Home Health Billing Information Manual
- Home Health Billing Information
- Provider Qualifications
- Billing Information
- General Prior Authorization Requirements (PARs)
- Home Health Prior Authorization Information
- PAR Form Instructions
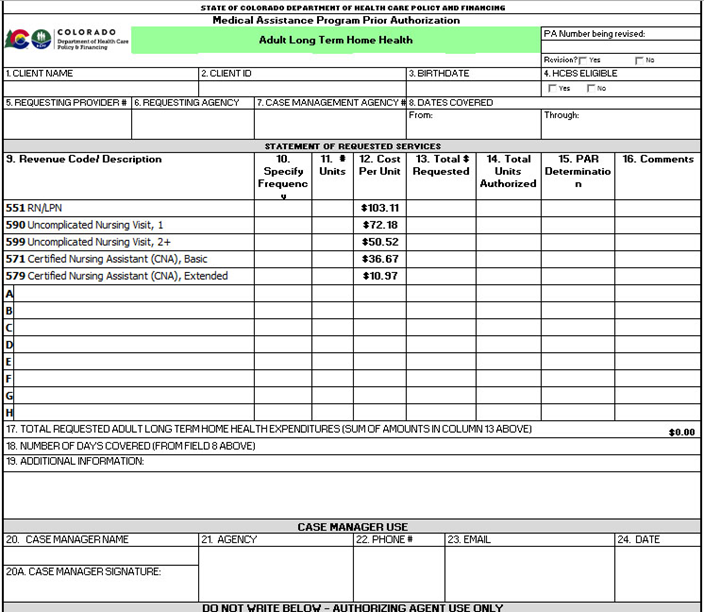
- PAR Form
- Revenue Coding
- Reimbursable Home Health Services
- Non-Reimbursable Home Health Services
- Special Reimbursement Conditions for Home Health Services
- Reimbursable Home Health Service Locations
- Other Billing Information
- Paper Claim Reference Table
- Institutional Provider Certification
- Timely Filing
- Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
- Electronic Visit Verification
- Home Health Billing Information Revisions Log
Return to Billing Manuals Web Page
Home Health Billing Information
The Department of Health Care Policy & Financing (the Department) periodically modifies billing information. Therefore, the information in this manual is subject to change, and the manual is updated as new billing information is implemented. Visit the Rates and Fee Schedule web page for daily and annual limits.
Provider Qualifications
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid program) provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
In order to become a Health First Colorado Home Health Provider, an agency must:
- Hold a current and active Class A Home Care License issued by the State of Colorado
- Obtain Medicare certification and/or deemed status with an accepted Home Health Accreditation entity: Joint Commission (JC), Community Health Accreditation Program (CHAP) or the Accreditation Commission for Health Care, Inc. (ACHC)
- Be enrolled as a Medicare provider
- Be in good standing with the Colorado Department of Health Care Policy & Financing, Colorado Department of Public Health and Environment (CDPHE) and Medicare
After obtaining licensure and certification as a Class A Home Care Agency, an applicant must submit a completed provider enrollment packet to become Health First Colorado eligible providers. Visit the Provider Enrollment web page and the Revalidation web page for enrollment information.
Home Health Agencies must comply with rules and regulations for Medicaid Home Health, including but not limited to the Home Health Benefit Coverage Standard and 10 C.C.R. 2505 -10 § 8.520-8.529.
All Home Health services provided are subject to post-payment review for medical necessity and regulation compliance.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for general billing information.
Ordering, Prescribing and Referring (OPR) Providers
Effective July 1, 2022, the Department began enforcing the federal requirement 42 CFR § 455.440, which requires that all claims for Home Health services include the National Provider Identifier (NPI) of the provider who ordered the service, and 42 CFR 455.440, which requires the NPI is associated with an actively enrolled Health First Colorado Provider.
Providers are required to enter the NPI of the ordering provider into the Attending Provider field (#76) or the Other ID fields (#78 or #79) for both paper and electronic claims. In the Provider Web Portal, this field may be labeled "Referring Provider".
Refer to the applicable UB-04 billing manuals located on the Billing Manuals web page for guidance on how each field is used.
Home Health services can be ordered by either a physician or an allowed practitioner. Allowed practitioners are defined in accordance with State law as Physician Assistant (PA), Nurse Practitioner (NP), or Clinical Nurse Specialist (CNS). The ordering provider must also be actively enrolled with Health First Colorado. If these conditions are not met, the claim will be denied.
Visit the OPR web page or refer to Program Rule 10 CCR 2505-10 8.125.8.A for further information.
General Prior Authorization Requirements (PARs)
Acute Home Health PARs
Acute Home Health Services do not need to be prior authorized. However, if the member is enrolled in a Health First Colorado Managed Care Organization (MCO), such as Denver Health, Rocky Mountain Health Plans or Colorado Access Health Plan, please contact the MCO directly to determine the health plan's acute Home Health prior authorization requirements.
Long-Term Home Health (LTHH) PARs
All LTHH Services shall be submitted to the Department's authorizing agency as soon as possible, but no more than ten (10) business days from the start date of the LTHH PAR. Refer to Appendix C and Appendix D located on the Billing Manuals web page under the Appendices drop-down for authorizing agency information. The Home Health PAR Form must be completed and reviewed by the Department's authorizing agency before services can be billed.
