Report to the Community
Report to the Community
Fiscal Year 2023-2024
The Colorado Department of Health Care Policy and Financing (HCPF) administers Health First Colorado (Colorado Medicaid), Child Health Plan Plus (CHP+), and other public health care programs for Coloradans who qualify.
Our mission is to improve health care equity, access and outcomes for the people we serve while saving Coloradans money on health care and driving value for Colorado.
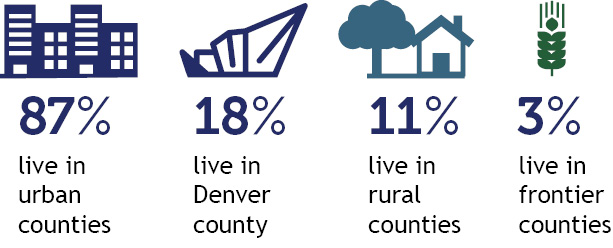
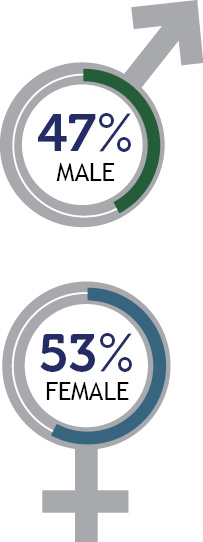
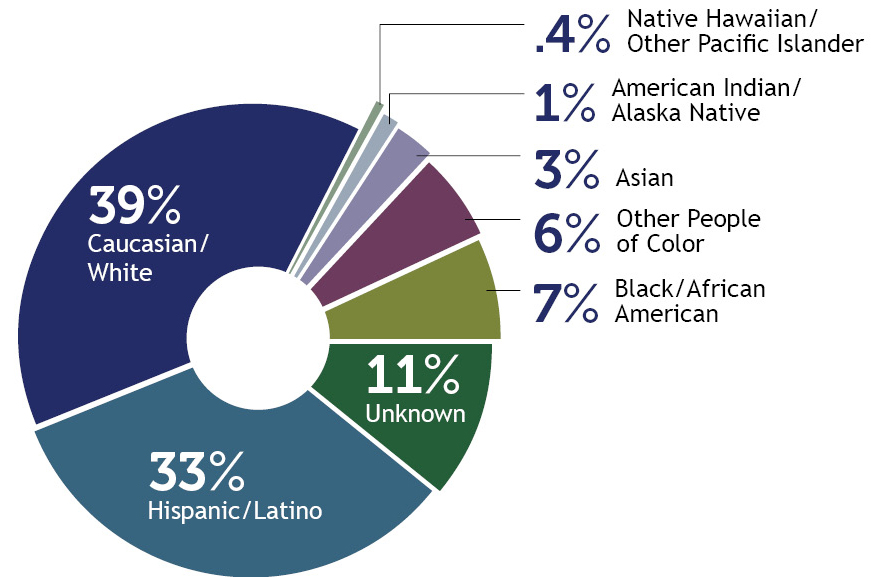
