Speech Therapy Billing Manual
- Provider Qualifications
- General Benefit Policies
- Covered Services
- Non-Covered Services
- Assistive Technology Assessments
- Benefit Limitations
- Co-Treatment Policy
- Coding Tables
- Reporting Of Service Units
- National Correct Coding Initiative (NCCI)
- General Billing Information
- Prior Authorization Requests (PARs)
- CMS 1500 Paper Claim Reference Table
- UB-04 Paper Claim Reference Table
- Institutional Provider Certification
- Timely Filing
- Speech Therapy Revisions Log
Return to Billing Manuals Web Page
Provider Qualifications
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid Program) provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
Eligible Providers
Eligible providers may be individual practitioners or may be employed by home care agencies, children's developmental service agencies, health departments, Federally Qualified Health Centers (FQHC), clinics, or hospital outpatient facilities. The provider agency or the individual provider must verify that rendering providers meet the following qualifications:
Speech-language Pathologists (SLPs, speech therapists) must have a current license pursuant to the Speech-language Pathology Practice Act.
Speech-language Pathology Assistants are support personnel who, following academic and/or on-the-job training, perform tasks prescribed, directed, and supervised by licensed speech-language pathologists. Speech-language pathologists must follow the ASHA guidelines on the training, use, and supervision of assistants. Speech-language pathology assistants must practice under the direct supervision of a Colorado licensed speech-language pathologist (10 CCR 2505-10 8.200.2.D.1.d., effective December 30, 2020).
- Speech-language pathology assistants cannot enroll with Health First Colorado and therefore cannot place any identifying number on a claim form. Therefore, the supervising therapist's NPI must be used as the rendering provider on the claim form for services rendered by the assistant.
Clinical Fellows, practicing under the general supervision of a licensed speech-language pathologist may provide speech therapy services.
- Clinical Fellows cannot enroll with Health First Colorado and therefore cannot place any identifying number on a claim form. Therefore, the supervising therapist's NPI must be used as the rendering provider on the claim form for services rendered by the Clinical Fellow.
Therapy may also be rendered by licensed and enrolled physicians, physician assistants and advanced practice nurses as allowed by their respective scopes of practice.
All providers must submit a completed provider enrollment to become a Health First Colorado provider. Visit the Provider Enrollment web page for enrollment information. Pursuant to 10 CCR 2505-10 8.200.3.D.2.b, providers of in-home health who employ therapists or audiologists shall apply for licensing through the Colorado Department of Public Health and Environment (CDPHE). (§ 25-27.5-103(1), C.R.S. and 6 CCR 1011-1, Chapter XXVI, Section 5.1) as a home care agency. This rule does not apply to providers delivering Early Intervention Services under an Individual Family Service Plan (IFSP) and billing through contracts with the Community Centered Boards.
General Benefit Policies
Speech therapists not employed by an agency, clinic, hospital, or physician may bill Health First Colorado directly; otherwise, it is the employer who bills directly for the services. Providers should refer to the Code of Colorado Regulations, Qualified Non-Physician Practitioners Eligible to Provide Physician's Services (10 CCR 2505-10, Section 8.200.2.C), for further regulatory information when providing speech therapy.
- All Outpatient Speech Therapy services must have a written order/prescription/referral by any of the following:
- Physician (M.D. or D.O.)
- Physician Assistant
- Nurse Practitioner
- An approved Individualized Family Service Plan (IFSP) for Early Intervention Speech Therapy. (Senate bill 07-004 states the IFSP "shall qualify as meeting the standard for medically necessary services." Therefore, no physician is required to sign a work order for the IFSP.)
- Pursuant to the Affordable Care Act's requirements that State Medicaid Agencies ensure correct ordering, prescribing, and referring (OPR) National Provider Identification (NPI) numbers be on the claim form (42 CFR § 455.440):
- All Outpatient Speech Therapy claims must contain the valid NPI number of the Ordering, Prescribing, Rendering (OPR) physician, physician assistant, nurse practitioner, or provider associated with an Individualized Family Service Plan (IFSP), in accordance with Program Rule 8.125.8.A.
- The Early Intervention Service Broker may have their rendering NPI listed as the referring NPI for IFSP-ordered early intervention services. The rendering and referring must be the individual NPI for the therapist or the ordering physician.
- All physicians, physician assistants, nurse practitioners, or providers associated with an IFSP who order, prescribe, or refer Outpatient Speech Therapy services for Health First Colorado members must be enrolled in Health First Colorado (42 CFR § 455.410), in accordance with Program Rule 8.125.7.D. OPR Providers can begin enrollment on Health First Colorado's website.
- The new enrollment requirement for OPR providers does not include a requirement to see Health First Colorado members or to be listed as a Health First Colorado provider for member assignments or referrals.
- Physicians or other eligible professionals who are already enrolled in Health First Colorado as participating providers and who submit claims to Health First Colorado are not required to enroll separately as OPR providers.
- Field 17.b on the CMS 1500 claim form must be used for the OPR NPI number.
- All Outpatient Speech Therapy claims must contain the valid NPI number of the Ordering, Prescribing, Rendering (OPR) physician, physician assistant, nurse practitioner, or provider associated with an Individualized Family Service Plan (IFSP), in accordance with Program Rule 8.125.8.A.
- The term "valid OPR NPI number" means the registered NPI number of the provider that legitimately orders, prescribes, or refers the Outpatient Speech Therapy service being rendered, as indicated by the procedure code on the claim.
- Claims without a valid OPR NPI number that are paid will then be subject to recovery.
- Medical documentation must be kept on file to substantiate the order, prescription, or referral for Outpatient Speech Therapy. Claims lacking such documentation on file will be subject to recovery.
- Health First Colorado recognizes that Outpatient Speech Therapy ordered in conjunction with an approved IFSP for Early Intervention may not necessarily have an ordering provider. Under this circumstance alone the rendering provider must use their own NPI number as the OPR NPI number.
- Early Intervention Outpatient Speech Therapy claims must have modifier 'TL' attached on the procedure line item for Health First Colorado to identify that the services rendered were associated with an approved IFSP.
- Any claim with modifier 'TL' attached must be for a service ordered by an approved IFSP.
- If the OPR NPI on the claim is that of the rendering provider, and the claim does not have modifier 'TL' attached, the claim is subject to recovery.
- Early Intervention Outpatient Speech Therapy claims must have modifier 'TL' attached on the procedure line item for Health First Colorado to identify that the services rendered were associated with an approved IFSP.
- The term "Outpatient" means any therapy which is not performed in an Inpatient Hospital or School setting, or by a Home Health Agency.
- Speech-language pathologists not employed by an agency, clinic, hospital, school district, or physician may bill Health First Colorado directly. Providers should refer to the Code of Colorado Regulations, Qualified Non-Physician Practitioners Eligible to Provide Physician's Services (10 CCR 2505-10, Section 8.2003.C), for specific information when providing speech therapy.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
8.280.4.E Other EPSDT Benefits
Other health care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Section 1905(a) of the Social Security Act are a covered benefit under EPSDT when medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, regardless of whether such goods and services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a good or service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one or more Activities of Daily Living; and meets the criteria set forth at Section 8.076.1.8.b - g.
- The service provides a safe environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly.
Payment for Covered Services
Regardless of whether Health First Colorado has actually reimbursed the provider, billing members for covered services is strictly prohibited. Balance billing is prohibited. If reimbursement is made, providers must accept this payment as payment in full (refer to Program Rule 8.012). The provider may only bill the member for services not covered by Health First Colorado.
- Members may be billed for non-covered services in accordance with C.R.S. 25.5-4- 301(1)(a)(I).
- (1) (a) (I) Except as provided in section 25.5-4-302 and subparagraph (III) of this paragraph (a), no recipient or estate of the recipient shall be liable for the cost or the cost remaining after payment by Medicaid, Medicare, or a private insurer of medical benefits authorized by Title XIX of the social security act, by this title, or by rules promulgated by the state board, which benefits are rendered to the recipient by a provider of medical services authorized to render such service in the state of Colorado, except those contributions required pursuant to section 25.5-4- 209 (1). However, a recipient may enter into a documented agreement with a provider under which the recipient agrees to pay for items or services that are non-reimbursable under the medical assistance program. Under these circumstances, a recipient is liable for the cost of such services and items.
