Non-Emergent Medical Transportation (NEMT) Billing Manual
- Benefit Overview
- General Billing Information
- NEMT Administration
- Eligible Providers
- Payment for Covered Services
- Member Eligibility
- Prior Authorization
- Covered Benefits and Limitations
- Urgent NEMT
- Exclusions
- Resources
- Procedure Coding
- NEMT Billing Information
- CMS Paper Claim Reference Table
- Timely Filing
- NEMT Billing Manual Revisions Log
Return to Billing Manuals Web Page
Benefit Overview
Non-emergent medical transportation (NEMT) is transportation to and from medically necessary services covered by Health First Colorado (Colorado's Medicaid program) for members who have no other means of transportation, including free transportation. NEMT can only be utilized to access non-emergency services.
NEMT can only be utilized to transport eligible members to and from Health First Colorado provider service locations that are enrolled to provide the service the member is transported to receive. Refer to the Find a Doctor tool to determine if a provider or service location is an approved Health First Colorado provider. NEMT must be used to access the closest qualified Health First Colorado provider willing and able to treat the member. NEMT can only be used to access non-emergency services. Transportation to receive Home and Community Based Services (HCBS) must be provided through Non-Medical Transportation (NMT).
Providers must be enrolled as a Health First Colorado provider in order to:
- Provide NEMT services to a Health First Colorado member
- Submit claims for payment to Health First Colorado
Providers should refer to the Code of Colorado Regulations (CCR), Program Rules (10 CCR 2505-10), for specific information when providing NEMT services.
NEMT Regulations can be found in 10 CCR 2505-10 8.014.
Emergency Medical Transportation (EMT) regulations allow inter-facility transfers between hospitals to be billed as EMT services. These transfers can include transportation of people who are experiencing a mental health or substance use disorder crisis.
Any services provided by Transportation Network Companies, as defined in 4 CCR 723-6701 (e.g., Uber, Lyft), are not covered or reimbursed under NEMT. Ride-sharing companies are not enrolled providers, and the Department of Health Care Policy & Financing (the Department) is unable to pay for or reimburse for use of these services.
An exception may be made, at the Department's discretion, for covered Out-of-State trips. The Department does not maintain a network of providers outside the State of Colorado and therefore may provide reimbursement for Members who have an approved NEMT Out-of-State trip.
9-1-1 response calls are not NEMT. If transportation is provided to the member in response to a 9-1-1 call, and the service meets the requirements of EMT, the service may be billed as EMT services.
General Billing Information
Refer to the General Provider Information Manual for general billing information.
NEMT Administration
The Department has established a State Designated Entity (SDE) responsible for administering NEMT in nine Colorado counties: Adams, Arapahoe, Boulder, Broomfield, Denver, Douglas, Jefferson, Larimer, and Weld. The SDE explores and utilizes the least costly, medically appropriate means of transportation for each member and arranges those transportation services. IntelliRide by TransDev Health Solutions is the Department’s State Designated Entity as its contracted NEMT broker.
NEMT providers help with administration in the remaining 55 counties.
Provider Responsibilities
Local NEMT providers outside of the nine (9) county broker service area will be responsible for the following:
- Verifying member and medical provider eligibility for all trip requests through Batch 270, the Provider Services Call Center Integrated Voice Response (IVR) system or the Provider Web Portal
- Verifying and retaining documentation for all trip requests including but not limited to: all required standard forms listed in this billing manual
Local transportation providers outside the broker service area are responsible for submitting their own claims through the Provider Web Portal. Claims should include the required information for each trip and corresponding documentation, as referenced in this billing manual.
Refer to HCPF OM-074 for contextual information.
Required Member Eligibility Verification Procedures
Effective June 1, 2025, Operational Memo OM25-028 has been published to instruct NEMT providers of the required procedures for verifying member benefit eligibility and documenting transportation requests. Following the procedures of this memo is mandatory for all NEMT providers outside of the current broker network (e.g., providers who do not receive trip assignments from the broker and who submit claims directly to the Department).
Eligible Providers
To provide NEMT services to Health First Colorado members and receive reimbursement, a provider must:
Have each of their drivers and vehicles credentialed. Providers are prohibited from providing NEMT services using drivers or vehicles that fail credentialing.
Credentialing with Transdev Health Solutions (formerly Intelliride)
All NEMT providers must be credentialed to provide Health First Colorado services. This includes all drivers and vehicles. Transdev Health Solutions manages driver and vehicle credentialing for all NEMT providers statewide.
Failure to complete this process will result in further action being taken in accordance with Section 25.5-4-301, C.R.S. and 10 C.C.R. 2505-10, Section 8.076.- Complete the Credentialing Request Form and License Agreement. Providers will receive an email that includes a username, password and link to sign up for software training.
- Participate in a credentialing software training session to learn how to use the software.
- Visit Platform.ProCredEx.com to upload the required driver and vehicle credentials.
- Sign up for a vehicle inspection. Vehicle inspections are required. Visit the Transdev Health Solutions website for a list of dates and times for inspections.
Transdev Health Solutions will review and provide a credentialing certificate once these steps are completed. This certificate must be submitted with the provider’s Health First Colorado revalidation application.
Contact ProCredex Provider Support at Support@procredex.com for support with the credentialing process.
Important: Any new drivers and vehicles added to the business, at any time, must be approved before they can be used to transport Health First Colorado members. Credentials for new drivers and vehicles must be submitted through the credentialing software. Any driver or vehicle which fails credentialing is prohibited from being used to provide NEMT services to Health First Colorado members.
Vehicle Inspections
All vehicles must be inspected regardless of the age of the current inspection. Providers must contact Transdev Health Solutions to schedule an inspection date and time.
Contact Transdev Health Solutions Provider Support at 833-643-3010 or email US.THSProviders@transdev.com with questions.- If in the nine (9)-county broker service area, contact the State-Designated Entity in the area to determine the need for providers, and the policies and procedures in that area. The SDE may require an agreement or contract to address processes and requirements specific to that SDE. All NEMT providers in the State-contracted broker service area must be fully credentialed by the broker before providing services. There may be a wait to become a provider based on the network need.
- Obtain the appropriate license, certificate, or permit for the services you want to provide. Licensure, or proof of exemption from licensure requirements, must be included in the Health First Colorado NEMT provider application. To determine the appropriate licensure, contact:
- Ground ambulances: Licensing of ground ambulance services are conducted by county governments. Contact the county commissioner’s office for specific county ambulance licensing requirements and/or verification of a valid license.
- Air ambulances: Air ambulance services are regulated by the state when they transport patients out of Colorado. If your air ambulance service agency wants to provide this service, it must be either licensed or authorized by the Colorado Department of Public Health and Environment.
