Winter 2026
Navigating Budget Realities, County Modernization, and Rural Health Transformation Program
The Department of Health Care Policy and Financing (HCPF) invites you to review the materials we covered during HCPF’s Joint Budget Committee (JBC) budget hearings on January 5 and 20, our SMART Act hearing on January 28 and fiscal year (FY) 2026–27 budget, including the supplemental request/budget amendments. With the submission of HCPF’s FY 2026-27 Budget Amendment 07, HCPF proposes several reductions for an additional $118 million General Fund savings in FY 2026-27 to achieve the state’s budget balancing targets.
The Governor’s proposed FY 2026–27 budget reflects the most fiscally constrained environment Colorado has faced in many years. State revenues continue to be challenged by the Taxpayer’s Bill of Rights (TABOR) limits, the end of federal stimulus funds, Medicaid escalated trends, and the ongoing impacts of H.R. 1, which reduces federal funding while creating new administrative requirements. As the fiscal year progresses, the budget process and the Medicaid Sustainability Framework will be important tools to better align appropriations with updated Medicaid and CHP+ enrollment projections, utilization, and cost trends. You are welcome to visit our Legislator Resource Center for more information.
As H.R. 1 increases administrative requirements on the eligibility process, four concurrent pathways are underway: CBMS ecosystem modernizations, business process standardizations, “Shared Services,” and regionalizing county administration into larger “Districts.” Shared Services would begin the process of centralizing select administrative functions into one county, optimizing best practices and performance. Regionalizing into Districts means that instead of 64 counties operating their own eligibility department, groups of counties will form Districts to pool resources and staff under performance-based contracts with the state. More information is available on our Proposed County Changes Resource Center page.
HCPF continues to prepare for implementation of the Rural Health Transformation Program (RHTP), authorized under H.R. 1. Colorado’s application builds on strong partnerships with rural providers, communities, and stakeholders and aligns with recent federal and state investments in rural health. In December, HCPF received notice from CMS that Colorado will receive just over $200 million for the first period of the grant, December 2025 through September 2027, for its RHTP to transform health care in Colorado’s rural and frontier counties. Across the entire grant period ending in federal fiscal year 2030, federal funding should total more than $1 billion to Colorado. Applications for the advisory committee are due February 16; an overview of the committee is here. For more information, please visit our RHTP website and press release.
We also invite you to review HCPF’s annual report to the community for the previous fiscal year, July 2024 through June 2025.
Finally, please save the date for our upcoming H.R. 1 Medicaid Coverage, Eligibility, & Implementation Updates Webinar on February 24 from 9 to 11 a.m. This event will share Medicaid related updates on the most recent CMS guidance, the implementation timeline of H.R. 1 for key changes such as semi-annual renewals and community engagement/work requirements, and opportunities for stakeholders to engage with us in the process. The webinar will also address the top concerns we heard from more than 700 respondents to our H.R. 1 survey. Please register here.
Thank you for your continued partnership and thoughtful engagement as we navigate state budget challenges and the complex federal landscape before us.
- November 2025
Colorado’s 5.9% Uninsured Rate, HCPF’s $20.66 Billion Fiscal Year 2026-27 Budget, Rural Health Transformation Program $100+ Million Opportunity
Colorado’s Uninsured Rate. The Department of Health Care Policy and Financing (HCPF) is pleased that the 2025 Colorado Health Access Survey (CHAS) shows that the state’s uninsured rate is 5.9%, even lower than prepandemic levels of about 6.5%. The recently released CHAS shows that since the end of the Public Health Emergency, the percentage of the total population enrolled in Medicaid decreased as expected, while the percentages of people covered by their employers and the individual marketplace increased.
This 5.9% result is the product of extraordinary collaboration in a united effort to get Coloradans disenrolling from Medicaid connected to other coverages to achieve our shared goal of Keeping Coloradans Covered through the end of the public health emergency. We celebrate this outstanding achievement with gratitude and appreciation to all who engaged - care providers, consumer advocates, insurance carriers, county and other eligibility partners, Connect for Health Colorado, vendor partners, sister agencies, and so many more.
HCPF’s Proposed Fiscal Year 2026-2027 Budget. On October 31, the Governor released his budget for fiscal year (FY) 2026-27. It reflects the most fiscally constrained environment Colorado has faced in recent memory. State revenues continue to be challenged by the Taxpayer’s Bill of Rights (TABOR) limits, the end of federal stimulus funds, and the ongoing impacts of H.R. 1, which reduces federal matching funds for Medicaid and creates new administrative requirements.
HCPF represents about one-third of the state’s General Fund. We are grateful for our allocation in the Governor’s FY 2026–27 proposed budget of $20.6 billion total funds, including $5.99 billion General Fund for Health First Colorado (Colorado’s Medicaid program) and Child Health Plan Plus (CHP+). HCPF’s proposed annual budget represents an increase of $2.3 billion in total funds, $413 million increase in General Fund and 32% of available state General Fund. Approximately 96% of this funding goes directly to providers who deliver care to our members. The budget also includes reductions of $537 million in total funds, including $217 million General Fund. That means the FY 2026-27 budget of $20.6 billion total fund, including $5.99 billion General Fund, is net of the $537 million total fund and $217 million General Fund reductions. HCPF’s budget recognizes the need for Colorado to balance its budget in light of the state’s budget deficit fueled by our Medicaid cost trends, TABOR revenue limits, revenue reductions due to H.R. 1 that resulted in the August Special Session, and future H.R. 1 federal funding reductions like the Provider Tax. We will continue to work with stakeholders to leverage the Medicaid Sustainability Framework as we navigate this difficult chapter.
Given the fiscal challenges Colorado faces, on October 31 as part of the budget release, the Governor issued Executive Order D25 020 to make additional FY 2025-26 reductions, which include $13.5 million in new HCPF general fund reductions, $41.7 million total fund reductions. All reductions included in the Executive Order D25 014, signed August 28, 2025, remain in effect. HCPF is requesting all Executive Order reductions be extended into FY 2026-27. These measures target outlier trends, promote program integrity, and preserve member coverage while minimizing service impacts. We expect additional reductions to be released in January 2026 through the supplemental and budget amendment processes, impacting both FY 2025-26 and FY 2026-27. The January reductions will further slow unsustainable Medicaid trends and help achieve a longer-term goal of bringing Medicaid cost trends more in line with TABOR. We deeply appreciate your collaboration and shared commitment to sustainability.
While these reductions are difficult, they are part of a broader effort to stabilize Medicaid cost trends and maintain access to care. Medicaid cost trends remain elevated, outpacing revenue growth and driving the need for cost management. Our ongoing work with a third-party consultant to benchmark Colorado’s Medicaid program against other states will provide valuable insights to refine cost management strategies, reimbursement methodologies, and policy approaches. Findings expected this winter will help inform both our FY 2026–27 and FY 2027–28 budget planning.
HCPF submitted the Rural Health Transformation Program (RHTP) application to the Centers for Medicare and Medicaid Services (CMS) on November 4. The RHTP is designed to transform the existing rural health care infrastructure and build sustainable health care systems that expand access, enhance quality of care, and improve outcomes for members. This federally funded opportunity will provide grants totaling $50 billion from Federal Fiscal Year (FFY) 2026 through FFY 2030, with $10 billion available each year. Half of the funding will be evenly distributed to all states with approved applications, totaling an estimated $100 million per state per year. The other half will be awarded to approved states based on individual state scored metrics and applications that reflect the greatest potential for, and scale of impact, on the health of rural communities. CMS is expected to announce awardees by December 31, 2025. For more information and to sign up for the RHTP newsletter, please visit our website. HCPF and the Colorado Rural Health Center will be hosting a joint webinar on December 2 from 10 to 11:30 a.m. to provide an overview of the RHTP application and walk through the next steps in the program process. Please register here.
