Federally Qualified Health Center and Rural Health Clinic Billing Manuals
- Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)
- Billing Information
- FQHC Services
- RHC Services
- FQHCs and RHCs Benefits
- UB-04 Paper Claim Reference Table
- Timely Filing
- Sterilization, Hysterectomies and Abortions
- Institutional Provider Certification
- FQHC/RHC Revisions Log
Return to Billing Manuals Web Page
Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid program) provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
Providers should refer to the Code of Colorado Regulations, Program Rules (10 C.C.R. 2505-10), for specific information when providing FQHC and RHC services.
FQHC
The U.S. Department of Health and Human Services certifies Federally Qualified Health Centers (FQHCs) that qualify as FQHCs. FQHCs may be either freestanding or federally defined as "provider based". FQHC services must be medically necessary and provided in outpatient settings only. Inpatient hospital stays are not included.
RHC
Rural Health Clinics (RHCs) are clinics located in rural areas and that have been certified under Medicare. These clinics are either freestanding or hospital affiliated. RHCs cannot be rehabilitation facilities or facilities primarily for the care and treatment of mental illness.
Billing Information
Refer to the General Provider Information Manual for general billing information.
For FQHCs participating in the Alternative Payment Methodology (APM) 2 reimbursement methodology, refer to the Alternative Payment Methodology 2 Billing Guidance located on the Federally Qualified Health Center Forms web page for more information.
Temporary Service Sites and Mobile Units
Mobile units and temporary service sites including temporary vaccination sites are not required to be separately enrolled with Health First Colorado. Temporary vaccination sites and mobile units can bill from the location where the staff or unit is based.
Per C.R.S. 25.5-4-420, which can be found on the Colorado Revised Statues web page on the Colorado General Assembly website, service sites that become permanent locations are required to obtain and use a unique National Provider Identifier (NPI) for each service location and enroll with Health First Colorado.
Health First Colorado policy requires that all FQHC locations enroll in Health First Colorado.
Colorado separately in order to obtain a separate Health First Colorado Provider ID. Hospital-based FQHCs are an exception to the policy and may use one (1) Provider ID for all sites on the main campus of the hospital-based FQHC. Hospital-based FQHCs are encouraged to obtain separate provider IDs for different locations on their main campus but are not required to do so. Mobile units of an FQHC are not required to be separately enrolled in Health First Colorado but are treated as part of the FQHC. Services provided in a temporary location do not require enrollment of the temporary location.
FQHC Services
Core services that are medically necessary are FQHC benefits. Core benefits include the following outpatient services:
- Physician services
- Physician assistant services
- Nurse practitioner services
- Nurse midwife services
- Clinical psychologist services
- Clinical social worker services
- Pneumococcal and influenza vaccines and administration
- Services and supplies incidental to professional services
- Part-time or intermittent nursing care and related medical supplies for homebound individuals
- Other reimbursable ambulatory services
- Dental
FQHCs that offer the Nurse Home Visitor Program (NHVP) and/or the Prenatal Plus Program are instructed to submit fee-for-service claims for services rendered under these programs. Claims for services should be submitted using the CMS 1500 and will be reimbursed based upon the supplemental fee schedule. All services provided under these two (2) programs must be excluded from the cost report as they are not considered when determining the encounter rates paid to FQHCs.
The NHVP is a home visitation program available to first-time moms in Colorado. Health First Colorado reimburses NHVP for targeted case management services provided to Health First Colorado members. The Prenatal Plus Program provides women access to a multidisciplinary care team throughout their pregnancy. Both programs have unique payment models and reporting mechanisms that necessitate Health First Colorado reimbursement remain separate from the encounter rate.
Rates for FQHCs are determined using an alternative payment methodology.
RHC Services
RHC services include:
- Services provided by a physician
- Services provided by physician assistants, nurse practitioners, and nurse midwives under the supervision of a physician
- Incidental related services and supplies, including visiting nurse care, and related medical supplies
- Other ambulatory services which meet specific program requirements
- Early and Periodic Screening, Diagnosis and Treatment (EPSDT) services which are not part of RHC services and meet EPSDT requirements
- Clinical psychologist services
- Clinical social worker services
FQHC and RHC Coding
Both FQHCs and RHCs use revenue codes to bill Health First Colorado.
FQHCs and RHCs Benefits
The valid revenue codes for reimbursement for services to the Health First Colorado are:
| Facility | Revenue code | Service |
|---|---|---|
| FQHC | 529 | Physical Health |
| RHC | 521 | Physical Health |
| FQHC/RHC | 900 | Behavioral Health |
Freestanding FQHC and RHC services are priced at an encounter rate. All routine services are included in the encounter rate.
In order to provide the Health First Colorado program with basic clinical information for use in evaluating services requested and received by Health First Colorado members, FQHCs are required to include all CPT codes and HCPCS codes for services provided during a visit on claims. In order to be reimbursed, an FQHC or RHC that submits a UB-04 or 837 Institutional (837I) electronic transaction must have at least one (1) claim line that identifies revenue code 0529 for FQHCs or revenue code 0521 for RHCs. All other lines on the claim should have the revenue code most appropriate for the service. The line item with revenue code 0529 or 0521 can appear at any line on the claim and with any procedure code.
Dental Services
CDT dental codes must be included on dental claims.
Beginning July 1, 2014, all FQHC claims for dental services and dentures must be submitted to DentaQuest, the Dental Administrative Service Organization (ASO), using the most current ADA Dental Claim form or by submitting the 837D electronic transaction via the DentaQuest Provider Web Portal. Information about claims submission for dental services can be found in the Office Reference Manual (ORM) under 'DentaQuest Resources' located on the Dentist page of DentaQuest's website.