- All other providers: Gainwell or County.
- Complete provider enrollment to become a Health First Colorado NEMT provider. Visit the Provider Enrollment web page for enrollment information.
- To be eligible to be reimbursed for Health First Colorado NEMT claims, providers must enroll correctly prior to providing services.
- Provider Type/Code: 73 – Transportation (Non-Emergent Medical Transportation)
- Specialty: Transportation Broker - Non-Emergency Medical Specialty Code: 326 This is for NEMT providers, that are providing services within the State-contracted broker’s service area: Adams, Arapahoe, Boulder, Broomfield, Denver, Douglas, Jefferson, Larimer, and Weld Counties.
- Specialty: Non-Emergency Medical Specialty Code: 525
This is for non-emergency medical transportation (NEMT) providers, including county departments of human services, that provide services in any county outside of: Adams, Arapahoe, Boulder, Broomfield, Denver, Douglas, Jefferson, Larimer, and Weld Counties.
- To be eligible to be reimbursed for Health First Colorado NEMT claims, providers must enroll correctly prior to providing services.
Note: Providers enrolled as any other provider type/code must complete a separate enrollment application to be eligible to provide NEMT services.
Ambulance Providers
Ambulance providers must complete a separate enrollment application to be eligible to provide Emergency Medical Transportation services.
HCBS Non-Medical Transportation (NMT) Providers
To provide Non-Medical Transportation (NMT) services, a separate enrollment application is necessary to submit claims for NMT services. A provider cannot bill NMT services through their NEMT Provider ID.
Exceptions
The only exceptions to these provider requirements are reimbursements or mileage paid to members, members' family, members' friends, or volunteers for covered services, and commercial air, train, and bus tickets. Lodging providers are not required to obtain PUC or ambulance licensure but must enroll as a Health First Colorado NEMT provider in order to submit claims for services.
Payment for Covered Services
Payment will only be made for the least expensive mode suitable to the member's condition.
Providers in the state-contracted broker service area must be enrolled in the broker's network in order to provide services and receive payment for covered services. The broker pays enrolled providers directly for NEMT services. Services provided in the broker service area are only reimbursable by the State Contracted Broker and cannot be submitted directly to the Department.
Reimbursement for services provided outside the state-contracted broker service area should be submitted directly to the Department.
Regardless of whether Health First Colorado has actually reimbursed the provider, billing members for covered services is strictly prohibited. Balance billing is prohibited. If reimbursement is made, providers must accept this payment as payment in full. Refer to Program Rule 8.012. The provider may only bill the member for services not covered by Health First Colorado.
Member Eligibility
To receive NEMT, a person must:
- Be a current Health First Colorado member, receiving Medicaid State Plan/Title XIX coverage on the date of service,
- Not have access to other means of transportation including free transportation and the Program of All-Inclusive Care for the Elderly (PACE),
- Require transportation to obtain non-emergency Health First Colorado covered medical services at Health First Colorado enrolled providers, and
Not be within the following eligibility groups or benefit plans:
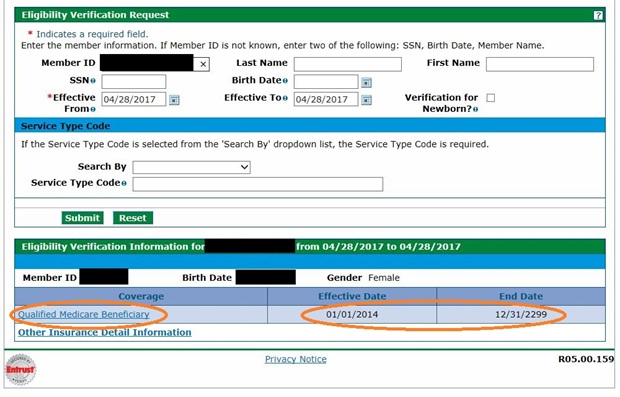
- Qualified Medicaid Beneficiary (QMB) Only
- Special Low-Income Medicare Beneficiary (SLMB) Only
- Medicare Qualifying Individual-1 (QI-1)
- Old Age Pension- State Only (OAP-state only)
- EMS - Emergency Medicaid and Reproductive Health Program” benefit plan coverage
Note: Child Health Plan Plus (CHP+) is not Health First Colorado and, therefore, is not eligible for NEMT services.
Provider Web Portal example of a member eligible for NEMT services:
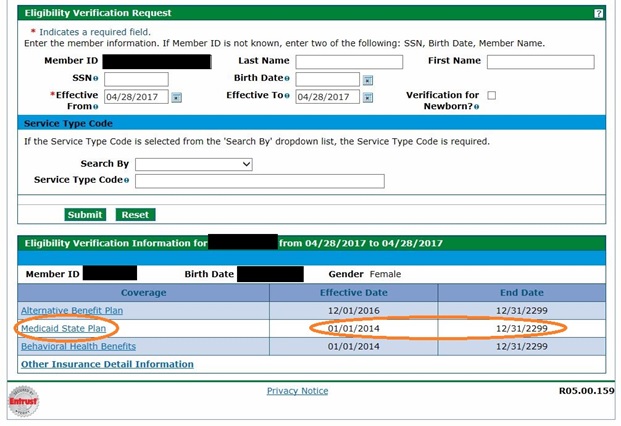
The member is not eligible for NEMT services if the member has only QMB coverage without "Medicaid State Plan."
Prior Authorization
All NEMT requests must be sent to the State Designated Entity (SDE) or, outside the broker service area. an NEMT provider. The member, or member's representative, is responsible for obtaining prior authorization and should be requested as soon as possible. Transportation provided without authorization from the SDE or provider, or their designee, will not be reimbursed or paid. For information on the SDE's or a provider’s authorization processes, contact the SDE or provider directly.
While not requiring prior authorization, mileage or bus pass reimbursement may be denied if the member does not provide proper documentation to the State Designated Entity within timely filing requirements, or sooner if required by the State Designated Entity's policies.
Train, Air and Out-of-State Travel
Train, air and out-of-state travel must be prior authorized by the Department. Members and/or medical professionals requesting train, air or out-of-state travel must contact their SDE.
NEMT can only be used to access approved medical services. 10 CCR 2505-10 8.013 requires all medical services to be provided in Colorado, unless the service is not available in-state.
Transportation of the member’s escort is covered for the return trip of the escort if they will not be accompanying the member for a complete round trip. This is applicable for circumstances in which the member is being placed in facility/residential treatment and the escort will not be staying with them.
Billing Instructions: The Health First Colorado ID of the person being transported should always be used for billing. However, if the person being transported is not enrolled in Health First Colorado or does not have an active Health First Colorado ID, the Health First Colorado ID of the child for whom the transportation is of direct benefit should be used for billing. This ensures that the transportation is correctly attributed to the child’s medically necessary care.