LTHH PARs that are submitted more than ten (10) business days from the start date of the LTHH PAR shall have the PAR start date amended to the date of submission to the Department's authorizing agency. A PAR is not considered complete until the authorizing agency reviews all information necessary to review the request. All LTHH PAR submissions must include:
- The complete and current plan of care using the HCFA-485 or other document that is identical in content, including a clear listing of:
- Member's diagnoses that will be addressed by Home Health, using V-codes whenever appropriate
- The specific frequency and expected duration of the visits for each discipline ordered
- The duties/treatments/tasks to be performed by each discipline during each visit
- All other supporting documentation to support the request, including physician's orders, treatment plans, nursing summaries, nurse aide assignment sheets, medications listing, etc.
- Any other documentation deemed necessary by the Department or its authorizing agency
The plan of care must be created by a registered nurse employed with the Home Health Agency or, when appropriate, by a physical, occupational or speech therapist. The plan of care must be signed by the member's attending physician prior to submitting the final claim for a certification period. Refer to the Home Health Services Benefit Coverage Standard referenced in 10 C.C.R 2505-10 § 8.522 - Covered Services for additional information on Health First Colorado plan of care requirements.
Submit the appropriate completed PAR via:
- Pediatric members - eQSuite®
- Adult members - the Adult Long-Term Home Health PAR Form located on the Provider Forms web page under the Prior Authorization Request (PAR) Forms drop-down menu
Pediatric PARs
All pediatric LTHH PARs must be submitted via the utilization management vendor. Visit the ColoradoPAR Program web page for more information.
Adult PARs
All adult LTHH PARs must be submitted on the Adult Long-Term Home Health PAR Form located on the Provider Forms web page under the Prior Authorization Request (PAR) Forms drop-down menu. Instructions for completing the PAR form are included in this manual.
The authorizing agency reviews all completed PARs and approves or denies, by individual line item, each requested service listed on the PAR. PAR status inquiries can be made through the File and Report System (FRS) in the Provider Web Portal, and PAR determinations are included on PAR letters sent to both the provider and the member. Read the determination carefully as some line items may be approved and others denied. Do not render or bill for services until the PAR has been processed.
The claim must contain the PAR number for payment.
Approval of a PAR does not guarantee Health First Colorado payment and does not serve as a timely filing waiver. Prior authorization only assures that the services requested are considered a benefit of Health First Colorado. All claims, including those for prior authorized services, must meet eligibility and claim submission requirements (e.g., timely filing, pursuit of third-party resources payment, included required attachments, etc.) before payment can be made.
If the PAR is denied, providers should direct inquiries to the authorizing agency who reviewed the PAR.
Do not submit claims before the PAR has been reviewed and approved unless submission is necessary to meet timely filing requirements. Visit the Medical Services Board web page for required attachments.
PAR Revisions
If the number of approved units needs to be amended, the provider must submit a request for a PAR revision prior to the PAR end date. Changes requested after a PAR is expired will not be made by the Department or the authorizing agency.
Note: When a PAR is revised, the number on the original PAR must be used on the claim. (Do not use the PAR number assigned to the revision when completing a claim. Use the original PAR number.)
Pediatric LTHH PAR revisions should be completed in eQSuite®. Adult LTHH PAR revisions must be made on the Department's designated form and submitted to the authorizing agency for review. Complete the Revision section of the PAR and include the PAR number that needs to be revised.
Note: The number of units should equal more or less than the number of units planned for use during the PAR period. The number of units being requested needs to be added to the original number of units approved and include all services that were approved on the original PAR.
Change of Provider Revisions
When a member in LTHH changes providers during an active PAR certification, the receiving Home Health Providers shall complete a Change of Provider Form, located on the Provider Forms web page under the Prior Authorization Request (PAR) Forms drop-down menu in order to transfer the member's care from the previous provider to the receiving agency.
Once the receiving agency completes the Change of Provider form, the form must include the member's signature to indicate that the member is in agreement with the change of provider request. The completed Change of Provider form must accompany a new Home Health PAR from the receiving agency.
The agency must submit the Change of Provider form along with a new PAR to the authorizing agency. The new PAR start date should coincide with the first day that the new agency plans to provide LTHH care. The provider should not include dates for Acute Home Health or any lapses in care between the last date of service provided by the previous Home Health agency and the receiving agency.
The previous provider's PAR end date will be revised to match the information provided in the "last date of service" box, and a new PAR will be entered for the receiving agency.
The Change of Provider letter authorizes the Department's Fiscal Agent to end the current PAR so that the new Home Health PAR may be entered. Single Entry Points (SEPs) and Community Centered Boards (CCBs) must include the Case Management Agency's (CMA) identification number on the PAR form.
If the receiving agency is unable to obtain the necessary PAR information from the previous agency, the receiving agency may call the Department's Fiscal Agent to find out whether there is a current Home Health PAR in the system. If a current PAR does exist, the Department's Fiscal Agent will provide the name and phone number of the Home Health Agency who currently has the approved PAR, but will not be able to provide any of the details for the PAR.
The receiving agency should contact the previous agency, when possible, and notify them that the member is transferring agencies and the effective date of the change.
Home Health Agencies should not bill LTHH services on another provider's LTHH PAR.
Home Health Prior Authorization Information
Medical Assistance Program Home Health is provided on an Acute Home Health basis or LTHH basis. Health First Colorado also reimburses Telehealth services for members who qualify for telehealth monitoring. (For more information on Home Health Telehealth services, refer to the Home Health Benefit Coverage Standard as referenced in 10 C.C.R 250-10 8.522 - Covered Services).
Acute Home Health
Acute Home Health is defined as intermittent Home Health services provided up to 60 consecutive calendar days after an acute onset of an illness, injury or disability, hospitalization or acute onset of exacerbations requiring skilled Home Health care as outlined in the Home Health Benefit Coverage Standard as referenced in 10 C.C.R 2505 - 10 § 8.522. Covered Services. Acute Home Health does not require prior authorization.