- If Prior Authorization Requests (PAR) for services are required, the following policy applies:
- Technical/lack of information (LOI) denial does not mean those services are not covered. Members may not be billed for services denied for LOI.
- Services partially approved are still considered covered services. Members may not be billed for the denied portion of the request.
- Services totally denied for not meeting medical necessity criteria are considered non-covered services.
Medically Necessary
Outpatient speech therapy services must be medically necessary to qualify for Health First Colorado reimbursement. Medical necessity (10 CCR 2505-10 8.076.1.8) means a Medical Assistance program good or service:
- Will, or is reasonably expected to, prevent, diagnose, cure, correct, reduce, or ameliorate the pain and suffering, or the physical, mental, cognitive, or developmental effects of an illness, condition, injury, or disability. This may include a course of treatment that includes mere observation or no treatment at all.
- Is provided in accordance with generally accepted professional standards for health care in the United States,
- Is clinically appropriate in terms of type, frequency, extent, site, and duration,
- Is not primarily for the economic benefit of the provider or primarily for the convenience of the member, caretaker, or provider,
- Is delivered in the most appropriate setting(s) required by the member's condition,
- Is not experimental or investigational, and
- Is not more costly than other equally effective treatment options.
Documentation Requirements
Rendering providers must document all evaluations, re-evaluations, services provided, member progress, attendance records, and discharge plans. All documentation must be kept in the member's records along with a copy of the referral or prescribing provider's order. Documentation must support both the medical necessity of services and the need for the level of skill provided. Rendering providers must copy the member's primary care provider (PCP), prescribing provider and/or medical home on all relevant records.
All documentation must include the following:
- The member's name and date of birth
- The date and type of service provided to the member
- A description of each service provided during the encounter including procedure codes and time spent on each (including start and stop times)
- The total duration of the encounter
- The name or names and titles of the persons providing each service and the name and title of the therapist supervising or directing the services.
Health First Colorado requires the following types of documentation as a record of services provided within an episode of care: initial evaluation, re-evaluation, visit/encounter notes and a discharge summary.
Initial Evaluation
Written documentation of the initial evaluation must include the following:
- Referral Information: Reason for referral and referral source.
- History: Must include diagnoses pertinent to the reason for referral, including date of onset, cognitive, emotional, and/or physical loss necessitating referral, and the date of onset, if different from the onset of the relevant diagnoses, current functional limitation or disability as a result of the above loss, and the onset of the disability, pre-morbid functional status, including any pre-existing loss or disabilities, review of available test results, review of previous therapies/interventions for the presenting diagnoses, and the functional changes (or lack thereof) as a result of previous therapies or interventions.
- Assessment: The assessment section must include a summary of the member's impairments, functional limitations and disabilities, based on a synthesis of all data/findings gathered from the evaluation procedures. Pertinent factors which influence the treatment diagnosis and prognosis must be highlighted, and the inter-relationship between the diagnoses and disabilities for which the referral was made must be discussed.
- Plan of Care: A detailed Plan of Care must be included in the documentation of an initial evaluation. This care plan must include the following:
- Specific treatment goals for the entire episode of care which are functionally-based and objectively measured
- Proposed interventions/treatments to be provided during the episode of care
- Proposed duration and frequency of services to be provided
- Estimated duration of episode of care.
- An episode of outpatient therapy is defined as the period of time from the first day the member is under the care of the clinician for the current condition(s) being treated by one therapy discipline until the last date of service for that plan of care for that discipline in that setting.
- The therapist's plan of care must be reviewed, revised if necessary, and signed, as medically necessary by the member's physician, or other licensed practitioner of the healing arts within the practitioner's scope of practice under state law at least once every 90 days.
- The care plan may not cover more than a 90-day period, or the time frame documented in the approved IFSP.
- A plan of care must be certified. Certification is the physician's, physician's assistant or nurse practitioner's approval of the plan of care. Certification requires a dated signature on the plan of care or some other document that indicates approval of the plan of care. If the service is a Medicare covered service and is provided to a member who is eligible for Medicare, the plan of care must be reviewed at the intervals required by Medicare.
Re-Evaluation
A re-evaluation must occur whenever there is an unanticipated change in the member's status, a failure to respond to interventions as expected or there is a need for a new plan of care based on new problems and goals requiring a significant modification of treatment plan. The documentation for a re-evaluation need not be as comprehensive as the initial evaluation, but must include at least the following:
- Reason for re-evaluation
- Member's health and functional status reflecting any changes
- Findings from any repeated or new examination elements
- Changes to plan of care
Written documentation of each encounter must be in the member's record of service. These visit notes document the implementation of the plan of care established by the therapist at the initial evaluation. Each visit note must include the following:
- The member's name and date of birth.
- The date of service.
- The type of service provided to the member.
- Total timed code treatment minutes and total treatment time in minutes.
- Total treatment time includes the minutes for timed code treatment and untimed code treatment.
- Total treatment time does not include time for services that are not billable (e.g., rest periods).
- The time spent providing each service. The number of units billed/requested must match the documentation (billing and the total timed code treatment minutes must be consistent).
- A description of each service provided during the encounter including procedure codes. The description should support each procedure code billed.
- The name or names and titles of the persons providing each service including assistants and the name and title of the therapist supervising or directing the services.
- Identification of the short or long-term goals being addressed during the encounter.
In addition to the above required information items the visit note documentation must contain the Subjective, Objective, Assessment and Plan format elements. These may be documented in any order (i.e., SOAP, APSO, etc.)
- A subjective element which includes the reason for the visit, the member/caregiver's report of current status relative to treatment goals, and any changes in member's status since the last visit,
- An objective element which includes the practitioner's findings, including abnormal and pertinent normal findings from any procedures or tests performed,
- An assessment component which includes the practitioner's assessment of the member's response to interventions provided, specific progress made toward treatment goals, and any factors affecting the intervention or progression of goals, and
- A plan component which states the plan for next visit(s).
Discharge Summary
At the conclusion of therapy services, a discharge summary must be included in the documentation of the final visit in an episode of care. This must include the following:
- Highlights of a member's progress or lack of progress towards treatment goals.
- Summary of the outcome of services provided during the episode of care.
Record Retention
Providers must maintain records that fully disclose the nature and extent of services provided. Upon request, providers must furnish information about payments claimed for Colorado Medical Assistance Program services. Records must substantiate submitted claim information. Such records include but are not limited to:
- Treatment plans
- Prior authorization requests
- Medical records and service reports
- Records and original invoices for items, including drugs that are prescribed, ordered, or furnished
- Claims, billings, and records of Colorado Medical Assistance Program payments and amounts received from other payers
- Each provider shall retain any other records created in the regular operation of business that relate to the type and extent of goods and services provided (for example, superbills).
- All records must be legible, verifiable, and must comply with generally accepted accounting principles and auditing standards (10 CCR 2505-10 8.130.2.E).
- Each entry in a medical record must be signed and dated by the individual providing the medical service. Stamped signatures are not acceptable (10 CCR 2505-10 8.130.2.F).
- Providers utilizing electronic record keeping may apply computerized signatures and dates to the medical record if their record-keeping systems guarantee the following security measures:
- Restrict application of an electronic signature to the specific individual identified by the signature. System security must prevent one person from signing another person's name.
- Prevent alterations to authenticated (signed and dated) reports. If the provider chooses to supplement a previous entry, the system must only allow a new entry that explains the supplement. The provider cannot be allowed to change the initial entry.
Printed or displayed electronic records must note that signatures and dates have been applied electronically (10 CCR 2505-10 8.130.2.G.).
Covered Services
Assessment
Service may include testing and/or clinical observation, as appropriate for chronological or developmental age, for one or more of the following areas, and must yield a written evaluation report.
- Expressive language.
- Receptive language.
- Cognition.
- Augmentative and alternative communication.
- Voice disorder.
- Resonance patterns.
- Articulation/phonological development.
- Pragmatic language.
- Fluency.
- Feeding and swallowing.
- Hearing status based on pass/fail criteria.
- Motor speech.
- Aural rehabilitation (defined by provider's scope of practice).
- Speech Therapy for the diagnosis of Gender Affirming Care.
Treatment
Service may include one or more of the following, as appropriate:
- Articulation/phonological therapy.