In addition to the RHTP, HCPF continues to prepare to meet the requirements of H.R. 1 mandates, including Work Requirements, six-month eligibility redeterminations, federal funding clawback risks, and more. These H.R. 1 federal mandates will create administrative burden for members, county partners and Medical Assistance sites, while requiring new technology investments to build the necessary administrative systems while increasing eligibility processing staff to handle the workload. The loss of coverage due to H.R. 1 will also impact members, care providers, and our economy. We will be working with members, providers and stakeholders to mitigate those negative impacts in the coming months. We thank you in advance for your partnership on this important, collaborative work.
How You Can Engage. We will continue to engage with stakeholders throughout the month to gather feedback on all this important work.
- HCPF recently launched a new webpage specific to H.R. 1, which provides information on the federally mandated changes to Health First Colorado, Colorado’s Medicaid program and Child Health Plan Plus (CHP+) and their impact on our programs in Colorado. This page also highlights educational resources to help with understanding the impact of H.R. 1 and federal changes to Medicaid, as well as an updated fact sheet on Work Requirements.
- Additionally, we launched Colorado’s Medicaid Sustainability Framework webpage that outlines our plans to manage Medicaid trends and avoid draconian cuts in the face of state budget challenges and decreased federal funding due to H.R. 1.
To submit a question or comment related to H.R. 1, please use our online form. You can also email us at hcpf_HR1@state.co.us. We are deeply grateful for your partnership and support.
- October 2025
H.R. 1 Update: Rural Health Transformation Program and Other Federal Policy Impacts
Rural Health Transformation Program. The Department of Health Care Policy and Financing (HCPF) is collaborating with a broad array of stakeholders to apply for the Rural Health Transformation Program (RHTP), authorized by H.R. 1. The RHTP is designed to transform the existing rural health care infrastructure and build sustainable health care systems that expand access, enhance quality of care, and improve outcomes for members. This federally funded opportunity will provide grants totaling $50 billion from Federal Fiscal Year (FFY) 2026 through FFY 2030, with $10 billion available each year. Half of the funding will be evenly distributed to all states with approved applications, totaling an estimated $100 million per state per year. The other half will be awarded to approved states based on individual state scored metrics and applications that reflect the greatest potential for, and scale of impact, on the health of rural communities.
Applications are due November 5, 2025, and the Centers for Medicare and Medicaid Services (CMS) is expected to announce awardees by December 31, 2025. In addition to engaging with stakeholders, HCPF is researching existing state programs and priorities to identify opportunities for alignment and efficiency; developing information on financial status and economic impact analysis; and establishing an Advisory Board to make recommendations for implementation. For more information and to sign up for the RHTP newsletter, please visit our website.
H.R. 1 Specifics and Impacts. In addition to the Rural Health Transformation Program, H.R. 1 will have a significant effect on the 375,000 low income adults without disabilities covered through the Affordable Care Act (ACA) Medicaid Expansion. Starting in January 2027, states must implement renewal redeterminations every 6 months instead of every 12 for this population. We also need to implement Work Requirements for most “able-bodied” Expansion adults, who will need at least 80 hours per month of work, job training, school, or volunteering to maintain their Medicaid coverage. People with disabilities are not subject to the Work Requirements mandate, nor are individuals who are defined by the state as Medically Frail. More information about exemptions is on our website.
These H.R. 1 federal mandates will create administrative burden for members, county partners and Medical Assistance sites, while requiring new technology investments to build the necessary administrative systems as well as increasing eligibility processing staff to handle the workload. The loss of coverage due to H.R. 1 will also impact members, care providers, and our economy. We will be working with members, providers and stakeholders to mitigate those negative impacts in the coming months. We thank you in advance for your partnership on this important, collaborative work.
All HCPF’s emerging advances and project work necessary to comply with H.R. 1 will pursue the following shared goals. Thank you for your support in achieving these critical goals:
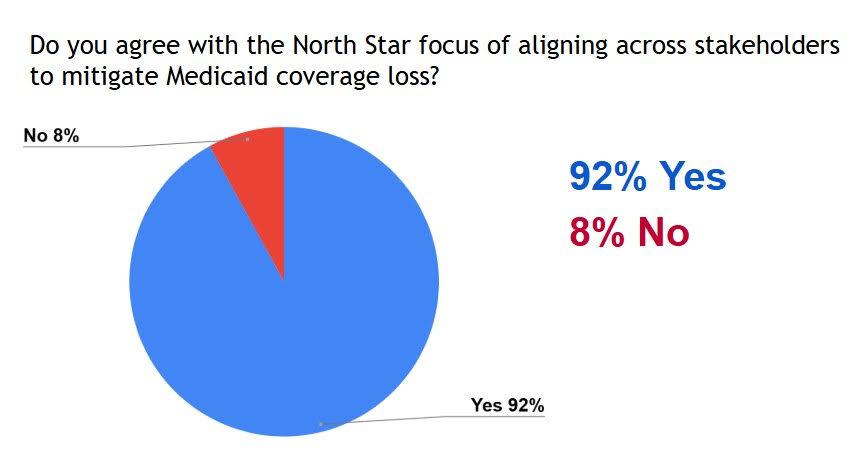
- North Star: Protecting Coloradans’ Access to Medicaid. Our North Star focuses on reducing inappropriate loss of Medicaid coverage impacting 375,000 Expansion members due to H.R. 1 federal mandates such as renewal determinations every 6 months versus 12, the new Work Requirements mandate, other H.R. 1 provisions and the downstreaming impact of H.R. 1 on members, providers, county and other eligibility site partners. Loss of coverage reduces the health and well-being of impacted Coloradans, fuels medical debt and personal bankruptcies, increases provider uncompensated care while also threatening available services and the health care workforce. 92% of our August 12 Webinar attendees agreed with this important North Star goal.
- Mitigation of Significant Federal Funding Clawback Risks. Medicaid and CHP+ benefits are subject to CMS’s Payment Error Rate Measurement (PERM) audits. Historically, CMS has accepted corrective action plans when audit findings exceed tolerance thresholds. Under H.R. 1, CMS federal funding clawback risk starts above a 3% error rate, with each 0.1% audit finding above 3% representing about $9.3 million General Fund in potential federal funding clawbacks. In other words, if we incur a 5% error rate, the hit to our General Fund could be around $186 million. Further, there is no longer an option to avoid state fiscal clawbacks with a corrective action plan. These PERM audits will cover 2026 eligibility determinations, so our ability to quickly implement risk mitigation initiatives is key. HCPF audit teams are evaluating the drivers of historic audit findings and the actions and resources necessary to insulate Colorado from this increasing H.R. 1 federal PERM clawback risk.
- Driving Operational Efficiencies and Compliance. Strained budgets combined with increasing administrative burden will necessitate new thinking and improved efficiencies to help us better navigate these realities. This may include county infrastructure efficiencies like the Joint Agency Interoperability work, advances in CBMS automation, increasing use of AI, other technology advances, HCPF/CDHS - County efficiency collaborative pathways, and more.
H.R. 1 Work Requirements. HCPF is actively working with CMS to pursue flexibilities to help us achieve these important shared goals. Final federal guidance will not be available until June 2026, so we are designing and building eligibility system advances leveraging interim CMS communications.
- First, CMS communications indicate states may release a “Minimum Viable Product” or MVP to be in compliance with H.R. 1 Medicaid Expansion Work Requirements effective January 2027 versus completing all the IT work and connectivity required in H.R. 1. This new MVP alternative provided by CMS makes sense given the extreme challenge in completing H.R. 1’s heavy IT lift by January 1, 2027, in combination with the lack of Waivers allowing states more time to build out H.R. 1’s massive IT infrastructure. The MVP approach will enable Colorado to pursue reasonable advances in automation to reduce member and county processor burden given the realities of Colorado’s system build capacity and budget constraints. This MVP allows us to educate stakeholders earlier so we can build the stakeholder partnerships and member outreaches necessary to help members get through the new processes.
- A second Work Requirements flexibility communicated by CMS is the ability to potentially leverage member “self-attestation” of their exemptions and compliance with Work Requirements, including some of the required 80 hours of volunteering and potentially school. That approach could mean members may complete a new questionnaire or form as part of the renewal or new application process to attest as to which exemptions or Work Requirements criteria that apply to them. Additional federal guidance on this potential flexibility is expected before the end of the year.