Services include skilled nursing, skilled certified nurse aide, physical therapy, occupational therapy, speech therapy and telehealth services.
If the member is enrolled in a Health First Colorado Managed Care Organization (MCO) health plan, such as Denver Health, Rocky Mountain Health Plans or Colorado Access Health Plan, the provider will need to contact the MCO directly to determine the MCO Acute Home Health prior authorization requirements.
Effective May 3, 2024, place of service 03 is an allowed place of service for all fee-for-service benefits. In order for community providers to bill fee-for-service to children in a school setting, the provider must follow school district policy. Please reference the Community Providers in a School Setting Policy memo.
Long-Term Home Health (LTHH)
LTHH is defined as intermittent Home Health services required for the care of chronic long-term conditions, and/or on-going care that exceeds the acute HH period (61st calendar day of Home Health service). All LTHH services must be prior authorized.
Services include skilled nursing, skilled certified nurse aide and telehealth services. Pediatric members may also receive physical therapy, occupational therapy and speech therapy.
If a member experiences a new acute event that would warrant Acute Home Health service, the agency may move the member to acute care, when:
- At least 10 calendar days have elapsed since the member's last Acute Home Health episode
and - There is a new onset of illness, injury or disability or the member experiences an acute change in condition from the member's past Acute Home Health episode(s).
Providers should refer to the Code of Colorado Regulations, Program Rules (10 C.C.R. 2505- 10), for specific information when providing Home Health care.
PAR Form Instructions
Complete this form for Prior Authorization Requests for Adult LTHH. Submit the PAR per the instructions listed at the bottom. Please include the Plan of Care and other supporting documentation.
For PAR Revisions:
Complete the Revision section at the top of the form only if revising a current approved PAR. The number of units should more or less equal the number of units planned for use during the PAR period. The number of units being requested needs to be added to the original number of units approved and include all services that were approved on the original PAR. Use one (1) of the eight (8) lettered (A-H) dropdown fields found in the first few lines immediately following the last code in Column 9, the "Description" column, when a revision requires:
- Additional lines of existing codes to indicate varying rates, units, etc.
- The inclusion of codes for a timeframe that used codes not listed on the existing form
- Change of Provider
Complete the following required fields:
- Member Name: Enter the member's name.
- Member ID: Enter the member's Medical Assistance Program ID number.
- Birthdate: Enter the member's date of birth.
- HCBS Eligible: Check "yes," if the member is currently enrolled in a waiver program with Home and Community-Based Services. Check "no," if the member is not currently enrolled in a waiver program or is on the wait list for a waiver program (the Department or Developmental Disabilities).
- Requesting Provider #: Enter the requesting provider's Medical Assistance Program provider number.
- Requesting Agency: Enter requesting Home Health agency.
- Case Management Agency #: Enter the Case Management Agency number.
- Dates Covered (From and Through): Enter the PAR start date and PAR end date.
- Description: List approved procedure codes.
- Specify Frequency: Enter visit frequency for Home Health service requested using daily, weekly, etc.
- # Units: Enter the number of units next to the services for which reimbursement is being requested.
- Cost Per Unit: Cost per unit automatically populates.
- Total $ Requested: The total dollar amount requested for the service automatically populates.
- Total Units Authorized: The Authorizing entity enters the total number of units approved per line.
- PAR Determination: This box is completed by the designated review agency. Select the appropriate determination: Approved (A), Partially Approved (PA), Denied (D)
- Comments - Optional: Enter any additional useful information. For PAR revisions, this is a required field and should include if a service is authorized for different dates than in Box 8. Please include the procedure code and date span here.
- Total Requested Expenditures: Total automatically populates.
- Number of Days Covered: The number of days covered automatically populates.
- Additional Information - Optional: Home Health Agencies may use this field to explain the reasons for requested frequency, duration, medical necessity, or by CMA to explain reasons for denial or approval of a reduced amount, as needed.
- Case Manager Name: Enter the name of the Case Manager.
- 20A. Case Manager Signature: Enter the Case Manager signature.
- Agency: Enter the name of the agency.
- Phone #: Enter the phone number of the Case Manager.
- Email: Enter the email address of the Case Manager.
- Date: Enter the date completed.
"DO NOT WRITE BELOW - AUTHORIZING AGENT USE ONLY." This is for Department use only.
Send only New and Revised PARs to:
Adult with Department of Human Services (DHS) Waivers (DD, DHSS, SLS): Community Centered Board (CCB)
Adult with or without Department Waivers (BI, CMHS, EBD, PLWA, SCI): Case Management Agency (CMA)/Single Entry Point (SEP)
Note: If submitted to the Department's Fiscal Agent, the following correspondence will not be returned to Case Managers, outreach will not be performed to fulfill the requests, and all such requests will be recycled:
- Paper PAR forms that do not clearly identify the case management agency or have incorrect member information in the event the form(s) need to be returned.
- PAR revision requests not submitted on Department-approved PAR forms, including typed letters with revision instructions.
Should questions arise about what Fiscal Agent staff can process, please contact the Home Health Policy Specialist.
