Laboratory Services Billing Manual
- Laboratory Services
- General Billing Information
- Unlisted Procedure Codes
- General Prior Authorization Requirements
- Laboratory Prior Authorized Procedure Codes
- Clinical Laboratory Improvement Amendments (CLIA) Claims
- Handling, Collection and Conveyance Charges
- Papanicolaou (Pap) Smears
- Drug Testing Unit Limitations and Documentation Requirements
- Definitive Drug Testing for Addiction Treatment
- Newborn Metabolic Screening
- BRCA Screening and Testing
- Prenatal Testing
- General Requirements
- Procedure/HCPCS Codes Overview
- Procedure Codes
- Laboratory Prior Authorized Procedure Codes
- CMS 1500 Paper Claim Reference Table
- Timely Filing
- Laboratory Services Revisions Log
Return to Billing Manuals Web Page
Laboratory Services
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid program) provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
A certified clinical laboratory means a provider who possesses a certificate of waiver or a certificate of registration from the Centers for Medicare & Medicaid Services (CMS) or its designated agency as meeting CMS guidelines and whose personnel and director are qualified to perform laboratory services.
An independent laboratory means a certified clinical laboratory that performs diagnostic tests and is independent both of the attending or consulting physician's office and of a hospital.
All clinical laboratory providers must furnish their Clinical Laboratory Improvement Amendment (CLIA) certification numbers to the Health First Colorado fiscal agent at the time of enrollment.
Medically necessary, physician-ordered laboratory services are a benefit of Health First Colorado.
Providers should refer to the Code of Colorado Regulations, Program Rules (10 CCR 2505-10), for specific information when providing laboratory services.
Important: Laboratory services for Emergency Medicaid (EMS) clients must include the emergency indicator on the claim for the claim to be paid.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page for general billing information.
Ordering, Prescribing and Referring (OPR) Providers
Health First Colorado complies with Federal Medicaid Regulations in 42 CFR 455.410(b) which provide that Medicaid must require all ordering or referring physicians or other professionals providing services be enrolled as providers, and 42 CFR 455.440, which provides that Medicaid must require all claims for the payment of items and services that were ordered, prescribed and referred to include the National Provider Identifier (NPI) of the OPR physician or other professional.
Effective July 1, 2022, the Department of Health Care Policy & Financing (the Department) will enforce the federal requirement 42 CFR § 455.440 that claims for all Laboratory services, rendered by any type of provider, contain the NPI of the provider who ordered the services, and that the NPI is actively enrolled with Health First Colorado. The ordering NPI may be that of the qualified provider overseeing the member’s care, for example as is the case with maternity services.
Providers are instructed to place the NPI of the ordering provider into the following locations for claim submission:
Professional Claims
- Paper claims use field 17b
- Electronic submissions use loop 2420e with qualifier DK
Laboratory services can be ordered by either a physician, physician assistant, osteopath, certified nurse midwife, advanced practice nurse, certified registered nurse, optometrist, pharmacist, anesthetist or podiatrist. The ordering provider must also be actively enrolled with Health First Colorado. If these conditions are not met the claim will be denied.
Visit the OPR web page for further information on this project.
Unlisted Procedure Codes
Unlisted laboratory procedure codes are used when there is no CPT or HCPCS code that accurately identifies the services performed. Unlisted procedure codes will be priced by a clinical reviewer with the Department's fiscal agent.
Claims with unlisted codes must include as attachments the operating report from the procedure and the Unlisted Procedure Code Form, located on the Provider Forms web page under the Claim Forms and Attachments drop-down. All lines on the Unlisted Procedure Code Form must be completed. The Department will deny claims lacking the required attachments. Claims denied for incomplete information will have to be resubmitted with the correct information for reimbursement.
General Prior Authorization Requirements
Refer to the General Provider Information Manual located on the Billing Manual web page for information about prior authorization requirements. Visit the ColoradoPAR web page for more information or visit the Provider Contacts web page for contact information.
