Audiology Benefit Billing and Policy Manual
Return to Billing Manuals Web Page
Audiology
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid program) provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
- Providers should refer to the Code of Colorado Regulations, Program Rules (10 CCR 2505-10 8.2.3.D.2), for specific information when providing audiology care.
General Benefit Policies
- All Audiology services must have a written order, referral, or prescription by any of the following:
- Physician (M.D. or D.O.)
- Physician's assistant
- Nurse practitioner
- An approved Individualized Family Service Plan (IFSP) for Early Intervention Audiology services
- Pursuant to the Affordable Care Act's requirements that State Medicaid Agencies ensure correct ordering, prescribing, and referring (OPR) National Provider Identification (NPI) numbers be on the claim form (42 CFR § 455.440):
- All Audiology claims must contain the valid NPI number of the OPR physician, physician assistant, nurse practitioner, or provider associated with an Individualized Family Service Plan (IFSP), in accordance with Program Rule 8.125.8.A.
- The Early Intervention Service Broker may have their rendering NPI listed as the referring NPI for IFSP-ordered early intervention services. The rendering and referring must be the individual NPI for the therapist or the ordering physician.
- All physicians, physician assistants, nurse practitioners, or providers associated with an IFSP who order, prescribe, or refer Audiology services for Health First Colorado members must be enrolled in Health First Colorado (42 CFR § 455.410), in accordance with Program Rule 8.125.7.D. OPR Providers can begin enrollment on Health First Colorado's website.
- The new enrollment requirement for OPR providers does not include a requirement to see Health First Colorado members or to be listed as a Health First Colorado provider for patient assignments or referrals.
- Physicians or other eligible professionals who are already enrolled in Health First Colorado as participating providers and who submit claims to Health First Colorado are not required to enroll separately as OPR providers.
- Field 17b on the CMS1500 claim form must be used for the OPR NPI number.
- All Audiology claims must contain the valid NPI number of the OPR physician, physician assistant, nurse practitioner, or provider associated with an Individualized Family Service Plan (IFSP), in accordance with Program Rule 8.125.8.A.
- The term "valid OPR NPI number" means the registered NPI number of the provider that legitimately orders, prescribes, or refers the Audiology service being rendered, as indicated by the procedure code on the claim.
- Claims without a valid OPR NPI number which are paid will then be subject to recovery.
- Medical documentation must be kept on file to substantiate the order, prescription, or referral for Audiology services. Claims lacking such documentation on file will be subject to recovery.
- Health First Colorado recognizes that Audiology services ordered in conjunction with an approved IFSP for Early Intervention may not necessarily have an ordering provider. Under this circumstance alone the rendering provider must use their own NPI number as the OPR NPI number.
- Early Intervention Audiology claims must have modifier 'TL' attached on the procedure line item for Health First Colorado to identify that the services rendered were associated with an approved IFSP.
- Any claim with modifier 'TL' attached must be for a service ordered by an approved IFSP and delivered within the time span noted in the IFSP.
- If the OPR NPI on the claim is that of the rendering provider, and the claim does not have modifier 'TL' attached, the claim is subject to recovery.
- Early Intervention Audiology claims must have modifier 'TL' attached on the procedure line item for Health First Colorado to identify that the services rendered were associated with an approved IFSP.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
8.280.4.E Other EPSDT Benefits
Other health care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Section 1905(a) of the Social Security Act are a covered benefit under EPSDT when medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, regardless of whether such goods and services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a good or service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one or more Activities of Daily Living; and meets the criteria set forth at Section 8.076.1.8.b - g.
- The service provides a safe environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly.
Billing Information
Refer to the General Provider Information manual for general billing information.
Eligible Providers
- Physicians may provide audiology services, but first must contact the fiscal agent to confirm their enrollment with an otolaryngology specialty.
- Certified audiologists are eligible to become Medical Assistance Program providers.
- Audiologists must be registered with the Department of Regulatory Agencies in order to dispense hearing aids.
- Colorado Home Intervention Program (CHIP) facilitators must be credentialed by Health Care Programs for Children with Special Needs (HCP) administered by the Colorado Department of Public Health and Environment. CHIP facilitators are eligible to become Medical Assistance Program providers and need to enroll in Health First Colorado.