- A third CMS flexibility allows states to define Medically Frail, which is one of the exempting factors from Work Requirements. That might include such attributes as homelessness, active chemotherapy treatment, inpatient substance use disorder treatment and more.
We are pursuing each of these flexibilities in the initial design of our Work Requirements Minimum Viable Product. As with implementation of any new federal law, we will balance evolving federal guidance in our operational design and planning.
How You Can Engage. We will be engaging with stakeholders beginning this month to gather feedback on all this important work. Please complete this survey to help us understand your concerns about H.R. 1 implementation and how we can best share information with you.
- HCPF recently launched a new webpage specific to H.R. 1, which provides information on the federally mandated changes to Health First Colorado, Colorado’s Medicaid program and Child Health Plan Plus (CHP+) and their impact on our programs in Colorado. This page also highlights educational resources to help with understanding the impact of H.R. 1 and federal changes to Medicaid, as well as an updated fact sheet on Work Requirements.
- In the coming weeks, we’ll be adding a calendar of events for stakeholders to engage with us on this important work as well as additional videos and FAQs to keep you updated on all things H.R. 1. The next upcoming stakeholder engagement opportunity is on Member Communications on October 16 at 12 p.m.
- Additionally, we launched Colorado’s Medicaid Sustainability Framework webpage that outlines our plans to manage Medicaid trends and avoid draconian cuts in the face of state budget challenges and decreased federal funding due to H.R. 1.
To submit a question or comment related to H.R. 1, please use our online form. You can also email us at hcpf_HR1@state.co.us. Together, we can navigate this new chapter to achieve our shared goals. As always, we thank you for your partnership and support.
- August/September 2025
Navigating State Budget Challenges and New Federal Mandates
Annual Webinar. Thank you to the 2,800 stakeholders who registered for the Department of Health Care Policy and Financing (HCPF) Annual Stakeholder Webinar on August 12. We discussed state budget challenges, Medicaid cost trend drivers and solutions to address them, the impact of H.R.1 (One Big Beautiful Bill Act), emerging plans to address it, and HCPF priorities for fiscal year (FY) 2025-2026. Recordings and materials are posted on our website.
State Budget and Medicaid Cost Trends. H.R.1, signed into law on July 4, 2025, saddled Colorado with a $1+ billion budget shortfall this fiscal year. As a result, Governor Polis called the General Assembly back into session from August 21 to 26 to address this budget gap. They did so by increasing revenues, tapping into the state’s rainy day reserves, and implementing budget reductions. Through the Governor’s August 28 Executive Order, budget reductions across state departments total $252 million, with HCPF budget reductions representing approximately $79 million or 31% of that total.
The level of HCPF’s reductions reflect that our budget represents about one-third of the state’s budget, and that Medicaid cost trends are running at unsustainable levels in recent years due to increases in medical inflation, increases in our benefits, expansion of our coverage programs, outlier trends in certain areas, and outlier increases to our provider reimbursement rates. Specifically, while the Medicaid General Fund cost trends from FY 2015-2016 to FY 2019-2020 averaged +5% annually (0% to 11% range), they averaged +19% from FY 2021-2022 to FY 2024-2025 (12% to 26% range). The chart of data is on slide 8 of the Aug. 12 webinar deck, posted on our website. These increases generally coincide with the allocated federal stimulus dollars intended to pull the nation out of the COVID-induced recession. Colorado leveraged a portion of these stimulus dollars to invest in Medicaid to help transform our behavioral health system, increase the workforce and supports that serve people with disabilities, raise the baseline of provider reimbursements, and more. We should be proud of this work, as it made a better tomorrow for so many. Still, it is important that we all realize that these federal stimulus dollars are behind us, and that the Medicaid increases afforded during this chapter were atypical.
Our more recent Medicaid cost trend increases were further propelled by higher than normal U.S. Medical inflation trends of about 8%, last year, this year, and projected again for calendar year 2026. Medical inflation is an underlying driver of Medicaid cost trends, commercial trends, and Medicare trends, too. When our Medicaid cost trends are running in the 5% range, as in the period noted above, the gap to state revenues is less challenging to navigate. But when the Taxpayer’s Bill of Rights (TABOR) limits state tax revenue growth to 3-4% annually and Medicaid cost trends are running at 19%, as they have averaged over the last several years, the state simply does not have the funds to close this expense to revenue gap, resulting in the need for significant reductions across our programs, benefits and provider reimbursements.
At our August webinar, we reviewed examples of outlier Medicaid benefit trends and provider trends and areas of flat or low trends as well. You can find these slides posted on our website. Several of the HCPF budget reductions shared on August 28 are intended to address areas of outlier and aggregate trends. We appreciate your partnership in helping us avoid draconian cuts to Medicaid by better managing Medicaid cost trends, now and going forward through the Medicaid Sustainability Framework (see slide 9). This framework includes six pillars that enable us to craft and target our trend management efforts in a thoughtful and reasonable way, without making draconian cuts to our programs. 89% of webinar attendees agreed with this framework, and 78% said it should be HCPF’s top focus.
To further support our efforts to reduce Medicaid trends, HCPF has retained a third party consultant to compare our programs, reimbursements, cost management solutions and more to other Medicaid programs around the nation. Our trend management strategies will be refined and expanded based on these learnings as well as stakeholder engagement using an external facilitator to invite broad-based stakeholder input. We should receive those consultant insights this winter and will conduct the final round of related stakeholder engagement to solicit feedback at that time.
We are also focused on innovations and advances to help us better control Medicaid cost trends. The Accountable Care Collaborative (ACC) is a major lever in this quest, with ACC Phase III implemented July 1, 2025, including advances such as: case management and health improvement programs; Accountable Care Organization (ACO)-like primary care systems and supports (free to rural health clinics and independent rural PCPs); advances in technologies such as eConsults, Prescriber Tool, Value Based Payments and more.
HCPF is also advancing our fraud, waste and abuse processes. Many of our existing efforts satisfy requirements within H.R.1, but additional efforts are needed based on outlier provider behaviors in certain benefit areas and within certain provider types. According to webinar attendees, advancing fraud, waste, and abuse tools and techniques should be one of HCPF’s top five priorities. Learn more about our fraud, waste, and abuse efforts from this fact sheet.
H.R.1 Federal Impacts
Much of the impact of H.R. 1 will be felt by the 377,000 Coloradans covered by Medicaid expansion. Medicaid expansion was a key provision of the Affordable Care Act (ACA) that allows states to cover more low-income individuals who may not have previously qualified for Medicaid. H.R. 1 impacts the expansion population in three major ways. First, it steadily decreases federal funding through reductions in provider fees, which are projected to reduce available state revenues by $1-2.5 billion by the end of the impact period 2028-2032. In Colorado, the provider fee is called the CHASE fee and is instrumental in increasing payments to providers as well as financing health coverage for low income adults; children and pregnant women covered by Child Health Plan Plus (CHP+); and adults and children with disabilities in the Medicaid Buy-In Program.
Second, H.R. 1 increases eligibility redeterminations for Medicaid expansion members from annually to every 6 months, creating more paperwork and administrative burden for both members and our county partners. Finally, H.R. 1 requires states to implement “work requirements” for most “able-bodied adults” to prove they are working, in a work program, going to school, or volunteering at least 80 hours a month (in the aggregate) to qualify for Medicaid coverage. In addition to the administrative burden these two federal mandates create, their implementation also requires new technology investments to build the necessary administrative systems. Risk of member disenrollment is also increased, for not meeting the requirements or not completing the necessary paperwork to prove that they did. Ninety percent (90%) of webinar attendees were alarmed by the emerging health insurance coverage loss threats to Coloradans created through H.R.1.
Loss of coverage also generates concerning downstreaming impacts, such as increased uninsured rates, poor health outcomes because of a lack of affordable access to care, medical debt or bankruptcies for those who lose coverage and seek care, increased provider uncompensated care, provider layoffs and reductions in services as their revenues fall, the cost shift of uncompensated care to commercial health insurance rates paid by Coloradans and employers, and the negative impact to our overall economy. For all of these reasons, our North Star focus is to mitigate inappropriate loss of Medicaid coverage from the impacts of H.R.1, which 92% of our webinar attendees agreed with. We thank our partners – providers, consumer advocates, counties, elected officials, Regional Accountable Entities, Case Management Agencies, contracted vendors and more for your collaborative efforts to help us achieve our North Star.
