Telemedicine and eConsult Billing Manual
- General Billing Information
- Telemedicine Overview
- Health First Colorado Reimbursement for Telemedicine
- Telemedicine for Primary Care Providers
- Telemedicine for Specialty Care Providers
- Telemedicine for Federally Qualified Health Centers, Rural Health Clinics and Indian Health Services
- Physical Therapy, Occupational Therapy, Home Health, Hospice and Pediatric Behavioral Therapy Providers
- Allowable Locations for Telemedicine
- Telemedicine Confidentiality Requirements
- Waiving the Face-to-Face Requirement & Required Disclosure Statements
- Telemedicine Billing Procedure Codes
- Billing Providers
- Originating Site Billing
- Distant Providers
- Billing HCPCS Q3014
- Telemedicine Place of Service Codes
- Rendering Providers
- Remote Patient Monitoring
- eConsults Overview
- CMS 1500 Paper Claim Reference Table
- Timely Filing
- Telemedicine Revision Log
Return to Billing Manuals Web Page
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page for general billing information.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
8.280.4.E Other EPSDT Benefits
Other health care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Section 1905(a) of the Social Security Act are a covered benefit under EPSDT when medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, regardless of whether such goods and services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a good or service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one or more Activities of Daily Living; and meets the criteria set forth at Section 8.076.1.8.b - g.
- The service provides a safe environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly.
Telemedicine Overview
Telemedicine is not a unique service, but a means of providing services approved by Health First Colorado through live interactive audio and video telecommunications equipment.
Telemedicine services may be provided under two arrangements:
- A member receives services via a live audio/visual connection from a single provider; or
- A member and a provider are physically in the same location and additional services are provided by a second (distant) provider via a live audio/visual connection. In this arrangement the provider who is present with the member is the originating provider, and the provider located at a different site, acting as a consultant, is called the distant provider.
The member must be present during telemedicine visits.
Providers should refer to the Code of Colorado Regulations Program Rules (10 CCR 2505-10, Section 8.095), for specific information when providing telemedicine services.
Telehealth Home Health Monitoring
Telehealth monitoring is available for members who are eligible through the Home Health benefit and should not be billed as telemedicine. Providers rendering telehealth monitoring should refer to the Home Health Billing Manual located on the Billing Manuals web page under the CMS 1500 drop-down menu.
eHealth Entity Provider Specialty Type
As of October 30th, 2022, there is a provider specialty type for Clinic and Non-Physician Practitioner groups that meet the following definition:
An eHealth entity is defined as a group practice that delivers services exclusively through telemedicine and is enrolled in a provider type that has an eHealth specialty.
Refer to the Code of Colorado Regulations (1- CCR 2505-10, Section 8.095) for more information. Providers who meet this definition must update their enrollment to this provider specialty type. Visit the Provider Enrollment web page for guidance on how to enroll. Services are restricted to those currently allowed for telemedicine. This information is located under Covered Services.
Requirements for Telemedicine Services
It is acceptable to use telemedicine to facilitate live contact directly between a member and a provider. Services can be provided between a member and a distant provider when a member is in their home or other location of their choice. Additionally, the distant provider may participate in the telemedicine interaction from any appropriate location.
Other standard requirements for telemedicine services include:
- The reimbursement rate for a telemedicine service shall, as a minimum, be set at the same rate as the medical assistance program rate for a comparable in-person service. [C. R. S. 2017, 25.5-5-320(2)].
- Providers may only bill procedure codes which they are already eligible to bill.
- Any health benefits provided through telemedicine shall meet the same standard of care as in-person care.
- For initial visits, providers must comply with the requirements posted under Waiving the Face-to-Face Requirement & Required Disclosure Statements. For each subsequent visit, providers must document the member's consent, either verbal or written, to receive telemedicine services.
- Contact with the provider must be initiated by the member for the service rendered.
- The availability of services through telemedicine in no way alters the scope of practice of any health care provider, nor does it authorize the delivery of health care services in a setting or manner not otherwise authorized by law.
- Services not otherwise covered by Health First Colorado are not covered when delivered via telemedicine.
- The use of telemedicine does not change prior authorization requirements that have been established for the services being provided.
- Record-keeping and patient privacy standards should comply with normal Medicaid requirements and HIPAA.
Covered Services
See Telemedicine - General Billing Information for a list of billing codes which may be used with Place of Service (POS) 02 or 10.
Services may be rendered via telemedicine when the service is:
- A covered Health First Colorado benefit,
- Within the scope and training of an enrolled provider's license, and
- Appropriate to be rendered via telemedicine.
All services provided through telemedicine shall meet the same standard of care as in-person care.
The availability of services through telemedicine in no way alters the scope of practice of any health care provider, nor does it authorize the delivery of health care services in a setting or manner not otherwise authorized by law. [C. R. S. 2018, 25.5-5-414 (7)(a) & (b)
Non-Covered Services
- Services not otherwise covered by Health First Colorado are not covered when delivered via telemedicine
- Telemedicine does not include provider-to-provider consultations provided by telephone (interactive audio), email or facsimile machines.
- Services appropriately billed to managed care should continue to be billed to managed care. All managed care requirements must be met for services billed to managed care. Managed care may or may not reimburse telemedicine costs.