Who we serve
 |  | ||
 | 
| ||
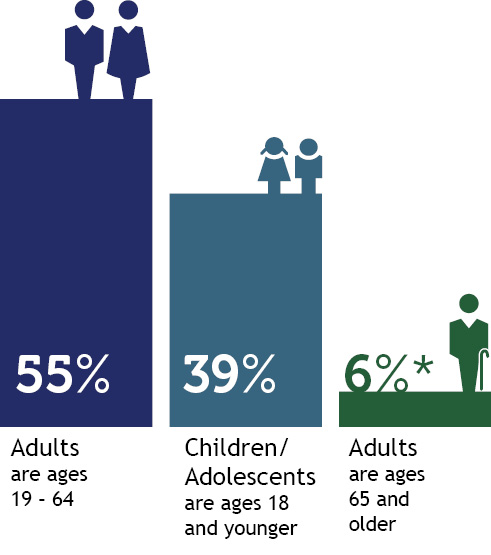 *Adults age 65 and older includes people partially eligible for Health First Colorado. |  | ||
 | |||
Percentage of total population enrolled in Health First Colorado and Child Health Plan Plus, by county
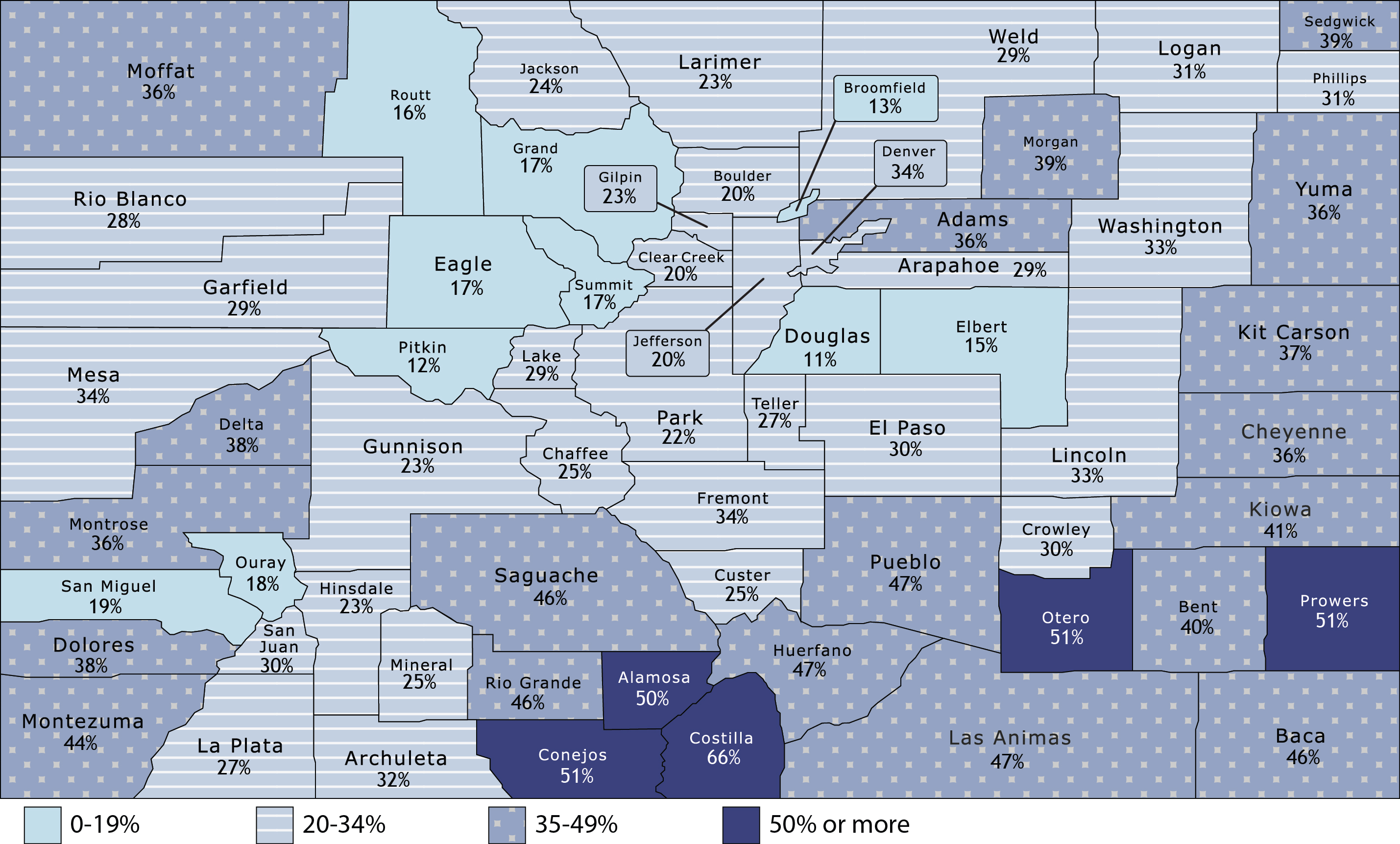
Source of enrollment data is Medicaid Management Information System (MMIS). Percentages represent people enrolled for one day or more during calendar year 2023. 2023 population data as forecasted by the state demographer.