Telemedicine
For Health First Colorado a billable encounter at an FQHC and RHC is an in person or telemedicine face to face visit with a Health First Colorado member. Telemedicine services are limited to the procedure codes identified in the Telemedicine Billing Manual. Services provided via telemedicine must use modifier GT on the claim. All other claim submission information is the same. Additionally, modifiers FQ and FR can be added to the claim:
- FQ: The service was furnished using audio-only communication technology.
- FR: The supervising practitioner was present through two-way, audio/video communication technology.
FQHCs, RHCs, and IHS providers can serve as an originating site allowing a member to connect with a distant provider that is not affiliated with the originating site. The service must be submitted on a professional service claim form (the 1500). Refer to the Telemedicine Billing Manual for the coverage of the originating site procedure code.
Imaging Services
For FQHCs, Health First Colorado does not cover the professional component of an imaging service as a billable encounter. Health First Colorado only allows reimbursement for a visit, which is a face-to-face encounter between a Health First Colorado member and a provider listed at 10 CCR 2505-10 sections 8.700.6 and 8.700.1. A direct visualization by a physician without the member present is not billable as an encounter. For the technical component of an imaging service, when free standing FQHCs own the equipment, the costs are accounted for in the Prospective Payment System (PPS) rate and the technical component is not billable. When free standing FQHCs order imaging from another provider, the technical component services are billed by the rendering provider. For hospital based FQHCs, the costs of imaging and labs are removed from the cost report when determining the encounter rate. Since the costs are removed from the cost report, the technical component of imaging may be billed separately to Health First Colorado by the hospital.
Long-Acting Reversible Contraceptives
Effective March 1, 2016, RHCs and their providers are able to bill for Long-Acting Reversible Contraceptive (LARC) devices on a Fee-For-Service (FFS) basis, outside of the normal FQHC and RHC billable encounter rate. Long-acting reversible contraceptive devices can be billed on the CMS 1500 claim form using the appropriate Healthcare Common Procedure Coding System (HCPCS) codes for the devices.
Short-Term Behavioral Health Services
Effective July 1, 2025, the Short-Term Behavioral Health (STBH) Benefit transitioned from FFS to the Behavioral Health Capitation. The standard psychotherapy services that were billable under the STBH Benefit will continue to be covered by Medicaid when provided by an FQHC or RHC, however these services must be billed to the RAEs. The following STBH codes may be billed using the 900 revenue code in accordance with the State Behavioral Health Services Billing Manual:
- 90791
- 90832
- 90834
- 90837
- 90846
- 90847
Per 10 CCR 25-05-10 8.700 FQHCs or RHCS can receive one (1) encounter payment for a behavioral health visit for a single patient in one (1) day.
Short-term behavioral health visits with dates of service before 7/1/25 should follow the prior STBH billing policy: the first six visits are billed to the Department using revenue code 900, and subsequent visits are billed to the RAE using revenue code 900.
Integrated Care Services
Effective July 1, 2025, FQHCs and RHCs may be reimbursed by Health First Colorado for Health Behavior Assessment & Intervention (HBAI) and Collaborative Care Model (CoCM) codes at the encounter rate. These sessions will not require a covered behavioral health diagnosis. These claims should be billed to the Department using the 900 revenue code. Integrated care services at FQHCs and RHCs, will follow standard reimbursement policies, including policies outlined in 10 CCR 2505-10 8.700. HBAI and CoCM procedure codes include:
HBAI
96156
96158
96159
96164
96165
96167
96168
96170
96171
CoCM
99484
99492
99493
99494
G0323
If a member receives both an integrated care service and a medical service on the same day, an FQHC must submit two (2) claims, one (1) with the HBAI or CoCM service using revenue code 900 and one (1) with the medical service using revenue code 529 for two (2) encounter rate payments from Health First Colorado.
A visit that includes an integrated care service and other behavioral health services should include all behavioral health services in the visit on the claim billed to Health First Colorado.
Per 10 CCR 25-05-10 8.700 FQHCs or RHCs can receive one (1) encounter payment for a behavioral health visit for a single patient in one (1) day. The FQHC or RHC is not allowed to bill for a behavioral health psychotherapy visit (to their RAE) and an integrated care visit (HBAI and CoCM) for the same member on the same day. The Department conducts ongoing retroactive review and compliance activities monitoring these policies.
For more information about integrated care and behavioral health services, please reference the Integrated Care Policy web page and the State Behavioral Health Services Billing Manual.
Behavioral Health Evaluation and Management Codes
Effective January 1, 2025, if a member receives FFS behavioral health evaluation and management (E/M) services, an FQHC or RHC must submit one (1) claim using revenue code 900 including the appropriate E/M code(s) to Health First Colorado.
A visit that includes FFS behavioral health E/M services and other behavioral health services should include all behavioral health services in the visit on the claim billed to Health First Colorado.
When billing for E/M consultation codes 99242-99245, FQHCs and RHCs should submit claims to the appropriate Regional Accountable Entity (RAE). Refer to Appendix E of the State Behavioral Health Services Billing Manual for information on when it is appropriate to use these consultation codes.
Per 10 CCR 25-05-10 8.700 FQHCs and RHCS can receive one (1) encounter payment for a behavioral health visit for a single patient in one (1) day.
eConsults
eConsult visits between primary care providers and specialty providers do not meet the definition of an FQHC or RHC visit as defined in 10 C.C.R. 2505-10 8.700. Costs associated with services provided through eConsult visits through an FQHC/RHC are considered allowable costs for the cost report and will be included in the calculation of the reimbursement rate for a patient visit at an FQHC/RHC.
Zero Pay Claims
If an FQHC submits claims that include two (2) codes that are included in the National Correct Coding Initiative (NCCI) Procedure to Procedure edits, the claim may result in $0 pay. FQHCs are required to comply with NCCI coding. Complying with NCCI coding will prevent $0 pay claims. Failure to include the National Drug Code (NDC) on claims that include a procedure for a physician-administered drug may result in $0 pay.