- Health First Colorado does not pay for provider education via telemedicine.
- The use of telecommunications equipment for delivery of services does not change prior authorization requirements established for the services being provided.
Hospital Services Rendered via Telemedicine
Only Physical Therapy (PT), Occupational Therapy (OT), and Speech Language Pathology (SLP) when rendered via telemedicine are allowed to be billed on an outpatient hospital claim. Services which may be rendered via telemedicine are outlined below in the Telemedicine Billing Procedure Codes.
Health First Colorado Reimbursement for Telemedicine
Telemedicine for Primary Care Providers
A primary care provider can be reimbursed as the "originating provider" for any eligible Telemedicine Services where the member is present with the provider at the "originating site." Please see the 'Originating Site Billing' section for further information on reimbursement requirements for providers at an originating site with a member.
In order for a primary care provider to be reimbursed for Telemedicine Services as the "distant provider" the primary care provider must be able to facilitate an in-person visit in the state of Colorado if necessary for treatment of the member's condition. Please see the 'Distant Provider Billing' section for further information.
Telemedicine for Specialty Care Providers
A medical specialist provider can be reimbursed as the "originating provider" for any Telemedicine Services where the member is present with the provider at the "originating site." Please see the 'Originating Site Billing' section for further information on reimbursement requirements for providers at an originating site with a member.
A medical specialist provider can be reimbursed as the "distant provider." Please see the 'Distant Provider Billing' section for further information.
Telemedicine for Federally Qualified Health Centers, Rural Health Clinics, and Indian Health Services
Health First Colorado allows telemedicine visits to qualify as billable encounters for Federally Qualified Health Centers (FQHCs), Rural Health Clinic (RHCs), and Indian Health Services (IHS). Services allowed under telemedicine may be provided via telephone, live chat, or interactive audiovisual modality for these provider types.
When a Federally Qualified Health Center (FQHC) or a Rural Health Clinic (RHC) provides care through telemedicine, the claim must include the modifier GT on line(s) identifying the service(s). The claims must follow the other requirements of an FQHC or RHC claim as identified in the FQHC and RHC Billing Manual.
Physical Therapy, Occupational Therapy, Home Health, Hospice and Pediatric Behavioral Therapy Providers
Physical therapists, occupational therapists, hospice, home health providers and pediatric behavioral therapy providers are eligible to deliver telemedicine services.
- Home Health Agency services and therapies, Hospice, and Pediatric Behavioral Treatment may be provided via any telemedicine modality.
- Outpatient Physical, Occupational, and Speech Therapy services must have an interactive audio/visual connection with the member to be provided via telemedicine.
Telemedicine is covered for behavioral therapy providers under the capitated behavioral health benefit administered by the Regional Accountable Entities (RAEs). Behavioral health providers should contact their RAE for guidance. Visit the Accountable Care Collaborative Phase II web page for more information.
Allowable Locations for Telemedicine
If no originating provider is present during a Telemedicine Services appointment, then the location of the originating site is at the member's discretion and can include the member's home. However, members can be required to choose a location suitable to delivery of telemedicine services that may include adequate lighting and environmental noise levels suitable for easy conversation with a provider.
Telemedicine Confidentiality Requirements
All Health First Colorado providers using telemedicine to deliver Health First Colorado services must employ existing quality-of-care protocols and member confidentiality guidelines when providing telemedicine services. Health benefits provided through telemedicine must meet the same standard of care as in-person care. Record-keeping should comply with Health First Colorado requirements in 10 CCR 2505-10, Section 8.130.2.
Transmissions must be performed on dedicated secure lines or must utilize an acceptable method of encryption adequate to protect the confidentiality and integrity of the transmission. Transmissions must employ acceptable authentication and identification procedures by both the sender and the receiver. Providers of telemedicine services must implement confidentiality procedures that include, but are not limited to:
- Specifying the individuals who have access to electronic records
- Using unique passwords or identifiers for each employee or other person with access to the member records
- Ensuring a system to routinely track and permanently record such electronic medical information
- Advising members of their right to privacy and that their selection of a location to receive telemedicine services in private or public environments is at the member's discretion
Waiving the Face-to-Face Requirement & Required Disclosure Statements
The Health First Colorado requirement for an initial face-to-face contact between provider and member may be waived when treating the member through telemedicine. In-person contact between a health care provider and a member is not required for services delivered through telemedicine that are otherwise eligible for reimbursement.
Prior to treating the member through telemedicine for the first time, the provider must furnish each member with all of the following written statements, which must be signed (electronic signatures will be accepted) by the member or the member's legal representative:
- The member retains the option to refuse the delivery of health care services via telemedicine at any time without affecting the member's right to future care or treatment and without risking the loss or withdrawal of any program benefits to which the member would otherwise be entitled.
- All applicable confidentiality protections shall apply to the services.
- The members shall have access to all medical information resulting from the telemedicine services as provided by applicable law for member access to his or her medical records. [C. R. S. 2018, 25.5-5-320 (4)].
These requirements do not apply in an emergency. [C. R. S. 2018, 25.5-5-320 (5)].
