Consent Forms drop-down menu. The Sterilization Consent form must be signed by the client at least 30 days prior to the estimated date of delivery. For additional sterilization information, see the Reproductive Health Billing Manual, under Family Planning/Sterilization. | ||||||||||||||||||||||||||||||||||||||||||||||
| Premature Delivery – Sterilization Consent | A pregnant individual may consent to sterilization at the time of a premature delivery if at least 72 hours have passed since she gave informed consent for the sterilization and the consent was obtained at least 30 days prior to the expected date of delivery. For additional sterilization information, see the Reproductive Health Billing Manual, under Family Planning/Sterilization. | ||||||||||||||||||||||||||||||||||||||||||||||
| Conditions unrelated to pregnancy | Medical or surgical services for conditions that are not related to pregnancy should be billed separately. Identify the condition requiring additional care. Services are subject to PCP referral. | ||||||||||||||||||||||||||||||||||||||||||||||
| Anesthesia | The delivery fee includes local, pudendal, and paracervical blocks by the delivering practitioner. If the delivering practitioner begins block anesthesia for a vaginal delivery that subsequently requires a cesarean, separate charges may be submitted using the appropriate block code. Anesthesia by a practitioner, other than the practitioner delivering the infant(s), must be billed by the provider who renders the service. | ||||||||||||||||||||||||||||||||||||||||||||||
| Epidural anesthesia | Epidural anesthesia by a provider other than the delivering practitioner is a covered benefit. Document member contact time on the claim. Paper claims for more than 120 minutes (eight (8) or more time units) of direct member contact epidural time require an attached copy of the anesthesia record. Electronic claims may be submitted (no attachments) but documents verifying extended direct member contact must be maintained and produced upon request. | ||||||||||||||||||||||||||||||||||||||||||||||
| Assistant surgeon at cesarean delivery | Modifier - 80 identifies assistant surgeon services. A family practitioner or certified nurse-midwife may bill as assistant surgeon at cesarean. Physician assistants, surgical assistants, and nurse practitioners may not bill as assistant surgeon. An assistant surgeon is not allowed on vaginal deliveries. | ||||||||||||||||||||||||||||||||||||||||||||||
| Treatment for high-risk pregnant women | Women who would be high risk given physical health, psychosocial history, and current life stressors may be eligible for involvement in the Prenatal Plus (PN+) Program, a Health First Colorado benefit that provides a care team for women at higher risk of adverse birth outcomes. The service package includes a care coordinator, a dietitian, and a mental health professional. Visit the Prenatal Plus web page to find a provider near you if you think the mother would be eligible. | ||||||||||||||||||||||||||||||||||||||||||||||
| Treatment for substance-abusing pregnant women | Substance abusing pregnant women may be eligible for involvement in Special Connections, a Health First Colorado-funded program for substance abuse treatment. The service package includes Risk assessment, case management, individual counseling, group counseling and health maintenance. Substance abusing pregnant women can refer themselves to Special Connections or be referred by a provider. | ||||||||||||||||||||||||||||||||||||||||||||||
| Emergency Medicaid Services Billing for Labor and Delivery and Reproductive Healthcare | Refer to the Emergency Medicaid Services Billing Manual for information about billing for labor and delivery and reproductive healthcare services. | ||||||||||||||||||||||||||||||||||||||||||||||
| Immediate Post-Partum Long-Acting Reversible Contraceptives (IPP-LARCs) | Effective January 1, 2020, IPP-LARC devices inserted in a DRG Hospital may be reimbursed at the fee schedule rate or the amount billed, whichever is less. Refer to the Inpatient/Outpatient (IP/OP) Billing Manual for additional IPP-LARC billing information. | ||||||||||||||||||||||||||||||||||||||||||||||