National Drug Code (NDC)
FQHCs and RHCs must include all non-carved out physician-administered drugs on claims when they are part of the treatment. Claims and encounters for physician-administered drugs purchased through the 340B program should include the "UD" code modifier on the 837P, 837I and CMS 1500 claim formats. For any physician-administered drugs not purchased through the 340B program, no code modifier is required. A valid national drug code (NDC) number must be included on all claims and encounters for physician-administered drugs. To assist providers with billing, an HCPCS/NDC crosswalk can be found under Appendices at /billing-manuals.
Same-Day Physical Health Visits
In accordance with 10 C.C.R. 2505-10 8.700 and 8.740, FQHCs and RHCs may bill for a second physical health encounter if after the first encounter, the member suffers illness or injury that requires a separate diagnosis or treatment.
A qualifying second, same day physical health visit should be submitted on a UB-04 claim form with a distinct diagnosis code(s) from the first encounter.
Obstetrics Billing at FQHCs and RHCs
Health First Colorado does not bundle payments for obstetrical services to FQHCs and RHCs. Prenatal and postpartum services should be billed on the UB-04 claim form with the appropriate codes for the services provided. For reporting purposes, F-codes can be included on the claim as outlined in the Obstetrical Care Billing Manual.
Labor and delivery (L&D) only services should be billed fee-for-service on the CMS 1500 claim form according to the Obstetrical Care Billing Manual.
Peer Support Services at FQHCs and RHCs
Services delivered by Peer Support Professionals at FQHCs and RHCs are not considered a billable visit per 10 C.C.R. 2505-10 8.700 and should be included in the FQHC/RHC cost report. Please see the Department’s Behavioral Health Policies, Standards, and Billing References webpage for information regarding Peer Support services and qualifying providers.
Abortion Services at FQHCs and RHCs
The Hyde Amendment, a legislative rider attached to annual federal appropriation bills, states that abortion services cannot be directly or indirectly funded by federal funds, except in cases of rape, incest, or when a pregnant person would be in danger of death if an abortion is not performed. Accordingly, abortion services are outside the scope of Medicare, Medicaid, IHS, and HRSA federal grant funds.
FQHCs, RHCs, and Tribal FQHCs can provide abortions as long as they do not use federal funds. To ensure compliance with these requirements and ensure that abortion services are reimbursed solely with state funds authorized by Senate Bill 25-183, FQHCs, RHCs, and Tribal FQHCs must report the service on the claim using ICD-10-CM diagnosis code Z33.2.
Transitions of Care (TOC) Services
Effective January 1, 2026, FQHCs and RHCs may bill for TOC codes 99495 and 99496. TOC services that meet the definition of an FQHC or RHC visit should be billed directly to HCPF using revenue code 529 (FQHCs) or revenue code 521 (RHCs). Refer to the Accountable Care Collaborative Provider and Stakeholder Resource Center web page for additional information on the TOC codes.
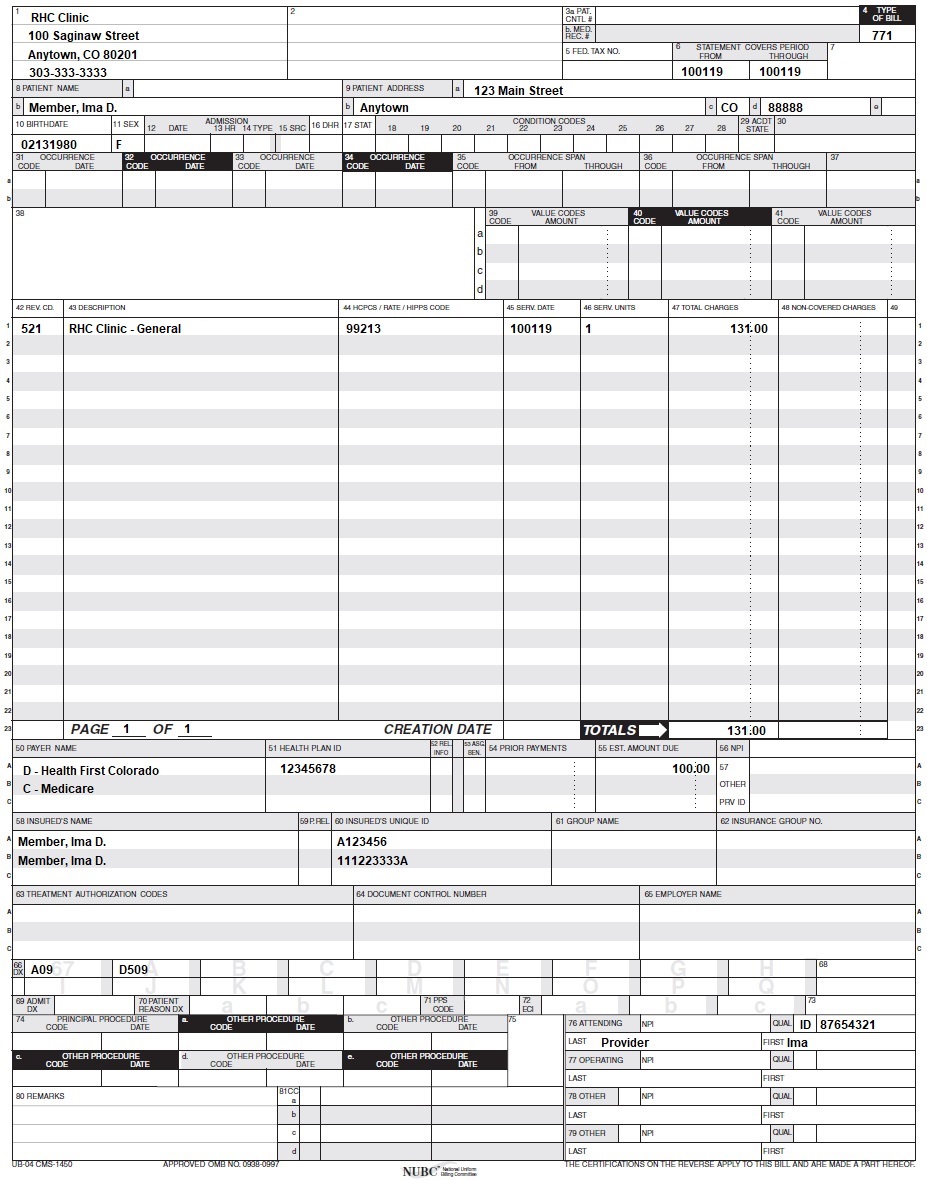
UB-04 Paper Claim Reference Table
The information in the following table provides instructions for completing form locators (FL) as they appear on the paper UB-04 claim form. Instructions for completing the UB-04 claim form are based on the current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data form locators on the UB-04 have the same attributes (specifications) for the Health First Colorado as those indicated in the NUBCUB-04 Reference Manual.