The SDE will request the required documentation and submit to the Department for review and decision. The decision will be communicated to the SDE.
SDEs must submit a completed NEMT Air, Train, and Out-of-State Request Form as indicated on the form. The form is located on the NEMT web page.
All rules and practices for in-state NEMT apply to travel for routine medical services provided to members in Colorado border communities performed across the state line in a Border Town/City indicated in Appendix F because of closer proximity to the closest qualified provider. Refer to Appendix F located on the Billing Manuals web page under the Appendices drop-down.
Covered Benefits and Limitations
Non-Emergent Medical Transportation (NEMT) is a Health First Colorado benefit when the member has no other means of transportation. The transportation services must be medically necessary and provided within the scope of the provider's certification and/or license. Transportation for Health First Colorado members to and from a medical provider is a benefit when the medical service provided is a benefit of the Health First Colorado and the provider is enrolled with Health First Colorado to deliver the service.
There is no limit to the number of daily trips a client can receive from one or multiple providers, but those trips must meet all NEMT regulatory and policy requirements. Billing multiple trips for one member in one day with different rendering providers may require the use of a modifier. Refer to the Procedure Coding section below.
The following modes of transportation are covered:
- Public/Mass Transportation
- Personal vehicle mileage reimbursement
- Mobility/Ambulatory vehicles
- Wheelchair van
- Taxicab
- Stretcher van
- Ambulance, ground and air
- Commercial plane
- Train
Ancillary services may also be covered. Ancillary services include:
- Escort transportation
- Lodging
- Meals
- Escort's lodging
- Escort's meals
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
8.280.4.E Other EPSDT Benefits
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
Members and/or providers may request coverage for transportation services that are not currently covered or exceed stated limitations if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All services must be medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, and 8.280.4.E. regardless of whether such services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one or more Activities of Daily Living; and meets the criteria set forth at Section 8.076.1.8.b - g.
- The service is not primarily for the convenience of the child, caretaker, or provider.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly of all alternatives while still being the most appropriate option for the child’s physical and emotional condition.
Visit the Transdev Health Solutions Book A Ride web page to make a request.
Visit the Non-Emergent Medical Transportation web page and complete the Out-of-State Non-Emergent Medical Transportation Request Form for out-of-state NEMT EPSDT requests.
All transportation services provided to children under 21 years of age and their guardians or caregivers are provided with no cost sharing or co-pay, which includes approved non-covered services under this section.
Transportation for the Direct Benefit of Children Under 21
Policy Statement
Pursuant to EPSDT mandates, Non-Emergency Medical Transportation (NEMT) is covered under medically necessary circumstances for the transportation of a child’s (age 0–20) parent, family member, or caregiver if the child member is not present for the transportation. This coverage is provided to ensure that the child receives timely access to medically necessary services.
Conditions for Coverage
If the participation of a parent, family member, or other caregiver is necessary to a child's care and such caregiver cannot access the child to participate in the care, then NEMT may be covered for the transportation of the parent, family member, or other caregiver. Examples of situations where this applies include, but are not limited to:
- A child receiving inpatient care, such as in a Neonatal Intensive Care Unit (NICU).
- A child in a Psychiatric Residential Treatment Facility (PRTF).
- A child requiring the presence of a caregiver for breast milk provision, breastfeeding, family therapy, medical decision-making, or consent for surgery.
Billing Instructions
- The Health First Colorado ID of the person being transported should always be used for billing. However, if the person being transported is not enrolled in Health First Colorado or does not have an active Health First Colorado ID, the Health First Colorado ID of the child for whom the transportation is of direct benefit should be used for billing. This ensures that the transportation is correctly attributed to the child’s medically necessary care.
- Documentation must substantiate the medical necessity of such transportation. The signature and date of the member’s treating provider who is ordering the participation of the parent, family member or caregiver must be included.
Child or At-Risk Adult Accompaniment
- Children and/or siblings of a member or the child or children of the member’s escort may use NEMT in the following circumstances:
- The child or children may accompany the member if the member does not have the following for the duration of the trip to and from the medical services:
- Access to childcare for their child or children
- Access to care for an At-Risk Adult for whom the member is responsible
- If a member’s escort does not have access to childcare for the member’s siblings for the duration of the trip to and from the member’s medical services, the member’s siblings may accompany the member.
- The escort’s children or At-Risk Adult, or both, may accompany the member and the escort if the member's escort does not have the following for the duration of the trip to and from the member’s medically necessary services:
- Access to childcare for their children
- Access to care for an At-Risk Adult for whom the escort is responsible
- The child or children may accompany the member if the member does not have the following for the duration of the trip to and from the medical services:
- The names of the additional passengers must be included in the trip log report.
At-Risk Adult means an individual eighteen (18) years of age or older:
- Who is susceptible to mistreatment because they are unable to perform or obtain services necessary for their health, safety and welfare; or,
- Who lacks sufficient understanding or capacity to make or communicate responsible decisions concerning their person or affairs.
- Persons are not considered “At-Risk” solely because of age and/or disability.
Trips to Pharmacies
Rides to enrolled pharmacies are a covered benefit for medically necessary covered services. This includes but is not limited to the following types of services:
- Vaccines
- Immunizations
- Preventive services
- Prescription pickups (if mail order is not available)
- Durable Medical Equipment (DME)
Types of Non-Emergent Medical Transportation
Public/Mass Transportation
Public/mass transportation, including fixed route, light rail, paratransit, and private bus transportation, may be available when these modes of transportation are the least costly and most appropriate to the member's condition. Transit passes may be issued when the cumulative cost of bus trips exceeds the cost of a pass.
Personal Vehicle Mileage Reimbursement
A private vehicle may be provided by a volunteer, (individual or organization, with no member vested interest) or a vehicle provided by an individual, (family member, self, neighbor), with a member vested interest.
Mileage reimbursement for a personal vehicle is reimbursed per vehicle, without regard to the number of members or escorts in the vehicle and is only reimbursed using the most direct route to and from the appointment. Exceptions can be made by the SDE if the shortest distance is impassable due to severe weather, road closure, or other unforeseen circumstances outside of the member's control that severely limit using the shortest route. If an exception is made, the SDE must document the reason and can pay mileage for the actual route traveled.
All mileage reimbursement requests must be approved by the SDE prior to the trip taking place. The SDE will assign a trip number, which is required for reimbursement of both mileage and any associated ancillary services, if applicable.
Failure to obtain prior approval may result in denial of reimbursement. For detailed information on eligible ancillary services, please refer to the Ancillary Services section of this NEMT Billing Manual.