Covered Audiology Benefits
Requirements can be found in the Audiology portion of the Code of Colorado Regulations 10 CCR 2505-10 8.200.3.D.e Covered Services.
Newborn Hearing Screening
The Colorado legislature passed House Bill 97-1095, which establishes hearing screenings for newborn infants [25-4-1004.7(VI)(b)]. Appropriate testing and identification of newborn infants with hearing loss makes early intervention and treatment possible and promotes the healthy development of children. Hearing Conservation Program (HCP) Audiology Regional Coordinators provide consultation information, technical assistance, and referral services to families of children with special health care needs.
Newborn Hearing Screening Reimbursement Policy
- Reimbursement for newborn hearing screening is included in the hospital DRG for inpatient hospital deliveries, and the birth center payment for freestanding birthing center deliveries (see Obstetrical Care billing manual). CPT/HCPCS codes for hearing screening cannot be billed for dates on or during the date span of the delivery stay.
- Follow-up testing for newborns who fail their initial hearing screening may be billed using CPT/HCPCS codes. Follow-up testing may be billed only if they occur on dates of service outside of the date span for the delivery.
Newborn hearing screenings are a Preventive Service, but that designation does not supersede the reimbursement policies listed above.
Unilateral and Bilateral Cochlear Implants
- Unilateral and bilateral cochlear implants are covered for members aged 12 months through 20 years. Criteria for coverage can found in the Code of Colorado Regulation 10 CCR 2505-10 8.200.3.D.e.iv.
- Replacement component(s) of an existing cochlear implant is a benefit for all ages when the currently used component(s) is no longer functional and cannot be repaired.
Hearing Aids
Hearing aids are a covered benefit for members ages 20 and under. Hearing aids for adults are not a covered service.
When billing for a pair of hearing aids, each individual hearing aid must be listed on a separate line on the claim form and must have the appropriate modifier noted to indicate the ear for which it is fitted. The "RT" modifier indicates the hearing aid is for the right ear, and the "LT" modifier indicates it is for the left ear. Billing for two (2) units of a hearing aid, on the same line, without the appropriate modifier will result in a denial.
Providers should bill the same CPT code on one detail line, then include all applicable modifiers.
Hearing Aid Trial Rental Period
The Trial Rental Period is included in the purchase reimbursement for the hearing aid(s). Use the last day of the rental period as the date of service.
Hearing Aid Replacement
Hearing aids are expected to last 3 - 5 years. Replacement of a hearing aid is covered for members ages 20 and under. Hearing aids may be replaced when they no longer fit, have been lost or stolen, or the current hearing aid is no longer medically appropriate for the child.
Softbands (including Bone Anchored Hearing Aids - BAHAs)
Softband hearing devices (including BAHAs) are a covered benefit for members ages 20 and under. All softband purchases require a PAR and must be accompanied by a signed letter from a physician documenting medical necessity. Health First Colorado reimburses softband devices using the following methodology:
On or after January 1, 2021, the method is fee schedule reimbursement. Claims do not require an attached invoice.
Refer to the table below for a list of procedure codes covered for softband devices.
| Covered Softband/BAHA Procedure Code Details | |||||
| Code | Description | PAR | Required PAR and Claim Modifier | Allowed Billing Provider Types | Allowed Rendering Provider Types |
| L8692 | Auditory osseointegrated device, external sound processor, used without osseointegration, body worn, includes headband or other means of external attachment. | Always | NU | Physician, Pharmacy, Supply, Clinics, Osteopath, Audiologist. | Physician, Osteopath, Audiologist |
| L8691 | Replacement. Auditory osseointegrated device, external sound processor. | Always | NU | ||
All Audiology PARs and revisions processed by the ColoradoPAR Program must be submitted through the Utilization Management (UM) vendor. Clinical information is required for a PAR review. When submitting PARs, please answer the clinical questions in the UM portal, attach the relevant clinical documentation needed for determinations, and select "Medical" type from the drop-down menu. If "DME" is selected this will result in non-payment of the device.
Procedure Code Table
Audiologists are indicated as a rendering provider for the following procedure codes. Whether the code is a Health First Colorado covered benefit is indicated. Reference the current Fee Schedule for rates.