All code values listed in the NUBCUB-04 Reference Manual for each form locator may not be used for submitting paper claims to the Health First Colorado. The appropriate code values listed in this manual must be used when billing the Health First Colorado.
The UB-04 Institutional Certification Form, located on the Provider Forms web page under the Claim Forms and Attachments drop-down menu, must be completed and attached to all claims submitted on the paper UB-04. Completed UB-04 paper Health First Colorado claims, including hardcopy Medicare claims, should be mailed to the correct fiscal agent address listed in Appendix A, under the Appendices drop-down section on the Billing Manuals web page.
Do not submit "continuation" claims. Each claim form has a set number of billing lines available for completion. Do not crowd more lines on the form. Billing lines in excess of the designated number are not processed or acknowledged. Claims with more than one (1) page may be submitted through the Provider Web Portal.
The Paper Claim Reference Table below lists the required, optional and/or conditional form locators for submitting the paper UB-04 claim form to the Health First Colorado for FQHC and RHC services.
| Form Locator and Labels | Completion Format | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Billing Provider Name, Address, Telephone Number | Text | Abbreviate the state using standard post office abbreviations. Enter the telephone number.
Abbreviate the state using standard post office abbreviations. Enter the telephone number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Pay-to Name, Address, City, State | Text | Required only if different from FL 1.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3a. Patient Control Number | Up to 20 characters: Letters, numbers or hyphens | Optional Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3b. Medical Record Number | 17 digits | Optional Enter the number assigned to the member to assist in retrieval of medical records. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Type of Bill | 3 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Federal Tax Number | None | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Statement covers period From/Through | From:6 digits MMDDYY Through: 6 digits MMDDYY | Required Each date of service must be billed on a separate line. Split an entire month into two (2) claims. This FL must reflect the beginning and ending dates of service listed on the detail dates of service lines. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8a. Patient Identifier | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8b. Patient Name | Up to 25 characters, letters and spaces | Required Enter the member's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Patient Address - Street | Characters Letters and numbers | Required Enter the member's street/post office box as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Patient Address - City | Text | Required Enter the member's city as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Patient Address - State | Text | Required Enter the member's state as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Patient Address - ZIP | Digits | Required Enter the member's zip code as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9e. Patient Address - Country Code | Digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10. Birthdate | 8 digits (MMDDYYYY) | Required Enter the member's birthdate using two (2) digits for the month, two (2) digits for the date, and four (4) digits for the year (MMDDYYYY format). Example: 01012010 for January 1, 2010. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Patient Sex | 1 letter | Required Enter an M (male) or F (female) to indicate the member's sex. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Admission Date | 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Admission Hour | 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Admission Type | 1 digit | Conditional Complete for emergency visits. 1 - Emergency Member requires immediate intervention as a result of severe, life threatening or potentially disabling conditions. Exempts outpatient hospital claims from co-payment and PCP referral only if Revenue Code 0450 or 0459 is present. This is the only benefit service for an undocumented alien. If span billing, emergency services cannot be included in the span bill and must be billed separately from other outpatient services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Source of Admission | 1 digit | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Discharge Hour | 2 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Patient Discharge Status | 2 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18-28. Conditions Codes | 2 digits | Conditional Complete with as many codes necessary to identify conditions related to this bill that may affect payer processing.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Accident State | 2 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31 - 34. Occurrence Code/Date | 2 digits and 6 digits | Conditional
*Other Payer occurrence codes 24 and 25 must be used when applicable. The claim must be submitted with the third-party information. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35-36. Occurrence Span Code From/ Through | 2 and 6 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38. Responsible Party Name/Address | None | Leave blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39 - 41. Value Codes and Amounts | 2 characters and up to 9 digits | Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 42. Revenue Code | 3 digits | Required
RHCs | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 43. Revenue code Description | Text | Required
Example:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 44. HCPCS/Rates/ HIPPS Rate Codes | 5 digits | FQHC
HCPCS codes cannot be repeated for the same date of service. Combine the units in FL 46 (Units) to report multiple services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 45. Service Date | 6 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 46. Service Units | Up to 3 digits | Required Enter a unit value on each line completed. Use whole numbers only. Do not enter fractions or decimals and do not show a decimal point followed by a 0 to designate whole numbers (e.g., Do not enter 1.0 to signify one (1) unit) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 47. Total Charges | Up to 9 digits | Required Enter the total charge for each line item. Calculate the total charge as the number of units multiplied by the unit charge. Do not subtract Medicare or third-party payments from line charge entries. Do not enter negative amounts. A grand total in line 23 is required for all charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 48. Non-covered Charges | Up to 9 digits | Required Enter incurred charges that are not payable by the Health First Colorado. Non-covered charges must be entered in both FL 47 (Total Charges) and FL 48 (Non-Covered Charges). Each column requires a grand total. Non-covered charges cannot be billed for outpatient hospital laboratory or hospital-based transportation services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 50. Payer Name | 1 letter and text | Enter the payment source code followed by name of each payer organization from which the provider might expect payment.