NEMT providers may not transport their own family or household members under standard NEMT billing. If the individual is an eligible Medicaid member, the provider must use the personal mileage reimbursement process. Mileage reimbursement information and the trip mileage form can be found on the Transdev member resources web page.
Non-Emergent Medical Transportation (NEMT) must be provided to transport the member to the closest available provider qualified to provide the treatment service the member needs. The closest provider is defined as a provider within a 25-mile radius of the member’s residence or the nearest provider if one is not practicing within a 25-mile radius of the member’s residence.
Exceptions are allowed based on the following:
- The closest provider is not willing to accept the member.
- The member has complex medical conditions that restrict the closest medical provider from accepting the member.
- The member may use NEMT to their established treatment provider seen in their previous locale if they have moved with the three (3) months preceding an NEMT transport.
- Note: The member and treatment provider must transfer care to the closest provider as defined in Section 8.014.4.B or determine transportation options other than NEMT during the three (3) months.
Any NEMT claim billed for procedure codes A0425, S0215 or S0209 will be suspended for review if the billed units of service exceed 52 or 125 (for designated rural counties). Suspended claims will be denied if they do not have an attachment which meets the requirements as specified below. Reviewed claims will be denied if the attachment is not sufficient pursuant to these specifications.
Effective September 30, 2025, a revision of the current 52-mile edit will go into effect for rural communities. The new edit increases the daily mileage limit to 125 miles (roundtrip) for members residing in designated rural counties.
- Eligibility for the expanded mileage limit will be based on the member's county of residence. A list of qualifying rural counties, determined by the Department using geographic criteria, will be posted on the Department’s NEMT Web page. No new forms or additional documentation will be required; existing trip logs and standard reporting processes remain in effect.
- The designated rural counties are: Alamosa, Archuleta, Bent, Chaffee, Cheyenne, Clear Creek, Conejos, Costilla, Crowley, Custer, Delta, Dolores, Fremont, Gilpin, Grand, Gunnison, Hinsdale, Huerfano, Jackson, Kiowa, Lake, Lincoln, Logan, Mineral, Moffat, Montrose, Morgan, Otero, Ouray, Park, Phillips, Pitkin, Rio Blanco, Rio Grande, Routt, Saguache, San Juan, San Miguel, Sedwick and Washington.
Claims must have a document attached which contains the following information about the trip which is being billed:
- The pick-up address
- The destination address
- Date and time of the trip
- Member’s name and identifier
- Confirmation the driver verified the member’s identity
- Confirmation by the member, escort or medical facility that the trip occurred
- The actual pick-up and drop-off times
- The driver’s name
- Identification of the vehicle in which the trip was provided
- A rationale and certification from the member’s treating provider as to why the member cannot be treated by the closest provider within 25 miles of the member’s residence
Effective May 1, 2024, the member’s referring or treating provider must complete the Verification Form for Transportation Services More Than 25 Miles, located on the Provider Forms web page under the Claim Forms and Attachments drop-down, to verify the medical necessity of trip requests that exceed 25 miles, one way. The member’s treatment provider may designate other appropriate employees, such as clinical or administrative staff, as being able to sign this form as verification.
- It is the NEMT driver or provider’s responsibility to get this form signed by the member’s provider. Drivers cannot require members to obtain the signatures for this form.
- The form can be completed and signed by either the member’s treating provider or the member’s referring provider.
- The provider signature is not required prior to the NEMT trip happening.
- The form will be valid for 90 days for recurring medical appointments (dialysis, cancer treatments, etc).
- The form should be submitted when the claim(s) are submitted through the Provider Web Portal for each trip.
Refer to program rules 10 C.C.R. 2505-10 8.000, 8.130.2 and 8.014.3.C for further details on NEMT and provider record maintenance. Each provider shall maintain legible, complete and accurate records necessary to establish that conditions of payment for Medical Assistance Program-covered goods and services have been met and to fully disclose the basis for the type, frequency, extent, duration and delivery of goods and/or services provided to Medical Assistance Program members, including but not limited to the following:
- Billings
- Prior Authorization Requests (PARs)
- All medical records, service reports and orders prescribing treatment plans
- Records of goods prescribed, ordered for or furnished to members as well as unaltered copies of original invoices for such items
- Records of all payments received from the Medical Assistance Program
- Records required elsewhere in Section 8.000et seq. The records shall be created at the time the goods or services are provided.
Mobility/Ambulatory Vehicles
Mobility/Ambulatory vehicle services are transportation services provided to individuals who are not wheelchair confined. A mobility/ambulatory vehicle is a passenger-carrying vehicle for hire, including those designed, constructed, modified or equipped to meet the needs of passengers with medical, physical or mobility impairments and, when medically necessary, their certified escorts. Mobility/ambulatory vehicle providers must have, and maintain one of the following:
- Contract Carrier permit
- Luxury Limousine
Providers must provide services in compliance with seven (7) state and federal laws.
Taxi service is not a mobility vehicle; however, a taxi company may also have an MCT permit or luxury limousine authority from the PUC and may operate its vehicles under that authority as mobility/ambulatory vehicles.
In this case, the taxi company agrees to the Health First Colorado reimbursement for mobility /ambulatory vehicles. A mobility vehicle may submit claims using wheelchair van procedure codes only when the member is a wheelchair user and the vehicle has been modified with appropriate wheelchair equipment. If these requirements are not met, the mobility/ambulatory vehicle may not bill using wheelchair van codes. Refer to the Wheelchair Van section.
Mobility/ambulatory vehicle transportation is a Health First Colorado benefit when the member's medical or physical condition precludes the use of member-purchased public or private transportation, or other less costly modes of Health First Colorado transportation. The SDE is responsible for ensuring documentation from the member's medical professional indicates, in writing, the member is unable to use less costly modes of NEMT services (e.g., mileage reimbursement, bus tickets).
Mileage shall be paid for the shortest trip length in miles as determined by an internet-based map, trip planner, or other Global Positioning System (GPS).
Effective July 1, 2025 the following coding policies are in effect:
- HCPCS S0215 must be used for billing ambulatory/mobility vehicle mileage. A0425 is no longer used for billing this mileage.
- HCPCS A0425 is no longer used for non-ambulance trip mileage for trips with a date of service on and after July 1, 2025.
- Note: For ambulatory/mobility vehicle trips with a date of service on/before June 30, 2025, HCPCS A0425 was used for billing trip mileage.
Wheelchair Van
A wheelchair van is a vehicle for hire that has been specifically designed, constructed, modified, or equipped to accommodate the needs of wheelchair users. Wheelchair van services are a Health First Colorado benefit only when the member's medical professional indicates, in writing, the member is wheelchair-confined and unable to use less costly modes of NEMT services (e.g., mileage reimbursement, bus tickets).