Laboratory Prior Authorized Procedure Codes
Some laboratory procedure codes require a Prior Authorization Request (PAR). Please reference the current Health First Colorado Fee Schedule for PAR requirements, definitive coverage of specific procedure codes, and rates.
Clinical Laboratory Improvement Amendments (CLIA) Claims
Laboratory providers submitting procedures covered by CLIA must have a CLIA number of the laboratory where the procedure was done on the claim or claim line. Pass-through billing is not allowed per the Laboratory and X-ray rule found at 10 CCR 2505-10 8.660.
- Providers billing on the 837P format should refer to the updated 837P Companion Guide located on the EDI Support web page. Providers billing on the 837P format and billing agents should update their billing systems for 837P transactions.
- Providers billing an 837P through the Health First Colorado Online Portal (Online Portal) are able to enter CLIA numbers on the Detail Line Item tab (claim line).
- Providers billing on the CMS 1500 paper claim form should enter their valid CLIA number in the REMARKS field (# 23). Enter "CLIA" before the CLIA number.
Note: Only one (1) CLIA number can be included on each paper claim form. It is applied to all CLIA covered procedures on the claim. Procedures covered by different CLIA numbers need to be submitted on separate claims. Enter the CLIA number in the REMARKS field only.
The Tax ID (TID) on record with the Centers for Medicare & Medicaid Services (CMS) for the CLIA number must correspond to the TID on record with the Department. Questions regarding claims processing or responses should be directed to Gainwell Technologies.
Handling, Collection and Conveyance Charges
Specimen collection (including venipuncture) is considered to be an integral part of the laboratory testing procedure when performed by a laboratory and is generally not reimbursable as a separate or additional charge.
Transfer of a specimen from one clinical laboratory to another is a benefit only if the first laboratory's equipment is not functioning or the laboratory is not certified to perform the ordered tests. Modifier -KX used with procedure code 99001 verifies that the lab's equipment is not functioning or that the laboratory is not certified to perform the ordered test.
Specimen collection, handling, and conveyance from the member's home, a nursing facility, or a facility other than the physician's office or place of service is a benefit only if the member is homebound, bedfast, or otherwise non-ambulatory and the specimen cannot reasonably be conveyed by mail. A physician's statement explaining the circumstances and medical necessity is required.
Each laboratory will be reimbursed only for those tests performed in the specialties or subspecialties for which it is certified.
Papanicolaou (Pap) Smears
Health First Colorado allows one (1) pap smear screening/examination per 12-month period in women under 40 years of age. Benefit for more than one (1) pap smear in a 12-month period is allowed for women ages 40 and over, women with a history of diethylstilbestrol exposure in utero, women with malignancy of the cervix, vagina, uterus, fallopian tubes or ovaries, women with cervical polyps, cervicitis, neoplastic disease of the pelvic organs, vaginal discharge or bleeding of unknown origin, postmenopausal bleeding, or vaginitis, or if the physician determines that more frequent testing is needed and is medically necessary. Claims will deny if the diagnosis code entered on the claim does not support the testing frequency.
Drug Testing Unit Limitations and Documentation Requirements
Current Procedural Terminology (CPT) codes 80305, 80306 and 80307 have a unit limit of four (4) per month per client for each code. This unit limit applies to all provider types.
As of August 1, 2021, HCPCS G0480-G0483 should be used when billing for substance-specific confirmatory tests. CPT codes 80320-80377 were closed as of July 31, 2021.
Definitive Drug Testing Annual Limits
Effective October 10, 2025 through June 30, 2026
Adult members are limited to 16 combined units of service for definitive drug testing HCPCS codes G0480, G0481, G0482, and G0483 during the period from October 10, 2025 through June 30, 2026, based on date of service.
Claim Processing:
- Claim edit EOB 1067 will deny claims submitted on or after October 10, 2025, when the member exceeds the 16-unit limit.
- The Department will review and adjust denied claims during this period to ensure proper system operation.