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 51. Health Plan ID | 8 digits | Required Enter the provider's Health Plan ID for each payer name. Enter the eight (8)-digit Health First Colorado Program provider number assigned to the billing provider. Payment is made to the enrolled provider or agency that is assigned this number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 52. Release of Information | None | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 53. Assignment of Benefits | None | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 54. Prior Payments | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter third party and/or Medicare payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 55. Estimated Amount Due | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter the net amount due from Health First Colorado after provider has received other third party, Medicare or member liability amount. Medicare Crossovers Enter the sum of the Medicare coinsurance plus Medicare deductible less third-party payments and member payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 56. National Provider Identifier (NPI) | 10 digits | Required Enter the billing provider's 10-digit National Provider Identifier (NPI). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 57. Other Provider ID | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 58. Insured's Name | Up to 30 characters | Required Enter the member's name on the Health First Colorado line. Other Insurance/Medicare Complete additional lines when there is third party coverage. Enter the policyholder's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 60. Insured's Unique ID | Up to 20 characters | Required Enter the insured's unique identification number assigned by the payer organization exactly as it appears on the health insurance card. Include letter prefixes or suffixes shown on the card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 61. Insurance Group Name | 14 letters | Conditional Complete when there is third party coverage. Enter the name of the group or plan providing the insurance to the insured exactly as it appears on the health insurance card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 62. Insurance Group Number | 17 digits | Conditional Complete when there is third party coverage. Enter the identification number, control number, or code assigned by the carrier or fund administrator identifying the group under which the individual is carried. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 63. Treatment Authorization Code | Up to 18 characters | Conditional Complete when the service requires a PAR. Enter the authorization number in this FL if a PAR is required and has been approved for services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 64. Document Control Number | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 65. Employer Name | Text | Conditional Complete when there is third party coverage. Enter the name of the employer that provides health care coverage for the individual identified in FL 58 (Insured Name). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 66. Diagnosis Version Qualifier | Submitted information is not entered into the claim processing system. Enter applicable ICD indicator to identify which version of ICD codes is being reported. 