Note: This table serves only as a reference guide for audiologists and not a guarantee of payment or coverage. Definitive coverage of a specific procedure code is found on the Fee Schedule.
Last table update: 01/27/2022
| Procedure Code | Covered Benefit | Prior Authorization Needed |
|---|---|---|
| 92502 | Yes | No |
| 92504 | Yes | No |
| 92507 | Yes | Yes |
| 92508 | Yes | Yes |
| 92511 | Yes | No |
| 92512 | Yes | No |
| 92516 | Yes | No |
| 92526 | Yes | Yes |
| 92531 | No | - |
| 92532 | No | - |
| 92533 | Yes | No |
| 92534 | Yes | No |
| 92540 | Yes | No |
| 92541 | Yes | No |
| 92542 | Yes | No |
| 92543 | Yes | No |
| 92544 | Yes | No |
| 92545 | Yes | No |
| 92546 | Yes | No |
| 92547 | Yes | No |
| 92548 | Yes | No |
| 92550 | Yes | No |
| 92552 | Yes | No |
| 92553 | Yes | No |
| 92555 | Yes | No |
| 92556 | Yes | No |
| 92557 | Yes | No |
| 92560 | Yes | No |
| 92561 | Yes | No |
| 92562 | Yes | No |
| 92563 | Yes | No |
| 92564 | Yes | No |
| 92565 | Yes | No |
| 92567 | Yes | No |
| 92568 | Yes | No |
| 92507 | Yes | No |
| 92571 | Yes | No |
| 92572 | Yes | No |
| 92575 | Yes | No |
| 92576 | Yes | No |
| 92577 | Yes | No |
| 92579 | Yes | No |
| 92582 | Yes | No |
| 92583 | Yes | No |
| 92584 | Yes | No |
| 92587 | Yes | No |
| 92588 | Yes | No |
| 92590 | No - See HCPCS V-codes for coverage | - |
| 92591 | No - See HCPCS V-codes for coverage | - |
| 92592 | No - See HCPCS V-codes for coverage | - |
| 92593 | No - See HCPCS V-codes for coverage | - |
| 92594 | No - See HCPCS V-codes for coverage | - |
| 92595 | No - See HCPCS V-codes for coverage | - |
| 92601 | Yes | No |
| 92602 | Yes | No |
| 92603 | Yes | No |
| 92604 | Yes | No |
| 92605 | Yes | No |
| 92606 | Yes | No |
| 92609 | Yes | Yes |
| 92620 | Yes | No |
| 92621 | Yes | No |
| 92625 | Yes | No |
| 92626 | Yes | No |
| 92627 | Yes | No |
| 92630 | Yes | No |
| 92633 | Yes | No |
| 92640 | Yes | No |
| 92650 | Yes | No |
| 92651 | Yes | No |
| 92652 | Yes | No |
| 92653 | Yes | No |
| 92654 | Yes | No |
| 95861 | Yes | No |
| 95920 | Yes | No |
| 95925 | Yes | No |
| 95926 | Yes | No |
| 95927 | Yes | No |
| 95928 | Yes | No |
| 95929 | Yes | No |
| 95930 | Yes | No |
| 95934 | Yes | No |
| 95936 | Yes | No |
| 95937 | Yes | No |
| 96111 | Yes | No |
| 97112 | Yes | No |
| 99201 | Yes | No |
| 99202 | Yes | No |
| 99203 | Yes | No |
| 99204 | Yes | No |
| 99205 | Yes | No |
| 99211 | Yes | No |
| 99212 | Yes | No |
| 99213 | Yes | No |
| 99214 | Yes | No |
| 99215 | Yes | No |
| L7510 | Yes | No |
| L8515 | Yes | No |
| L8615 | Yes | No |
| L8616 | Yes | No |
| L8617 | Yes | No |
| L8618 | Yes | No |
| L8619 | Yes | No |
| L8621 | Yes | No |
| L8622 | Yes | No |
| L8623 | Yes | No |
| L8624 | Yes | No |
| L8691 | Yes | Yes |
| L8692 | Yes | Yes |
| S0618 | Yes | No |
| V5010 | Yes | No |
| V5011 | Yes | No |