Exception: Members aged 0–20 may receive additional testing with Prior Authorization when clinically appropriate.
Effective July 1, 2026
Adult members are limited to 12 combined units per State Fiscal Year (SFY) (July 1–June 30) for definitive drug testing HCPCS codes G0480, G0481, G0482, and G0483, based on date of service.
Claim Processing:
- Claim edit EOB 2364 will count only services provided on or after July 1, 2026 toward the 12-unit SFY limit.
Exception: Members aged 0–20 may receive additional testing with Prior Authorization when clinically appropriate.
Reference: 10 C.C.R. 2505-10, Section 8.660.3.D.
Note: The Medical Services Board (MSB) established a limit of 16 tests per SFY for adults effective October 10, 2025, then reduced this limit to 12 tests on December 12, 2025. Due to operational limitations of processing claims in accordance with a limitation change reducing covered tests from 16 to 12, the 12-test limit will be implemented beginning July 1, 2026. The 16-test limit will be in effect until June 30, 2026.
All documentation, including the order for the drug test, the clinical indication/medical necessity and the lab results must be maintained in the member’s medical record.
Definitive Drug Testing for Addiction Treatment
Purpose and Clinical Framework
Health First Colorado (Colorado’s Medicaid Program) recognizes clinical drug testing as an evidence-based component of the identification, diagnosis, treatment, and ongoing monitoring of substance use disorders (SUDs) and recovery. Drug testing is used to supplement, not replace, clinical assessment and patient self-report.
For addiction treatment settings, Health First Colorado references the nationally recognized standard of The American Society of Addiction Medicine (ASAM) Appropriate Use of Drug Testing in Clinical Addiction Medicine (2017) as the primary clinical reference in determining when definitive drug testing is medically necessary. These standards emphasize:
- Using drug testing as a therapeutic tool integrated into treatment planning and engagement
- Using “smarter” testing strategies (appropriate matrix, drug panel, and frequency based on the clinical question rather than routine, arbitrary patterns)
- Avoiding overuse such as very large untargeted panels, excessively frequent testing unrelated to detection windows, and routine confirmation of all results
Coverage of definitive drug testing is based on medical necessity which includes the required alignment with national standards (10 CCR 2505-10 8.076.1.8.b), evaluated in light of these national standards and the member’s individual clinical circumstances.
Definitions
Presumptive Drug Test - A qualitative test (typically immunoassay) that detects the presence or absence of a drug or drug class at a specified cutoff concentration. Presumptive tests are generally used for initial and ongoing assessment because they provide more rapid, but less specific, results.
Definitive Drug Test - A test performed with high-sensitivity and high-specificity methods (e.g. gas or liquid chromatography combined with mass spectrometry) that can identify specific drugs and/or metabolites and may quantify their concentration. Definitive tests are typically performed in a laboratory and are more costly than presumptive tests.
General Coverage Statement
For the purposes of this section, “addiction treatment” includes services delivered in outpatient, intensive outpatient/partial hospitalization, residential/inpatient, medically managed intensive inpatient, opioid treatment programs (OTPs), and office-based opioid treatment (OBOT) programs. Health First Colorado covers medically necessary definitive drug testing when:
- The member is being evaluated or treated for a known or suspected substance use disorder; and
- Testing is ordered by a licensed prescriber or other qualified practitioner within their scope of practice; and
- The test result is expected to directly influence clinical decision-making in accordance with ASAM’s appropriate recommendations (for example, treatment level or modality, or medication changes).
Coverage is contingent on documentation that the type of test, drug panel, and testing frequency are consistent with individualized clinical needs and with nationally recognized ASAM standards for appropriate use of drug testing in addiction treatment.