Wheelchair van providers must have, and maintain the following:
- Common Carrier permit
Providers must provide services in compliance with state and federal laws.
When operating as a wheelchair van, the provider agrees to wheelchair van reimbursement.
Wheelchair vans must bill using mobility/ambulatory vehicle procedure codes if the member's medical professional has not indicated in writing that the member is wheelchair confined. In this case, the mobility /ambulatory vehicle must also meet PUC requirements for mobility vehicle services and agrees to the Health First Colorado reimbursement for mobility/ambulatory vehicles. Refer to the Mobility/Ambulatory Vehicle section.
Effective 11-1-2025, XL Wheelchair services are covered if two attendants are used for assisting the member with loading and unloading. Bill A0130+U9 for the service of XL Wheelchair transportation using two attendants. Wheelchair Van transportation services only using one attendant are billed using A0130 with no modifier.
Mileage shall be paid for the shortest trip length in miles as determined by an internet-based map, trip planner, or other Global Positioning System (GPS).
HCPCS S0209 is to be used only for wheelchair van trip mileage.
Taxicab
A taxicab service means passenger transportation by a common carrier on a call-and-demand basis in a taxicab, with the first passenger therein having exclusive use of the taxicab unless such passenger agrees to multiple loading. Taxicab providers must have and maintain a common carrier certificate with authority to provide taxicab service. Providers must provide services in compliance with PUC licensure and/or state and federal laws.
Taxicab services are a Health First Colorado benefit when the member's medical or physical condition precludes the use of member-purchased public or private transportation, or other less costly modes of Health First Colorado transportation. The SDE is responsible for ensuring documentation from the member's medical professional indicates, in writing, the member is unable to use less costly modes of NEMT services (e.g., mileage reimbursement, bus tickets). Mileage shall be paid for the shortest trip length in miles as determined by an internet-based map, trip planner, or other Global Positioning System (GPS).
Taxicab service is not a mobility vehicle; however, a taxi company may also have an MCT permit or luxury limousine authority from the PUC and may operate its vehicles under that authority as mobility / ambulatory vehicles. In this case, the taxi company agrees to the Health First Colorado reimbursement for mobility /ambulatory vehicles. Refer to the Mobility/Ambulatory Vehicle section.
Effective July 1, 2025 the following coding policies are in effect:
- HCPCS S0215 must be used for billing taxicab vehicle mileage. A0425 is no longer used for billing this mileage.
- HCPCS A0425 is no longer used for taxicab trip mileage for trips with a date of service on and after July 1, 2025.
- Note: for taxicab trips with a date of service on/before June 30, 2025, HCPCS A0425 was used for billing trip mileage.
- Note: for taxicab trips with a date of service on/before June 30, 2025, HCPCS A0425 was used for billing trip mileage.
Stretcher Van
Stretcher van is a vehicle that can legally transport a client in a prone or supine position when the client does not require medical attention en route. This may be by stretcher, board, gurney or other appropriate device. Medical or safety requirements must be the basis for transporting a client in the prone or supine position.
Stretcher van service is a Health First Colorado benefit when the member's medical professional indicates, in writing, the member must be transported in a prone or supine position and they are unable to use less costly modes of NEMT services (e.g., mileage reimbursement, bus tickets).
Mileage shall be paid for the shortest trip length in miles as determined by an internet-based map, trip planner, or other Global Positioning System (GPS).
Ground Ambulance
Ambulance means any publicly or privately-owned vehicle that is specially designed, constructed, modified or equipped to be used, maintained and operated on streets or highways to transport clients to a hospital or other treatment facility in cases of accident, trauma or severe illness. Transport of clients requiring cardiac/hemodynamic monitoring is considered to be non-emergency only if such monitoring is required both before and after transport. Advanced airway management shall include clients who are ventilator dependent, require intubation and/or deep suctioning en route, or are on an apnea monitor before, during and after transport. Administration of intravenous (IV) medication en route shall not include self-administered IV medications.
Non-emergent ground ambulance service is a Health First Colorado service when the member's medical professional indicates that the member requires an ambulance in order to be transported safely and they are unable to use less costly modes of NEMT services (e.g., mileage reimbursement, bus tickets). All out-of-state ground ambulance trips must be prior approved by the Department. Refer to the Prior Authorization section.
Effective July 1, 2025, Healthcare Common Procedural Coding System (HCPCS) A0425 is to be used only for ambulance trip mileage. It is no longer used for non-ambulance trip mileage.
Effective November 1, 2025, HCPCS A0434 is no longer used in the NEMT benefit.
Procedure Codes: A0428, A0426, A0433, A0425, A0021, A0422
Air Ambulance
Air ambulance means a fixed wing or rotor wing aircraft that is equipped to provide air transportation and is specifically designed to accommodate the medical needs of individuals who are ill, injured, or otherwise mentally or physically incapacitated and who require in-flight medical supervision.
Non-emergent air ambulance benefits are provided when:
- Non-emergent, pre-planned services are authorized by the State authorizing agency.
- Great distances or other obstacles prohibit transporting the member by land to the nearest appropriate facility and the member's condition requires immediate attention.
- The member is suffering from an illness or injury making other forms of transportation inadvisable.
Non-emergent air ambulance service is a Health First Colorado service when the member's medical professional indicates, in writing, that the member requires air ambulance in order to be transported safely and they are unable to use less costly modes of NEMT services. All NEMT air ambulance trips must be prior approved by the Department. Refer to the Prior Authorization section.
Commercial Air
Commercial air means travel via an airline which provides scheduled air transportation for passengers.
Commercial air transport is a Health First Colorado service when the member's medical professional indicates that the member requires commercial air in order to be transported safely and they are unable to use less costly modes of NEMT services. All NEMT commercial air trips must be prior approved by the Department. Refer to the Prior Authorization section.
Train
Train means passenger-carrying railroad cars.
Train transport is a Health First Colorado service when the member's medical professional indicates that the member requires train transportation in order to be transported safely and they are unable to use less costly modes of NEMT services. All NEMT train trips must be prior approved by the Department. Refer to the Prior Authorization section.
Standard Forms Required
Effective October 1, 2024, all NEMT providers must begin using the Department provided Standard Trip Log for all rides provided. Please submit forms along with your claims. NEMT providers must keep the completed trip report(s) on file. The Department may request copies of any and all trip reports for the provider's claims at any time. Visit the Provider Forms web page to locate the Standard Trip Log, 25+ Mile Verification Form and Consent and Liability Release for Minors Form. These forms are fillable online, if needed. No other trip logs will be accepted after October 1, 2024.
Providers may bill only the procedure code that corresponds to the vehicle type actually used and the level of service necessary to transport the member to the destination.