PAR Form
Revenue Coding
The following table identifies the only valid revenue codes for billing Home Health services to Health First Colorado. Valid revenue codes are not always a Health First Colorado benefit. When valid non-benefit revenue codes are used, the claim must be completed according to the billing instructions for non-covered charges. Home Health providers billing on the UB-04 institutional claim form for services provided to authorized members must use the appropriate condition code in form locators 18 through 28 (Condition Codes) and use the revenue codes listed below. Claims submitted with revenue codes that are not listed below are denied.
| Service Type | Revenue Code | Unit Value | |
| Acute Home Health | Long-Term Home Health | ||
| Supplies (General) | 0270 | Non-covered benefit (non-covered charges must be shown in both form locator 47 and 48 of the claim form) | |
| RN/LPN Standard Visit | 0550 | 0551 | One (1) visit (not to exceed 2.5 hours) |
| Uncomplicated Nursing (Visit 1) | n/a | 0590 | One (1) Visit |
| Uncomplicated Nursing Visit (Visit 2+) | n/a | 0599 | One (1) visit |
| HHA BASIC | 0570 | 0571 | One (1) hour |
| HHA Extended | 0572 | 0579 | For visits lasting more than one (1) hour, extended units of 15-30 minutes. |
| PT | 0420 | 0421 (pediatric LTHH only) | One (1) visit (not to exceed 2.5 hours) |
| OT | 0430 | 0431 (pediatric LTHH only) | One (1) visit (not to exceed 2.5 hours) |
| S/LT | 0440 | 0441 (pediatric LTHH only) | One (1) visit (not to exceed 2.5 hours) |
| Home Health Telehealth Set-up Fee | 0583 TG 98969 (proc) | 0780 TG 98970 (proc) | Installation and member education of telehealth equipment (one (1) time only) |
| Home Health Telehealth Daily Monitoring | 0583 98969 (proc) | 0780 98970(proc) | One (1) unit per day that telehealth monitoring is obtained (limit 31 units/ month) |
Reimbursable Home Health Services
The licensed and certified Class A Home Care shall not utilize staff that has been excluded from participation in federally funded health care programs by the US Department of Health and Human Services (HHS)/Office of Inspector General (OIG) and shall be in good standing with the Colorado Department of Regulatory Agencies (DORA) or other regulatory agency:
Registered Nurses (RN) and Licensed Practical Nurses (LPN) must have a current, active license in accordance with the DORA Colorado Nurse Practice Act at § 12-38-111, C.R.S.
- Acute Home Health: All nursing services provided during the Acute Home Health period shall be billed under revenue code 550. No PAR is required.
- Long-Term Home Health (LTHH): Nursing services provided during Long-Term Home Health shall be billed using the appropriate revenue codes based on the purpose and complexity of the nursing visit. Standard, infrequent or complicated nursing visits may be billed using revenue code 551. Nursing visits that are uncomplicated in nature, or visits that are uncomplicated with frequent revisits completed by the nurse, shall be billed using revenue codes 590 and 599).
- Long-Term Home Health nursing visits for the sole purpose of assessing a member may be reimbursed for a limited time when managing and reporting to the member's physician on specific conditions and/or symptoms which are not stable.
Certified Nurse Aides (CNA) must have a current, active license in accordance with the DORA Colorado Nurse Aide Practice Act at § 12-38-111, C.R.S.
- Acute Home Health: Skilled CNA visits are reimbursed based on the amount of time the CNA is providing skilled care to a member. If a CNA provides care for at least 15 minutes but not more than 60 minutes, the agency shall bill a basic unit with revenue code 570. For each additional 30-minute block that the CNA provides hands-on assistance to the member, the agency may bill an extended CNA unit with revenue code 572. A unit of time that is less than 15 minutes shall not be reimbursable as a basic unit and at least 15 minutes must elapse before an agency may bill an extended unit. No PAR is required.
- Long-Term Home Health: Skilled CNA visits are reimbursed based on the amount of time the CNA is providing skilled care to a member. If a CNA provides care for at least 15 minutes but not more than 60 minutes, the agency shall bill a basic unit with revenue code 571. For every additional 30 minutes the CNA provides hands-on assistance to the member, the agency may bill an extended CNA unit with revenue code 579. A unit of time that is less than 15 minutes shall not be reimbursable as a basic unit and at least 15 minutes must elapse before an agency may bill an extended unit.
Physical Therapists (PT) must have a current, active license in accordance with the Colorado Physical Therapy Practice Act at § 12-41-107, C.R.S.
- Acute Home Health: All physical therapy services may be provided on pediatric and adult Home Health member and are billed using revenue code 420 on a per visit basis. No PAR is required.
- Long-Term Home Health: Physical therapy is available to pediatric members when prior authorized and deemed medically necessary. Physical therapy is reimbursed on a per visit basis using revenue code 421.
Occupational Therapists (OT) must have a current, active registration in accordance with the DORA Colorado Occupational Therapy Practice Act at § 12-40.5-106, C.R.S.
- Acute Home Health: All occupational therapy services may be provided to all Health First Colorado Home Health members with a demonstrated need for speech therapy interventions. Occupational therapy services are reimbursed on per visit basis using revenue code 430. No PAR is required.
- Long-Term Home Health: Occupational therapy is available to pediatric members when prior authorized and deemed medically necessary. All Home Health occupational therapy is reimbursed on a per visit basis using revenue code 431.
Speech/Language Pathologists (SLP) who have a current, active certification from the American Speech-Language-Hearing Association (ASHA).
- Acute Home Health: All speech therapy services may be provided to all Health First Colorado Home Health members with a demonstrated need for speech therapy interventions. Speech therapy services are reimbursed on per visit basis using revenue code 440. No PAR is required.
- Long-Term Home Health: Speech therapy is available to pediatric members when prior authorized and deemed medically necessary. All Home Health speech therapy is reimbursed on a per visit basis using revenue code 441.
Telehealth Remote Monitoring Services include the installation and on-going remote monitoring of clinical data through technologic equipment in order to detect minute changes in the member's clinical status that will allow Home Health agencies to intercede before a chronic illness exacerbates requiring emergency intervention or inpatient hospitalization.