| Inpatient Hospital Billing for Birthing Parent and Newborn | Refer to the Inpatient/Outpatient (IP/OP) Billing Manual. | ||||||||||||||||||||||||||||||||||||||||||||||
| Newborn Hearing and Metabolic Screenings | Costs associated with the Newborn Hearing Screening and the initial Newborn Metabolic Screening are included in the delivery DRG calculation or the birthing center facility payment. They may not be billed separately. Refer to the Inpatient/Outpatient (IP/OP) Billing Manual. Current Procedural Terminology (CPT)/ Healthcare Common Procedure Coding System (HCPCS) codes for the Newborn Hearing Screening cannot be billed for dates on or during the date span of the delivery stay. Refer to the Audiology Benefit Billing and Policy Billing Manual or the Laboratory Services Billing Manual for more information. | ||||||||||||||||||||||||||||||||||||||||||||||
| Examination and evaluation of the healthy newborn | EPSDT Periodicity Guidelines recommend initial newborn screenings at 3-5 days and 2 weeks. | ||||||||||||||||||||||||||||||||||||||||||||||
| Routine or ritual circumcision | As of July 1, 2017, circumcision is available as a benefit of the program. The following CPT codes are being reimbursed 54150, 54160 or 54161. This change does not affect the CHP+ Program. | ||||||||||||||||||||||||||||||||||||||||||||||
| Services provided at place of service (POS) 03 - school | Effective May 3, 2024, place of service 03 is an allowed place of service for all fee-for-service benefits. In order for community providers to bill fee-for-service to children in a school setting, the provider must follow school district policy. Please reference the Community Providers in a School Setting Policy memo. |
Special Provider Considerations
| Provider | Service |
|---|---|
| Enrolled Certified Nurse Midwives (CNM) | May provide OB care in accordance with the Colorado Medical Practice Act. Certified Nurse Midwives submit claims in the same manner as physicians. Certified nurse-midwives may act as assistant surgeon at cesarean deliveries. |
| Enrolled Certified Midwives (CM) | May provide OB care in accordance with the Colorado Medical Practice Act. Certified Midwives submit claims in the same manner as physicians and CNMs. Certified Midwives may act as assistant surgeon at cesarean deliveries. |
| Direct-Entry or Certified Professional Midwives (DEM / CPM) | May render low-risk OB care in Health First Colorado-enrolled Free-Standing Birth Centers, as identified and in accordance with the Colorado Department of Regulatory Agency’s (DORA) Rule and Statutory Guidelines: 4 CCR 739-1 and C.R.S.12-225-101 through 12-225-113. DEM/CPMs may provide home deliveries services when enrolled and covered within compliance with the Maternity Rule (10 CCR 2505-10 8.732) |
| Certified Family Nurse Practitioners or Certified Pediatric Nurse Practitioners | Must be specifically identified and enrolled according to Health First Colorado's provider enrollment policy. These non-physician practitioners do not require direct and personal supervision of an on-premises, licensed, Health First Colorado-enrolled physician and may receive direct reimbursement. |
| Physician assistants other nurse practitioners | These providers do not qualify for direct reimbursement. The provider number of the supervising physician must appear in the supervising provider field on the claim record. Physician assistants, surgical assistants, and nurse practitioners may not serve as assistant surgeons. |
Freestanding Birth Centers
A Birthing Center is a licensed free-standing healthcare facility (not a hospital, nor attached to or located within a hospital) where care providers, including licensed Certified Nurse Midwives (CNMs) and physician (MDs/DOs) identified in Rule (6 CCR 1011-1 Chapter 22) as clinical staff, provide family-centered, culturally competent and comprehensive prenatal, labor and delivery and postpartum care to healthy low-risk pregnant women and their newborns. Birth Center Health Care Facilities are licensed through the Colorado Department of Public Health & Environment (CDPHE) and regulated through statutory authority identified in sections 25-1.5-103 & 25-3-100.5, et seq., C.R.S. and C.R.S.12-30-118.