How we deliver care
Health First Colorado (Colorado's Medicaid program) |
Child Health Plan Plus (CHP+) |
Colorado Indigent Care Program (CICP) and Hospital Discounted Care |
Accountable Care CollaborativeThe Accountable Care Collaborative (ACC) is at the core of Medicaid. Launched in 2011, it creates Regional Accountable Entities (RAEs) that deliver innovations, programs and supports that improve care access, equity, and care outcomes while better controlling Medicaid cost trends. Learn more about the ACC. |
676,529 Dental Programs |
23,149 Buy-In Programs |
Long-Term Services and Supports (LTSS) | ||
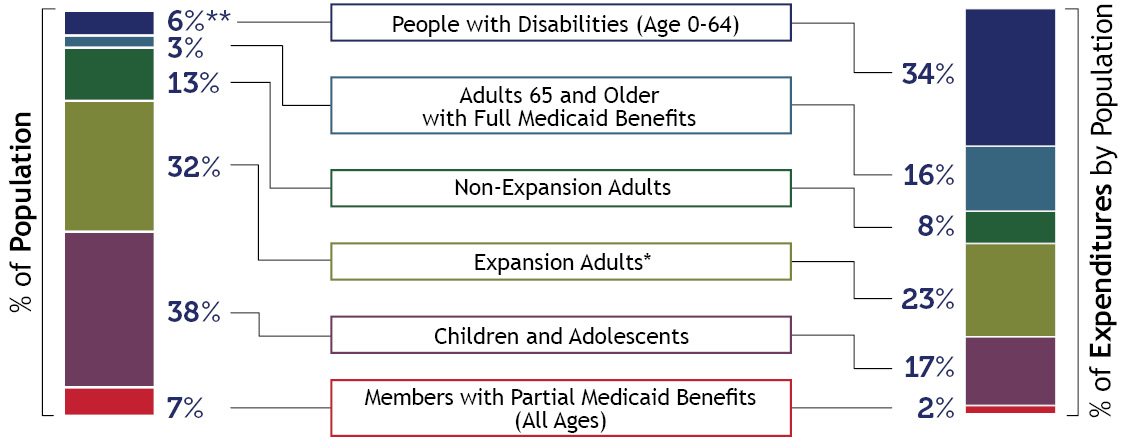
Who is covered and what does it cost?
Patient Protection and Affordable Care Act (ACA) Medicaid Expansion. Due to rounding, percentages may not total 100%. |
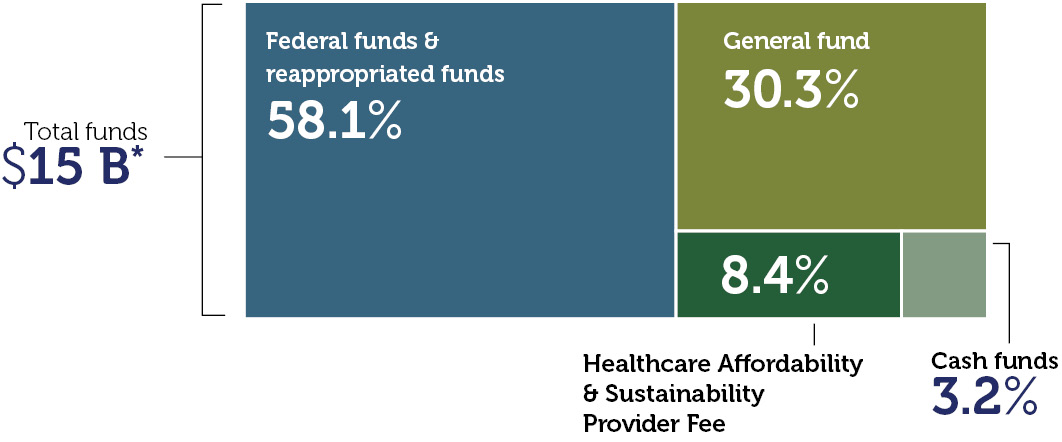
HCPF expenditures by fund
*Includes all services and administrative line items, including Colorado Indigent Care Program and Old Age Pension. Due to rounding, percentages may not total 100%. |
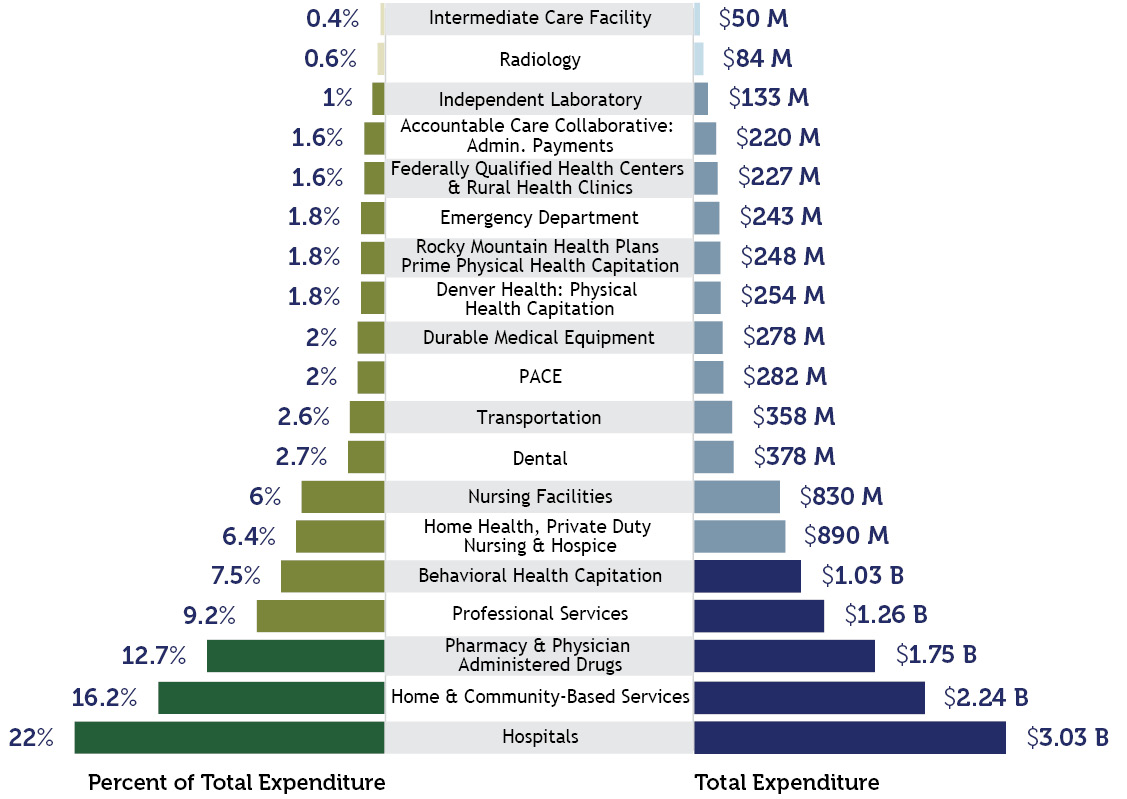
Payment breakdown to Health First Colorado partners
This chart refers to claim costs for member services only, not total Department spending. It is based on claims data by date of service and will differ from data calculated on a cash accounting basis. Due to rounding, percentages may not total 100%. |
Some of our accomplishments in FY 2023-24
To support our mission, we focused on several priority areas:
| Transforming home & community-based care We are leveraging $550 million from section 9817 of American Rescue Plan Act (ARPA) to implement lasting transformation for older adults and people with disabilities. The initiatives we’ve undertaken will enhance, expand and strengthen home and community-based services (HCBS) in Colorado. With an end date of March 31, 2025, we are beginning to wrap up over 60 projects which have supported recipients of HCBS or people with behavioral health needs, their families, providers, and the health care workforce. Our most recent quarterly reports are available on our website. | Leading on affordability HCPF is working to Save People Money on Health Care, focused on the top two drivers of health care costs: prescription drugs and hospital prices. HCPF submitted our state Canadian drug importation plan. To make hospital services more affordable, HCPF is partnering with hospitals to make pricing more transparent and make meaningful changes. As part of that effort, HCPF published nationally leading hospital price, cost and profit transparency reports and analyses, and supported key policies to help inform and drive increased hospital transparency and affordability. |
| Transforming behavioral health HCPF is expanding behavioral health access and services for our members through continued interagency collaboration and new models of care informed by extensive stakeholder engagement. This includes expanding services, adding residential beds, growing the provider network, training and supporting providers, improving transparency and reporting, and catalyzing care coordination. Through federal recovery funds, HCPF invested $140M in community programs including supporting peers with lived experience, piloting permanent supportive housing, improving care transitions, and increasing intensive