Ancillary Services
Escort
An escort may accompany a member when:
- The member is a child or an at-risk adult and is unable to make personal/medical determinations or provide necessary self-care as certified in writing by the member's attending Health First Colorado-enrolled provider.
- The escort or attendant must be physically and cognitively capable of providing the needed services for the member.
NEMT may cover the cost of transporting a second escort with written certification for medical necessity from the member's medical provider, if:
- The member has a behavioral or medical condition which may cause the member to be a threat to self or others if only one escort is provided, or
- The member's primary caretaker has a disability that precludes the caregiver from providing all of the member's needs during transport or extended stay.
Minors who are at least thirteen (13) years old, but younger than eighteen (18) years old, may travel alone with a written release from their parent or guardian, as long as an adult is present to receive the minor at the destination and at the return location. Minors under thirteen (13) years old shall not travel without an escort.
Children in a day treatment program may travel without an escort, as long as there is a written release from their parent or guardian, stating that an adult will be present to receive the minor at the destination and return location. Children are not eligible for NEMT travel to and from school-funded day treatment programs, unless itis for specialized transportation to school-based services when medically necessary and specified in the child's Individual Education Plan (IEP). This includes transportation to and from school or other educational settings to receive Health First Colorado-covered services as outlined in the IEP.
Meals/Lodging
Meals and lodging for members are available for:
- In-state treatment when travel cannot be completed in one calendar day
- Authorized out-of-state treatment if meals or lodging is not included as part of an inpatient stay.
Meals and lodging may be covered for the escort when a member is a child or an at-risk adult who requires the escort's continued stay.
Reimbursement will only be made for meals and lodging that members and escorts are actually charged for, up to the daily per diem rate established by the Department. If a member is not normally billed for meals and lodging will not be reimbursed.
Meals and lodging are limited to one unit per day each, per member or escort.
Important: A minor child’s parent, guardian or custodian may use the child’s Medicaid ID number for ancillary services (meals and lodging) if the parent, guardian or custodian is traveling with the child as an escort for overnight or out of state medical treatment.
Procedure Codes: A0180, A0190, A0200, A0210
Urgent NEMT
Effective January 1, 2019, eligible transportation providers can provide urgent Non-Emergent Medical Transportation (NEMT) trips scheduled directly by Medical Facilities. This is a change to current processes where facilities and transportation vendors work with the State Designated Entity.
Urgent NEMT is transportation needed to receive necessary medical services when a member is unable to provide advanced notice. This includes:
- Transportation after discharge from a hospital
- Failure of a NEMT provider to pick up a member from an appointment within one hour of the scheduled pick up time.
- Transportation to and from critical, unplanned medical appointments.
Transportation will still only be provided to and from services that are covered under Health First Colorado and meet the requirements for NEMT services. Non-urgent NEMT will continue to follow the same process required by the NEMT State Designated Entity.
Exclusions
The following services are not Health First Colorado NEMT benefits:
- Services provided only as a convenience to the member as opposed to medical necessity.
- Charges incurred while the member is not in the vehicle, except for lodging and meals.
- Transportation to/from non-covered medical services, including services that do not qualify due to coverage limitations.
- Waiting time.
- Cancellations.
- Transportation which is covered by another entity (e.g., transportation provided by the Veterans Administration or a school).
- Metered taxi services.
- Charges for additional passengers except when acting as an escort for a child or at-risk adult.
- Response calls when, upon arrival at the site of the call, no transportation is needed or provided.
- Transportation for nursing facility or group home residents to medical or rehabilitative services required in the facility's program, unless the facility does not have an available vehicle. Nursing facilities and group homes should instead report transportation as part of their allowable costs on their state-approved cost report.
When transporting more than one member in the same vehicle to the same location, only one Health First Colorado ID may be used for billing. The Department will not reimburse multiple claims for the same vehicle’s trip mileage.
Resources
Code of Federal Regulations (CFR)
Title 42 CFR, § 431.53 requires states to:
- Ensure transportation for members to and from providers, and
- Specify in the Medicaid State Plan, which must be approved by the Centers for Medicare & Medicaid Services (CMS), the methods the state will use to ensure transportation.
Visit the Electronic Code of Federal Regulations website for more information.
Colorado's Medicaid State Plan
Colorado's Medicaid State Plan is the contract with CMS outlining how Colorado will run the Medicaid program. Attachment 3.1.-D, Methods of Assuring Transportation covers NEMT and specifies the methods used to ensure transportation for members, as required by 42 CFR, § 431.53. Visit the Colorado Medicaid State Plan web page for more information.
Colorado Code of Regulations (CCR)
The Colorado Code of Regulations are the state's rules governing programs and services. 10 CCR 2505-10.8.014 covers NEMT.
Visit the Code of Colorado Regulations web page to find the current version of 10 CCR 2050-10 8.000 (which includes 8.014).
Rate and Fee Schedule
The Provider Rate and Fee Schedule outlines the current NEMT rates and available procedure codes. The Rate and Fee Schedule is updated annually around July 1 with the new rates implemented by the legislature for the new State Fiscal Year.
Refer to the Transportation Rate Schedule located on the Provider Rates and Fee Schedules web page.
NEMT Web Page
Visit the NEMT web page for a brief overview of NEMT and resources.
Find a Doctor Tool
NEMT must be used to access the closest qualified provider of that service. Refer to the Find a Doctor tool to find the closest provider.
Provider Contacts
Provider contacts are located on the Provider Contacts web page.
Procedure Coding
Health First Colorado uses the Centers for Medicare & Medicaid Services (CMS) Healthcare Common Procedural Coding System (HCPCS). The codes are used for submitting claims for services provided to Health First Colorado members and represent services that may be provided by enrolled, certified Health First Colorado providers.
HCPCS are used to identify and reimburse non-emergent medical transportation services.
The Department updates and revises HCPCS codes through Health First Colorado billing manuals.
The series of local procedure codes used to bill for mobility van services (X6022-X6030) are no longer available. Providers should use HCPCS A0120 plus modifier TK (Extra member or passenger) to bill for mobility van services. Use the appropriate number of units to identify the actual number of riders.
Multiple Trips in the Same Day
When billing for one member taking multiple trips in the same day with the same rendering provider, modifier 76 must be used.
When billing for one member taking multiple trips in the same day with different rendering providers, modifier 77 must be used.