Telemedicine Billing Procedure Codes
Specific coverage and billing information may exist for the benefit being provided via Telemedicine. Refer to the Billing Manuals web page for benefit-specific details.
The following list of CPT/HCPCS codes are allowable via telemedicine. When delivered via telemedicine Place of Service code 02 or 10 must be used:
| Procedure Code | Date Allowed for Telemedicine | Allowed for FQHC, RHC, IHS Telemedicine Billing | Allowed for Outpatient Hospital Telemedicine Billing |
|---|---|---|---|
| 76801 | Prior to March 20, 2020 | Yes | No |
| 76802 | Prior to March 20, 2020 | Yes | No |
| 76805 | Prior to March 20, 2020 | Yes | No |
| 76811 | Prior to March 20, 2020 | Yes | No |
| 76812 | Prior to March 20, 2020 | Yes | No |
| 76813 | Prior to March 20, 2020 | Yes | No |
| 76814 | Prior to March 20, 2020 | Yes | No |
| 76815 | Prior to March 20, 2020 | Yes | No |
| 76816 | Prior to March 20, 2020 | Yes | No |
| 76817 | Prior to March 20, 2020 | Yes | No |
| 90791 | Prior to March 20, 2020 | Yes | No |
| 90792 | Prior to March 20, 2020 | Yes | No |
| 90832 | Prior to March 20, 2020 | Yes | No |
| 90833 | Prior to March 20, 2020 | Yes | No |
| 90834 | Prior to March 20, 2020 | Yes | No |
| 90836 | Prior to March 20, 2020 | Yes | No |
| 90837 | Prior to March 20, 2020 | Yes | No |
| 90838 | Prior to March 20, 2020 | Yes | No |
| 90839 | Prior to March 20, 2020 | Yes | No |
| 90840 | Prior to March 20, 2020 | Yes | No |
| 90846 | Prior to March 20, 2020 | Yes | No |
| 90847 | Prior to March 20, 2020 | Yes | No |
| 90849 | Prior to March 20, 2020 | Yes | No |
| 90853 | Prior to March 20, 2020 | Yes | No |
| 90863 | Prior to March 20, 2020 | Yes | No |
| 92507 | Prior to March 20, 2020 | Yes | Yes |
| 92508 | March 20, 2020 | Yes | Yes |
| 92521 | March 20, 2020 | Yes | Yes |
| 92522 | March 20, 2020 | Yes | Yes |
| 92523 | March 20, 2020 | Yes | Yes |
| 92524 | March 20, 2020 | Yes | Yes |
| 92526 | March 20, 2020 | Yes | Yes |
| 92606 | March 20, 2020 | Yes | Yes |
| 92607 | March 20, 2020 | Yes | Yes |
| 92608 | March 20, 2020 | Yes | Yes |
| 92609 | March 20, 2020 | Yes | Yes |
| 92610 | March 20, 2020 | Yes | Yes |
| 92630 | March 20, 2020 | Yes | No |
| 92633 | March 20, 2020 | Yes | No |
| 96040 | March 20, 2020 | Yes | No |
| 96101 | March 20, 2020 | Yes | No |
| 96102 | March 20, 2020 | Yes | No |
| 96110 | March 20, 2020 | Yes | Yes |
| 96111 | March 20, 2020 | Yes | Yes |
| 96112 | March 20, 2020 | Yes | Yes |
| 96113 | March 20, 2020 | Yes | Yes |
| 96116 | March 20, 2020 | Yes | No |
| 96118 | March 20, 2020 | Yes | No |
| 96119 | March 20, 2020 | Yes | No |
| 96121 | March 20, 2020 | Yes | No |
| 96125 | March 20, 2020 | Yes | No |
| 96130 | March 20, 2020 | Yes | No |
| 96131 | March 20, 2020 | Yes | No |
| 96132 | March 20, 2020 | Yes | No |
| 96133 | March 20, 2020 | Yes | No |
| 96136 | March 20, 2020 | Yes | No |
| 96137 | March 20, 2020 | Yes | No |
| 96138 | March 20, 2020 | Yes | No |
| 96139 | March 20, 2020 | Yes | No |
| 96146 | March 20, 2020 | Yes | No |
| 97110 | March 20, 2020 | Yes | Yes |
| 97112 | March 20, 2020 | Yes | Yes |
| 97129 | March 20, 2020 | Yes | Yes |
| 97130 | March 20, 2020 | Yes | Yes |
| 97140 | March 20, 2020 | Yes | Yes |
| 97150 | March 20, 2020 | Yes | Yes |
| 97151 | March 20, 2020 | Yes | No |
| 97153 | March 20, 2020 | Yes | No |
| 97154 | March 20, 2020 | Yes | No |
| 97155 | March 20, 2020 | Yes | No |
| 97158 | March 20, 2020 | Yes | No |
| 97161 | March 20, 2020 | Yes | Yes |
| 97162 | March 20, 2020 | Yes | Yes |
| 97163 | March 20, 2020 | Yes | Yes |
| 97164 | March 20, 2020 | Yes | Yes |
| 97165 | March 20, 2020 | Yes | Yes |
| 97166 | March 20, 2020 | Yes | Yes |
| 97167 | March 20, 2020 | Yes | Yes |