The passage of H.R. 1 also created the Rural Health Transformation Program, which will provide $50 billion in federal grant funding across states to support rural providers from Federal Fiscal Year 2026 to 2030 ($5 billion/year). Colorado is leveraging HCPF’s expertise and our partner’s expertise to apply for this newly available federal funding. We invite you to visit our fact sheet to learn more about this opportunity. When asked how these funds should be invested in Colorado, webinar attendees ranked “recruiting and retaining clinical workforce talent in rural areas” as their top priority (65%).
Our Ask of You and How You Can Engage to Help. Clearly, H.R.1 creates new challenges. But we are Coloradans, and we know how to come together to tackle a challenge and help each other through that challenge. We are experts at climbing mountains to get to our destination, charting our path, and navigating through difficult terrains.
We have about a year to better prepare for - and do all we can to mitigate - the negative impacts of H.R.1. This makes the challenges we face different than the short time we had to ready the state for the Public Health Emergency (PHE) Unwind. Please join us in leveraging this time to achieve our shared goals. One of the ways you can help is by sharing our messages to members early and often. Many of you are also trusted messengers - primary care docs and specialists, behavioral health providers, dentists, consumer advocates, community partners, RAEs, counties, elected officials and more. Our expansion members need to know what actions they need to take, and they need to take them. In this spirit, please share our newly recorded, short Member Message.
We also invite you to bookmark our Understanding the Impact of Federal Changes to Medicaid website where we will share key implementation information, post updated fact sheets and facilitate opportunities to engage with us all throughout this chapter. Everyone reading this message has a role to play in our quest to achieve our North Star - avoid inappropriate coverage loss, and we are doubling down on facilitating opportunities for you to engage in the coming weeks and months.
You can also send related questions to hcpf_HR1@state.co.us. And please invite your colleagues and associates to stay informed by signing up to receive HCPF’s At A Glance Monthly Newsletter.
Thank you for your collaborative engagement as we work together to better manage Medicaid trends, avoid draconian cuts to Medicaid, and implement H.R. 1 in a way that achieves our North Star of mitigating inappropriate coverage loss. We appreciate your partnership.
- July 2025
Federal Changes to Medicaid
H.R.1 – the One Big Beautiful Bill Act (OBBB), was signed into law July 4 and represents the largest cuts to Medicaid since the program began in the 1960s. The Department of Health Care Policy and Financing (HCPF) anticipates that the bill will ultimately result in the large-scale loss of health coverage for Coloradans and an extraordinary, longer term funding shift from the federal government to our state that Colorado’s state budget cannot absorb.
One change took effect immediately - our ability to use federal funds to pay certain reproductive health care providers, largely impacting Planned Parenthood and the thousands of Medicaid members who use them for primary care and women’s health services. We are working to ensure members impacted by this change are connected to other providers to receive needed services.
Some provisions that affect Colorado Medicaid members and providers do not take effect until December 2026. This includes increasing eligibility renewal frequency from annually to every 6 months, as well as the new work requirements provision, both of which impact the 377,000 member Medicaid Expansion population. Implementing these federal mandates will require significant IT system investments, staffing resources, industry and efficiency advances, massive communications, stakeholder engagement and more. The work requirements aspect of the bill is especially concerning.
HCPF remains committed to improving efficiencies within our eligibility ecosystem while advancing automation where possible to reduce administrative burden for our members, county partners and others impacted by the bill. That said, creating an entire industry and ecosystem that captures and feeds work requirements related, member-specific data insights into the eligibility process required by the bill - like student status, work hours, and volunteer or community work - will be a very heavy lift, especially given the December 2026 deadline. Further, automating the processing of those insights into the eligibility ecosystem will also be an important part of the design, build and investment process to mitigate this new and significant barrier to Coloradans securing or maintaining eligibility. While federal waivers to states that need additional time to build this capability are a component of the bill, securing a waiver is not a certainty, nor is the additional time a waiver might allow.
HCPF efforts will focus on our north star, which is to mitigate inappropriate health care coverage loss and the challenging downstreaming results, such as increased uninsured rates, poor health outcomes and medical bankruptcies for those who lose coverage, increased provider uncompensated care, and the cost shifting that will increase commercial health insurance rates paid by Coloradans and employers as a result.
OBBB provisions that decrease provider fees and related federal funding will significantly reduce revenues to cover Medicaid and the Children's Health Insurance Program (CHP+) beginning October 2027. This reduction in federal funding will propel very difficult conversations necessary to balance program expenses with lower available revenues. Specifically, federal funding collected through HCPF, in partnership with the Colorado Healthcare Affordability and Sustainability Enterprise (CHASE) will decrease; this funding finances care for more than 425,000 Coloradans covered under Medicaid Expansion, Buy-In Programs for Individuals with Disabilities, and CHP+ coverage for children and pregnant women each year. This funding also significantly increases reimbursements to Colorado’s hospitals. Beginning October 2027, the amount of federal funds that states can draw down decreases each year by 0.5%. Each incremental reduction of 0.5% to the threshold would result in an estimated reduction of over $115 million in provider fees that can be collected from the hospitals and a loss of approximately $180 million to $525 million in federal matching funds for hospital reimbursement or expansion coverage, depending on policy decisions made by the state. Once the threshold reaches the target of 3.5% in federal fiscal year 2032, the estimated annual reduction would be over $550 million in collected fees from hospitals, generating a reduction in federal funds that could be drawn down ranging from $900 million to $2.5 billion annually, depending on policy decisions made by the state.
This federal reduction in funding to all states will further complicate our existing state budget challenges, requiring advanced planning, early action, efficiency partnerships, stakeholdering, and lots of collaboration to balance Medicaid and CHP+ costs with shrinking revenues.
Related, last month HCPF also submitted a State-Directed Payment (SDP) proposal for hospital payments to the Centers for Medicare and Medicaid Services (CMS) for review. The SDP is a mechanism that state Medicaid programs have used to allow targeted supplemental payments for care provided under Medicaid managed care arrangements. These efforts represent another step taken by hospitals, the Colorado Hospital Association, the CHASE Board and HCPF to address fiscal concerns, in accordance with HCPF’s Medicaid Sustainability Framework. The addition of hospital SDP funds would provide more ways to bolster inpatient and outpatient services for both urban and rural hospitals across Colorado, as well as psychiatric institutions. If CMS approves the proposal, the new SDPs could increase overall funds by an estimated $378 million beginning in the state fiscal year 2025-2026. This would represent more than $295 million of estimated net new funds going to urban hospitals, more than $75 million of estimated funds going to rural and critical access hospitals and $4 million of estimated funds going to psychiatric institutions. Thank you to all partners who worked so hard with HCPF experts to complete a huge amount of complex work in a short amount of time to make this happen.
HCPF recognizes that these new federally mandated changes will impact all Coloradans, not just those served by our safety net coverage programs. We will collaborate with other state departments and stakeholders to double down on efforts to mitigate the commercial health insurance price increases that will result from the provisions of this bill. We must also advance and increase efforts to mitigate the financial threats to doctors, hospitals, and other care providers from this bill - especially rural providers - that will occur as uninsured rates rise, driving increases in uncompensated care costs that will threaten care access, health care jobs, and ultimately the solvency of certain providers.
HCPF will continue to communicate broadly and transparently with members and stakeholders on these and other issues, and in advance of changes to program eligibility requirements, processes, benefits, coverage or provider reimbursements.