Public/Mass Transportation
| Procedure Code | Mod-1 | Mod-2 | Mod-3 | Unit | Description |
|---|---|---|---|---|---|
| A0110 | TN | Ticket, One-Way | Fixed Route, One-Way, Local | ||
| A0110 | SC | SE | TN | Ticket, One-Way | Fixed Route, One-Way, Regional |
| A0110 | SE | Ticket, One-Way | Paratransit, One-Way | ||
| A0110 | Ticket, One-Way | Public/Mass Transportation, Bus Service |
Personal Vehicle Mileage Reimbursement
| Code | Unit | Description |
|---|---|---|
| A0080 | Mile | Volunteer Vehicle Mileage - vehicle provided by volunteer (individual or organization), with no vested interest |
| A0090 | Mile | Individual Vehicle Mileage - vehicle provided by individual (family member, self, neighbor) with vested interest |
Mobility / Ambulatory Vehicles
| Code | Unit | Description | NOTES |
|---|---|---|---|
| A0120 | One Way Trip | Mobility / Ambulatory Vehicles | |
| A0425 | Mile | Ground mileage, per statute mile | Only used for billing trips with a date of service on/before June 30, 2025 |
| S0215 | Mile | Ground mileage, per statute mile | Only used for billing trips with a date of service on/after July 1, 2025 |
Wheelchair Van
| Code | Unit | Description |
|---|---|---|
| A0130 | One Way Trip | Wheelchair Van |
| S0209 | Mile | Wheelchair Van Mileage |
Taxicab
| Code | Unit | Description | NOTES |
|---|---|---|---|
| A0100 | One Way Trip | Taxi | Only used for billing each leg of the trip. 1 unit of service = 1 leg of the trip. For example, a round trip to a destination and back would have 2 units of service billed. |
| A0425 | Mile | Ground mileage, per statute mile | Only used for billing trips with a date of service between July 1, 2024 and June 30, 2025 |
| S0215 | Mile | Ground mileage, per statute mile | Only used for billing trips with a date of service on/after July 1, 2025 |
Stretcher Van
| Code | Unit | Description |
|---|---|---|
| T2005 | One Way Trip | Stretcher van |
| T2049 | Mile | Stretcher Van Mileage |
Ground Ambulance
| Code | Unit | Description |
|---|---|---|
| A0428 | One Way Trip | Nonemergency transportation: Ambulance service- Basic Life Support (BLS) |
| A0426 | One Way Trip | Nonemergency transportation: Ambulance service- Advanced Life Support (ALS), level 1 |
| A0433 | One Way Trip | Ambulance service- Advanced Life Support (ALS), level 2 |
| A0434 | One Way Trip | Specialty care transport (SCT). Discontinued from NEMT benefit effective 11-1-2025. |
| A0425 | Mile | Ground mileage, per statute mile |
| A0021 | Mile | Ambulance service, outside state per mile, transport |
| A0422 | Per Unit | Ambulance (ALS or BLS) oxygen and oxygen supplies, life sustaining situation |
Air Ambulance
| Code | Unit | Description |
|---|---|---|
| A0430 | One Way Trip | Ambulance service, conventional air services, transport, one way (fixed wing) |
| A0431 | One Way Trip | Ambulance service, conventional air services, transport, one way (rotary wing) |
Commercial Air and Train
| Code | Unit | Description |
|---|---|---|
| A0140 | Per Trip | Train and/or Air |
Ancillary Services
| Code | Unit | Unit Limit | Description |
|---|---|---|---|
| T2001 | One Way Trip | N/A | Escort Transportation |
| A0180 | Per Diem | 1 per day | Travel Lodging for Member |
| A0190 | Per Diem | 1 per day | Travel Meals for Member |
| A0200 | Per Diem | 1 per day, per escort | Travel Lodging for Escort |
| A0210 | Per Diem | 1 per day, per escort | Travel Meals for Escort |
NEMT Billing Information
The 837 Professional (837P) transaction should be utilized for electronic billing.
Claim Type
NEMT Claims submitted via the Provider Web Portal are Professional Claims.
Diagnosis Codes
A diagnosis is required on all claims. Enter code R68.89 for all claims. Do not fill unused spaces with zeroes. The diagnosis must be referenced to each detail line by placing a "1" in the diagnosis indicator field.
Dates of Services
Each detail line includes space to enter two (2) dates of service: a 'From' Date Of Service (FDOS) and a 'To' Date Of Service (TDOS). Both dates must be completed on the electronic record. For services rendered on a single date, complete the FDOS and the TDOS with the same date.
Span Billing
Span billing is not allowed for transportation services.
Place of Service Codes
Use CMS place of service codes. Use place of service codes:
- 41-land transportation
- 42-air transportation
Procedure Codes
Each detail line must include a valid NEMT procedure code.
Providers may bill only the procedure code that corresponds to the vehicle type actually used and the level of service necessary to transport the member to the destination.
EMG (Emergency) Indicator
The Emergency Indicator is used to differentiate some NEMT services from Emergency Medical Transportation. Enter N or leave blank to indicate the service was non-emergency medical transportation.
Transportation Certification
Transportation Certification is optional for NEMT claims.
Attachments
Attachments may be included with electronic claims submitted via the Provider Web Portal. NEMT claims which require manual pricing must include an attachment that supports the claim.
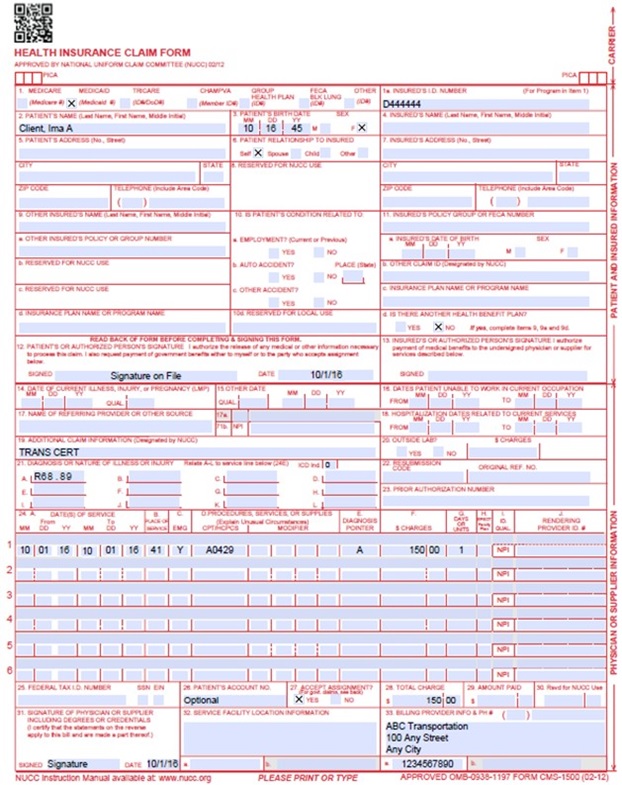
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the EPSDT claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two digits for the month, two digits for the date, and two digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. | ||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | |||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two digits for the month, two digits for the date and two digits for the year. Example: 070114 for July 1, 2014. Place an X" in the appropriate box to indicate the sex of the insured. | ||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||
| 17b. NPI of Referring Physician | Conditional | |||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||
| 19. Additional Claim Information | Conditional | When applicable, enter the words "TRANSPORT CERT" to certify that you have a transportation certificate or trip sheet on file for this service. | ||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one but no more than twelve diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. NEMT Enter diagnosis code R68.89. | ||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six lines of information on the paper claim. If more than six lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two dates: a "From" date of services and a "To" date of service. Enter the date of service using two digits for the month, two digits for the date and two digits for the year. Example: 010116 for January 1, 2016.