0ICD-10-CM (DOS 10/1/15 and after) 9ICD-10-CM (DOS 9/30/15 and before) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67. Principal Diagnosis Code | Up to 6 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67A. - 67Q. - Other Diagnosis | 6 digits | Optional Enter the exact diagnosis code corresponding to additional conditions that co-exist at the time of admission or develop subsequently and which effect the treatment received or the length of stay. Do not add extra zeros to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 69. Admitting Diagnosis Code | 6 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 70. Patient Reason Diagnosis | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 71. PPS Code | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 72. External Cause of Injury code (E-Code) | 6 digits | FQHC Required if known Enter the diagnosis code for the external cause of an injury, poisoning, or adverse effect. This code must begin with an "E". RHC Optional Enter the diagnosis code for the external cause of an injury, poisoning, or adverse effect. This code must begin with an "E". | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74. Principal Procedure Code/Date | 7 characters and 6 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74A. Other Procedure Code/Date | 7 characters and 6 digits | Conditional Complete when there are additional significant procedure codes. Enter the procedure codes identifying all significant procedures other than the principal procedure and the dates on which the procedures were performed. Report those that are most important for the episode of care and specifically any therapeutic procedures closely related to the principal diagnosis. Enter the date using MMDDYY format. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 76. Attending NPI - Required Attending Last/First Name | NPI - 10 digits Text | Health First Colorado ID Required NPI - Enter the 10-digit NPI number assigned to the physician having primary responsibility for the member's medical care and treatment. This number is obtained from the physician and cannot be a clinic or group number. (If the attending physician is not enrolled in Health First Colorado or if the member leaves the ER before being seen by a physician, the hospital may enter their individual numbers.) Hospitals and FQHCs may enter the member's regular physician's 10- digit NPI in the Attending Physician ID form locator if the locum tenens physician is not enrolled in the Health First Colorado. QUAL - Enter "1D" for Health First Colorado Enter the attending physician's last and first name. This form locator must be completed for all services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 77. Operating NPI | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 78 - 79. Other ID NPI - Conditional | NPI - 10 digits | Conditional Complete when attending physician is not the PCP or to identify additional physicians. NPI - Enter up to two (2) 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attending physician is not the PCP or if a clinic is a PCP agent, enter the PCP NPI number as the referring physician. The name of the Health First Colorado member's PCP appears on the eligibility verification. Review either for eligibility or PCP. The Health First Colorado does not require that the PCP number appear more than once on each claim submitted. The attending physician's last and first name are optional. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 80. Remarks | Text | Enter specific additional information necessary to process the claim or fulfill reporting requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 81. Code - QUAL/CODE/VALUE (a-d) | Qualifier: 2 digits Taxonomy Code: 10 digits | Optional Complete both the qualifier and the taxonomy code for the billing provider in field 81CC-a. Field 81CC-a must be billed with qualifier B3 for the taxonomy code to be captured in the claims processing system. If B3 is missing, no taxonomy code will be captured in the claims processing system. Only one (1) taxonomy code can be captured from field 81CC. If more than one (1) taxonomy code is provided, only the first instance of B3 and taxonomy code will be captured in the claims processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