| 97168 | March 20, 2020 | Yes | Yes |
| 97530 | March 20, 2020 | Yes | Yes |
| 97533 | March 20, 2020 | Yes | Yes |
| 97535 | March 20, 2020 | Yes | Yes |
| 97537 | March 20, 2020 | Yes | Yes |
| 97542 | March 20, 2020 | Yes | Yes |
| 97755 | March 20, 2020 | Yes | Yes |
| 97760 | March 20, 2020 | Yes | Yes |
| 97761 | March 20, 2020 | Yes | Yes |
| 97763 | March 20, 2020 | Yes | Yes |
| 97802 | March 20, 2020 | Yes | No |
| 97803 | March 20, 2020 | Yes | No |
| 97804 | March 20, 2020 | Yes | No |
| 98000 | January 1, 2025 | Yes | Yes |
| 98001 | January 1, 2025 | Yes | Yes |
| 98002 | January 1, 2025 | Yes | No |
| 98003 | January 1, 2025 | Yes | No |
| 98004 | January 1, 2025 | Yes | No |
| 98005 | January 1, 2025 | Yes | Yes |
| 98006 | January 1, 2025 | Yes | Yes |
| 98007 | January 1, 2025 | Yes | No |
| 98008 | January 1, 2025 | Yes | No |
| 98009 | January 1, 2025 | Yes | No |
| 98010 | January 1, 2025 | Yes | No |
| 98011 | January 1, 2025 | Yes | Yes |
| 98012 | January 1, 2025 | Yes | No |
| 98013 | January 1, 2025 | Yes | No |
| 98014 | January 1, 2025 | Yes | No |
| 98015 | January 1, 2025 | Yes | No |
| 98016 | January 1, 2025 | Yes | No |
| 98966 | March 20, 2020 | Yes | No |
| 98967 | March 20, 2020 | Yes | No |
| 98968 | March 20, 2020 | Yes | No |
99091 | July 1, 2025 | Yes | No |
| 99201 | Prior to March 20, 2020 | Yes | No |
| 99202 | Prior to March 20, 2020 | Yes | No |
| 99203 | Prior to March 20, 2020 | Yes | No |
| 99204 | Prior to March 20, 2020 | Yes | No |
| 99205 | Prior to March 20, 2020 | Yes | No |
| 99211 | Prior to March 20, 2020 | Yes | No |
| 99212 | Prior to March 20, 2020 | Yes | No |
| 99213 | Prior to March 20, 2020 | Yes | No |
| 99214 | Prior to March 20, 2020 | Yes | No |
| 99215 | Prior to March 20, 2020 | Yes | No |
| 99401 | March 20, 2020 | Yes | No |
| 99402 | March 20, 2020 | Yes | No |
| 99403 | March 20, 2020 | Yes | No |
| 99404 | March 20, 2020 | Yes | No |
| 99406 | March 20, 2020 | Yes | No |
| 99407 | March 20, 2020 | Yes | No |
| 99408 | March 20, 2020 | Yes | No |
| 99409 | March 20, 2020 | Yes | No |
| 99417 | January 1, 2021 | Yes | No |
| 99441 | March 20, 2020 | Yes | No |
| 99442 | March 20, 2020 | Yes | No |
| 99443 | March 20, 2020 | Yes | No |
99453 | July 1, 2025 | Yes | No |
99454 | July 1, 2025 | Yes | No |
99457 | July 1, 2025 | Yes | No |
99458 | July 1, 2025 | Yes | No |
G0011 | September 30, 2024 | Yes | No |
G0013 | September 30, 2024 | Yes | No |
G0108 | March 20, 2020 | Yes | No |
G0109 | March 20, 2020 | Yes | No |
G0310 | April 1, 2021 | Yes | No |
G0311 | April 1, 2021 | Yes | No |
G0312 | April 1, 2021 | Yes | No |
G0313 | April 1, 2021 | Yes | No |
G0314 | April 1, 2021 | Yes | No |
G0315 | April 1, 2021 | Yes | No |
G0447 | April 1, 2025 | Yes | No |
| G8431 | March 20, 2020 | Yes | No |
| G8510 | March 20, 2020 | Yes | No |
| G9006 | March 20, 2020 | Yes | No |
| H0001 | March 20, 2020 | Yes | No |
| H0002 | March 20, 2020 | Yes | No |
| H0004 | March 20, 2020 | Yes | No |
| H0006 | March 20, 2020 | Yes | No |
| H0025 | March 20, 2020 | Yes | No |
| H0031 | March 20, 2020 | Yes | No |
| H0032 | March 20, 2020 | Yes | No |
| H0049 | March 20, 2020 | Yes | No |
| H1005 | March 20, 2020 | Yes | No |
| H2000 | March 20, 2020 | Yes | No |
| H2011 | March 20, 2020 | Yes | No |
| H2015 | March 20, 2020 | Yes | No |
| H2016 | March 20, 2020 | Yes | No |
S9443 | December 1, 2024 | Yes | No |
| S9445 | March 20, 2020 | Yes | No |
| S9485 | March 20, 2020 | Yes | No |
| T1017 | March 20, 2020 | Yes | No |
| V5011 | March 20, 2020 | Yes | No |
Billing Providers
Telemedicine services will only be reimbursed for providers who are enrolled in Health First Colorado at the time of service.