Single Date of Service Enter the six-digit date of service in the "From" field. | ||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||
| 24C. EMG | Conditional | Enter an "N" or leave blank for NO in the bottom, unshaded area of the field to indicate the service was non-emergent medical transportation. | ||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||
| 24D. Modifier | Not Required | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four modifiers may be entered when using the paper claim form. NEMT Only A0110 may require a modifier. Refer to Transportation HCPCS codes. | ||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of 4 characters in the unshaded area. | ||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Submitted charges cannot be more than charges made to non-Health First Colorado-covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||
| 24G. Days or Units | Required | Enter the number of units provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||
| 24H. EPSDT/Family Plan | Not Required | |||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI or Provider ID of the Health First Colorado provider who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two digits for the month, two digits for the date and two digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | ||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||
| 33a- NPI Number | Required | |||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | |||||||||||||
CMS 1500 Transportation Claim Example
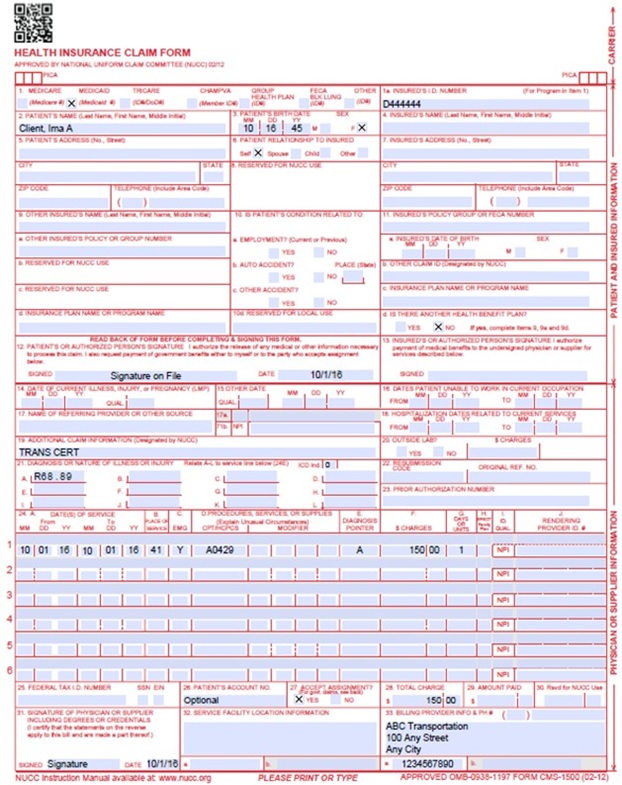
Transportation Third Party Claim - No Mileage Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the Appendices drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
NEMT Billing Manual Revisions Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE |
| 12/12/2017 | Manual revised to separate NEMT and EMT services. Changed the name to NEMT Billing Manual. Updates made throughout to align with current policies and billing rules. | HCPF |
| 4/12/2018 | Corrected Wheelchair Van procedure code | HCPF |
| 6/22/2018 | Updated billing and timely to point to General Billing manual | HCPF |
| 6/28/2018 | Edited link, edited timely | HCPF |
| 11/15/2018 | Clarified interfacility transfers, 9-1-1 response calls, and unit limits for ancillary services. Removed crossover claim example. Added Urgent Transportation. | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 7/11/2019 | Updated Appendices links and verbiage | DXC |
| 11/20/2019 | Changed specific term to "transportation vendor" | DXC |
| 12/9/2019 | Updated SDE entry to IntelliRide, added link for provider contacts | HCPF |
| 12/19/2019 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 12/17/2020 | Updated SDE entry to reflect IntelliRide as the statewide broker | HCPF |
| 12/29/2020 | Added information on modifiers for billing multiple daily trips per member | HCPF |
| 6/30/2021 | Added information on SDE service and provider billing | HCPF |
| 7/22/2021 | Added verbiage for multiple trips by member in single day | HCPF |
| 8/18/2021 | Removed references to now-defunct web page | HCPF |
| 8/14/2023 | Removed references to PUC and MCT permits where necessary as it is no longer a requirement pursuant to HB21-1206 | HCPF |
| 2/21/2024 | Added billing rules and information for 25 mile or longer NEMT rides | HCPF |
| 6/17/2024 | Added clarification around EPSDT policies and references, credentialing, return trips without the member present, trips relating to school services, clarification around billing for multi-loaded vehicles, 25-mile verification form link | HCPF |
| 7/1/2024 | Updated EPSDT language. Clarified that 25-mile verification form can be signed by the member’s referring provider. | HCPF |
| 9/9/2024 | Added Trips to Pharmacies info. Added Standard Forms (Trip Log). Updated 25-mile form provider info for completing the form. Added Child Accompaniment language. Clarified pharmacy trip coverage. | HCPF |
| 01/31/25 | Added Provider Responsibilities for NEMT providers outside the broker service area including checking eligibility and claim submission information, in accordance with previously published memo HCPF OM-074. | HCPF |
| 04/10/25 | Added important reminder to Ancillary Services for traveling with minor children. | HCPF |
| 05/27/25 | Added NEMT provider eligibility and verification responsibilities that reference Operational Memo 25-028. Added HCPCS coding changes for mobility/ambulatory vehicles and taxicab for A0425, S0215 and S0209 effective July 1, 2025 | HCPF |
| 08/13/2025 | Added rural mileage edit info effective 9/30/25. Added NEMT providers may not bill NEMT they must use mileage reimbursement. Added information about the member personal vehicle mileage reimbursement policy. | HCPF |
| 10/15/2025 | Member Eligibility section, clarified that “EMS - Emergency Medicaid and Reproductive Health Program” benefit plan coverage is not eligible for NEMT. | HCPF |
| 11/3/2025 | Added XL Wheelchair billing info with modifier effective 11-1-2025. Discontinued use of HCPCS A0434 for NEMT benefit effective 11-1-25. | HCPF |
| 11/12/2025 | Corrected modifier for XL wheelchair from U1 to U9 | HCPF |
| 01/09/2026 | Added claims info for actual mode of transport and level of medical need for billing claims | HCPF |