Indications for Definitive Drug Testing (Covered Uses)
Definitive testing is not a routine first-line test in addiction treatment. It is a targeted tool used when greater analytical specificity is necessary. Health First Colorado considers definitive testing medically necessary in addiction treatment when at least one (1) of the following indications is present:
- Disputed Presumptive Result
A member disputes a presumptive positive or presumptive negative result, and clarification will affect the treatment plan (for example, level of care, medication adjustment, or contingency management incentives). - Need to Identify a Specific Drug or Metabolite
The provider needs to distinguish between specific substances that presumptive testing cannot adequately differentiate (e.g. heroin vs. other opioids within an opiate class screen) and the result will guide clinical management. - High-Impact Clinical Decisions
The result will inform decisions with major clinical implications, such as:- Initiation, discontinuation, or significant change in pharmacotherapy (for example, medications for opioid use disorder)
- Transition between levels of care (e.g. outpatient to residential)
- Safety-critical determinations (for example, ability to safely receive take-home opioid agonist doses in an OTP)
- Clinical Indicators of Use Despite Negative Presumptive Test
The member demonstrates signs or symptoms strongly suggestive of recent substance use (e.g. intoxication or withdrawal) that conflict with a negative presumptive test and definitive testing is needed to clarify the discrepancy. - Monitoring Complex Pharmacotherapy or Diversion Risk
The test is used to monitor adherence to prescribed medications for addiction treatment (e.g. methadone, buprenorphine or naltrexone) or to evaluate possible diversion when presumptive methods are insufficient. - Clarifying Unexpected Results With Significant Treatment Impact
Definitive testing is needed to clarify unexplained or incongruent presumptive findings when results may lead to treatment intensification or additional safety measures. - Direct Ordering of Definitive Test When Precision Is Required
When substance use is already acknowledged by the member or otherwise expected and the provider requires specific analyte identification and/or quantification (e.g. to select an appropriate medication or evaluate relapse severity), it may be clinically appropriate to order a definitive test without a preceding presumptive test.
Frequency and Scheduling of Testing
- Clinical Tailoring
Frequency of both presumptive and definitive tests must be individualized based on:- Stage of treatment or recovery
- Level of care
- Member acuity and risk
- Expected detection windows of the drugs being tested
- Early Treatment / High-Acuity Period
Consistent with ASAM, members in early recovery should be tested more frequently (often at least weekly), using primarily presumptive tests, with definitive tests added only when clinically indicated as described in Indications for Definitive Drug Testing (Covered Uses). - Stable Recovery / Maintenance
As members stabilize in treatment or recovery, reduce test frequency to no less than monthly unless clearly justified by sustained stability and low risk. - Random, Unannounced Testing
When feasible, testing should be scheduled on a random, unannounced basis rather than fixed predictable interval to better detect use and support recovery. - Numerical Limitations
Health First Colorado limits the quantity of covered presumptive and definitive drug testing in accordance with the policies stated in Drug Testing Unit Limitations and Documentation Requirements.
Non-Covered Uses / Limitations
Definitive drug testing will not be considered medically necessary, and therefore not covered, when:
- Routine, Automatic Reflex on All Presumptive Positives or Negatives
Definitive confirmation of every presumptive positive or negative result, regardless of clinical relevance or member-reported use, is not supported by ASAM and is not covered. - Large, Untargeted Panels Without Clinical Justification
Routine use of broad “catch-all” definitive panels that are not tailored to the member’s drug history, prescribed medications, and local drug trends is considered inappropriate. Test panels must be targeted to clinically relevant substances. - Testing Unrelated to Treatment or Diagnosis of SUD
Testing ordered for employment, legal, forensic, or other non-clinical purposes is not covered. - Duplicate Testing
Repeating definitive testing on the same specimen without a documented need (e.g. to re-bill or use multiple laboratories) is not medically necessary. - Excessive Frequency Not Supported by Detection Windows
Testing frequency greatly exceeding what is required by the pharmacokinetics of the substances being monitored and the member’s clinical status may be considered overuse and is subject to denial or recoupment.