The availability of services through telemedicine in no way alters the scope of practice of any health care provider, nor does it authorize the delivery of health care services in a setting or manner not otherwise authorized by law. [C. R. S. 2018, 25.5-5-414 (7)(a) & (b)].
Originating Site Billing
The originating site (originating provider) is where the member is located. For an allowable provider type to bill for the originating site facility fee, the member and provider must be physically present in the same location.
The originating provider may bill for other Health First Colorado-covered services that were provided during the same visit as the Telemedicine visit.
In some cases, the originating provider site will not be providing clinical services, but only providing a site and telecommunications equipment. In this situation, the telemedicine originating site facility fee is billed using procedure code Q3014.
Originating providers bill as follows:
- If the originating provider is making a room and telecommunications equipment available but is not providing clinical services, the originating provider bills Q3014 (the procedure code for the telemedicine originating site facility fee).
- If the originating provider also provides clinical services to the member, the provider bills the rendering provider's appropriate procedure code and bills Q3014.
- The originating provider may also bill, as appropriate, on the UB-04 paper claim form or as an 837I transaction for any clinical services provided on-site on the same day that a telemedicine originating site claim is made. The originating provider must submit two separate claims for the member's two separate services.
Distant Providers
All distant providers should bill the appropriate procedure code and Place of Service 02 or 10 and FQ or FR modifiers if appropriate on the CMS 1500 paper claim form or as an 837P transaction.
When the patient is located in a hospital, please use the appropriate place of service code for where the patient is located.
Billing HCPCS Q3014
The following provider types may bill procedure code Q3014 (telemedicine originating site facility fee):
| Physician | 05 |
| Clinic | 16 |
| Osteopath | 26 |
| FQHC | 32 |
| Doctorate Psychologist | 37 |
| MA Psychologist | 38 |
| Physician Assistant | 39 |
| Nurse Practitioner | 41 |
| RHC | 45 |
Provider types not listed above may facilitate Telemedicine Services with a distant provider but may not bill procedure code Q3014. Examples include Nursing Facilities, Intermediate Care Facilities, Assisted Living Facilities, etc.
If practitioners at both the originating site and the distant site provide the same service to the member, both providers submit claims using the same procedure code with modifier 77 (Repeat procedure by another physician).
The originating site may not bill for assisting the distant site provider with an examination.
Telemedicine Place of Service Codes
All rendering providers must bill the appropriate procedure code using Place of Service code 02 or 10 and the appropriate modifiers FQ, FR, 93 or 95 on the CMS 1500 paper claim form or as an 837P transaction.
When the patient is located in a hospital, please use the appropriate place of service code for where the patient is located.
Place of Services codes 02 and 10 can be used during telehealth encounters:
- POS 02: Telehealth provided other than in the patient’s home.
- POS 10: Telehealth provided in patient’s home.
Additionally, modifiers FQ, FR, 93 and 95 can be added to POS 2 and 10:
- FQ: The service was furnished using audio-only communication technology.
FR: The supervising practitioner was present through two (2)-way, audio/video communication technology.
- 93: Synchronous Telemedicine Service Rendered Via Telephone or Other Real-Time Interactive Audio-Only Telecommunications System
- 95: Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunications System
The following provider types may bill using modifier GT:
| Physician | 05 |
| Clinic | 16 |
| Osteopath | 26 |
| FQHC | 32 |
| Doctorate Psychologist | 37 |
| MA Psychologist | 38 |
| Physician Assistant | 39 |
| Nurse Practitioner | 41 |
| RHC | 45 |
Procedure codes listed below under Telemedicine Modifier GT" will receive an additional $5.00 to the fee listed on the most recent Health First Colorado Fee Schedule when billed using modifier GT.
Rendering Providers
If a rendering provider's number is required on the claim for a face-to-face visit, it is required on the claim for a telemedicine visit.
Clinics and the other provider types are required to enter the rendering provider's Health First Colorado provider number in field 19D.
When an originating site bills Q3014 (telemedicine originating site facility fee), there is generally no rendering provider actually involved in the service at the originating site.
However, a rendering provider number is still required and must be affiliated with the billing provider. The facility may enter either the member's usual provider's number, or another provider number affiliated with that site as the rendering provider.
When the member sees a rendering provider at the originating site and also uses the site as the telemedicine originating site, the facility bills the rendered service procedure code and Q3014 for the use of the telemedicine facility. The same rendering provider number is entered in field 19D.
Telemedicine Modifier GT
When used by an FQHC or RHC, the modifier GT identifies the services as being delivered through telemedicine modality. There is no enhanced payment to FQHCs and RHCs when using the modifier GT.