outpatient care. HCPF partnered with the Behavioral Health Administration to strengthen and support Colorado's safety net by creating new Comprehensive and Essential provider types, developing alternative payment methodologies, and applying for a Certified Community Behavioral Health Clinic (CCBHC) Planning Grant. | Investing in health related social needs HCPF is also expanding benefits for people facing homelessness, food instability, or involved in the criminal justice system through an expansion of the state’s 1115 Demonstration Waiver. This work is creating a future in which Medicaid is able to help cover health-related social needs, providing whole person support to members when they need it most. |
Supporting Coloradans we serve HCPF was involved in two bills that address substance use disorders (SUD). HB24-1045 creates and expands programs and services for SUD treatments while SB24-047 creates several measures regarding the prevention of SUD. HCPF also focused on creating and expanding programs for youth who are in, or at risk of being placed in, out-of-home care through HB24-1038. Both HB24-1400 and HB24-1229 address Colorado Medicaid’s eligibility procedures. HB24-1400 allows HCPF to no longer require additional verification during a member's Medicaid redetermination if certain criteria are met. HB24-1229 gives HCPF the authority to request an expansion of presumptive eligibility to include individuals with disabilities and facilitate prompt delivery of services in a community setting. Other bills passed protect the health and safety of members and state dollars in cases of organized crime or organized fraud schemes (HB24-1146); make a variety of technical changes to multiple state agencies’ required legislative reports to ensure relevancy, timeliness, accountability and transparency (SB24-135); allow a one-time payment of $5 million to safety net hospital Denver Health (HB24-1401); and extend Rural Stimulus Grants funding through the end of 2024 (HB24-1465). | Public Health Emergency Unwind During the COVID-induced public health emergency (PHE), Colorado grew its Health First Colorado (Colorado Medicaid) and Child Health Plan Plus (CHP+) safety net enrollment by more than 45%, or about 550,000 Coloradans. As the nation’s economy recovered, the federal government called an end to the PHE, requiring states to return to regular eligibility renewal processes. We took the time CMS provided to do so - 12 months, or 14 months including noticing. HCPF and its contracted partners outreached more than 2.4 million times via text, email, mailings and phone calls to about 645,000 Colorado households as of June 2024 to educate on what they needed to do to maintain their coverage. For Colorado, April 2024 marked the last month of our year-long “unwinding” of the Medicaid continuous coverage requirement (“PHE Unwind”). In accordance with our February 2024 budget assumptions, Health First Colorado membership has returned to prepandemic levels. HCPF continues its efforts - in collaboration with other state agencies, providers, advocates, partners and stakeholders - to connect members disenrolled through the PHE Unwind to coverage, including employer-sponsored, Medicare, and the Connect for Health marketplace as well as Medicaid and CHP+ as they requalify for our programs. |