We will continue to post updates on our federal resource center. There you will find the most recent information and a variety of tools, such as:
- CO Medicaid Insights and Potential Federal Medicaid Reduction Impact Estimates
- Hospital Provider Fee fact sheet - in the process of being updated
- Work Requirements fact sheet - in the process of being updated
- Long Term Services and Supports fact sheet
- Protecting Against Fraud, Waste and Abuse
- County specific fact sheets
- Congressional District specific fact sheets
- Medical Assistance Coverage fact sheet
With the federal changes creating more pressure on an already strained Colorado budget, we must focus on controlling Medicaid cost trends. One of the ways we are doing this is by advancing our Accountable Care Collaborative (ACC), the primary delivery system for Health First Colorado. On July 1, 2025, we transitioned to Phase III of this program. Designing ACC Phase III has been a multi-year effort with the participation of thousands of stakeholders across Colorado. Thank you to everyone who engaged in the stakeholder efforts. All efforts are now paying off in real time.
Phase III of the ACC makes comprehensive advances to increase accountability and transparency; enhance care and case management and health improvement programs; create Accountable Care Organization (ACO)-like primary care performance with a special focus on better supporting rural primary care providers and rural health clinics advance their infrastructure to drive quality of care, affordability and their sustainability; and advance technology across the board. Regional Accountable Entities (RAEs) are a critical component of the ACC and are responsible for promoting member health and well-being. As part of Phase III, RAEs will: increase focus around supporting member transitions of care from inpatient and residential settings; implement member incentives over time; and provide ACO-like primary care infrastructure support for independent rural primary care providers and Rural Health Clinics. In addition to RAEs, the ACC includes two managed care organizations (MCOs) that contract with providers and manage member physical health benefits in their service areas. HCPF’s new partners effective July 1, 2025, include:
- RAE Region 1 and MCO: Rocky Mountain Health Plans (RMHP) and RMHP PRIME
- RAE Region 2: Northeast Health Partners
- RAE Region 3: Colorado Community Health Alliance
- RAE Region 4: Colorado Access
- Elevate (Denver Health) Medicaid Choice
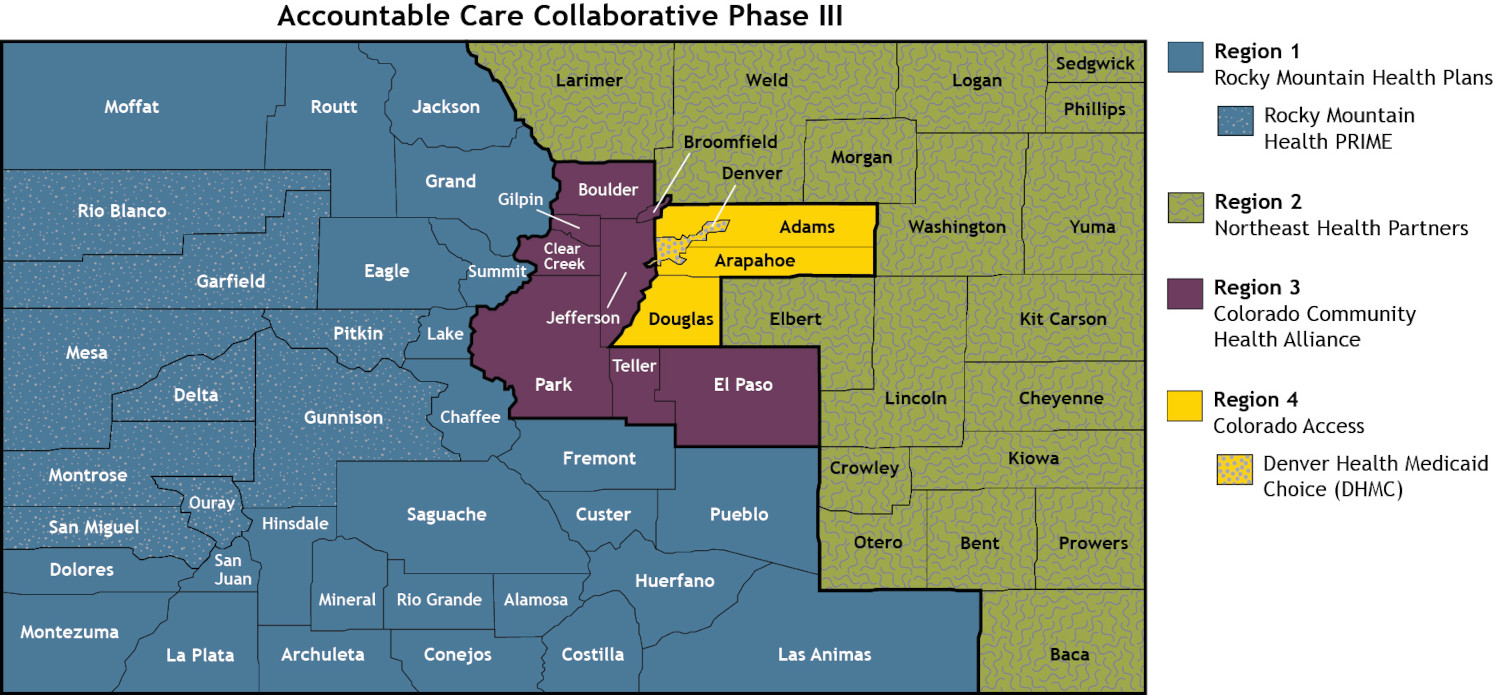
HCPF’s RAE Regions match the Behavioral Health Administrative Service Organizations (BHASOs) regions, administered by the BHA, to the betterment of the provider and member experience, patient outcomes and administrative efficiencies. RMHP is also the BHASO in Region 1; Signal Behavioral Health Network is the BHASO in Regions 2, 3, and 4. For more information on ACC Phase III, please visit our website.
This and other HCPF priorities are included in our Department Performance Plan, which has been updated and posted to our website as of July 1.
We invite you to register for our Annual Stakeholder Webinar on August 12 from 9 -11 a.m., which will cover additional details on the OBBB provisions, the process to address them, state budget challenges, Medicaid cost trend drivers, and priorities for fiscal year 2025-2026. We look forward to engaging with you then.
Thank you again for your collaborative partnership in tackling our emerging, shared realities.
- June 2025
2025 Legislative, Trend Controls, and Federal Update
Thank you to the General Assembly, advocates, providers and other stakeholders for partnering to advance bills that support the Coloradans we cover and serve. Below are highlights of the legislative session related to the Department of Health Care Policy and Financing (HCPF). Please visit our Legislator Resource Center for our latest fact sheets on the 2025 legislative session.
- Sound stewardship of taxpayer dollars is a daily focus for HCPF. SB25-314 implements improvements to the Medicaid Recovery Audit Contractor (RAC) program such as: reducing RAC program administrative burden for providers, improving provider training to mitigate overbillings, improving program efficiencies, reducing delays in overpayment recoupments to the benefit of state General Fund, and increasing provider accountability. HB25-1033 reinforces that HCPF is the payer of last resort with commercial carriers and any inappropriate payments are refunded to HCPF.
- HCPF also streamlined waivers to create the Children with Complex Health Needs Waiver (HB25-1003); continuing the Complementary and Integrative Services Waiver through September 1, 2030 (SB25-226); developing a Workforce Capacity Development Center to train and certify more providers in evidence-based interventions so they can best serve kids with complex behavioral health needs through (SB25-292); and delaying the move of residential treatment from the child welfare block to behavioral health capitation via Regional Accountable Entities (SB25-294) for one year.
- SB 25-264, SB25-228, and SB25-270 repeal outdated cash funds and move certain cash funds to an enterprise to address state budget challenges. SB25-308 creates a cash fund for state dollars designated to 1115 waiver programs, such as health related social needs and re-entry services for those leaving prison or jail after incarceration.
HCPF Budget. Signed into law through the Long Bill, the HCPF fiscal year 2025-26 budget is $18.2 billion total fund and $5.5 billion General Fund, which represents about one-third of the state’s budget. 96% of HCPF’s budget pays our health care providers with 4% going to HCPF administration. More information about our budget can be found on our website.