| V5014 | Yes | No |
| V5060 | Yes | No |
| V5090 | Yes | No |
| V5095 | No | - |
| V5140 | Yes | No |
| V5171 | Yes | No |
| V5172 | Yes | No |
| V5181 | Yes | No |
| V5211 | Yes | No |
| V5213 | Yes | No |
| V5214 | Yes | No |
| V5215 | Yes | No |
| V5221 | Yes | No |
| V5244 | Yes | No |
| V5245 | Yes | No |
| V5246 | Yes | No |
| V5247 | Yes | No |
| V5250 | Yes | No |
| V5251 | Yes | No |
| V5252 | Yes | No |
| V5253 | Yes | No |
| V5254 | Yes | No |
| V5255 | Yes | No |
| V5256 | Yes | No |
| V5257 | Yes | No |
| V5258 | Yes | No |
| V5259 | Yes | No |
| V5260 | Yes | No |
| V5261 | Yes | No |
| V5262 | No | - |
| V5263 | No | - |
| V5264 | Yes | - |
| V5265 | No | - |
| V5266 | Yes | No |
| V5267 | Yes | No |
| V5275 | Yes | No |
| V5299 | Yes | No |
| V5336 | No | - |
| V5362 | No | - |
| V5363 | No | - |
| V5364 | No | - |
Specific Non-Covered Benefits
- Training or consultation provided by an Audiologist to an agency, facility, or other institution is not covered.
- The upgrading of an existing cochlear implant system or component if the existing unit is properly functioning is not covered.
- Hearing aids for adults (Hearing exams and evaluations are a benefit for adults only when a concurrent medical condition exists) are not covered.
- Hearing aid insurance is not covered.
- Any service not documented in the member's plan of care is not covered.
- Ear molds for the purpose of noise reduction or swimming are not covered.
- Any audiological services rendered by a non-licensed audiologist (except for licensed otolaryngologists and enrolled CHIP providers, are not covered.
Timely Filing
Refer to the General Provider Information Manual for more information on the timely filing policy, including the resubmission rules for denied claims.
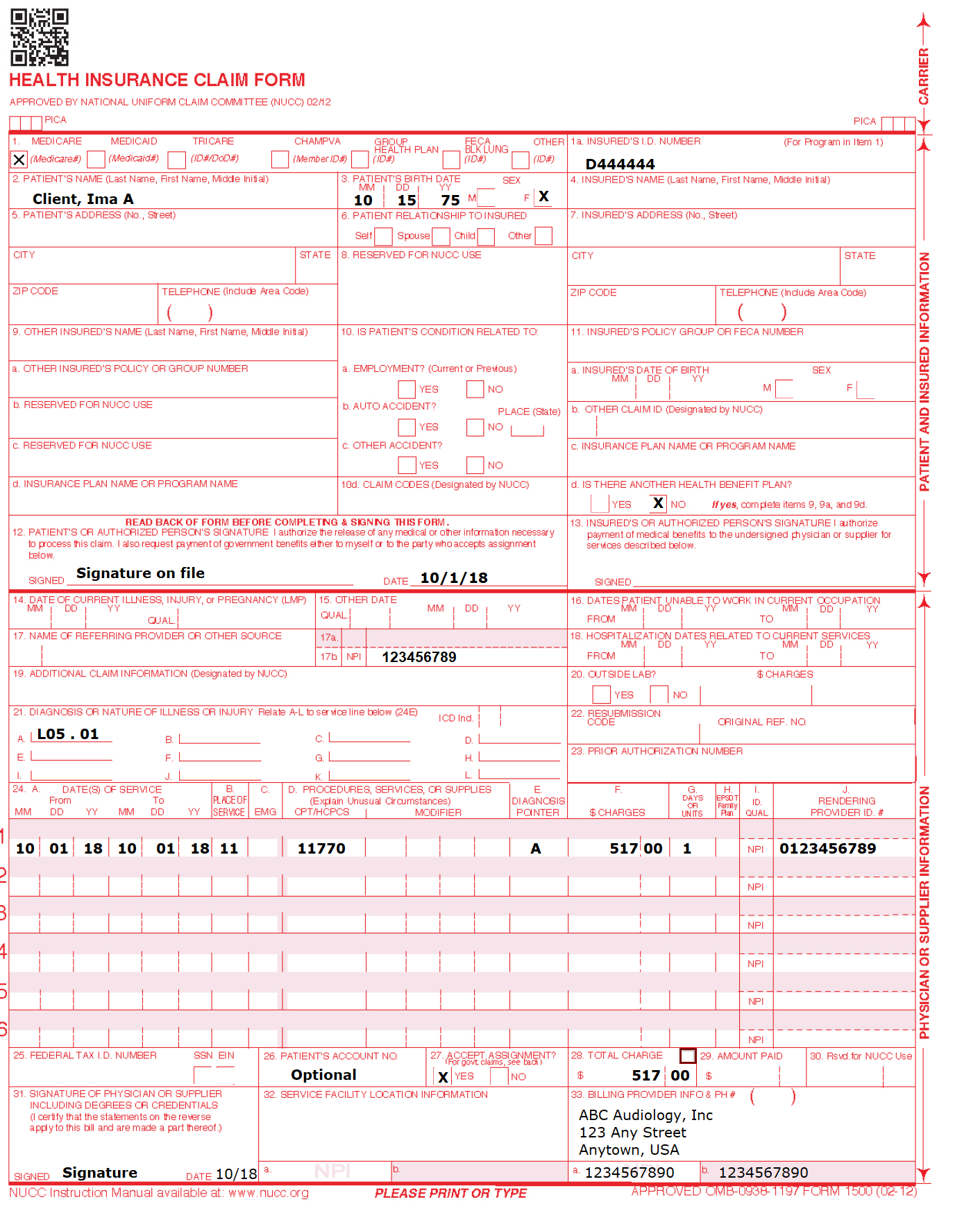
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||||||||||||||
1a. Insured's ID Number | Required | Enter the member's seven-digit Health First Colorado ID number as it appears on the Health First Colorado identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||||||||||||||
2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||
3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two digits for the month, two digits for the date, and two digits for the year. Example: 070114 for July 1, 2014. | ||||||||||||||||||||||||||||||||||||||||||||||||
4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. | ||||||||||||||||||||||||||||||||||||||||||||||||
5. Patient's Address | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||||||||||||||
7. Insured's Address | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
8. Reserved for NUCC Use | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||
9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||||||||||||||