- Language therapy including expressive, receptive, and pragmatic language.
- Augmentative and alternative communication therapy. Adults with chronic conditions may qualify for augmentative and alternative communication services when justified and supported by medical necessity to allow the individual to achieve or maintain maximum functional communication for performance of Activities of Daily Living.
- Auditory processing/discrimination therapy.
- Fluency therapy.
- Voice therapy.
- Oral motor therapy.
- Swallowing therapy.
- Speech reading.
- Cognitive treatment.
- Necessary supplies and equipment.
- Aural rehabilitation (defined by provider's scope of practice).
Rehabilitative Speech Therapy
In accordance with 10 CCR 2505-10 8.200.3.D.2.d.i, Rehabilitative speech therapy is a covered benefit under the following conditions. "Rehabilitative" means therapy that treats acute injuries and illnesses which are non-chronic conditions. Rehabilitative is therefore short-term in nature.
- Adult Policy
- All Health First Colorado members age 21 and over may receive Rehabilitative speech therapy to treat non-chronic conditions and acute illness and injury.
- Child Policy
- All Health First Colorado members age 20 and under may receive Rehabilitative speech therapy to treat non-chronic conditions and acute illness and injury.
- The acute condition must be documented in all medical/treatment session notes and must be accompanied by an order/referral/prescription by a licensed Health First Colorado enrolled physician, physician assistant, or nurse practitioner.
Habilitative Speech Therapy
"Habilitative" means therapy that treats chronic conditions with the purpose of helping the member retain or improve skills and functioning that are affected by the chronic condition. Habilitative therapy may therefore be long-term in nature.
- Adult Policy
- All Health First Colorado members ages 21 and over are considered adults. Effective July 1, 2025, Health First Colorado covers adult habilitative speech therapy services for eligible adult members when medically necessary. These services are subject to the same PAR requirements as other speech therapy services.
- The member's chronic condition must be documented in all medical/treatment session notes, as well as in the Prior Authorization Request, and must be accompanied by an order/referral/prescription by a licensed Health First Colorado enrolled physician, physician assistant, or nurse practitioner.
- Eligible members may receive Habilitative speech therapy in addition to Rehabilitative speech therapy so long as the therapies are not duplicative and rendered on the same date of service.
- Child Policy
- All Health First Colorado members ages 20 and under may receive Habilitative speech therapy to treat a chronic condition which requires ongoing speech therapy to prevent against the loss of functional ability.
- The chronic condition must be documented in all medical/treatment session notes and must be accompanied by an order/referral/prescription by a licensed Health First Colorado enrolled physician, physician assistant, or nurse practitioner.
- Eligible members may receive Habilitative speech therapy in addition to Rehabilitative speech therapy so long as the therapies are not duplicative and rendered on the same date of service.
Additional Notes
- Habilitative therapies are not categorized as an Inpatient or Home Health benefit. 'Acute' and 'Long-term' therapies remain benefits per Home Health coverage.
- Habilitative therapies are not categorized as a benefit if provided in nursing facilities, Rehabilitative speech therapy remain a benefit in that setting.
- Habilitative therapies should not be confused with Habilitation services found within Home and Community Based Services (HCBS) waivers.
Non-Covered Services
- Health First Colorado does not cover items and services which generally enhance the personal comfort of the eligible person but are not necessary in the diagnosis of, do not contribute meaningfully to the treatment of an illness or injury, or the functioning of a malformed body member.
- Services provided without a written referral from a physician or other licensed practitioner of the healing arts within the practitioner's scope of practice under state law are not covered, unless they are covered by an Individual Family Service Plan (IFSP).
- Treatment of speech and language delays not associated with an acquired or chronic medical condition, neurological disorder, acute illness, injury, or congenital defect are not covered, unless they are covered by an IFSP.
- Any service that is not determined by the provider to be medically necessary according to the definition of medical necessity in this document is not covered.
- Services not documented in the member's health care record are not covered.
- Services not part of the member's plan of care are not covered.
- Services specified in a plan of care that is not reviewed and revised as medically necessary by the member's physician (M.D. or D.O.), physician's assistant, nurse practitioner, or specified in an approved IFSP for Early Intervention speech therapy are not covered.
- Art and craft activities for the purposes of recreation are not covered.
- Services which are experimental, investigational, or are provided as part of a clinical trial are not covered.
- Supplies or prefabricated supplies that can be obtained from a medical supplier are not covered.
- Services for conditions of chronic pain that do not interfere with the member's functional status and that can be treated by routine nursing measures are not covered.
- Services that are not designed to improve or maintain the functional status of a recipient with a physical loss or a cognitive or psychological deficit are not covered.
- A therapeutic service that is denied Medicare payment because of the provider's failure to comply with Medicare requirements is not covered.
- Vocational or educational services, except as provided under IEP-related or waiver services are not covered.
- Services provided by unsupervised therapy assistants as defined by the American Speech-Language Hearing Association (ASHA) are not covered.
- Treatment for dysfunction that is self-correcting (for example, natural dysfluency or developmental articulation errors) is not covered.
- Psychosocial services are not covered.
- Educational, personal need and comfort therapies are not covered.
- Record keeping documentation and travel time (the transport and waiting time of a member to and from therapy sessions) is not reimbursable.
- Time spent for preparation, report writing, processing of claims, or documentation regarding billing or service provision is not reimbursable.
- Therapy that replicates services that are provided concurrently by another type of therapy is not covered. Particularly, occupational therapy which should provide different treatment goals, plans, and therapeutic modalities from speech therapy.
Assistive Technology Assessments
The following billing policies are effective for CPT procedure code 97755 to accommodate HB14-1211. HB14-1211 requires that all Health First Colorado members seeking complex rehabilitation technology must have an initial Assistive Technology Assessment (complex rehabilitative technology evaluation/assessment) prior to receiving complex rehabilitation technology, and follow-up assessments, as needed. Only licensed speech, physical, and occupational therapists may render this specialty evaluation.
All providers using procedure code 97755 must follow these guidelines. The Department recognizes that only a portion of Assistive Technology Assessments will be used for complex rehabilitation technology evaluation/assessment. Providers will be asked upon PAR submission if the service is for a complex rehabilitation technology assessment.
| Policy | Notes |
|---|---|
| Complex rehabilitation technology evaluations / assessments are billed using only 97755. | Combinations of procedure codes, including procedure code 97542, for the purposes of complex rehabilitation technology evaluation / assessment are not allowed. |
| 97755 always requires a Prior Authorization Request (PAR). | PARs must be submitted electronically using ColoradoPAR. Visit the ColoradoPAR web page for details. |
| Member daily limit of 97755 is 20 units. | Up to five hours of assessment is allowed per date of service. |
| Member yearly limit of 97755 is 60 units. | Members may have up to 60 units of procedure code 97755 per State Fiscal Year (July 1 - June 30). This limit will reset with the start of each new State Fiscal Year. |
PARs for 97755 must comply with the following policies:
- Must have a current prescription/referral for an Assistive Technology Assessment from the member's primary care physician.
- May indicate up to one-year duration.
- May indicate initial/new assessments or follow-up assessment visits.
- Only one active PAR for 97755 is allowed per member, per span of time. Overlapping 97755 PAR requests will be denied.
- Initial speech therapy evaluation services, such as 92521, are not required prior to requesting 97755.
- 97755 is separate from physical and occupational therapy (PT/OT) and is not part of the PT/OT benefit limitation.
- PARs for 97755 should be submitted independently from other services. The Medical PAR type should be selected for 97755.
97755 performed by a Speech Therapist is considered Rehabilitative speech therapy and is covered for both adults and children.
If a member requires further assessment by a different provider not indicated on the original PAR, and that PAR is still active, then it must be closed by the original requesting provider. Once closed a new PAR can be submitted. Members may request a 'change of provider' on their PAR by contacting the vendor directly. Please see the Prior Authorization Request section of this manual.
Benefit Limitations
- Eligible members may not receive both Rehabilitative and Habilitative speech therapy services on the same date of service.
- Providers are required to consult the American Medical Association's (AMA) Current Procedural Terminology (CPT) manual for each coded service. Some codes represent a treatment session without regard to its length of time (one unit maximum) while other codes may be billed incrementally as "timed" units.