Provider Enrollment
Reimbursement for birth centers for services rendered to Health First Colorado-eligible members is only available to licensed (through CDPHE) freestanding birth centers (FSBC) that enroll with Health First Colorado as a Health First Colorado provider with a birth center specialty designation (58/116 = provider type/specialty type). Include a copy of your CDPHE license with your Health First Colorado provider enrollment application and request the specialty designation for FSBCs. Practitioners, such as certified nurse midwives (CNM), certified Midwives (CM ) or Direct-Entry/Certified Professional midwives (DEM/CPM) providing services at birth centers must also be enrolled as Health First Colorado providers and affiliated with the birth center under which claims are submitted.
Billing Requirements
In addition to the submission of claims for antepartum, delivery, and postpartum care (following global OB billing guidelines), freestanding birth centers can also submit claims for a birth center facility payment for that delivery and when a member must be transferred to a hospital.
| Description | Code(s) | Modifier - first position |
| Birth center payment | 59899 | HD |
The modifier included in the tables above and below are required for the claim to pay correctly. If 'HD' (women's program/service) is not included in the first position, the claim will pay incorrectly.
Occasionally, members are unable to deliver at the birth center and need to be transferred to a hospital. In these cases, a reduced birth center facility payment is available, as is reimbursement for time spent with the member.
| Description | Code(s) | Modifier - first position | Modifier - second position |
| Transfer payment: Payment for costs incurred prior to transporting a member to a hospital | 59899 | HD | 52 |
In addition to the payment made for members who transfer, claims can be submitted for the time a midwife spends with the member prior to her transfer and for antepartum care.
| Code(s) | Reimbursement |
| 99215 | Payment is based upon Health First Colorado's fee schedule. |
| 99215 + 99354 | Payment is based upon Health First Colorado's fee schedule. |
| 99215 + 99354 + 99355 (1 unit of 99355 per each additional 30 minutes) | Payment is based upon Health First Colorado's fee schedule. |
Fetal Anomalies Incompatible with Life Outside the Womb
Therapeutic abortions performed due to fetal anomalies incompatible with life outside the womb are not a Health First Colorado benefit.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
8.280.4.E Other EPSDT Benefits
Other health care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Section 1905(a) of the Social Security Act are a covered benefit under EPSDT when medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, regardless of whether such goods and services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a good or service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one or more Activities of Daily Living; and meets the criteria set forth at Section 8.076.1.8.b - g.
- The service provides a safe environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly.
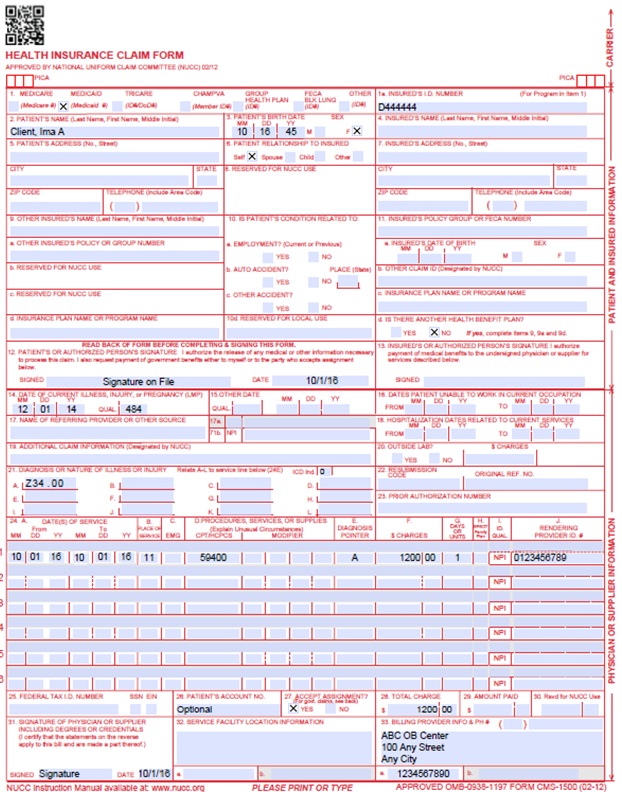
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 013125 for January 31, 2025. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 013125 for January 31, 2025. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 013125 for January 31, 2025. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | Transportation When applicable, enter the word "TRANSPORT CERT" to certify that you have a transportation certificate or trip sheet on file for this service. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left-hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | CLIA When applicable, enter the word "CLIA" followed by the number. Prior Authorization Enter the six (6)-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
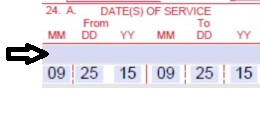
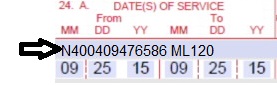
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 013125 for January 31, 2025.