9b. Reserved for NUCC Use |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||
9c. Reserved for NUCC Use |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||
9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||||||||||||||
10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||||||||||||||
10d. Reserved for Local Use |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||
11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. | ||||||||||||||||||||||||||||||||||||||||||||||||
11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. | ||||||||||||||||||||||||||||||||||||||||||||||||
11b. Other Claim ID | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
11c. Insurance Plan Name or Program Name | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||||||||||||||
12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". | ||||||||||||||||||||||||||||||||||||||||||||||||
13. Insured's or Authorized Person's Signature | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two digits for the month, two digits for the date and two digits for the year. Example: 070114 for July 1, 2014. | ||||||||||||||||||||||||||||||||||||||||||||||||
15. Other Date Not | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
16. Date Patient Unable to Work in Current Occupation | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
17. Name of Referring Physician | Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||||||||||||||||||||||||||||||||||||||
18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two digits for the month, two digits for the date and two digits for the year. Example: 070116 for July 1, 2016. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||||||||||||||
19. Additional Claim Information | Conditional |
| ||||||||||||||||||||||||||||||||||||||||||||||||
20. Outside Lab? | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one but no more than twelve diagnosis codes based on the member's diagnosis/condition. | ||||||||||||||||||||||||||||||||||||||||||||||||
22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. | ||||||||||||||||||||||||||||||||||||||||||||||||
23. Prior Authorization | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
24. Claim Line Detail | Information | The paper claim form allows entry of up to six detailed billing lines. Fields 24A through 24J apply to each billed line. | ||||||||||||||||||||||||||||||||||||||||||||||||
24A. Dates of Service | Required | The field accommodates the entry of two dates: a "From" date of services and a "To" date of service. Enter the date of service using two digits for the month, two digits for the date and two digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
Single Date of Service: Enter the six-digit date of service in the "From" field. Completion of the "To" field is not required. Do not spread the date entry across the two fields.