- Members determined to need a speech generating device (HCPCS codes E2500, E2502, E2504, E2510, E2211, E2512, and E2599) should be referred to a Health First Colorado participating medical supplier to be prior authorized.
- All claims must meet eligibility and claim submission requirements (e.g., timely filing, third-party resources payment pursued, required attachments included, etc.) before payment can be made.
Co-Treatment Policy
Co-treatment sessions between two outpatient therapists (pediatric behavioral therapists, physical therapists, occupational therapists, and/or speech-language pathologists) are a covered service under the following conditions:
- Valid clinical rationale for providing co-treatment must be present. Refer to the Joint Guidelines for Therapy Co-Treatment developed by the American Speech-Language-Hearing Association (ASHA), American Occupational Therapy Association (AOTA), and American Physical Therapy Association (APTA).
- Each provider must have an approved Plan of Care (or IFSP for Early Intervention) which includes co-treatment.
- Each provider must have an approved Prior Authorization which includes the Plan of Care/IFSP documentation that co-treatment will be used.
- Each provider may only bill for the time they directly treat the member during the co-treatment session. Direct treatment means a one-on-one treatment interaction between the provider and the member and does not include observation. The intent of the Department is to not reimburse twice for the same increments of time the member receives treatment. Direct treatment times are not required to be contiguous spans of time and may be broken-up as the therapists alternate interacting with the member. The providers must then only bill for the total amount of time they individually spent providing direct treatment.
Example:
A child receives one hour of co-treatment involving a Pediatric Behavioral Therapist and a Speech Therapist. While both providers are with the child for the full hour, during that time the Speech Therapist provides direct treatment for 30 minutes and the Pediatric Behavioral Therapist provides direct treatment for 30 minutes.
The Speech Therapist would report one unit of Current Procedural Terminology (CPT) 92507, because CPT 92507 is a visit-based unit regardless of time. The Pediatric Behavioral Therapist would report two units of CPT 97153, because CPT 97153 is billed in increments of 15 minutes.
Coding Tables
Allowed Place of Service Codes
The following place of service codes are allowed:
| Place of Service (POS) | Code Description |
| 02 | Telemedicine- not provided in patient’s home. Refer to the Telemedicine Billing Manual. |
| 03 | School - (non-public) services provided in or during public school must be billed by the school district only |
| 10 | Telehealth- provided in patient’s home. Refer to the Telemedicine Billing Manual. |
| 11 | Office |
| 12 | Home |
| 13 | Assisted Living Facility |
| 99 | Other - (Community Based Organization) |
- Effective May 3, 2024, place of service 03 is an allowed place of service for all fee-for-service benefits. In order for community providers to bill fee-for-service to children in a school setting, the provider must follow school district policy. Please reference the Community Providers in a School Setting Policy memo.
- Telemedicine place of service (POS) code 02 is available for specific procedure codes. Visit the Telemedicine - Provider Information web page for a list of allowed procedure codes.
- Speech therapy services provided at an Outpatient Hospital are reported on the institutional claim type and are reimbursed as part of the hospital's EAPG payment. Institutional claim types do not have the POS code field.
- Speech therapy services provided at a Federally Qualified Health Center (FQHC) are billed as part of the encounter rate for the FQHC. They are not billed separately on professional claims.
- Rule allows for speech therapy services to be rendered at a location of "Community Based Organization". Since there is no exact POS code which aligns with this description, POS code 99 should be reported.
- NCCI MUE edits stipulate maximum daily units for each code. Visit the NCCI web page for further information.
- Providers should reference official AMA CPT resources for full descriptions of codes and instruction for proper use.
Required Billing and PAR Modifiers
Effective December 1, 2023, appropriate modifiers must be included on both the PAR and claim submission.
| Outpatient Therapy Type | Modifier 1 | Modifier 2 |
|---|---|---|
| Rehabilitative Speech Therapy | GN | 97 |
| Habilitative Speech Therapy | GN | 96 |
| Early Intervention Speech Therapy | GN | TL |
Allowed Outpatient Speech Therapy Procedure Codes
| Procedure Code | Unit Limits Max # units per member, per provider, per DOS | Prior Authorization Required | Notes |
|---|---|---|---|
| 92521 | NCCI MUE value | No | |
| 92522 | NCCI MUE value | No | |
| 92523 | NCCI MUE value | No | |
| 92524 | NCCI MUE value | No | |
| 92507 | NCCI MUE Value (this is an encounter-based code to be billed at a maximum of 1 unit of service per day) | Does not require a PAR for the first 12 sessions, requires PAR after 12 sessions are utilized. | |
| 92508 | NCCI MUE Value (this is an encounter-based code to be billed at a maximum of 1 unit of service per day) | Does not require a PAR for the first 12 sessions, requires PAR after 12 sessions are utilized. | |
| 92520 | NCCI MUE Value | No | |
| 92526 | NCCI MUE Value | Does not require a PAR for the first 12 sessions, requires PAR after 12 sessions are utilized. | |
| 92597 | NCCI MUE Value | No | |
| 92605 | NCCI MUE Value | No | |
| 92606 | NCCI MUE Value | No | |
| 92607 | NCCI MUE Value | No | |
| 92608 | NCCI MUE Value | No | |
| 92609 | NCCI MUE Value | Does not require a PAR for the first 12 sessions, requires PAR after 12 sessions are utilized. | |
| 92610 | NCCI MUE Value | No | |
| 92611 | NCCI MUE Value | No | |
| 92612 | NCCI MUE Value | No | |
| 92614 | NCCI MUE Value | No | |
| 92626 | NCCI MUE Value | No | |
| 92627 | NCCI MUE Value | No | |
| 96105 | NCCI MUE Value | No | |
| 96111 | NCCI MUE Value | No | |
| 96112 | NCCI MUE Value | No | |
| 96113 | NCCI MUE Value | No | |
| G0515 (End date 12/31/2019) | NCCI MUE Value | No | |
| 97129 | NCCI MUE Value | Does not require a PAR for the first 12 sessions, requires PAR after 12 sessions are utilized. | |
| 97130 | NCCI MUE Value | Does not require a PAR for the first 12 sessions, requires PAR after 12 sessions are utilized. | |
| 97755 | 20 per day, 60 per fiscal year | Yes | Modifiers 96 or 97 are not required for this procedure code as this evaluation cannot be classified as either 'rehabilitative' or 'habilitative'. |
| Q3014 | NCCI MUE Value | No | |
| V5011 | NCCI MUE Value | No | For use with Colorado Home Intervention Program |
Reporting of Service Units
A. Timed and Untimed Codes
When reporting service units for CPT/HCPCS codes where the procedure is not defined by a specific timeframe ("untimed" CPT/HCPCS), the provider enters "1" in the field labeled "units." For untimed codes, units are reported based on the number of times the procedure is performed, as described in the CPT/HCPCS code definition.
Example: A member received a speech-language pathology evaluation represented by HCPCS "untimed" code 92521. Regardless of the number of minutes spent providing this service, only one unit of service is appropriately billed on the same day.
Several CPT codes used for therapy modalities, procedures, tests and measurements specify that the direct (one-on-one) time spent in patient contact is 15 minutes. Providers report these "timed" procedure codes for services delivered on any single calendar day using CPT codes and the appropriate number of 15-minute units of service.
Example: A member received a total of 60 minutes of occupational therapy, e.g., HCPCS "timed" code 97530 which is defined in 15-minute units, on a given date of service. The provider would then report 4 units of code 97530.
B. Counting Minutes for Timed Codes in 15-Minute Units
When only one service is provided in a day, providers should not bill for services performed for less than 8 minutes. For any single timed CPT code in the same day measured in 15-minute units, providers bill a single 15-minute unit for treatment greater than or equal to 8 minutes through and including 22 minutes. If the duration of a single modality or procedure in a day is greater than or equal to 23 minutes, through and including 37 minutes, then 2 units should be billed. Time intervals for 1 through 8 units are as follows:
| Units | Number of Minutes |
|---|---|
| 1 unit: | ≥ 8 minutes through 22 minutes |
| 2 units: | ≥ 23 minutes through 37 minutes |
| 3 units: | ≥ 38 minutes through 52 minutes |
| 4 units: | ≥ 53 minutes through 67 minutes |
| 5 units: | ≥ 68 minutes through 82 minutes |
| 6 units: | ≥ 83 minutes through 97 minutes |
| 7 units: | ≥ 98 minutes through 112 minutes |
| 8 units: | ≥ 113 minutes through 127 minutes |
The pattern remains the same for treatment times in excess of 2 hours.