Provider Responsibilities and Documentation
To support medical necessity for definitive testing, the medical record must clearly document:
- Clinical Rationale
The clinical question being addressed and why a definitive test rather than presumptive alone is required, including reference to one or more indications listed in Indications for Definitive Drug Testing (Covered Uses). - Test Selection
The selected matrix and drug panel tied to the member’s substances of concern, prescribed medications and relevant local drug trends. - Testing Schedule
The frequency and timing of tests linked to stage of treatment, level of care and risk of use or relapse. - Integration With Treatment
How the results are used therapeutically (e.g. treatment plan changes, contingency management incentives or medication adjustments) rather than solely punitive responses. - Test Results and Interpretation
Results of presumptive and definitive tests, any communication with the laboratory/treatment provider and interpretation including consideration of potential cross-reactivity or tampering where relevant. - Member Communication and Consent
That the member was informed of the therapeutic purpose of drug testing and how results will be used, consistent with ASAM’s emphasis on using testing to support, and not undermine, the therapeutic alliance.
Newborn Metabolic Screening
Costs associated with Newborn Metabolic Screening (NMS) are included in the inpatient hospital diagnosis-related grouper (DRG) calculation and the birthing center facility payment and may not be billed separately by the hospital or birth center. Billing S3620 while receiving a DRG or facility payment for the delivery is duplicative.
S3620 may only be billed by providers, not reimbursed for the delivery, who submit a second-specimen screen and are charged for an initial-specimen screen by Colorado Department of Public Health & Environment (CDPHE) because the second specimen could not be linked to an initial-specimen. S3620 does not require a CLIA certification.
Because the NMS are performed by CDPHE's laboratory and not the provider collecting and submitting the specimen, unbundling the NMS and billing for the individual tests performed by CDPHE's laboratory is not allowed per the Laboratory and X-ray rule found at 10 CCR 2505-10 8.660.
BRCA Screening and Testing
Per the Women's Health Services rule found at 10 CCR 2505-10 8.731, the following are requirements for BRCA screening and testing:
- BRCA screening, genetic counseling and testing is only covered for clients over the age of 18.
- BRCA screening is covered and must be conducted prior to any BRCA-related genetic testing.
- The provider shall make genetic counseling available to clients with a positive screening both before and after genetic testing, if the provider is able, and genetic counseling is within the provider's scope of practice. If the provider is unable to provide genetic counseling, the provider shall refer the client to a genetic counselor*.
- Genetic testing for breast cancer susceptibility genes BRCA1 and BRCA2 is covered for clients with a positive screening.
*Genetic Counselors cannot be directly reimbursed for services. A supervising physician may be reimbursed. The services require direct supervision if done by a genetic counselor, with the supervisor on site.
Prenatal Testing
Effective July 1, 2022, Genetic Screening, including but not limited to Non-Invasive Prenatal Testing (NIPT), and Genetic Counseling are covered in accordance with nationally recognized standards of care per the American College of Obstetricians and Gynecologists. Screening coverage is available for women carrying a singleton gestation who meet national standard guidelines.
Coverage of this service was available under more specific criteria prior to June 30, 2022.
General Requirements
- Fees for blood drawing, specimen collection, or handling are generally not reimbursable to laboratories.
- The provider who actually performs the laboratory procedure is the only one who is eligible to bill and receive payment. Physicians may only bill for tests actually performed in their office or clinic. Tests performed by laboratories or hospital outpatient laboratories must be billed by the performing laboratory.
- CPT identifies tests that can be and are frequently done as groups and combinations ("profiles") on automated multi-channel equipment. For any combination of tests among those listed, use the appropriate Level 1 or Level 2 CMS codes.
- For organ or disease-oriented panels (check CPT narrative), use the appropriate Level 1 CMS codes. These tests are not to be performed or billed separately when ordered in a group/combination and must be billed with one (1) unit of service.
Procedure/HCPCS Codes Overview
The Department accepts procedure codes that are approved by the Centers for Medicare & Medicaid Services (CMS). The codes are used for submitting claims for services provided to Health First Colorado members and represent services that may be provided by enrolled certified Health First Colorado providers.