VP - Vendor Product Number | ||||||||||||||||||||||||||||||||||||||||||||||||
24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes. Refer to the Allowed Place of Service Codes section in the Speech Therapy Billing Manual. Effective May 3, 2024, place of service 03 is an allowed place of service for all fee-for-service benefits. In order for community providers to bill fee-for-service to children in a school setting, the provider must follow school district policy. Please reference the Community Providers in a School Setting Policy memo. | ||||||||||||||||||||||||||||||||||||||||||||||||
24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. | ||||||||||||||||||||||||||||||||||||||||||||||||
24D. Procedures, Services, or Supplies | Required | Enter the procedure code that specifically describes the service for which payment is requested. | ||||||||||||||||||||||||||||||||||||||||||||||||
24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four modifiers may be entered when using the paper claim form. Refer to the Allowed Place of Service Codes section in the Speech Therapy Billing Manual. | ||||||||||||||||||||||||||||||||||||||||||||||||
24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. | ||||||||||||||||||||||||||||||||||||||||||||||||
24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||
24G. Days or Units | Required | Enter the number of services provided for each procedure code. | ||||||||||||||||||||||||||||||||||||||||||||||||
24G. Days or Units | General Instructions | A unit represents the number of times the described procedure or service was rendered. | ||||||||||||||||||||||||||||||||||||||||||||||||
24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) | ||||||||||||||||||||||||||||||||||||||||||||||||
24I. ID Qualifier | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||||||||||||||
25. Federal Tax ID Number | Not Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||
27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||||||||||||||
28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||
29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. | ||||||||||||||||||||||||||||||||||||||||||||||||
30. Rsvd for NUCC Use |
|
| ||||||||||||||||||||||||||||||||||||||||||||||||
31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. | ||||||||||||||||||||||||||||||||||||||||||||||||
32. Service Facility Location Information | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: | ||||||||||||||||||||||||||||||||||||||||||||||||
33. Billing Provider | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: | ||||||||||||||||||||||||||||||||||||||||||||||||
33a- NPI Number | Required |
| ||||||||||||||||||||||||||||||||||||||||||||||||
33b- Other ID # |
| If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||||||||||||||
Audiology Claim Example
Audiology Revisions Log
| Revision Date | Additions/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/1/2016 Please refer to Archive. | DXC |
| 12/27/2016 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_2.xlsx | DXC |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | DXC |
| 1/19/2019 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | DXC |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | DXC |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 6/22/2018 | Removed PAR and other info that can be found in general manual (link under billing), updated timely filing with reference back to general billing | HCPF |
| 10/1/2018 | Corrected ear mold policy to separate them from the dispensing fee reimbursement. Updated proc code table to reflect coverage of V5264. | HCPF |
| 1/9/2019 | Updated proc code table for new 2019 HCPCS | HCPF |
| 5/2/2019 | Updated newborn hearing screening reimbursement explanation | HCPF |
| 6/17/2019 | Updated PAR status on certain CPTs in the coding table | HCPF |
| 12/12/2019 | Converted to web page | HCPF |
| 2/12/2020 | Clarified Softband claim submission type (not paper) | HCPF |
| 5/8/2020 | Added OPR policy to General Policy Section | HCPF |
| 12/15/2020 | Updated payment language in Softband Hearing Devices section | HCPF |
| 4/30/2021 | Updated eQSuite to Utilization Management | HCPF |
| 1/27/2022 | Updated Coding Tables | HCPF |
| 3/9/2023 | Added EPSDT Benefit Information | HCPF |
| 5/11/2023 | Removed incorrect information regarding adult coverage of hearing aids in the SLS Waiver. | HCPF |
| 9/6/2023 | Added table for SoftBand and reference table | HCPF |
| 10/17/2023 | Added clarifying line for billing under Hearing Aids section | HCPF |
| 1/8/2024 | Update to Cochlear Implants section | HCPF |
| 4/18/2024 | Updated Early Intervention under General Benefits | HCPF |
| 7/24/2024 | Addition of POS 03-School as an allowed place of service | HCPF |
| 10/24/2025 | Changed CPT code type from 96570 to 92507 | HCPF |