- Acute Home Health: Agencies are reimbursed for the initial installation and education of telehealth remote monitoring equipment by billing revenue code 583 with the procedure code 98970 and the modifier 'TG'. This initial charge shall only be billed once per member per agency. The agency may bill for every day they receive and review the member's clinical information by billing revenue code 583 along with procedure code 98970. No PAR is required prior to billing for acute telehealth remote monitoring services, but agencies should notify the Department or its designee when a member is enrolled in the service.
- Long-Term Home Health: Agencies are reimbursed for the initial installation and education of telehealth remote monitoring equipment by billing revenue code 780 with the procedure code 98970 and the modifier 'TG'. This initial charge shall only be billed once per member per agency. The agency may bill for every day they receive and review the member's clinical information by billing revenue code 780 along with procedure code 98970. No PAR is currently required prior to billing for long-term telehealth remote monitoring services, but agencies should notify the Department at homehealth@state.co.us when a member is enrolled in the service.
Non-Reimbursable Home Health Services
- Supplies used for routine Home Health are not reimbursed separately through the Home Health or Durable Medical Equipment (DME) benefit. Non-routine or member specific supplies must be reimbursed through the member's DME benefit.
- Nursing Visits for purpose of psychiatric counseling
- Certified nurse aide visits for the purpose of providing only unskilled personal care and/or homemaking services
- Nursing or CNA visits provided in a shift (visits lasting more than 4.5 consecutive hours)
- Nursing visits for the sole purpose of providing supervision of the CNA or other Home Health staff
- Nursing visits for the sole purpose of completing the Home Health plan of care/recertification
- Long-Term Home Health nursing visits for the sole purpose of teaching the member or their family member
- Long-Term Home Health nursing visits for the sole purpose of assessing a stable member
- Where management, and reporting to physician of specific conditions and/or symptoms which are not stable
Special Reimbursement Conditions for Home Health Services
- Acute Home Health services provided to Health First Colorado MCO members shall be prior authorized (if required) and reimbursed under Health First Colorado MCO rules.
- If a member is eligible for Medicare and Health First Colorado, Medicare is always the first payer when a member has skilled Home Health needs and the member is unable to leave their residence for non-medical programs and treatments (Homebound). All Medicare requirements shall be met and exhausted prior to billing Health First Colorado for Home Health services, except when:
- Medication box pre-filling is the only service provided
- Certified Home Health Aide Services are the only services provided
- Occupational Therapy Services when provided as the sole skilled service
- Routine Laboratory Draw Services is the only service provided
- If the member is (1) stable, (2) not experiencing an acute episode, and (3) routinely leaves the home unassisted for social, recreational, educational and/or employment purposes (not Homebound)
- Medicare and Health First Colorado may be billed simultaneously if Medicare deems that the member is homebound based on the documentation, provided all Health First Colorado funds shall be repaid to Health First Colorado.
- Any combination of a through e above
- The record contains clear and concise documentation describing any exceptions
- Home Health services provided to members who are eligible for both Medicare and Health First Colorado or have another third-party insurance and Health First Colorado must be billed to Medicare first. All insurance requirements must be met and exhausted prior to billing Home Health services to Health First Colorado.
- A denial must be kept in the member's record and updated annually on the anniversary of the denial.
- The third-party insurance denials must be based on non-coverage and not due to the failure of adhering to the requirements set forth by the insurance agency.
- Health First Colorado will not accept a "no-pay" denial (type of bill 320, condition code 21) from Medicare as a valid denial of Medicare coverage.
- The Home Health Agency must maintain a signed Advance Beneficiary Notice (ABN) that is completed as prescribed by Medicare.
Reimbursable Home Health Service Locations
The Home Health program reimburses for skilled nursing, skilled certified nurse aide, physical therapy, occupational therapy, and speech therapy services that are provided on an intermittent or per visit basis to Health First Colorado members in their place of residence.
Health First Colorado pediatric members may receive Home Health services outside of their place of residence when:
- The Home Health services can be provided safely and adequately in a location other than the member's residence.
- Home Health service and interventions will be at least equally effective in a location other than the member's residence.
- It is clinically appropriate for the Home Health services to be provided in a location other than the member's residence.
- It is not primarily for the convenience of the member, member's family, physician or other care provider.
- It is not provided in a group home, nursing facility, hospital or other facility.
Other Billing Information:
- Health First Colorado will reimburse two (2) Home Health staff to care for a member when it is necessary to safely provide member care due to complexity of tasks, member weight, etc. and when it has been prior authorized.
- Member's Home Health Medical records must be retained by the agency for at least seven (7) years unless State or Health First Colorado regulations require that the member's records be maintained for more than seven (7) years.