Better Controlling Medicaid Claim Costs & Trends. While there were no large cuts made to Medicaid through the legislative or budget process this year, collaboration on better controlling Medicaid cost trends is a high priority as we begin the fiscal year 2026-27 budget process. HCPF’s Medicaid Sustainability Framework is designed to help us navigate Medicaid’s multi-year, fiscal challenge while fostering partnership and collaboration to achieve the shared goal of mitigating draconian cuts. The Accountable Care Collaborative (ACC) is the delivery system for Colorado’s Medicaid program and a major lever to better control Medicaid cost trends while improving quality outcomes and access. Phase III of the ACC makes comprehensive advances starting July 1, 2025, and is designed to increase accountability and transparency; advance technology across the board; enhance care and case management and health improvement programs; create Accountable Care Organization (ACO)-like primary care performance with a special focus on better supporting rural PCPs and Rural Health Clinics (RHCs) advance their infrastructure to drive quality of care, affordability and their sustainability. For more information on ACC Phase III, please visit our website.
In addition to the implementation of the ACC Phase III effective July 1, HCPF experts are diving deep into the identification of Medicaid trend drivers as well as the solutions to address them to better manage Medicaid costs. We are also seeking to increase federal funds through a State Directed Payments model prepared in collaboration with hospitals, the Colorado Hospital Association and the CHASE Board - due to CMS by July 1, 2025. As well, we are in the process of hiring third party consultants to help us compare Colorado to other Medicaid programs to identify opportunities as well as outlier trends and related drivers to further our quest to ensure sustainability for Medicaid going forward.
A Focus on Federal Actions. The U.S. House passed a federal budget reconciliation bill on May 22 and that bill is now in the Senate. In its current state, it will drive losses in Medicaid coverage due to the administrative hoops Coloradans would have to jump through to get and stay covered, especially from mandated twice a year renewals and work requirements. Read my full statement after passage of the bill in the House here. Specifically, some proposals being considered by Congress include the following, which may change as the bill moves through the process:
- Implementing work requirements for able bodied adults without dependents, creating mandates and actions for up to 377,000 Coloradans.
- Reducing federal matching funds for the Affordable Care Act expansion population (from 90% to 80% FMAP, representing an estimated reduction of $300 million in funding) if a state provides coverage or subsidizes care for undocumented individuals with state dollars (i.e., Cover All Coloradans, which has about 20,000 children and pregnant women enrolled, so far, and we are seeking further technical clarifications on impacts).
- Increasing frequency of redetermining eligibility for the expansion adults, from annually to semi-annually.
- Reducing federal matching funds during the 90-day “reasonable-opportunity” period until citizenship/immigration verified. (This period refers to a timeframe during which states must provide Medicaid or CHIP benefits to individuals who are otherwise eligible but whose citizenship or immigration status is pending verification. It allows applicants to provide the necessary documentation to verify their status or to work towards obtaining it.)
- Limiting provider fees and state-directed provider payments. (HCPF will submit the new CHASE funding request by July 1 on State Directed Payments, in collaboration with the CHASE Board and the CHASE workgroup.)
- Reducing funding for gender affirming care.
- Reducing funding for providers of family planning services, ie: Planned Parenthood.
Based on the House version of the bill, the Congressional Budget Office estimated that 10.9 million Americans could lose coverage from the bill, and a Kaiser Family Foundation poll found that more than half respondents are worried that Medicaid budget cuts would negatively affect their family’s ability to obtain and afford care.
The U.S. Senate has different rules and norms than the House, which include the deliberation of the Senate Parliamentarian. The Senate Parliamentarian holds the independent authority to make the determination as to if a provision in the reconciliation bill is permitted or not. Specifically, the Senate Parliamentarian ensures that the reconciliation bill’s primary focus is on fiscal matters and may eliminate any provision that is an unrelated policy change. For example, the Senate Parliamentarian has, in the past, removed provisions from reconciliation bills that do not, in their judgement, relate directly to the budget.
We will continue to monitor federal changes and update our Impact of Federal Funding Cuts to Medicaid webpage as details become known. There you will find the most recent information and a variety of tools, such as:
- Video message from me to Medicaid members explaining potential impacts of federal cuts and what we’re doing to protect Medicaid coverage here in Colorado. Member facing partners and providers, please feel free to share this message with covered Medicaid and CHP+ members. We will continue to post similar messages as the federal direction grows clearer and as state budget issues and solutions evolve.
- Updated! CO Medicaid Insights and Potential Federal Medicaid Reduction Impact Estimates
- New! Hospital Provider Fee fact sheet
- New! Long Term Services and Supports fact sheet
- Protecting Against Fraud, Waste and Abuse
- County specific fact sheets
- Congressional District specific fact sheets
- Work Requirements fact sheet
- Medical Assistance Coverage fact sheet
We will continue to voice that the more effective approach to our nation’s fiscal challenges is to drive down the U.S. cost of health care and health coverage, to the benefit of Medicaid, Medicare, the federal budget, state budgets, employers and all Americans. Certainly, this more sustainable approach is preferred over reducing federal Medicaid funding and creating administrative barriers to Medicaid coverage, which reduces enrollment, impacting Coloradans, care providers, the national economy and our state’s economy.
With all this in process, we are also finalizing our FY 2025-26 goals to formalize our priorities and the project work needed to achieve them. Thank you for your partnership through the 2025 legislative session. We will navigate these challenges together in support of serving Coloradans who rely on our safety net coverage programs and the funding that supports them.
- May 2025
Accountable Care Collaborative: Major Lever to Curb Cost Trends
The fiscal year 2025-26 Department of Health Care Policy & Financing (HCPF) budget includes $18.2 billion total funds and $5.5 billion General Fund, representing an increase over fiscal year 2024-25 of 7.4% in total funds, 6.8% in General Fund and 5.4% in the number of Coloradans covered by HCPF’s safety net programs.
Controlling Medicaid cost trends is essential to the sustainability of our safety net programs and the proper management of the state budget. The HCPF Medicaid Sustainability Framework seeks to organize emerging budget reduction concepts and strategies to enable the thoughtful navigation of the state’s multi-year fiscal challenge, while fostering collaboration and alignment between HCPF and key stakeholders to achieve the shared goal of mitigating draconian Medicaid cuts.
The Accountable Care Collaborative (ACC) is a major lever to better control Medicaid cost trends. The ACC is the delivery system for Colorado’s Medicaid Program. Phase III of the ACC makes comprehensive advances starting July 1, 2025, and is designed to increase accountability and transparency; enhance care and case management and health improvement programs; create Accountable Care Organization (ACO)-like primary care performance; better support rural provider sustainability and affordability; and leverage advances in technologies across the board.
Regional Accountable Entities (RAEs) are managed care entities (MCEs) that are a critical component of the ACC. RAEs are expected to understand the nuances among populations in the geographic area they cover to create cohesive provider and community support networks that deliver coordinated, whole-person care that improves health outcomes and better controls Medicaid cost trends. As part of Phase III, RAEs will: increase focus around supporting member transitions of care from inpatient and residential settings; implement member incentives over time; and provide ACO-like primary care infrastructure support for independent rural primary care providers and Rural Health Clinics.
ACC Phase III will build on innovations and tools in Medicaid to help curb cost trends:
- eConsults allow primary care and specialty providers to work together to decide the best treatment options with a member-centered approach to care that reduces unnecessary specialist visits, lowers cost trends, improves member access to care, and reduces specialist visit “no-shows.”
- Prescriber Tool automates the prescribing and prior authorization process to reduce provider admin burden, improve member drug compliance to drive better patient outcomes, improve trend control by increasing preferred drug list compliance and provide information on prescription drug costs so providers can be part of the affordability solution and earn value based payments that reward their efforts.
- RAE ACO-like primary care tools as well as an analytics platform alternative developed in collaboration with HCPF, the Office of eHealth Innovation and the Colorado Community Managed Care Network that provides improved coordination between health care providers through ACO-like analytics, resulting in better trend controls, improved patient outcomes, and ease of administration for providers.
- Providers of Distinction drives quality and affordability indicators and insights to providers and members to help inform decisions on where to access care. Providers can receive value based incentives and referrals for higher quality and trend management performance.
- Value Based Payments incentivize providers to prioritize patient health outcomes as well as affordability. Currently, 52% of Colorado Medicaid payments are value based, exceeding the 50% CMS target for 2025.