When more than one service represented by 15-minute timed codes is performed in a single day, the total number of minutes of service (as noted on the chart above) determines the number of timed units billed. See example 1 below.
If any 15-minute timed service that is performed for 7 minutes or less than 7 minutes on the same day as another 15-minute timed service that was also performed for 7 minutes or less and the total time of the two is 8 minutes or greater than 8 minutes, then bill one unit for the service performed for the most minutes. This is correct because the total time is greater than the minimum time for one unit. The same logic is applied when three or more different services are provided for 7 minutes or less than 7 minutes. See example 5 below.
The Outpatient Physical and Occupational, and Speech Therapy Billing Manuals, Documentation Requirements section, indicates that the amount of time for each specific intervention/modality provided to the member is required to be documented in the Visits/Encounter Note. The total number of timed minutes must be documented. These examples indicate how to count the appropriate number of units for the total therapy minutes provided.
Example 1
24 minutes of neuromuscular reeducation, code 97112,
23 minutes of therapeutic exercise, code 97110,
Total timed code treatment time was 47 minutes.
Refer to the chart above. The 47 minutes falls within the range for 3 units = 38 to 52 minutes.
Appropriate billing for 47 minutes is only 3 timed units. Each of the codes is performed for more than 15 minutes, so each shall be billed for at least 1 unit. The correct coding is 2 units of code 97112 and one unit of code 97110, assigning more timed units to the service that took the most time.
Example 2
20 minutes of neuromuscular reeducation (97112)
20 minutes therapeutic exercise (97110),
40 Total timed code minutes.
Appropriate billing for 40 minutes is 3 units. Each service was done at least 15 minutes and should be billed for at least one unit, but the total allows 3 units. Since the time for each service is the same, choose either code for 2 units and bill the other for 1 unit. Do not bill 3 units for either one of the codes.
Example 3
33 minutes of therapeutic exercise (97110),
7 minutes of manual therapy (97140),
40 Total timed minutes
Appropriate billing for 40 minutes is for 3 units. Bill 2 units of 97110 and 1 unit of 97140. Count the first 30 minutes of 97110 as two full units. Compare the remaining time for 97110 (33-30 = 3 minutes) to the time spent on 97140 (7 minutes) and bill the larger, which is 97140.
Example 4
18 minutes of therapeutic exercise (97110),
13 minutes of manual therapy (97140),
10 minutes of gait training (97116),
8 minutes of ultrasound (97035),
49 Total timed minutes
Appropriate billing is for 3 units. Bill the procedures you spent the most time providing. Bill 1 unit each of 97110, 97116, and 97140. You are unable to bill for the ultrasound because the total time of timed units that can be billed is constrained by the total timed code treatment minutes (i.e., you may not bill 4 units for less than 53 minutes regardless of how many services were performed). You would still document the ultrasound in the treatment notes.
Example 5
7 minutes of neuromuscular reeducation (97112)
7 minutes therapeutic exercise (97110)
7 minutes manual therapy (97140)
21 Total timed minutes
Appropriate billing is for one unit. The qualified professional shall select one appropriate CPT code (97112, 97110, 97140) to bill since each unit was performed for the same amount of time and only one unit is allowed.
Note: The above schedule of times is intended to provide assistance in rounding time into 15-minute increments. It does not imply that any minute until the eighth should be excluded from the total count. The total minutes of active treatment counted for all 15-minute timed codes includes all direct treatment time for the timed codes. Total treatment minutes - including minutes spent providing services represented by untimed codes - are also documented.
C. Determining What Time Counts Towards 15-Minute Timed Codes
Providers report the code for the time actually spent in the delivery of the modality requiring constant attendance and therapy services. Pre- and post-delivery services are not to be counted in determining the treatment service time. In other words, the time counted as "intra-service care" begins when the therapist or physician (or an assistant under the supervision of a physician or therapist) is directly working with the patient to deliver treatment services. The patient should already be in the treatment area (e.g., on the treatment table or mat or in the gym) and prepared to begin treatment.
The time counted is the time the patient is treated. For example, if gait training in a patient with a recent stroke requires both a therapist and an assistant, or even two therapists, to manage in the parallel bars, each 15 minutes the patient is being treated can count as only one unit of code 97116. The time the patient spends not being treated because of the need for toileting or resting should not be billed. In addition, the time spent waiting to use a piece of equipment or for other treatment to begin is not considered treatment time.
Treatment time for untimed codes is not to be counted towards the total treatment time for 15-minute unit codes.
National Correct Coding Initiative (NCCI)
National Correct Coding Initiative Procedure-To-Procedure (PTP) and Medically Unlikely Edits (MUE) edits apply to certain combinations of speech therapy procedure codes. Visit the National Correct Coding Initiative in Medicaid web page on the CMS website with edits for the NCCI Policy Manual, a complete list of impacted codes, guidance on bypass modifier uses and general information.
Policy guidance for NCCI provided in this manual does not supersede Federal NCCI policy. It is published to assist providers in understanding how the Health First Colorado Speech Therapy benefit is affected by NCCI edits and policy.
Although every effort is made to guide providers accordingly, this manual may not always reflect the most up to date NCCI policies, nor is it an exhaustive list of any edit/policy that may affect the speech therapy benefit. Providers should always reference the Medicaid website for the most current NCCI policies as those policies may change.
Health First Colorado does not create NCCI policy.
All providers are required to comply with NCCI policy.
Pursuant to the NCCI Policy Manual (Current Revision 1-1-2026, Chapter XI):
- Speech language pathologists shall not report HCPCS/CPT codes 97110, 97112, 97150, 97530, 97127 or G0515 as unbundled services included in the services coded as 92507, 92508, or 92526. (CPT code 97532 was deleted on January 1, 2018.)
- A single practitioner should not report CPT codes 92507 (treatment of speech, language, voice ..., individual) and/or 92508 (treatment of speech, language, voice . . ., group) on the same date of service as HCPCS/CPT codes 97127 (therapeutic interventions that focus on cognitive function . . .), or 97533 (sensory integrative techniques to enhance . . .), or G0515 (development of cognitive skills to improve . . .).
- However, if the two types of services are performed by different types of practitioners on the same date of service, they may be reported separately by a single billing entity. For example, if a speech language pathologist performs the procedures described by CPT codes 92507 and/or 92508 on the same date of service that an occupational therapist performs the procedures described by HCPCS/CPT codes 97127, 97533 and/or G0515, a provider entity that employs both types of practitioners may report both services utilizing an NCCI PTP-associated modifier. (CPT code 97532 was deleted on January 1, 2018.)
- Treatment of swallowing dysfunction and/or oral function for feeding (CPT code 92526) may utilize electrical stimulation. The HCPCS code G0283 (electrical stimulation (unattended), to one or more areas for indication(s) other than wound care...) should not be reported with CPT code 92526 for electrical stimulation during the procedure. The NCCI PTP edit (92526/G0283) for practitioner service claims does not allow use of NCCI PTP-associated modifiers with this edit because the same provider would never perform both of these services on the same date of service. However, the same edit for outpatient hospital facility claims does allow use of NCCI PTP-associated modifiers because two separate practitioners in the same outpatient hospital facility or institutional therapy provider might perform the two procedures for different purposes at different member encounters on the same date of service.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Prior Authorization Requests (PARs)
12 Sessions Before a PAR is Required
Effective December 1, 2023, 12 sessions of speech therapy in each rolling calendar year will be available to all members before a prior authorization request is required. One date of service is equivalent to one session, regardless of the number of units billed on one date of service. Providers are still required to reference and follow NCCI and MUE edits to avoid a claim denial.
Independent speech therapists and outpatient hospital-based therapy clinics providing outpatient speech therapy must submit, and have approved, PARs for medically necessary services prior to rendering the services when the 12 allowed sessions have been utilized. Providers are highly encouraged to submit a PAR if the member is reaching the 12 sessions mark, to avoid a lapse in services.