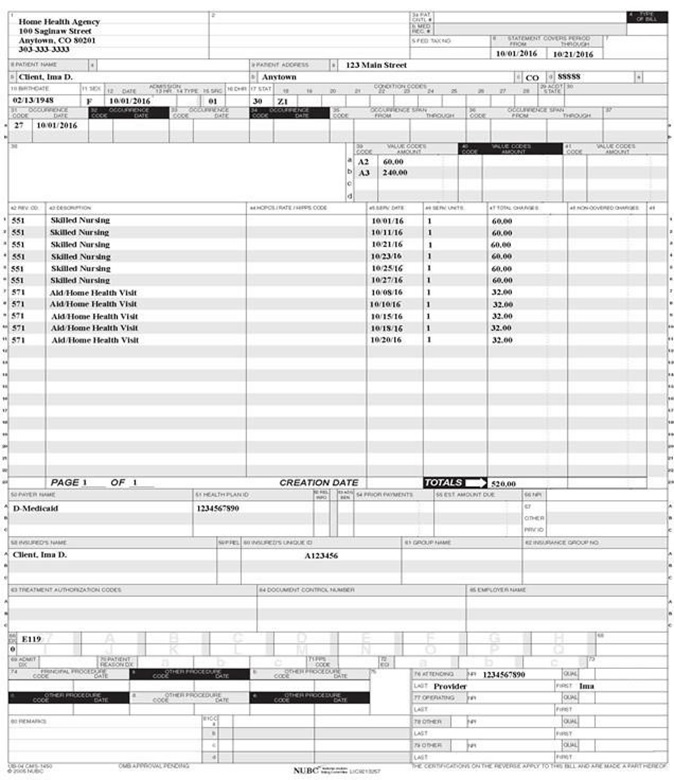
Paper Claim Reference Table
The information in the following table provides instructions for completing form locators as they appear on the paper UB-04 claim form. Instructions for completing the UB-04 claim form are based on the current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data form locators on the UB-04 have the same attributes (specifications) for the Health First Colorado as those indicated in the NUBC UB-04 Reference Manual.
All code values listed in the NUBC UB-04 Reference Manual for each form locator may not be used for submitting paper claims to the Health First Colorado. The appropriate code values listed in this manual must be used when billing the Health First Colorado.
The UB-04 Institutional Certification Form, located on the Provider Forms web page under the Claim Forms and Attachments drop-down menu, must be completed and attached to all claims submitted on the paper UB-04. Completed UB-04 paper Health First Colorado claims, including hardcopy Medicare claims, should be mailed to the correct fiscal agent address listed in Appendix A located on the Billing Manuals web page under the Appendices drop-down.
The Paper Claim Reference Table below lists the required, optional and/or conditional form locators for submitting the paper UB-04 claim form to Health First Colorado for home health claims.
| Form Locator and Labels | Completion Format | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Billing Provider Name, Address, Telephone Number | Text | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Pay-to Name, Address, City, State | Text | Required only if different from FL 1.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3a. Patient Control Number | Up to 20 characters: Letters, numbers or hyphens | Optional Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3b. Medical Record Number | 17 digits | Optional Enter the number assigned to the member to assist in retrieval of medical records. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Type of Bill | 3 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Federal Tax Number | None | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Statement covers period From/Through | From:6 digits MMDDYY Through: 6 digits MMDDYY | Required Home Health-Private Duty Nursing/Hospice "From" date is the actual start date of services. "From" date cannot be prior to the start date reported on the initial prior authorization, if applicable, or is the first date of an interim bill. "Through" date is the actual discharge date, or final date of an interim bill. "From" and "Through" dates cannot exceed a calendar month (e.g., bill 01/15/10 thru 01/31/10 and 02/01/10 thru 02/15/10, not 01/15/10 thru 02/15/10). Match dates to the prior authorization if applicable. If member is admitted and discharged the same date, that date must appear in both fields. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8a. Patient Identifier | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8b. Patient Name | Up to 25 characters, letters and spaces | Required Enter the member's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Patient Address - Street | Characters Letters and numbers | Required Enter the member's street/post office box as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Patient Address - City | Text | Required Enter the member's city as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Patient Address - State | Text | Required Enter the member's state as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Patient Address - ZIP | Digits | Required Enter the member's zip code as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9e. Patient Address - Country Code | Digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10. Birthdate | 8 digits (MMDDCCYY) | Required Enter the member's birthdate using two (2) digits for the month, two (2) digits for the date, and four (4) digits for the year (MMDDCCYY format). Example: 01012010 for January 1, 2010. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Patient Sex | 1 letter | Required Enter an M (male) or F (female) to indicate the member's sex. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Admission Date | 6 digits | Required Home Health/Hospice Enter the date care originally started from any funding source (e.g., Medicare, Health First Colorado, Third Party Resource, etc.). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Admission Hour | 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Admission Type | 1 digit | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Source of Admission | 1 digit | Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Discharge Hour | 2 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Patient Discharge Status | 2 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18-28. Conditions Codes | 2 digits | Conditional Use condition code A1 to bill PDN hours greater than 16 for children. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Accident State | 2 digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31 - 34. Occurrence Code/Date | 2 digits and 6 digits | Required Required Use occurrence code 52 and enter the Plan of Care start date. Enter the date using MMDDYY format. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35-36. Occurrence Span Code From/ Through | none | Leave Blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38. Responsible Party Name/Address | None | Leave blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39 - 41. Value Codes and Amounts | 2 characters and up to 9 digits | Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 42. Revenue Code | 4digits | Required Enter the revenue code that identifies the specific accommodation or ancillary service provided. List revenue codes in ascending order. A revenue code must appear only once per date of service. If more than one (1) of the same services is provided on the same day, combine the units and charges on one (1) line accordingly. Home Health Enter the appropriate Revenue code. Home health services cannot be provided to Nursing Facility residents. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 43. Revenue code Description | Text | Required Enter the revenue code description or abbreviated description. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 44. HCPCS/Rates/ HIPPS Rate Codes | 5 digits | When billing HCPCS codes, the appropriate revenue code must also be billed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 45. Service Date | 6 digits | Required Enter the date of service using MMDDYY format for each detail line completed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 46. Service Units | 3 digits | Required Enter a unit value on each line completed. Use whole numbers only. Do not enter fractions or decimals and do not show a decimal point followed by a zero (0) to designate whole numbers (e.g., Do not enter 1.0 to signify one [1] unit) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 47. Total Charges | 9 digits | Required Enter the total charge for each line item. Calculate the total charge as the number of units multiplied by the unit charge. Do not subtract Medicare or third-party payments from line charge entries. Do not enter negative amounts. A grand total in line 23 is required for all charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 48. Non-covered Charges | Up to 9 digits | Conditional Enter incurred charges that are not payable by Health First Colorado. Non-covered charges must be entered in both FL 47 (Total Charges) and FL 48 (Non-Covered Charges). Each column requires a grand total. Non-covered charges cannot be billed for outpatient hospital laboratory or hospital-based transportation services. Each column requires a grand total. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 50. Payer Name | 1 letter and text | Enter the payment source code followed by name of each payer organization from which the provider might expect payment.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 51. Health Plan ID | 8 digits | Required Enter the provider's Health Plan ID for each payer name. Enter the eight (8)-digit Health First Colorado Program provider number assigned to the billing provider. Payment is made to the enrolled provider or agency that is assigned this number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 52. Release of Information | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 53. Assignment of Benefits | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 54. Prior Payments | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter third party and/or Medicare payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 55. Estimated Amount Due | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter the net amount due from Health First Colorado after provider has received other third party, Medicare or member liability amount. Medicare Crossovers Enter the sum of the Medicare coinsurance plus Medicare deductible less third-party payments and member payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 56. National Provider Identifier (NPI) | 10 digits | Required Enter the billing provider's 10-digit National Provider Identifier (NPI). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 57. Other Provider ID | Optional Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 58. Insured's Name | Up to 30 characters | Required Enter the member's name on the Health First Colorado line. Other Insurance/Medicare Complete additional lines when there is third party coverage. Enter the policyholder's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 60. Insured's Unique ID | Up to 20 characters | Required Enter the insured's unique identification number assigned by the payer organization exactly as it appears on the health insurance card. Include letter prefixes or suffixes shown on the card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 61. Insurance Group Name | 14 letters | Conditional Complete when there is third party coverage. Enter the name of the group or plan providing the insurance to the insured exactly as it appears on the health insurance card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 62. Insurance Group Number | 17 digits | Conditional Complete when there is third party coverage. Enter the identification number, control number, or code assigned by the carrier or fund administrator identifying the group under which the individual is carried. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 63. Treatment Authorization Code | Up to 18 characters | Conditional Complete when the service requires a PAR. Enter the authorization number in this FL if a PAR is required and has been approved for services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 64. Document Control Number | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 65. Employer Name | Text | Conditional Complete when there is third party coverage. Enter the name of the employer that provides health care coverage for the individual identified in FL 58 (Insured Name). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 66. Diagnosis Version Qualifier | Submitted information is not entered into the claim processing system. Enter applicable ICD indicator to identify which version of ICD codes is being reported. 0ICD-10-CM (DOS 10/1/15 and after) 9ICD-10-CM (DOS 9/30/15 and before) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67. Principal Diagnosis Code | Up to 6 digits | Required Enter the exact diagnosis code describing the principal diagnosis that exists at the time of admission or develops subsequently and affects the length of stay. Do not add extra zeros (0) to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67A. - 67Q. - Other Diagnosis | 6 digits | Optional Enter the exact diagnosis code corresponding to additional conditions that co-exist at the time of admission or develop subsequently and which effect the treatment received or the length of stay. Do not add extra zeros (0) to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 69. Admitting Diagnosis Code | 6 digits | Not required Enter the diagnosis code as stated by the physician at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 70. Patient Reason Diagnosis | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 71. PPS Code | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 72. External Cause of Injury code (E-Code) | 6 digits | Optional Enter the diagnosis code for the external cause of an injury, poisoning, or adverse effect. This code must begin with an "E". | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74. Principal Procedure Code/Date | 7 characters and 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74A. Other Procedure Code/Date | 7 characters and 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 76. Attending NPI - Required Attending Last/First Name | NPI - 10 digits Text | Health First Colorado ID Required NPI - Enter the 10-digit NPI number assigned to the physician having primary responsibility for the member's medical care and treatment. This number is obtained from the physician and cannot be a clinic or group number. (If the attending