The Healthcare Common Procedural Coding System (HCPCS) is divided into two (2) principal subsystems, referred to as level I and level II of the HCPCS. Level I of the HCPCS is comprised of Current Procedural Terminology (CPT), a numeric coding system maintained by the American Medical Association (AMA). The CPT is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other health care professionals. Level II of the HCPCS is a standardized coding system that is used primarily to identify products, supplies, and services not included in the CPT codes, such as ambulance services and durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) when used outside a physician's office. Level II codes are also referred to as alpha-numeric codes because they consist of a single alphabetical letter followed by four (4) numeric digits, while CPT codes are identified using five (5) numeric digits.
HIPAA requires providers to comply with the coding guidelines of the AMA CPT Procedure Codes and the International Classification of Disease, Clinical Modification Diagnosis Codes. If there is no time designated in the official descriptor, the code represents one (1) unit or session.
Visit the Bulletins web page for monthly bulletins, which include updates on approved procedures codes and the maximum allowable units billed per procedure. Visit the Provider News web page to sign up for provider bulletin communications.
Procedure Codes
Services must be reported using HCPCS procedure codes.
Use procedure codes listed in the most recent HCPCS bulletin located on the Bulletins web page.
The fiscal agent updates and revises CMS codes through Health First Colorado bulletins.
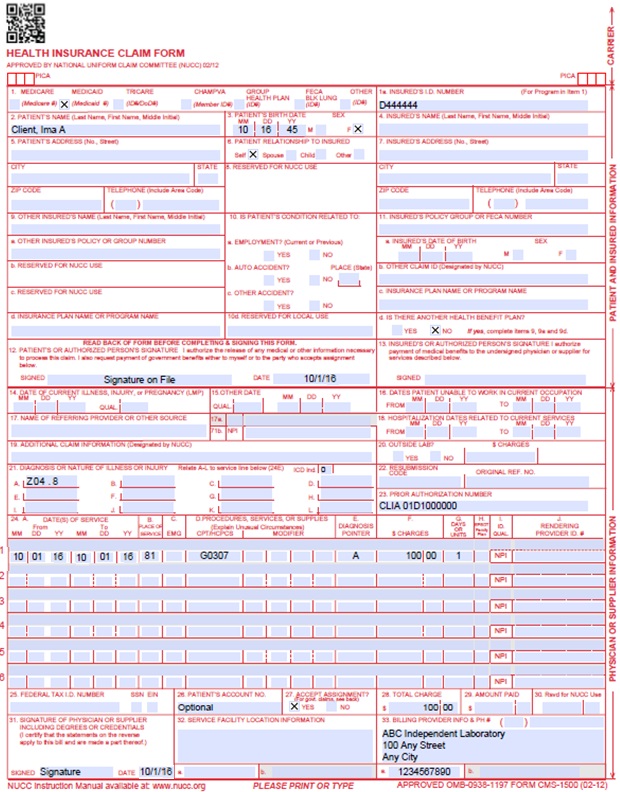
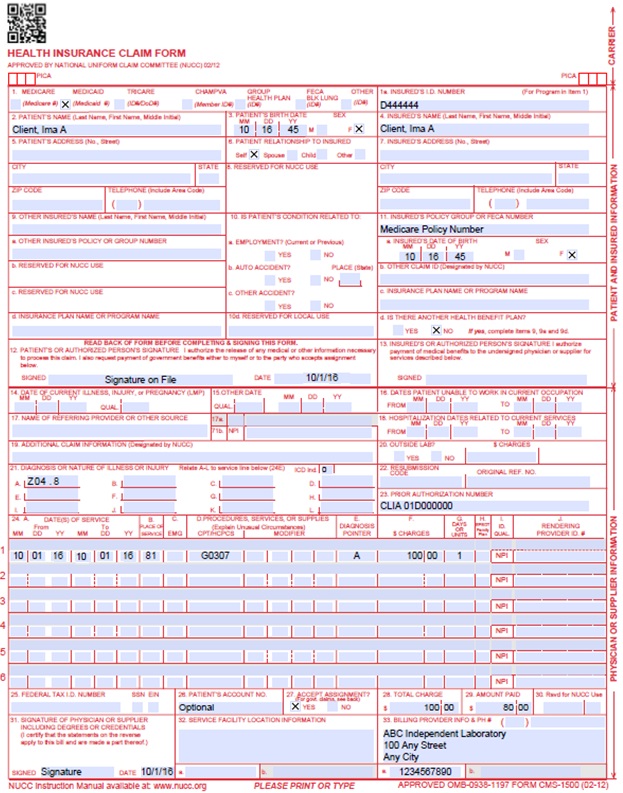
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven (7)-digit ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. NPI of Referring Physician or other source | Required | Required in accordance with Program Rule 8.125.8A | ||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than twelve (12) diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | CLIA When applicable, enter the word "CLIA" followed by the number. Prior Authorization Enter the six (6)-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. | ||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
| ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form.
| ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co-payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | General Instructions | A unit represents the number of times the described procedure or service was rendered. Except as instructed in this manual or in Health First Colorado bulletins, the billed unit must correspond to procedure code descriptions. The following examples show the relationship between the procedure description and the entry of units. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area)
Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
CMS 1500 Laboratory Services Claim Example with CLIA Number
CMS 1500 Laboratory Services Crossover Claim Example with CLIA Number
Timely Filing
Refer to the General Provider Information Manual for more information on timely filing policy, including the resubmission rules for denied claims.
Laboratory Services Revision Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 12/01/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016 Please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manuals Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 2/9/2018 | Removed NDC supplemental qualifier - not relevant for independent laboratory providers | DXC |
| 6/25/2018 | Updated general billing and timely to point to general manual | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 2/22/19 | Add Section on Drug Testing Unit Limitations and Documentation Requirements Added term dates and new codes to PAR table | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 5/6/19 | Add Section on Newborn Metabolic Screening Update Title to Laboratory Services | HCPF |
| 5/22/19 | Add Codes to Prior Authorization Table | HCPF |
| 9/16/19 | Updated Drug Limitations section | HCPF |
| 12/27/19 | Converted to web page | HCPF |
| 1/10/2020 | Added BRCA/Prenatal section, added codes to PAR table | HCPF |
| 1/14/2020 | Update Drug Limitations section | HCPF |
| 9/10/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 8/2/2021 | Updated to box 17 of CMS 1500 Claims Example | HCPF |
| 8/2/2021 | Update to Drug Testing Unit Limitations and Documentation Requirements | HCPF |
| 8/31/2021 |
| HCPF |
| 8/1/2022 | • Updated ordering, prescribing, referring policy • Updated prenatal testing policy to align with changed policy in rule 10 CCR 2505-10 8.732 • Added unlisted procedure code section. | HCPF |
| 10/14/2022 | Removed Phone Number to Gainwell Technologies. Linked verbiage to Provider Help web page. | HCPF |
| 8/2/2023 | Removed CPT 81220 as requiring a PAR | HCPF |
| 6/20/2024 | Added Place of Service Code 03 to field 24B | HCPF |
| 8/19/2024 | Clarified Podiatrist as a provider type that can order Laboratory Services. | HCPF |
| 1/2/2025 | Clarified Optometrist, Pharmacist, Certified Registered Nurse, and Anesthetist as provider types that can order Laboratory Services. | HCPF |
| 1/23/25 |
| HCPF |
| 10/10/2025 | Update to Unit Limitations and Documentation Requirements for Substance Specific Confirmatory Tests (HCPCS G0480-G0483). | HCPF |
| 12/05/2025 | Added medical necessity specifications for Definitive Drug Testing for Addiction Treatment | HCPF |
| 01/09/2026 | Clarified definitive drug testing claim processing logic description. Updated policy for limit of 12 units per SFY. | HCPF |
| 01/15/2026 | Updated definitive drug testing claim processing logic description for limit of 12 units per SFY | HCPF |