Prior Authorization Requests are approved for up to a 12-month period effective July 1, 2022 (depending on medical necessity determined by the authorizing agency).
- Retroactive PAR requests will be accepted for children ages 0-4 who are under the direction of the Early Intervention program. Retro-authorization requests will be approved for a window of 30 calendar days from the date on which the provider submits the PAR, even if this does not encompass the start-date of the IFSP. Dates requested on the PAR must be within the dates on the IFSP.
- Overlapping PAR request dates for same provider types will not be accepted.
- Incomplete, incorrect or insufficient member information on a PAR request form will not be accepted.
- An approved Individualized Family Service Plan serves as medical necessity, an order/prescription, and a Plan of Care.
Submit PARs for the number of units for each specific procedure code requested, not for the number of services. Modifiers must be included on both the PAR and claim submission. When submitting a PAR for either rehabilitative or habilitative services, the procedure codes must include GN + 96/97 modifiers (e.g., 92507+GN+97).
PAR submission must include either appropriate Individual Family Service Plans (IFSP) or a signed Plan of Care (POC), a.k.a., treatment plan, therapy plan, patient analysis effective July 1, 2022.
Provider Responsibility on Verification of Available Sessions
- For outpatient Speech Therapy, up to 12 sessions are allowed before a prior authorization request is required. Providers must verify available sessions in the Provider Web Portal prior to each member appointment.
- The Provider Web Portal displays current information based on claims processed to date; however, it is not a real-time tracker of units or sessions used. If a member receives services from another provided and those services billed after the Provider Web Portal is checked, before the next appointment occurs, the available session shown in the Provider Web Portal may change.
- If available sessions are exhausted, the rendering provider is responsible for submitting a PAR for any services requiring prior authorization, as identified in the applicable Allowed Code Table in this billing manual.
- Failure to verify availability prior to each visit may result in services being provided without authorization, which may lead to claims denial.
PAR Requirements
- Legibly written and signed ordering practitioner prescription, approved Plan of Care, or approved Individualized Family Service Plan, to include:
- diagnosis (preferably with ICD-10 code), and
- reason for therapy, and
- the number of requested therapy sessions per week, and
- total duration of therapy.
- The member's speech therapy treatment history, including current assessment and treatment. Include duration of previous treatment and treating diagnosis.
- Documentation indicating if the member has received PT or OT under the Home Health Program or inpatient hospital treatment.
- Current treatment diagnosis.
- Course of treatment, measurable goals and reasonable expectation of completed treatment.
- Documentation supporting medical necessity for the course and duration of treatment being requested. This may include documentation of home exercise programs.
- Assessment or progress notes submitted for documentation, must not be more than sixty (60) days prior to submission of PAR request.
- If the PAR is submitted for services delivered by an independent therapist, the name and address of the individual therapist providing the treatment must be present in field #24 of the PAR.
- The billing provider name and address needs to be present in field #25 on the PAR.
- The Health First Colorado provider number of the independent therapist must be present in PAR field #28.
- The billing provider's Health First Colorado number must be present in field #29 of the PAR.
- The authorizing agency reviews all completed PARs and approves or denies, by individual line item, each requested service or supply listed on the PAR. PAR status inquiries can be made through the Provider Web Portal and results are included in PAR letters sent to both the provider and the member. Read the results carefully as some line items may be approved and others denied. Do not render or bill for services until the PAR has been processed.
Approval of a PAR does not guarantee Health First Colorado payment and does not serve as a timely filing waiver. Prior authorization only assures that the service is considered a benefit of Health First Colorado. All claims, including those for prior authorized services, must meet eligibility and claim submission requirements (e.g., timely filing, third party resources payment pursued, required attachments included, etc.) before payment can be made.
If the PAR is denied, providers should direct inquiries to the authorizing agency, located on the Provider Contact web page of the Department's website.
The Health First Colorado PAR forms are located on the Provider Forms web page or by contacting the ColoradoPAR Program.
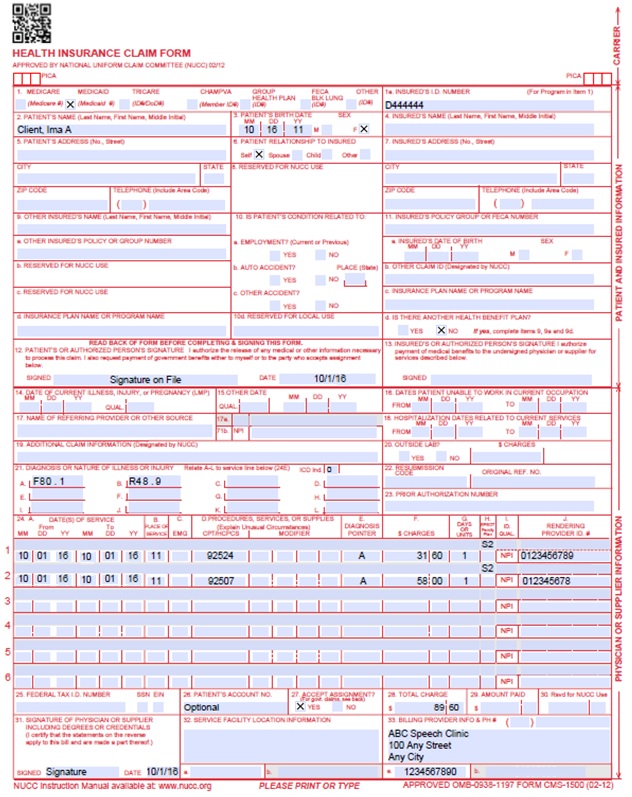
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number & Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven-digit Health First Colorado ID number as it appears on the Health First Colorado identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two digits for the month, two digits for the date, and two digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two digits for the month, two digits for the date and two digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two digits for the month, two digits for the date and two digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Required | |||||||||||||||||||||||||||||||||||||
| 17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two digits for the month, two digits for the date and two digits for the year. Example: 070116 for July 1, 2016. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one but no more than twelve diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six lines of information on the paper claim. If more than six lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two dates: a "From" date of services and a "To" date of service. Enter the date of service using two digits for the month, two digits for the date and two digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
Single Date of Service: Enter the six-digit date of service in the "From" field. Completion of the "To" field is not required. Do not spread the date entry across the two fields.
VP - Vendor Product Number | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes. Refer to the Allowed Place of Service Codes section in this manual. | ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the procedure code that specifically describes the service for which payment is requested. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four modifiers may be entered when using the paper claim form. Refer to the Allowed Place of Service Codes section in this manual. | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of 4 characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | General Instructions | A unit represents the number of times the described procedure or service was rendered. Except as instructed in this manual or in Health First Colorado bulletins, the billed unit must correspond to procedure code descriptions. The following examples show the relationship between the procedure description and the entry of units. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early & Periodic Screening, Diagnosis, and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available- Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) Not Required | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two digits for the month, two digits for the date and two digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
CMS 1500 Speech Therapy Claim Example
UB-04 Paper Claim Reference Table
Speech therapy outpatient hospital paper claims must be submitted on the UB-04 claim form.
The information in the following table provides instructions for completing form locators (FL) as they appear on the paper UB-04 claim form. Instructions for completing the UB-04 claim form are based on the current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data form locators on the UB-04 have the same attributes (specifications) for Health First Colorado as those indicated in the NUBC UB-04 Reference Manual.
All code values listed in the NUBC UB-04 Reference Manual for each form locator may not be used for submitting paper claims to Health First Colorado. The appropriate code values listed in this manual must be used when billing Health First Colorado.
The UB-04 Institutional Certification Form, located on the Provider Forms web page under the Claim Forms and Attachments drop-down menu, must be completed and attached to all claims submitted on the paper UB-04. Completed UB-04 paper Health First Colorado claims, including hardcopy Medicare claims, should be mailed to the correct fiscal agent address listed in Appendix A, under the Appendices drop-down menu on the Billing Manuals web page.
Do not submit "continuation" claims. Each claim form has a set number of billing lines available for completion. Do not crowd more lines on the form.
Billing lines in excess of the designated number are not processed or acknowledged. Claims with more than one page may be submitted through the Provider Web Portal.
Bill with a date span (From and To dates of service) only if the service was provided every consecutive day within the span. The From and To dates must be in the same month.