or
Span dates of service
Practitioner claims must be consecutive days.
Example: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. G7 – Termination of pregnancy resulting from rape, incest, or certified by physician as life-threatening. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado-covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Anesthesia Services Anesthesia time begins when the anesthetist begins member preparation for induction in the operating room or an equivalent area and ends when the anesthetist is no longer in constant attendance. No additional benefits or additional units are added for emergency conditions or the member's physical status. Codes that define units as inclusive numbers | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the National Provider Identifier (NPI) of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 013125 for January 31, 2025. Unacceptable signature alternatives: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type (PT) is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the PT is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
OB Claim Example
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Obstetrical Care Manual Revision Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manuals Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 1/2/2018 | Supplemental Qualifier addition - instructions for reporting an NDC | DXC |
| 6/27/2018 | Edited all, addition of more global OB billing specifics and slight rearrangement of information regarding Other reproductive health care services. | HCPF |
| 6/28/2018 | Removal of duplicated and superfluous verbiage, restoring links | HCPF |
| 7/2/2018 | Minor style and consistency edits | DXC |
| 7/9/2018 | Corrected "permissible" | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 1/15/2020 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 4/13/2021 | Changes have been made due to required claim system changes (ClaimsXTN). Additional billing information, such as billing for Immediate post-partum LARCs and separation of maternal & infant billing has been added. | HCPF |
| 8/24/2022 | 2021 Legislative bill implementations have required billing manual and system changes for maternal postpartum care, family planning services and abortion services | HCPF |
| 1/12/2023 | Restored Hysterectomy section | HCPF |
| 3/31/2023 | Added OB billing change instructions for required reporting of prenatal and postpartum visits. Provided clarifying instructions for sterilizations provided to new family planning eligibility groups that are also enrolled for labor and delivery services and added some clarifying edits. | HCPF |
| 9/15/2023 | Cleaned up alignment in tables and verbiage regarding in-hospital billing for mother and newborn | HCPF |
| 4/30/2024 | Modified/clarified billing for postpartum & antepartum services & DOS, added Direct-entry/Certified Professional Midwife (DEM/CPM) Provider type with info and link to related DORA statute and Free-standing birth Center services (with CDPHE’s statutory link) and added CDPHE’s Public Health Order information RE: syphilis testing/treatment during pregnancy. | HCPF |
| 7/31/2024 | Added Place of Service (POS) 03 | HCPF |
| 9/10/2024 | Updates to sections of the Separate Procedures table (Emergency Medicaid Services, Clinical Laboratory Testing, Immediate Post-Partum Long-Acting Reversible Contraceptives (IPP-LARCs), Inpatient Hospital Billing for Birthing Parent and Newborn, Newborn Hearing and Metabolic Screenings). Removed outdated language from CMS 1500 Paper Claims Reference Table, box 24G. Added Gender-Specific Procedures section. | HCPF |
| 02/05/2025 | Revision of Global Obstetric Billing Guidance | HCPF |
| 10/01/2025 | Addition of Certified Midwives to the Special Provider Considerations section and addition of home birth guidance for CPMs and DEMs | HCPF |
| 1/05/2026 | Separation of Original OB Billing Manual OB information from Other Reproductive Health Care related information. Creation of two Separate billing manuals 1) for OB services & 2) for Reproductive Health Care Related services | HCPF |