| Committing to health equity HCPF created a robust and comprehensive health equity plan to address health outcomes and disparity indicators in three areas: prevention (which includes COVID vaccinations and many other areas), maternal health, and behavioral health in Health First Colorado and CHP+ programs. As part of this focus, HCPF led a statewide health equity task force of more than 60 ambassadors, applied sophisticated analytics and insights to track health equity core measures and indicators, and required vendors to have health equity plans. HCPF also hosted 20 community town halls with over 2,500 members, providers, and other key stakeholders to share HCPF priorities and initiatives. We published the Maternity report in April 2023, which highlights birthing experiences of members and informed HCPF’s roadmap to improve maternal health care and equity. HCPF programs cover over 40% of all Colorado births. | Innovations & advances We continued to innovate to achieve our goals. Value-based payments, which incent our provider partners to focus on delivering better outcomes, represented 36% of our payments, transcending primary care, maternity care, prescription drugs, behavioral health, and hospital care. The Prescriber Tool, eConsults, and the Colorado Social Health Information Exchange are innovations that make it easier to connect members to what they need, whether it be affordable medications, specialist consults or supports for health related social needs, such as housing and nutrition services. |
| Improving the member and provider service experience The members who participate in our programs are at the center of everything we do. We track several metrics to ensure we’re improving their service experience and collect real-time feedback from our Member Experience Advisory Council. In the past year, both our member and provider call centers answered calls in less than one minute, on average. Automatic approval from May 2023 through April 2024 was approximately 33%; in June 2024 the rate jumped to 56% of all renewing households. This means there was no member or eligibility worker activity needed for these approvals. These system innovations have also enabled us to provide real-time eligibility for about 86% of eligible renewals submitted online through Colorado PEAK, allowing members to receive an eligibility decision in real-time. For our providers, claims were processed in less than one minute on average. Together, we navigated the 45% membership growth without major operational issues and expanded the Health First Colorado provider network by adding over 13,000 new providers in fiscal year 2023-24 to increase member access to care. HCPF significantly increased its efforts and focus to address the service issues impacting individuals on LTSS that resulted from the concurrent PHE Unwind, Case Management Redesign, rollout of the Care & Case Management Tool, and Streamlined Eligibility. | |
A message from the Executive Director
I am pleased to share the fiscal year July 2023 through June 2024 annual report for the Colorado Department of Health Care Policy & Financing (HCPF). We were honored to cover and serve an average of 1.46 million Coloradans during this period, including more than 40% of Colorado’s children and more than 40% of births in the state during this year.