physician is not enrolled in the Health First Colorado or if the member leaves the ER before being seen by a physician, the hospital may enter their individual numbers.) Hospitals and FQHCs may enter the member's regular physician's 10-digit NPI in the Attending Physician ID form locator if the locum tenens physician is not enrolled in the Health First Colorado. QUAL - Enter "1D" for Medicaid. Enter the attending physician's last and first name. This form locator must be completed for all services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 77. Operating NPI | Optional Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 78 - 79. Other ID NPI - Required | NPI - 10 digits | Required Complete when attending physician is not the PCP or to identify additional physicians. Ordering, Prescribing, or Referring NPI NPI - Enter up to two (2) 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attending physician is not the PCP or if a clinic is a PCP agent, enter the PCP NPI number as the referring physician. The name of the Health First Colorado member's PCP appears on the eligibility verification. Review either for eligibility or PCP. Health First Colorado does not require that the PCP number appear more than once on each claim submitted. The attending physician's last and first name are optional. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 80. Remarks | Text | Enter specific additional information necessary to process the claim or fulfill reporting requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 81. Code - QUAL/CODE/VALUE (a-d) | Qualifier: 2 digits Taxonomy Code: 10 digits | Optional Complete both the qualifier and the taxonomy code for the billing provider in field 81CC-a. Field 81CC-a must be billed with qualifier B3 for the taxonomy code to be captured in the claims processing system. If B3 is missing, no taxonomy code will be captured in the claims processing system. Only one (1) taxonomy code can be captured from field 81CC. If more than one (1) taxonomy code is provided, only the first instance of B3 and taxonomy code will be captured in the claims processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Home Health Claim Example
Home Health Crossover Claim Example
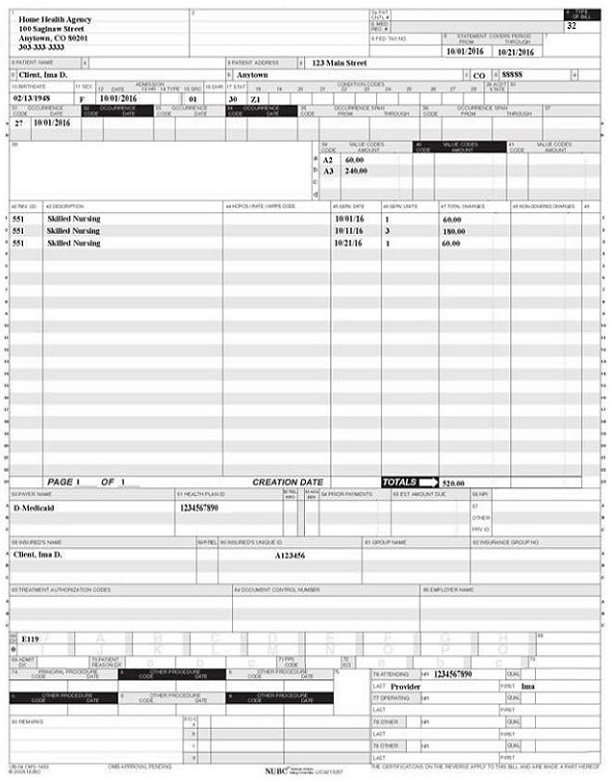
Note: Medicare crossover claims are valid only with Medicare claims for visits rather than episodes. LUPA payments not episode case mix payment.
Institutional Provider Certification
The Institutional Certification Form is located on the Provider Forms web page under the Claim Forms and Attachments drop-down menu.
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Early and Periodic Screening, Diagnostic and Treatment
Hospice benefits are provided in accordance with Early and Periodic Screening, Diagnostic and Treatment (EPSDT) requirements as listed in 8.280.4.E: “Other EPSDT Benefits” 8.280.4.E reads as follows:
Other health care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Section 1905(a) of the Social Security Act are a covered benefit under EPSDT when medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, regardless of whether such goods and services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a good or service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one (1) or more Activities of Daily Living; and meets the criteria set forth at Section 8.076.1.8.b - g.
- The service provides a safe environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly.
Providers can ask for these additional services by following the PAR process as outlined for this benefit.
Visit the EPSDT web page for more information regarding EPSDT.
Contact Gina Robinson at Gina.Robinson@state.co.us with questions about EPSDT.
Electronic Visit Verification
Federal guidance requires Electronic Visit Verification (EVV) for Home and Community Based Services (HCBS) that include an element of Personal Care Services and State Plan Home Health Care Services. Colorado requires the use of EVV for several other services that are similar in nature and delivery to the federally mandated services. These additional services are included to enhance care coordination, promote quality outcomes for members, and to streamline requirements for providers.
All Home Health services require EVV.
Visit the EVV web page or refer to the EVV Program Manual for further information regarding the EVV program. Contact EVV@state.co.us with EVV questions.
Home Health Billing Information Revisions Log
| Revision Date | Changes | Made by |
|---|---|---|
| Revision Date | Additions/Changes | Made by |
| 12/01/2016 | Manual revised for interChange implementation. Form annual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 3/08/2017 | Removed the 4 bullet items in the right column of row 44. | HCPF |
| 3/13/2017 | Updated the Type of Bill section in the Paper Claims Table to reflect the NUBC manual | HCPF |
| 3/14/2017 | Updated the type of bill in the paper claim examples | HCPF |
| 3/15/2017 | Updated Source of admission (Row 15) is Not Required | HCPF |
| 5/26/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 6/15/2018 | Updated timely filing information and removed references to LBOD, removed general billing information already available in the General Provider Information manual | DXC |
| 11/13/18 | Updated links to provider forms | HCPF |
| 2/20/19 | Updated Telehealth table to match the narrative regarding TG modifier below it. Removed reference to continuation claims, as we do take them | HCPF |
| 5/7/2019 | Changed language at bottom of page to correctly read 'occupational therapy' instead of 'speech therapy' | HCPF |
| 6/19/2019 | Updated Appendices' links and verbiage | DXC |
| 8/19/2019 | Updated logo usage and minor errors | DXC |
| 12/04/2019 | Converted to web page | HCPF |
| 8/7/2020 | Updated item 81 of the Paper Claim Reference Table for taxonomy code billing | DXC |
| 4/23/2021 | Updated Telehealth Remote Monitoring information to align CPT codes and clarify PAR requirements | HCPF |
| 9/17/2021 | Updated Billing manual with existing guidance regarding EPSDT and EVV | HCPF |
| 7/25/2022 | Clarifying CNA visits cannot be longer than 4 ½ consecutive hours | HCPF |
| 10/14/2022 | Removed Phone Number for fiscal agent. Linked verbiage to Provider Help web page. | HCPF |
| 9/11/2023 | Added the Ordering, Prescribing, Referring (OPR) Policy. Updated Field #78-79 on the claim reference table. | HCPF |
| 5/7/2024 | Update to Reimbursable Home Health Service Locations to remove restrictions for school settings. | HCPF |
| 7/24/2024 | Addition of POS 03-School as an allowed place of service | HCPF |