The following procedure codes, when billed with modifier GT by appropriate providers, pay the telemedicine transmission fee (an additional $5.00 to the fee listed in the most recent Health First Colorado Fee Schedule). Any other procedure codes billed with modifier GT will not pay the telemedicine transmission fee. When providing Family Planning via Telemedicine, appropriate providers may use the combination modifier codes of FP/GT (in this order).
| Procedure Codes | Comments |
|---|---|
| Outpatient Mental Health | |
| 90791 | If interactive complexity then report with add on code 90785 |
| 90832 | If interactive complexity then report with add on code 90785 |
| 90833 | Use in conjunction with appropriate E/M code If interactive complexity then report with add on code 90785 |
| 90834 | If interactive complexity then report with add on code 90785 |
| 90836 | If interactive complexity then report with add on code 90785 |
| 90837 | Medicare crossover only |
| 90838 | Medicare crossover only |
| 90863 | can be added to primary psychotherapy code |
| 90846 | |
| 90847 | |
| Evaluation & Management | |
| 99201 | |
| 99202 | |
| 99203 | |
| 99204 | |
| 99205 | |
| 99211 | |
| 99212 | |
| 99213 | |
| 99214 | |
| 99215 | |
| Speech Therapy | |
| 92507 | |
| 97532 | |
| Obstetrical Ultrasounds | |
| 76801 | |
| 76802 | |
| 76805 | |
| 76810 | |
| 76811 | |
| 76812 | |
| 76813 | |
| 76814 | |
| 76815 | |
| 76816 | |
| 76817 | |
| Other | |
| 96116 | |
Remote Patient Monitoring
Effective July 1, 2025, Remote Patient Monitoring (RPM) is a covered benefit.
Remote patient monitoring (RPM) is the continuous use of technology to track a patient’s clinical data, enabling early detection of health changes and timely medical interventions to prevent emergency intervention or inpatient hospitalization. Refer to the Code of Colorado Regulations (10 CCR 2505-10, Section 8.096) for more information.
Remote Patient Monitoring must be rendered and supervised in accordance with the scope of practice for the enrolled provider and performed by one of the following licensed healthcare professionals:
- Physician
- Podiatrist
- Advanced Practice Registered Nurse
- Physician Assistant
- Respiratory Therapist
- Pharmacist
- Licensed healthcare professional working under the supervision of a Medical Director
A member is eligible for Remote Patient Monitoring (RPM) if the member’s health care provider determines that RPM is medically necessary and can prevent member’s admission or readmission to a hospital, Emergency department, nursing facility, or other clinical setting and the member has one of the qualifying conditions:
- Diabetes
- Chronic Obstructive Pulmonary Disease (COPD)
- Heart Failure
- Asthma
- Pneumonia
- Members who are pregnant and carrying a high-risk pregnancy
Criteria for Technology Equipment Required for Remote Patient Monitoring:
- FDA-Certified or UL Listed: Technological equipment required for RPM must be FDA certified, or UL listed and used according to the manufacturer’s instructions.
- Maintained: In good repair and free from safety hazards
- Sanitization: Technological equipment must be sanitized before utilization in the Member’s home per the manufacturer’s instructions.
- HIPPA Compliance: Healthcare software should meet the security standards related to patient health information by protecting patient data confidentiality, integrity and availability.
- Automatic Data Upload: Equipment must be capable of automatically uploading data without the member needing to manually self-report or self record the data.
Remote Patient Monitoring Procedure Codes:
| Procedure Codes | Detail | Frequency |
| 98016 | Brief telephone E/M (5-10 minutes) by a physician or qualified professional for an established patient, not related to a prior E/M in the past 7 days and not leading to one within 24 hours. | Once Per Episode of Care |
| 99091 | Collection and interpretation of digitally stored/transmitted physiologic data (eg, ECG, blood pressure, glucose monitoring) by qualified provider, requiring 30 + minutes. | Once a Month |
| 99453 | Reports initial set-up and patient education on the use of equipment. | Once Per Episode of Care |
| 99454 | Covers the supply of the RPM device, including daily recording and programmed alert transmission. Used for each additional 20 minutes of clinician time per month. | Once a Month |
| 99457 | Used for 20 minutes of clinician time per month managing care based on RPM data, with live interaction with the patient or caregiver. | Once a Month |
| 99458 | Used for an additional 20 minutes of clinician time managing care with RPM data. | Once a Month |
*Episode of Care: Beginning when the remote physiologic monitoring service is initiated and ends with attainment of targeted treatment goals.
Frequently Asked Questions:
For additional information, refer to the Remote Patient Monitoring for Outpatient Clinical Services FAQ.
eConsults Overview
Effective February 1, 2024, eConsults that meet the criteria below are a covered benefit.
eConsult: An asynchronous dialogue initiated by a Treating Practitioner seeking a Consulting Practitioner’s expert opinion without a face-to-face member encounter with the Consulting Practitioner.
Treating Practitioner: A member’s treating physician or other qualified health care practitioner who is a primary care provider contracted with a Regional Accountable Entity to participate in the Accountable Care Collaborative as a Network Provider.
Effective July 1, 2025, A Treating Practitioner may also be a member’s treating provider who has education, training, or qualification in a specialty field other than primary care and is a medical doctor (MD), doctor of osteopathy (DO), Nurse Practitioners (NPs), and Physician Assistants (PAs).
Consulting Practitioner: A provider who has education, training or qualifications in a specialty field other than primary care.
eConsult Platform: Providers can utilize the Department's eConsult platform, Colorado Medicaid eConsult, or a third-party eConsult platform that meets the Department’s criteria.