The Paper Claim Reference Table below lists the required, optional and/or conditional form locators for submitting the paper UB-04 claim form to Health First Colorado for nursing facility services.
| Form Locator and Labels | Completion Format | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Billing Provider Name, Address, Telephone Number | Text | Required
Abbreviate the state using standard post office abbreviations. Enter the telephone number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Pay-to Name, Address, City, State | Text | Required only if different from FL 1.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3a. Patient Control Number | Up to 20 characters: Letters, numbers or hyphens | Optional Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3b. Medical Record Number | 17 digits | Optional Enter the number assigned to the member to assist in retrieval of medical records. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Type of Bill | 3 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Federal Tax Number | None | Not Required Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Statement covers period From/Through | From:6 digits MMDDYY Through: 6 digits MMDDYY | Required (Note: OP claims cannot span over a month's end) Enter the From (beginning) date and Through (ending) date of service covered by this bill. Example: 01012018 = January 1, 2018 This form locator must reflect the beginning and ending dates of service. When span billing for multiple dates of service and multiple procedures, complete FL 45 (Service Date). Providers not wishing to span bill following these guidelines, must submit one claim per date of service. "From" and "Through" dates must be the same. All line item entries must represent the same date of service. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8a. Patient Identifier | Text | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8b. Patient Name | Up to 25 characters, letters & spaces | Required Enter the member's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Patient Address - Street | Characters Letters & numbers | Required Enter the member's street/post office box as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Patient Address - City | Text | Required Enter the member's city as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Patient Address - State | Text | Required Enter the member's state as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Patient Address - ZIP | Digits | Required Enter the member's zip code as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9e. Patient Address - Country Code | Digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10. Birthdate | 8 digits (MMDDCCYY) | Required Enter the member's birthdate using two digits for the month, two digits for the date, and four digits for the year (MMDDCCYY format). Example: 01012015 for January 1, 2015. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Patient Sex | 1 letter | Required Enter an M (male) or F (female) to indicate the member's sex. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Admission Date | 6 digits | Conditional Required for observation holding beds only. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Admission Hour | 6 digits | Conditional Required for observation holding beds only. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Admission Type | 1 digit | Required Enter the following to identify the admission priority: 1 - Emergency Member requires immediate intervention as a result of severe, life threatening or potentially disabling conditions. Exempts inpatient hospital & clinic claims from co-payment and PCP referral. Exempts outpatient hospital claims from co-payment and PCP only if revenue code 450 or 459 is present. This is the only benefit service for an undocumented alien. If span billing, emergency services cannot be included in the span bill and must be billed separately from other outpatient services. 2 - Urgent The member requires immediate attention for the care and treatment of a physical or mental disorder. 3 - Elective The member's condition permits adequate time to schedule the availability of accommodations. 4 - Newborn Required for inpatient and outpatient hospital. 5 - Trauma Center Visit to a trauma center/hospital as licensed or designated by the state or local government authority authorized to do so, or as verified by the American College of Surgeons and involving trauma activation. Clinics Required only for emergency visit. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Source of Admission | 1 digit | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Discharge Hour | 2 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Patient Discharge Status | 2 digits | Conditional
Use code 02 for a PPS hospital transferring a member to another PPS hospital. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18-28. Conditions Codes | 2 digits | Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Accident State | 2 digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31 - 34. Occurrence Code/Date | 2 digits & 6 digits | Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35-36. Occurrence Span Code From/ Through | 2 Digits and 6 Digits | Leave blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38. Responsible Party Name/Address | None | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39 - 41. Value Codes and Amounts | 2 characters and up to 9 digits | Conditional
For Rancho Coma Score bill with appropriate diagnosis for head injury. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 42. Revenue Code | 4 digits | Required Enter the revenue code 0911. A revenue code must appear only once per date of service. If more than one of the same service is provided on the same day, combine the units and charges on one line accordingly. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 43. Revenue code Description | Text | Required Enter the revenue code description or abbreviated description. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 44. HCPCS/Rates/ HIPPS Rate Codes | 5 digits | Conditional
HCPCS codes cannot be repeated for the same date of service. Combine the units in FL 46 (Service Units) to report multiple services.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 45. Service Date | 6 digits | For span bills only Enter the date of service using MMDDYY format for each detail line completed. Each date of service must fall within the date span entered in the "Statement Covers Period" field (FL 6). Not required for single date of service claims | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 46. Service Units | 3 digits | Required Enter a unit value on each line completed. Use whole numbers only. Do not enter fractions or decimals and do not show a decimal point followed by a 0 to designate whole numbers (e.g., Do not enter 1.0 to signify one unit). The grand total line (Line 23) does not require a unit value. For span bills, the units of service reflect only those visits, miles or treatments provided on dates of service in FL 45. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 47. Total Charges | 9 digits | Required Enter the total charge for each line item. Calculate the total charge as the number of units multiplied by the unit charge. Do not subtract Medicare or third-party payments from line charge entries. Do not enter negative amounts. A grand total on line 23 is required for all charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 48. Non-covered Charges | Up to 9 digits | Conditional Enter incurred charges that are not payable by Health First Colorado. Non-covered charges must be entered in both FL 47 (Total Charges) and FL 48 (Non-Covered Charges.) Each column requires a grand total. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 50. Payer Name | 1 letter and text | Enter the payment source code followed by name of each payer organization from which the provider might expect payment.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 51. Health Plan ID | 8 digits | Required Enter the provider's Health Plan ID for each payer name. Enter the eight-digit Health First Colorado provider number assigned to the billing provider. Payment is made to the enrolled provider or agency that is assigned this number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 52. Release of Information | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 53. Assignment of Benefits | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 54. Prior Payments | Up to 9 digits | Inpatient - Conditional Complete when there are Medicare or third-party payments. Enter third party and/or Medicare payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 55. Estimated Amount Due | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter the net amount due from Health First Colorado after provider has received other third party, Medicare or member liability amount. Medicare Crossovers Enter the sum of the Medicare coinsurance plus Medicare deductible less third-party payments and member payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 56. National Provider Identifier (NPI) | 10 digits | Required Enter the billing provider's 10-digit National Provider Identifier (NPI). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 57. Other Provider ID | Optional Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 58. Insured's Name | Up to 30 characters | Required Enter the member's name on the Health First Colorado line. Other Insurance/Medicare Complete additional lines when there is third party coverage. Enter the policyholder's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 60. Insured's Unique ID | Up to 20 characters | Required Enter the insured's unique identification number assigned by the payer organization exactly as it appears on the health insurance card. Include letter prefixes or suffixes shown on the card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 61. Insurance Group Name | 14 letters | Conditional Complete when there is third party coverage. Enter the name of the group or plan providing the insurance to the insured exactly as it appears on the health insurance card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 62. Insurance Group Number | 17 digits | Conditional Complete when there is third party coverage. Enter the identification number, control number, or code assigned by the carrier or fund administrator identifying the group under which the individual is carried. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 63. Treatment Authorization Code | Up to 18 characters | Conditional Complete when the service requires a PAR. Enter the authorization number in this FL if a PAR is required and has been approved for services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 64. Document Control Number | none | Conditional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 65. Employer Name | Text | Conditional Complete when there is third party coverage. Enter the name of the employer that provides health care coverage for the individual identified in FL 58 (Insured Name). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 66. Diagnosis Version Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67. Principal Diagnosis Code | Up to 6 digits | Required Enter the exact diagnosis code describing the principal diagnosis that exists at the time of admission or develops subsequently and affects the length of stay. Do not add extra zeros to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67A. - 67Q. - Other Diagnosis | 6 digits | Optional Enter the exact diagnosis code corresponding to additional conditions that co-exist at the time of admission or develop subsequently and which effect the treatment received or the length of stay. Do not add extra zeros to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 69. Admitting Diagnosis Code | 6 digits | Optional Enter the diagnosis code as stated by the physician at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 70. Patient Reason Diagnosis | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 71. PPS Code | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 72. External Cause of Injury code (E-Code) | 6 digits | Optional Enter the diagnosis code for the external cause of an injury, poisoning, or adverse effect. This code must begin with an "E". | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74. Principal Procedure Code/Date | 7 characters and 6 digits | Conditional Enter the procedure code for the principal procedure performed during this billing period and the date on which procedure was performed. Enter the date using MMDDYY format. Apply the following criteria to determine the principle procedure: The principal procedure is not performed for diagnostic or exploratory purposes. This code is related to definitive treatment, and The principal procedure is most related to the primary diagnosis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74A. Other Procedure Code/Date | 7 characters and 6 digits | Conditional Complete when there are additional significant procedure codes. Enter the procedure codes identifying all significant procedures other than the principle procedure and the dates on which the procedures were performed. Report those that are most important for the episode of care and specifically any therapeutic procedures closely related to the principle diagnosis. Enter the date using MMDDYY format. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 76. Attending NPI - Conditional QUAL - conditional ID - (Health First Colorado Provider #) - Required Attending- Last/First Name | NPI - 10 digits | Health First Colorado ID Required NPI - Enter the 10-digit NPI number assigned to the physician having primary responsibility for the member's medical care and treatment. This number is obtained from the physician and cannot be a clinic or group number. (If the attending physician is not enrolled in Health First Colorado or if the member leaves the ER before being seen by a physician, the hospital may enter their individual numbers.) Hospitals and FQHCs may enter the member's regular physician's 10- digit NPI in the Attending Physician ID form locator if the locum tenens physician is not enrolled in Health First Colorado. QUAL - Enter "1D" for Health First Colorado Enter the attending physician's last and first name. This form locator must be completed for all services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 77. Operating NPI | Not required Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 78 - 79. Other ID NPI - Required QUAL - Required ID - (Health First Colorado Provider #) - Required | NPI - 10 digits | Required Complete when attending physician is not the PCP or to identify additional physicians. NPI - Enter up to two 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attending physician is not the PCP or if a clinic is a PCP agent, enter the PCP NPI number as the referring physician. The name of the Health First Colorado member's PCP appears on the eligibility verification. Review either for eligibility or PCP. Health First Colorado does not require that the PCP number appear more than once on each claim submitted. The attending physician's last and first name are optional. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 80. Remarks | Text | Optional Enter specific additional information necessary to process the claim or fulfill reporting requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 81. Code - QUAL/CODE/VALUE (a-d) | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
UB-04 Outpatient Speech Therapy Claim Example
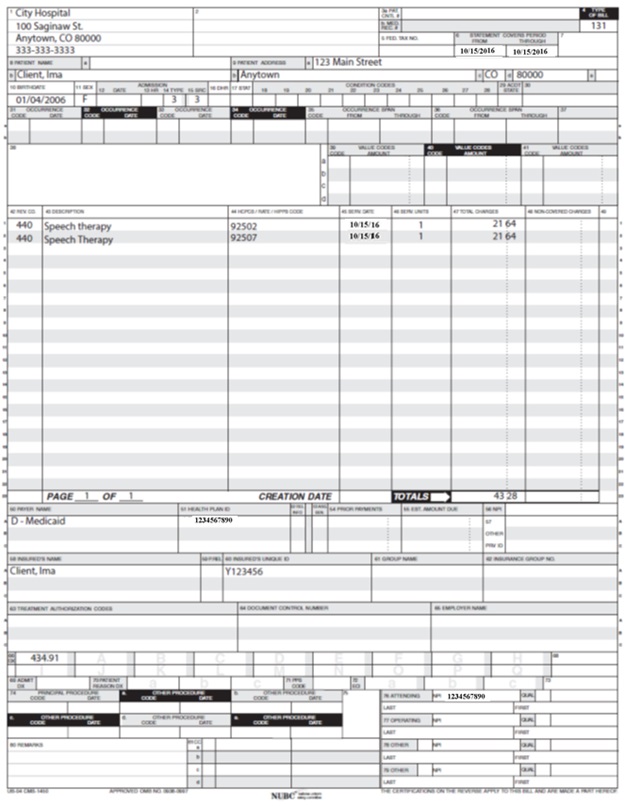
Institutional Provider Certification
The Institutional Provider Certification form is available on the Provider Forms web page under the Claim Forms and Attachments drop-down menu.
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
Speech Therapy Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 3/7/2017 | Clarified billing for assistants, clinical fellows. Clarified PAR documentation requirements. Updated eligibility message for HPE response. | HCPF |
| 5/26/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 8/22/2017 | Organizational updates, clarification on CCBs as referring providers for IFSP early intervention services | HCPF |
| 1/15/2018 | Organizational updates, inclusion of documentation policy, incorporation of policy from the Speech-language and Hearing Services Benefit Coverage Standard. Revision of coding table for 2018 HCPCS changes. Updated page numbering system so that document page number matched the actual page number. | HCPF |
| 2/22/2018 | Removed NDC supplemental qualifier - not relevant for speech therapy providers | DXC |
| 6/15/2018 | Updated timely filing information and removed references to LBOD, removed general billing information already available in the General Provider Information manual | DXC |
| 10/19/2018 | Updated coding table. Code descriptions removed. Providers must reference coding resources for full descriptions. | HCPF |
| 12/20/2018 | Clarification to signature requirements | HCPF |
| 1/24/2019 | Updated visit note documentation requirements to require SOAP format, updated procedure code table with current PAR status, updated Prior Authorization Requirements section. Updated NCCI reference language to match current NCCI manual revision 2019. | HCPF |
| 1/25/2019 | Added link to Provider Forms for Institutional Provider certification | HCPF |
| 2/13/2019 | Revised the amount of NCCI language copied from the NCCI manual. Add 96112 to coding table (new in 2019) | HCPF |
| 4/4/2019 | Incorporated in-home care provider requirements from rule, added 96112 and 96113 to procedure code table. | HCPF |
| 7/10/2019 | Updated Appendices links and verbiage | DXC |
| 9/23/2019 | Added reporting units of service instruction from October 2019 special provider bulletin | HCPF |
| 10/8/2019 | Updated retro PAR policy for EI program to be 30 calendar days not dependent on IFSP start date. | HCPF |
| 1/2/2020 | Converted to web page | HCPF |
| 2/14/2020 | Update to coding table for G0515 97129 97130. | HCPF |
| 4/27/2020 | Updated 'Visit/Encounter Notes' section in Documentation Requirements to match Outpatient PT/OT policy. Other note formats like APSO, instead of strictly SOAP, are allowed effective 5/1/20. | HCPF |
| 6/4/2020 | Revised SLP qualifications to refer to SLP Practice Act. Fixed hyperlink. Included field 17.b instruction for OPR policy. | HCPF |
| 7/13/2020 | Revised SLPA qualifications to practice under supervision of a licensed SLP. Added POS 13 to allowed POS code table. | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 12/16/2020 |
| HCPF |
| 4/23/2021 |
| HCPF |
| 7/2/2021 | Added EPSDT policy reference | HCPF |
| 10/5/2021 | Updated SLPA supervision reference to CCR change. | HCPF |
| 3/1/2022 | • Added co-treatment policy. • Moved NCCI section to be below the co-treatment policy section. • Included reference to home exercise programs in PAR section. | HCPF |
| 4/5/2022 | • Clarified PAR policies for Early Intervention requests. | HCPF |
| 5/3/2022 | Clarified Early Intervention PARs for Children ages 0-4 | HCPF |
| 6/6/2022 | Added Speech Therapy for Gender Dysphoria Diagnosis to “Covered Services” | HCPF |
| 6/6/2022 | Added POS 10 to Coding Table | HCPF |
| 6/6/2022 | Changed 6-month PAR policy to 12-month PAR policy effective 7/1/22 | HCPF |
| 3/27/2023 | Updated AWS URL Links | HCPF |
| 9/5/2023 | Changed claim requirements per the OPR project | HCPF |
| 11/21/2023 | Added 12 sessions before a PAR is required | HCPF |
| 1/10/2024 | Added clarification of rolling calendar year for 12 sessions | HCPF |
| 4/18/2024 | Updated Early Intervention under General Benefits | HCPF |
| 07/25/2024 | Add place of service 03 information | HCPF |
| 01/08/2025 | Removal of “The claim must contain the PAR number for payment” guidance. Removal of hippotherapy is considered experimental and not covered guidance. | HCPF |
| 06/30/2025 | Added new policy of adult habilitative speech therapy | HCPF |
| 01/22/2026 | Addition of provider responsibility to verify available sessions | HCPF |