During this past fiscal year, and into this current year, we have continued our focus on several key areas.
- Keep Coloradans Covered. Our PHE Unwind was May 2023 through April 2024, plus the 90-day reconsideration period (which ended July 2024), during which members have the opportunity to submit renewal information late and counties have the opportunity to work through their processing backlogs. This period of transition, after more than three years of not acting on renewal determinations, was felt by many. We recognize how challenging that has been and the impact it continues to have. Eligibility performance metrics are improving to the betterment of the member experience and county eligibility processing workloads. Keeping Coloradans Covered remains a focus, as we make ongoing improvements to the Medicaid renewal process while collaborating with partners to connect Coloradans to affordable coverage within and outside of our safety net programs.
- Advance the Medicaid delivery system. The Accountable Care Collaborative (ACC) is the primary vehicle for delivering health care to Health First Colorado members, with Regional Accountable Entities (RAEs) propelling members’ physical and behavioral care coordination, case management and health. During the fiscal year, HCPF focused on crafting and releasing a request for proposal that would advance and modernize the ACC, in the form of Phase III, scheduled to begin July 1, 2025. Combining stakeholder feedback with our experts’ guidance, Phase III is designed to improve care access, equity and quality, and member and provider experience, while managing costs to protect member coverage, benefits, and provider reimbursements. Thank you to the more than 5,700 participants across 135 stakeholder meetings over the past 18 months for your engagement on this important work.
- Transform Behavioral Health. In collaboration with the Behavioral Health Administration (BHA), we continued our work to strengthen Colorado’s Behavioral Health Safety Net System to ensure access to a full continuum of care. This includes a new set of safety net services, connecting new provider types to new Medicaid payment models, services for children and youth, and substance use disorder resources.
- Stabilize Long Term Supports and Services (LTSS). We continued to take actions to stabilize the LTSS system. This includes protecting coverage for LTSS members, timely provider payments to protect access to services, identifying and resolving known issues in the new Care and Case Management Tool (CMM), reducing case management and county backlogs, and leveraging the escalation process.
- Drive affordability and health equity. We continued to innovate to drive quality and reduce disparities that improve the health of our members. Value-based payments in primary care, maternity care, prescription drugs, behavioral health, and hospital care reward improved access to high-quality, equitable and affordable care for our members. As of the writing of this report, 36% of Medicaid payments are value based, and growing. The Prescriber Tool, eConsults, and the Colorado Social Health Information Exchange are innovations that make it easier to connect members to what they need, whether it be affordable medications, specialist consults or supports for health related social needs, such as housing and nutrition services. At the same time, HCPF leverages our health care experts to lead prescription drug and hospital affordability policies, tools and innovations that help save Coloradans and employers money on health care.
For more on what we accomplished together in this past fiscal year, please see our Performance Plan. Thank you again for your ongoing partnership in transforming health care for the betterment of our members and all Coloradans. I hope you enjoy this annual report.

Kim Bimestefer, Executive Director, HCPF

 Live in a setting they choose with the supports they need
Live in a setting they choose with the supports they need Participate in communities that value their contributions
Participate in communities that value their contributions Access services in a simple, timely and streamlined manner
Access services in a simple, timely and streamlined manner Get the highest quality services
Get the highest quality services