Approved Third-Party eConsult Platform Criteria
- Platform must be capable of maintaining documentation that the eConsult is directly relevant to the individual patient’s diagnosis and treatment, and the consulting practitioner has specialized expertise in the particular health concerns of the patient.
- Platform must be capable of identifying the Colorado Medicaid enrollment status of providers using the platform. All providers must be licensed in the state of Colorado.
- Platform meets all state and federal privacy laws regarding the exchange of patient information.
- Platform must be capable of providing sufficient documentation for the treating and consulting provider to demonstrate that the consultation was provided for the direct benefit of the member.
- Platform must provide the treating and consulting practitioner with the information necessary to file a claim including date of service; name of recipient; Medicaid identification number; name of provider agency or person providing the service; nature, extent or units of service and the place of service.
eConsult Billing and Reimbursement
Treating Practitioners Billing:
- Use CPT code 99452
- The date of service for 99452 should be the date the eConsult was completed.
- Treating practitioners use 99452 to report an eConsult outside of an evaluation and management service. An eConsult completed on the same date of service as an office visit is considered part of the evaluation and management service and will not be reimbursed separately per NCCI.
- Services must meet the procedural definition and components, including time requirements, of the CPT code as defined by the AMA in addition to requirements listed here.
Treating Practitioner Reimbursement:
- All Treating Practitioners rendering eConsults should submit claims for completed eConsults to the Colorado interChange for fee-for-service reimbursement.
- Please see the Health First Colorado fee schedule
Consulting Practitioners Billing:
- Use CPT Code 99451
- Services must meet the procedural definition and components including time requirements, of the CPT code as defined by the AMA in addition to requirements listed here.
Consulting Practitioner Reimbursement:
- Consulting practitioners who use the Department's eConsult platform will be reimbursed by Safety Net Connect's subcontractor, ConferMED.
- Consulting practitioners who use an approved eConsult platform should submit claims for completed eConsults to the Colorado interChange for fee-for-service reimbursement.
- Please see the Health First Colorado fee schedule
Federally Qualified Health Centers (FQHCs) and Rural Health Centers (RHCs)
eConsult dialogues between Treating Practitioners and Consulting Practitioners do not meet the definition of an FQHC or RHC visit as defined in CCR 8.700. Costs associated with performing eConsults through an FQHC/RHC are considered allowable costs for the cost report and will be included in the calculation of the reimbursement rate for a patient visit at an FQHC/RHC.
Refer to the Code of Colorado Regulations (1- CCR 2505-10, Section 8.095) for more information.
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number & Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven-digit Health First Colorado ID number as it appears on the Medicaid Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070125 for July 1, 2025. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070125 for July 1, 2025. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070125 for July 1, 2025. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not required | |||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than twelve (12) diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | Enter the six-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. | ||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010125 for January 1, 2025.
or
Span dates of service
Practitioner claims must be consecutive days.
VP - Vendor Product Number | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code 02 or 10 for services delivered using telemedicine modality. | ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not Required | |||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the procedure code that specifically describes the service for which payment is requested. | ||||||||||||||||||||||||||||||||||||