- Member incentives will be incorporated under the ACC Phase III in time to improve member engagement in programs like pre-natal care or case management, which improve member health outcomes and trend management.
In ACC Phase III, there will be four RAE regions, plus two managed care organizations (MCOs). This structure creates greater efficiencies and membership volumes necessary to support the increased demands on the RAEs and MCOs, associated with the requirements and advances explained above. HCPF’s new partners effective July 1, 2025, include:
- RAE Region 1 and MCO: Rocky Mountain Health Plans (RMHP) and RMHP PRIME
- RAE Region 2: Northeastern Health Partners
- RAE Region 3: Colorado Community Health Alliance
- RAE Region 4: Colorado Access
- Denver Health Medicaid Choice MCO
HCPF’s RAE Regions match the Behavioral Health Administration’s Behavioral Health Administrative Service Organizations (BHASOs) regions, as promised, to the betterment of the provider and member experience, patient outcomes and administrative efficiencies. RMHP is also the BHASO in Region 1; Signal Behavioral Health Network is the BHASO in Regions 2, 3, and 4.
Thank you to the thousands of participants who engaged in the stakeholder process to inform the ACC Phase III development. All that work comes to fruition effective July 1, 2025. For more information on ACC Phase III, please visit our website.
From a rural perspective, HCPF is working with hospital leadership to implement these innovations, tools and programs as a priority, as they enable rural PCPs to significantly improve quality of care and affordability performance across not just Medicaid, but Commercial and Medicare Advantage plans as well, and earn value based payments for doing so - creating a win/win/win for rural providers, payers and Coloradans. We are also collaborating to identify rural hospital efficiencies in licensure, structure, rural collaborative partnerships and expense sharing through SB23-298 and SB25-078, as well as care coordination infrastructure. This evolution across rural hospitals, rural health clinics and independent rural PCPs is critical to their sustainability, as pillars in care access to rural communities across the state.
On the federal landscape, HCPF continues to monitor the Congressional Reconciliation process. We should begin to have optics into emerging legislation around May 7, which will help inform specific areas of risk for Medicaid. Right now, top threats to Medicaid funding seem to relate to:
- Reducing or eliminating provider taxes: putting in jeopardy Colorado Healthcare Affordability and Sustainability Enterprise (CHASE) federal dollars, which finances coverage for over 425,000 Coloradans covered by Medicaid and CHP+ Expansion; increases Medicaid reimbursements to hospitals, especially rural hospitals while providing an additional $12 million a year in rural hospital assistance to 23 of the lowest revenue rural hospitals; and finances Coloradans with disabilities who buy-in to Medicaid, thereby enabling them to be gainfully employed, while accessing critical support services.
- Medicaid fraud, waste and abuse (FWA), including federal penalties and funding claw-backs for performance in areas such as: not employing comprehensive or aggressive enough efforts and programs; not being in compliance with emerging requirements; and findings associated with federal audits of Medicaid claim payments or eligibility performance. Here is a fact sheet on HCPF’s current and advancing FWA efforts. While FWA has always been a focus for HCPF, all stakeholders should expect continued HCPF advances in this area, in parallel with federal direction and the trend control needs of the state.
- Reducing the federal match rates (FMAP): decreasing the 90% Expansion factor or the CHASE factors that determine the provider fee and the related federal match, such as the Net Patient Revenue 6% formula factor; decreasing the base FMAP (for Colorado, that impacts our 50% base match rate); eliminating or reducing the FMAP floor, which is now at 50%; and reducing or eliminating enhanced administration federal match rates.
- Mandating Work Requirements on the Expansion population or other adult populations.
- Creating a per member funding capitation model.
We continue to update our Impact of Federal Funding Cuts to Medicaid webpage. There you will find the most recent information and a variety of tools:
- New! Video message from me to Medicaid members explaining potential impacts of federal cuts and what we’re doing to protect Medicaid coverage here in Colorado. Member facing partners and providers, please feel free to share this message with covered Medicaid and CHP+ members. We will continue to post similar messages as the federal direction grows clearer and as state budget issues and solutions evolve.
- New! Protecting Against Fraud, Waste and Abuse
- Updated! County specific fact sheets
- Updated! CO Medicaid Insights and Potential Federal Medicaid Reduction Impact Estimates
- Congressional District specific fact sheets
- Work Requirements fact sheet
- Medical Assistance Coverage fact sheet
Given the systemic challenges with the state budget and the continued federal threats to Medicaid funding, we thank you in advance for your engagement in HCPF efforts to educate Congressional elected officials on the impact of Medicaid cuts, to better control Medicaid trends and expenses, to support our rural providers, and to evolve our budget reduction options in a way that mitigates draconian cuts and impact to benefits, populations and providers. And thank you for your partnership and collaboration as we implement ACC Phase III effective July 1.
- April 2025
April 2025
State and Federal Medicaid Budget Pressures
Colorado’s Joint Budget Committee (JBC) has been making very difficult balancing decisions to address a budget gap of more than $1 billion. The Long Bill, which is the mechanism that funds all state programs for the next fiscal year 2025-2026, allocates $18.2 billion total funds and $5.5 billion General Fund for the Department of Health Care Policy & Financing (HCPF). It includes a 1.6% across-the-board Medicaid provider rate increase, as well as budget balancing proposals, such as: decrease of 1.5% HCPF personnel services; $250k Office of eHealth Innovation General Fund reduction; reduction to the Non-Emergency Medical Transportation (NEMT) rate from $6.41/mile to $3.00/mile; prepayment claims review funding to reduce improper payment; delay Medicaid reimbursement for services provided by a Community Health Worker by six months (SB 23-002 originally scheduled to start July 2025); limit behavioral health peer services to certain provider types most appropriate to provide that care; true-up funding for the SB21-009 Reproductive Health Program; rule change to aspheric lenses for prescriptions and enforce requirement of one pair of eyeglasses every two years; revert 988 Suicide and Crisis Lifeline funding; and restructure the nursing home fees and disability insurance premiums financing model.
The JBC scaled back, but approved, our budget requests focusing on increasing support for county administration to improve efficiencies and customer service in connecting Coloradans to our safety net programs; ensuring Colorado supports an equitable system resulting in high-quality, coordinated Medicaid services through the Accountable Care Collaborative Phase III; and funding for the state's All Payer Claims Database. More information about our budget can be found on our website.
Our continued collaboration on better controlling Medicaid cost trends must continue as we begin the process of addressing the fiscal year 2026-2027 budget. HCPF’s Medicaid Sustainability Framework is designed to help us navigate Medicaid’s multi-year, fiscal challenge while fostering partnership and collaboration to achieve the shared goal of mitigating draconian cuts.
Medicaid covers 72 million people nationwide, including about 1.2 million Coloradans. Concerns about federal Medicaid cuts are on everyone’s mind. HCPF has new and updated fact sheets on potential impacts of federal proposals provided below.
- New! Video message from me explaining to Medicaid members the potential impacts of federal cuts and what we’re doing to protect Medicaid coverage here in Colorado
- New! Congressional District specific fact sheets provide district specific Medicaid enrollment and economic impact information
- New! Work Requirements fact sheet explains the potential impact of work requirements proposed as part of federal budget reconciliation
- Updated with new data! CO Medicaid Insights and Potential Federal Medicaid Reduction Impact Estimates provides insights on the most commonly discussed federal Medicaid reduction proposals as well as impacts on Colorado
- Updates with new data coming soon! County specific fact sheets provide county specific Medicaid enrollment and economic impact information
- Medical Assistance Coverage fact sheet provides Colorado specific information on Medicaid eligibility and benefits as well as financing mechanisms
Depending on what Congress ultimately passes, the impact to Colorado’s budget may climb well above $1 billion General Fund. To put that figure in perspective, every $1-1.5 billion in lost federal revenue represents a 20-30% needed increase in the state General Fund to replace it. HCPF’s projected fiscal year 2025-26 General Fund budget is $5.5 billion, meaning a $1 billion federal cut would represent about a 20% impact. Unique to Colorado is the combination of state constitutional provisions impacting our balanced budget requirement as well as revenue limitations propelled by Colorado’s Taxpayer Bill of Rights (TABOR) limit. As such, reductions to federal Medicaid funding may disproportionately impact Health First Colorado (Colorado’s Medicaid program) and Child Health Plan Plus (CHP+) benefits, coverage, eligibility requirements and/or provider reimbursements.