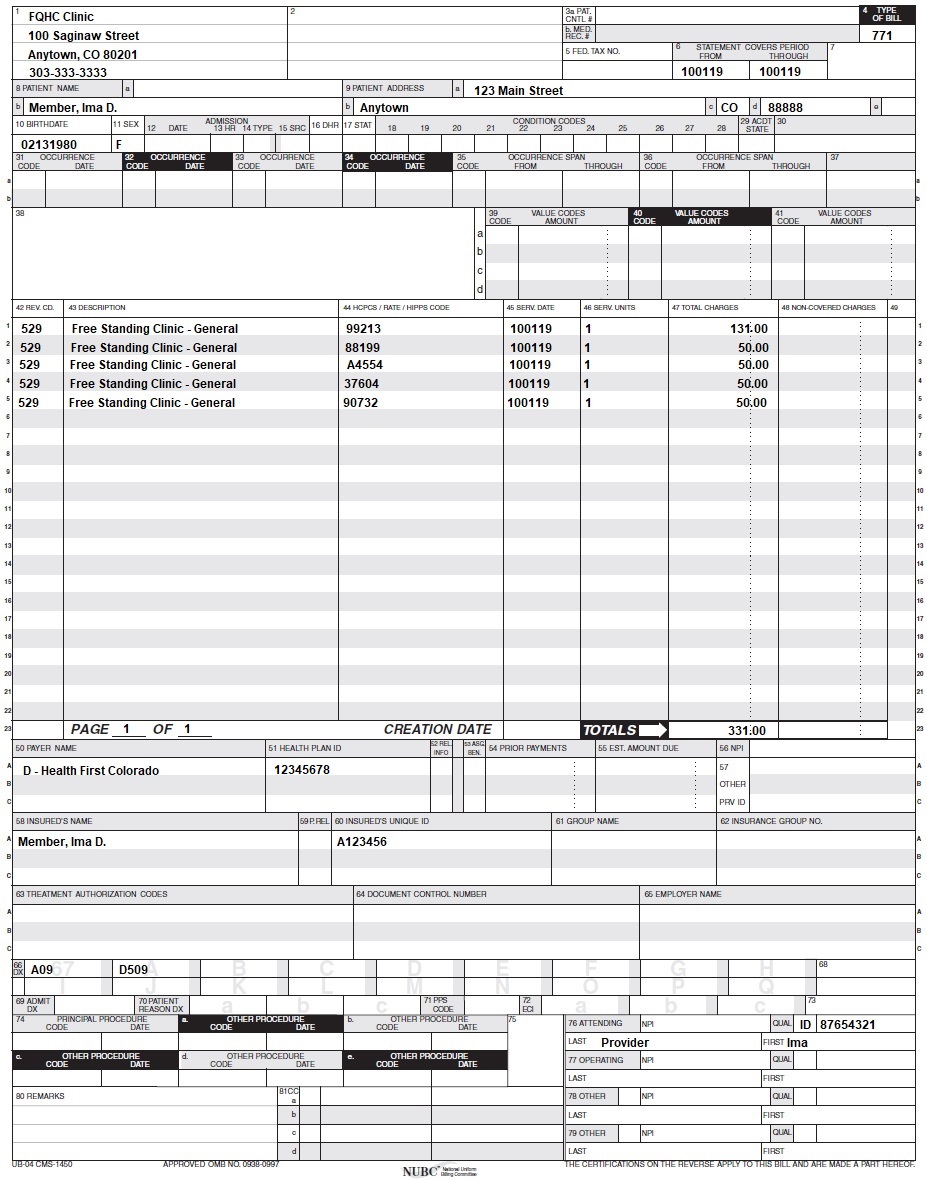
FQHC Claim Example
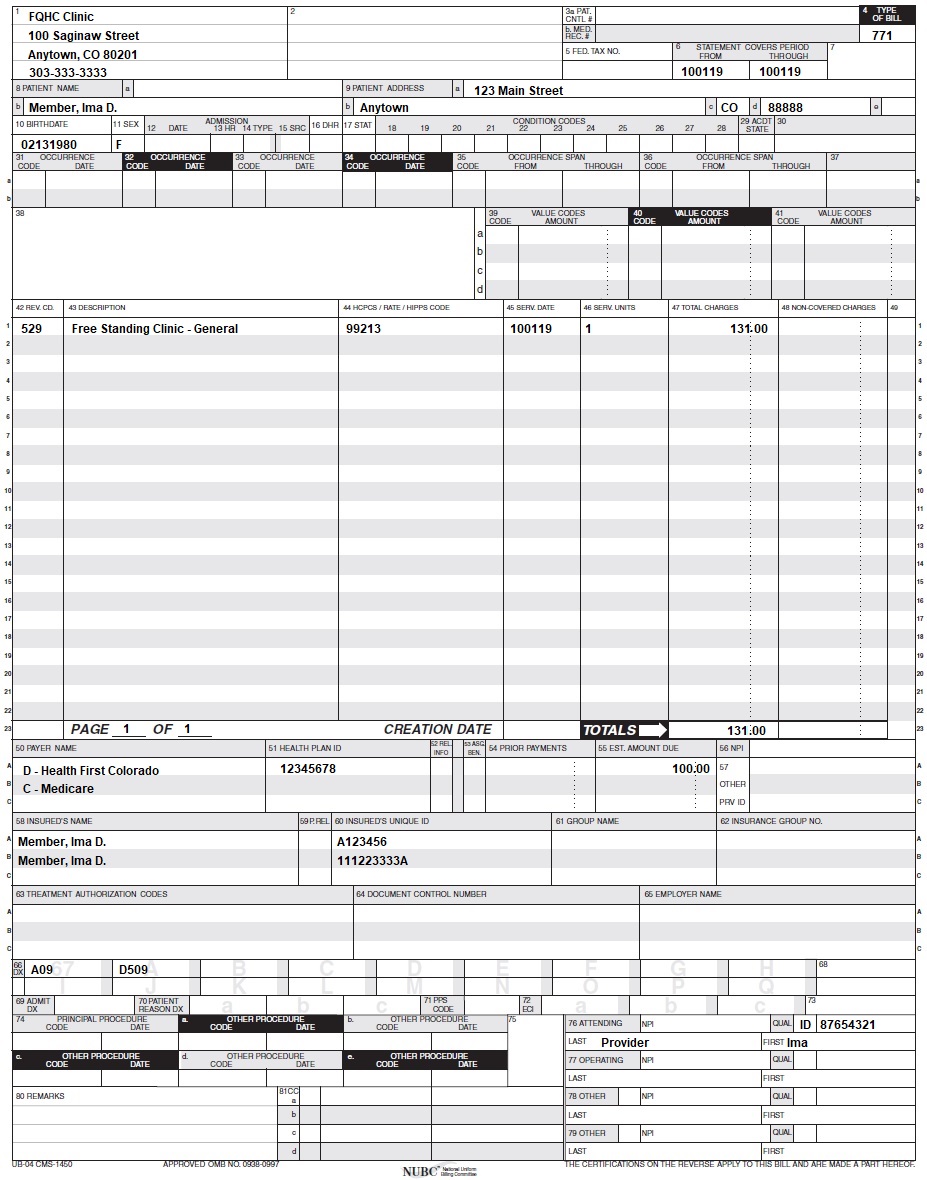
FQHC Crossover Claim Example
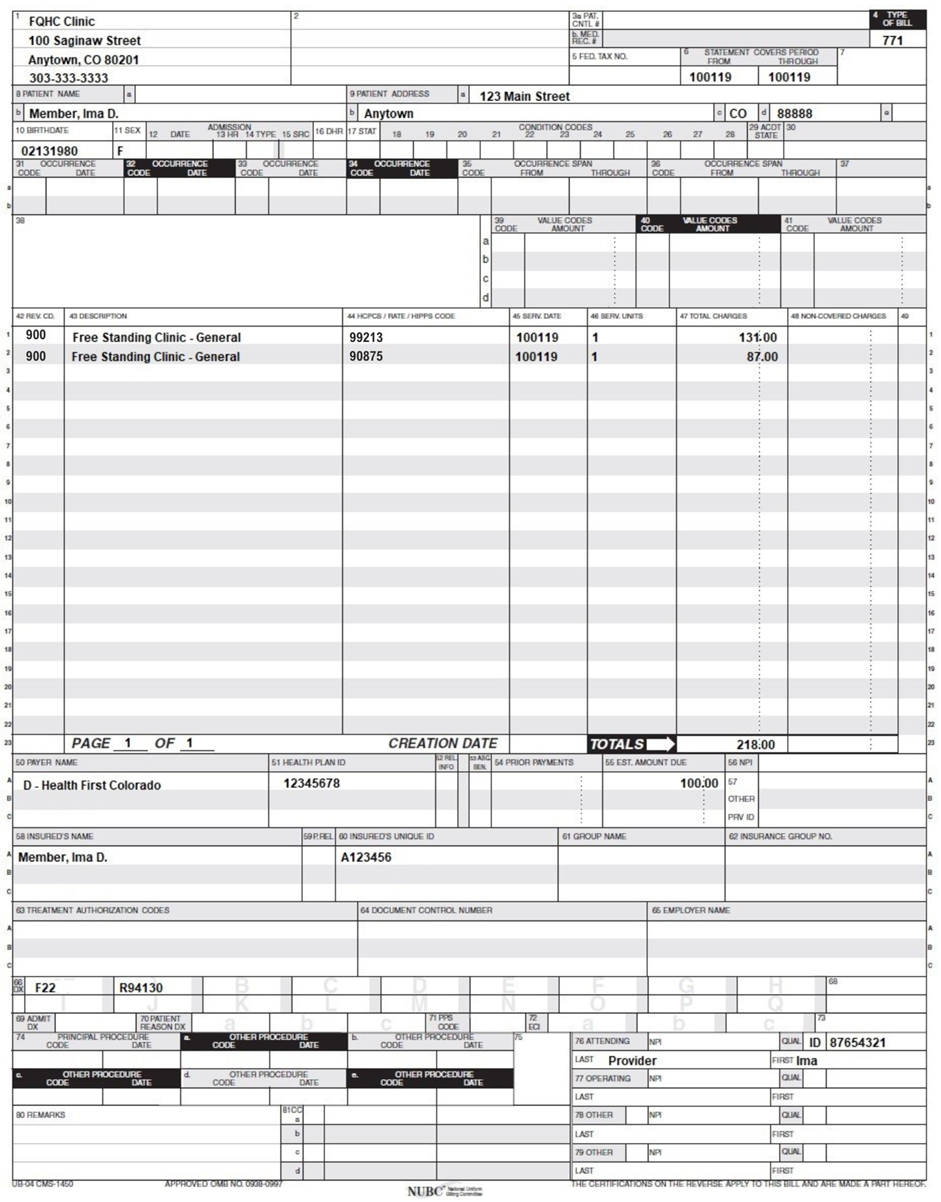
FQHC Behavioral Health E/M FFS Claim Example
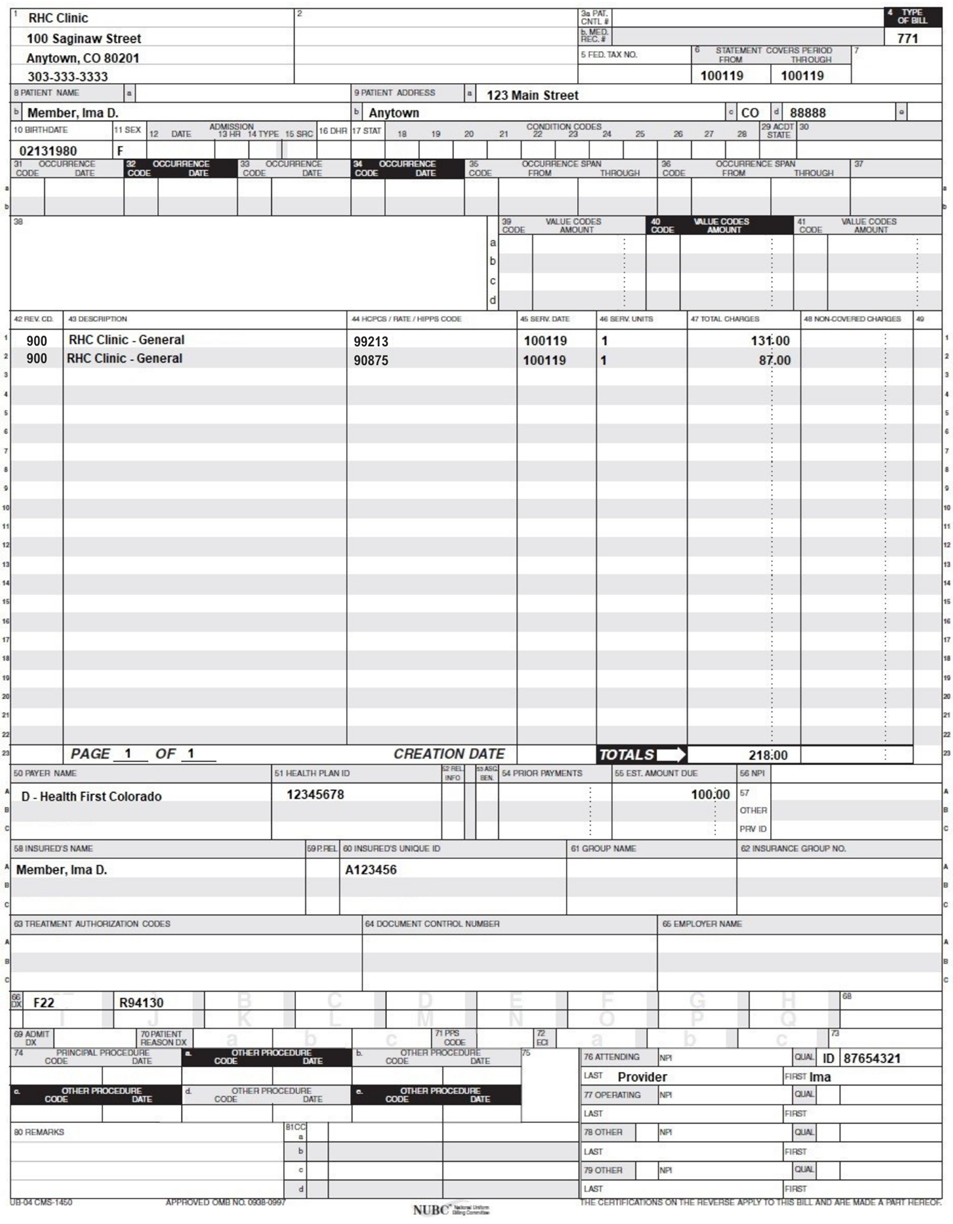
RHC Behavioral Health E/M FFS Claim Example
RHC Crossover Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
Sterilization, Hysterectomies and Abortions
Refer to the Obstetrical Care Billing Manual located on the Billing Manuals web page under the CMS 1500 drop-down menu for more information on sterilization, hysterectomies and abortions.
Institutional Provider Certification
The UB-04 Institutional Certification Form is located on the Provider Forms web page under the Claim Forms and Attachments drop-down menu.
FQHC/RHC Revisions Log
| Revision Date | Addition/Changes | Made by |
| 12/01/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016 Please refer to Archive. | HPE (now DXC) |
| 1/19/2017 | Updates based on the Colorado iC Stage II Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 2/9/2017 | Added RAE E&M policy and Type of Bill 77x | HCPF |
| 2/9/2017 | Made formatting changes to references of FQHCs and RHCs | HCPF |
| 5/17/2017 | Updated the Freestanding FQHCs and RHCs section | HCPF |
| 5/17/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 1/2/2018 | Revenue Code Description - instructions for reporting an NDC | DXC |
| 6/22/2018 | Updated general billing and timely filing, changed BHO to RAE | HCPF |
| 7/11/2019 | Updated Appendices' links and verbiage | DXC |
| 8/21/2019 | Added language for valid revenue codes | HCPF |
| 8/22/2019 | Updated links, removed duplicated information | HCPF |
| 11/20/2019 | Added clarification to 0529 | HCPF |
| 8/7/2020 | Updated item 81 of the Paper Claim reference Table for taxonomy code billing | DXC |
| 12/2/2020 | Updated billable encounter information, replaced instances of Colorado Medicaid with Health First Colorado | HCPF |
| 2/18/2022 | Enrollment of Temporary Service Sites and Mobile Unit Policy Clarification | HCPF |
| 7/1/2022 | Added APM 2 Billing Guidance link | HCPF |
| 8/5/2022 | Added FQ and FR modifier information | HCPF |
| 3/7/2024 | Updated link for C.R.S. 25.5-4-420 | HCPF |
| 4/24/2024 | Removed outdated E/M guidance | HCPF |
| 5/15/2024 | Added eConsult information | HCPF |
| 11/12/2024 | Added language clarifying FQHC billing process for FFS behavioral health E/M services | HCPF |
| 12/19/2024 | Added language clarifying RHC billing process for FFS behavioral health E/M services | HCPF |
| 02/05/2025 | Updated claim example images for FQHC and RHC RAE claims | HCPF |
| 04/15/2025 | Added billing guidance for same-day physical health visits and obstetrics services at FQHCs and RHCs | HCPF |
| 07/25/2025 | Updated the STBH section and added new integrated care billing guidance. | HCPF |
| 09/03/2025 | Updated language in Dental Services section. | HCPF |
| 10/01/2025 | Added clarification language to Short-Term Behavioral Health section. | HCPF |
| 11/17/2025 | Added billing guidance for peer support services. | HCPF |
| 12/18/2025 | Added abortion care billing guidance | HCPF |
| 12/23/2025 | Added Transitions of Care billing guidance | HCPF |