| 24D. | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. Telemedicine For originating provider use procedure code Q3014. For distant provider use procedure code + modifier GT. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. GT Via Interact Audio/Video System/strong>, | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early & Periodic Screening, Diagnosis, and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available- Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) Not Required | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070125 for July 1, 2025. Unacceptable signature alternatives: Claim preparation personnel may not sign the enrolled provider's name. Initials are not acceptable as a signature. Typed or computer printed names are not acceptable as a signature. Signature on file notation is not acceptable in place of an authorized signature. | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
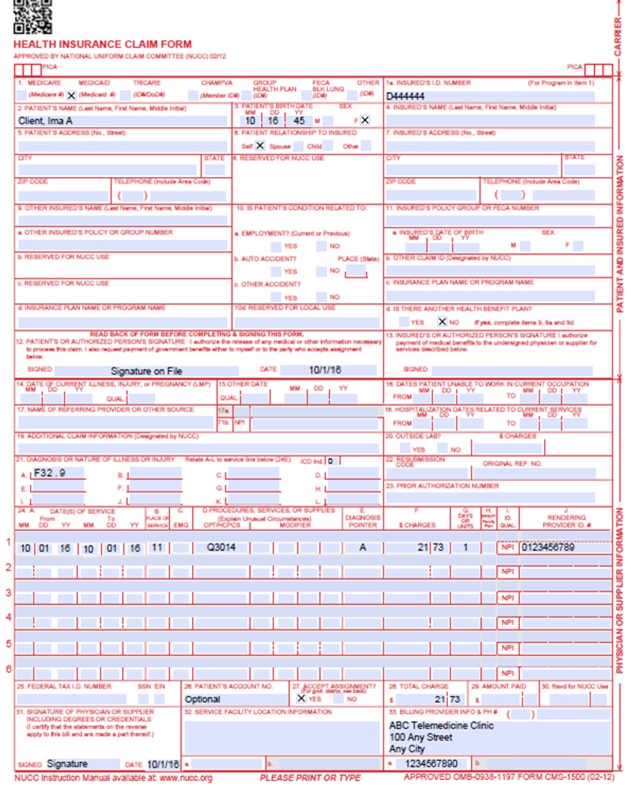
Telemedicine Originator Claim Example
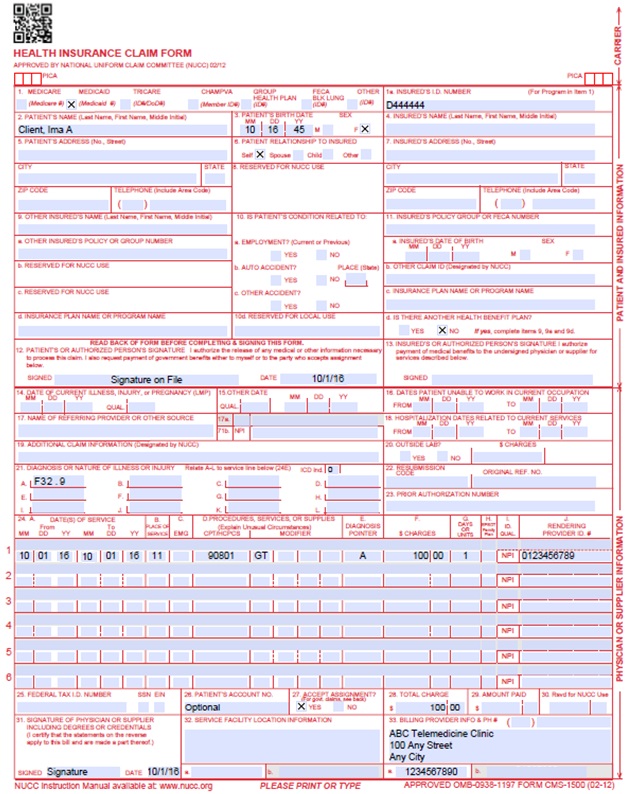
Telemedicine Distance Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
Telemedicine Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 2/20/2018 | Updates based on Departments | DXC |
| 2/23/2018 | Removed NDC supplemental qualifier - not relevant for Telemedicine providers | DXC |
| 6/15/2018 | Updated timely filing information and removed references to LBOD, removed general billing information already available in the General Provider Information manual | DXC |
| 6/7/2019 | Language clarification. removed education-only services from the "Not Covered Services" section as these will now be covered. Not moving forward with requiring POS 02 for telemedicine claims so removed. POS was clarified to read "where the patient is located" as opposed to "where services were rendered." | HCPF |
| 6/19/2019 | Reformatted to correct page numbering issue | HCPF |
| 01/03/2020 | Converted to web page | HCPF |
| 05/20/2020 | Revised content through for clarity. | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 11/23/2020 | Adding information specific to FQHC/RHC billing and distant site coverage | HCPF |
| 4/6/2021 | Adding information specific to Telemedicine Modifier GT | HCPF |
| 2/1/2022 | Editing POS to include 02 and 10. Adding info on modifier FQ and FR | HCPF |
| 2/14/2022 | Added information on EPSDT | HCPF |
| 10/20/2022 | Added information on eHealth Entity Provider Specialty Types | HCPF |
| 5/9/2023 | Added for end of PHE, added list of allowed procedure codes | HCPF |
| 7/7/2023 | Added clarifying language under Non-Covered Services | HCPF |
| 1/18/2024 | Added eConsults under Program Overview | HCPF |
| 5/15/2024 | Added clarifying language for FQHC/RHC eConsults | HCPF |
| 7/30/2024 | Added clarifying language for Physical Therapy, Occupational Therapy, Home Health, Hospice and Pediatric Behavioral Health Providers. | HCPF |
| 10/15/2024 | Clarified billing requirements for eConsults. | HCPF |
| 2/5/2025 | Added code S9443 under general billing information for Telehealth Billing | HCPF |
| 5/7/2025 | Added codes 98000 - 98016 to procedure code table | HCPF |
| 5/9/2025 | Changed Pediatric Behavioral Health Providers to Pediatric Behavioral Therapy Providers. Added allowable codes. Under Requirement for Telemedicine Services #9 OCR section removed. Telemedicine -Provider Information was changed to General Billing Information with updated link. Added COVID-19 Emergency Policy Flexibilities Made Permanent section. Updated overall billing manual. | HCPF |
| 6/12/2025 | Added codes 99091 and 99453 - 99458 to the procedure code table. Updated information about Remote Patient Monitoring/included in the table of contents. | HCPF |
| 6/18/2025 | Added information about Specialty-to-Specialty Consultation under eConsult overview and updated billing manual language for clarity. | HCPF |
| 7/31/2025 | Added FAQ under Remote Patient Monitoring with brief description. | HCPF |
| 8/28/2025 | Updated section of "COVID-19 Emergency Policy Flexibilities Made Permanent" to include information instead of link. | HCPF |
| 9/25/2025 | Removing COVID-19 Emergency Policy Flexibilities Made Permanent | HCPF |
| 12/4/2025 | Added Procedure Codes G0310 – G0315 and adjusted telemedicine place of service FR definition spacing. | HCPF |