Thank you and our many partners for all you do to care for and support our Health First Colorado and CHP+ members. We appreciate your ongoing engagement as we navigate both federal and state fiscal challenges.
- March 2025
Navigating Federal Funding Threats to Medicaid Concurrent with State Budget Concerns
Concerns about federal threats to Medicaid funding are on everyone’s mind. Here are four tools that will help our partners get their arms around these threats to Colorado, which could impact members and benefits, and climb well above $1 billion General Fund, depending on which options Congress passes. To put that figure in perspective, HCPF’s projected fiscal year 2024-25 General Fund budget is $5.2 billion, meaning a $1 billion federal cut would represent about a 20% impact.
- We crafted two CO Federal Medicaid Funding Threats tools (see the links in the Federal Resources box on the right at the top of the page). One version helps individuals understand funding cut options under consideration to achieve the Congressional Energy and Commerce Committee $880 billion target reduction. The version includes budget reduction projections at the federal level over 10 years, largely provided by the Congressional Budget Office (CBO) and also provides an annual Colorado General Fund budget reduction impact estimate. The second version of the tool leverages the same base information but removes the federal budget reduction estimates.
- To help individuals understand the impact to their local community, HCPF has made available county by county fact sheets with enrollment information, total population in each county covered by Health First Colorado (Colorado’s Medicaid program) or Child Health Plan Plus (CHP+), total Medicaid funding for members covered in that county and top provider types receiving Medicaid funding by county.
- The Medical Assistance Coverage Fact Sheet (see the first link under Overviews and Fact Sheets) answers many questions coming into HCPF, such as: income requirements for Medicaid, CHP+ and to secure Connect for Health subsidies; Medicaid mandatory versus optional benefits; federal and state funding splits by populations, and more.
- HCPF’s Annual Report is on our website, providing a lot of specific information on our safety net coverage specific to fiscal year 2023-24, such as populations covered, payments to providers, federal funding and more.
HCPF is closely monitoring emerging federal revenue reduction or budget cut concepts that may impact Medicaid, our state budget and our members. We will keep you informed as the landscape evolves. Time for HCPF and the state to respond to Federal rule, policy and funding changes may be more challenging due to the recent communication by the U.S. Department of Health and Human Services (HHS), indicating that they are rescinding the policy on Public Participation in Rule Making (Richardson Waiver) and re-aligning HHS’s rule-making procedures. We thank you in advance for your collaboration given this reality.
Colorado Medicaid Sustainability Efforts
Unique to Colorado is the combination of state constitutional provisions impacting our balanced budget requirement as well as revenue limitations propelled by Colorado’s Taxpayer Bill of Rights (TABOR). Accordingly, reductions to Federal Medicaid funding may disproportionately impact Colorado’s Medicaid and CHP+ benefits, coverage, eligibility requirements and provider reimbursements.
The Joint Budget Committee (JBC) is in the process of making very difficult balancing decisions as they tackle a $1 billion budget deficit challenge, though that is subject to change with the next revenue forecast scheduled for March 17. HCPF’s budget represents about one-third of the state’s budget and moves at a historic cost trend of about 7-8% annually, while state General Fund revenues move at a rate of about 3-4% annually. The HCPF Medicaid Sustainability Framework seeks to organize emerging budget reduction concepts and strategies to enable the thoughtful navigation of Medicaid’s multi-year, fiscal challenge while fostering partnership and collaboration to achieve the shared goal of mitigating draconian Medicaid and CHP+ cuts due to our state budget challenges.
Our February forecast update to the JBC included an increase for the current fiscal year 2024-25 ($114 million) and fiscal year 2025-26 ($83 million) based on our most updated insights. This forecast is our best projection of our expenditures for Health First Colorado and CHP+ services and will inform this month’s JBC’s figure setting decisions. The Office of State Planning and Budgeting (OSPB) sent the JBC a letter including potential HCPF budget reduction offsets for the JBC's consideration, given our forecast need for additional funds. The balancing proposals total $22.8 million General Fund in fiscal year 2024-25 and $132.5 million General Fund in fiscal year 2025-26. Ninety-six percent of HCPF’s budget goes to pay health care providers rendering services to our members, while 4% goes to cover HCPF’s administration costs, making Health First Colorado the most efficiently run health plan in the state. More information is available on our budget website and Legislator Resource Center.
HCPF released its annual, statutorily required Hospital Transparency reports on January 15. These reports measure Colorado hospital profits, costs, expenses, the level of community benefit that tax-exempt hospitals offer their communities in lieu of paying taxes, and more. The hospital reports and other materials have been posted on the Hospital Reports Hub website. Key findings from these reports, including Hospital Financial Transparency, Colorado Healthcare Affordability and Sustainability Enterprise (CHASE), and Hospital Community Benefit Accountability, were reviewed during HCPF’s Hospital Transparency Reports Webinar on February 13. Recordings of this event are available in English and Spanish, as is the slide deck. 2025 Hospital Reports Webinar - English/ASL; 2025 Hospital Reports Webinar - Spanish; 2025 Hospital Reports Webinar - Slide Deck.
I want to thank our many partners who serve our members. Your insights and collaboration are important as we navigate the state’s fiscal challenges in combination with the emerging Federal threats to Medicaid. We thank you in advance for your partnership on both these fronts. We are in this together!
- February 2025
Collaborating through a Challenging Chapter
The state is in the midst of balancing a challenging budget, with the Joint Budget Committee (JBC) making difficult balancing decisions over the coming weeks. A contributing factor is the mismatch between medical inflation and related Medicaid cost trends versus TABOR’s impact on available revenues. At the same time, the evolving federal landscape may also impact Medicaid's fiscal challenges. It will take all of us working together to navigate this reality.
HCPF’s Medicaid Sustainability Framework seeks to organize emerging concepts and strategies to enable the thoughtful navigation of this multi-year, fiscal challenge while fostering partnership and collaboration to achieve shared goals. The six points of this framework include:
- Address Drivers of Trend: Better address all the controllable factors that drive Medicaid cost trends.
- Maximize Federal Funding: Leverage and maximize HCPF’s ability to draw down additional federal dollars.
- Invest in Coloradans: Continue investing in initiatives to drive a Colorado economy and educational system to reduce the demand for Medicaid over the long term as Coloradans rise and thrive.
- Make Reasonable Medicaid Cuts or Adjustments: Identify where programs, benefits, and reimbursements are comparative outliers or designed in such a way that we are seeing - or will experience - higher than intended trends or unintended consequences.
- Reassess New Policies: Consider pausing or adjusting recently passed policies not yet implemented.
- Exercise Caution in Crafting Increases to the Medicaid program going forward.
For your convenience, we are providing links to our fiscal year 2025-26 Budget Agenda Summary, Joint Budget Committee budget hearing documents, and December message on the HCPF budget.
We continue to monitor and respond appropriately and thoughtfully to federal actions impacting our programs and will keep you posted with quick but informative communications, as needed.
HCPF’s 2025 legislative agenda includes proposals that merge waivers for children with complex health needs, ensure Medicaid is the payer of last resort with commercial carriers, create a cash fund to support 1115 Demonstration Waiver programs, and create a permanent waiver program offering benefits to specific members. We also welcome your review of our Jan. 22 SMART Act hearing materials and our fiscal year 2023-24 annual report to the community to learn more about HCPF’s strategic priorities, opportunities and challenges, legislative agenda, performance against published goals, and more.
Hospital Transparency Reports Webinar
Thank you to all who attended our recent Hospital Transparency Reports Webinar. These reports measure Colorado hospital profits, reserves, costs, expenses and the level of community benefit that tax-exempt hospitals offer their communities in lieu of paying taxes. Hospitals are essential pillars within the communities they serve. These reports provide insight into hospital financial health. The reports and materials are on our website.
Thank you for your collaborative partnership and thoughtful engagement. We truly appreciate it.
