Report to the Community
Report to the Community
Fiscal Year 2022-2023
The Department administers Health First Colorado (Colorado’s Medicaid program), Child Health Plan Plus (CHP+), and other public health care programs for Coloradans who qualify.
Our mission is to improve health care equity, access and outcomes for the people we serve while saving Coloradans money on health care and driving value for Colorado.
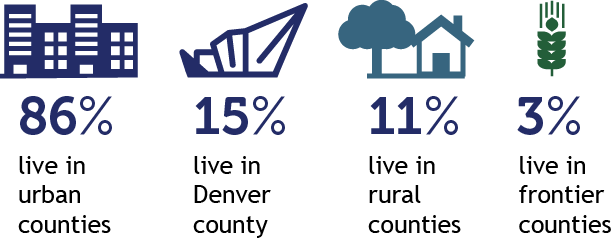
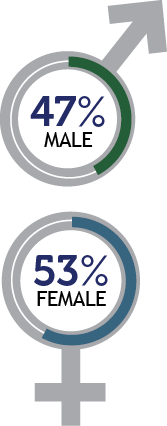
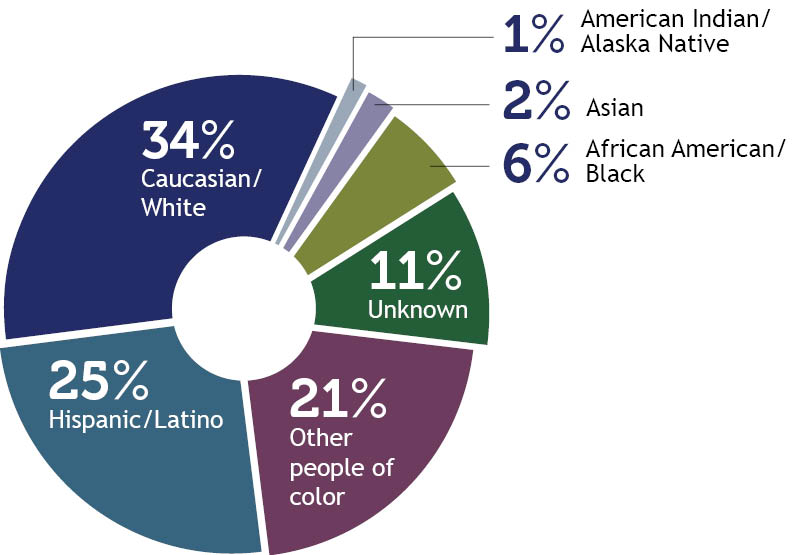
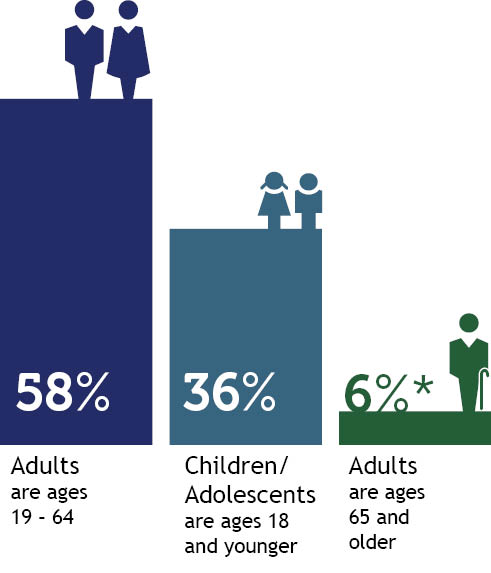
Who we serve
 |  | ||
 | 
| ||
|  | ||
 | |||
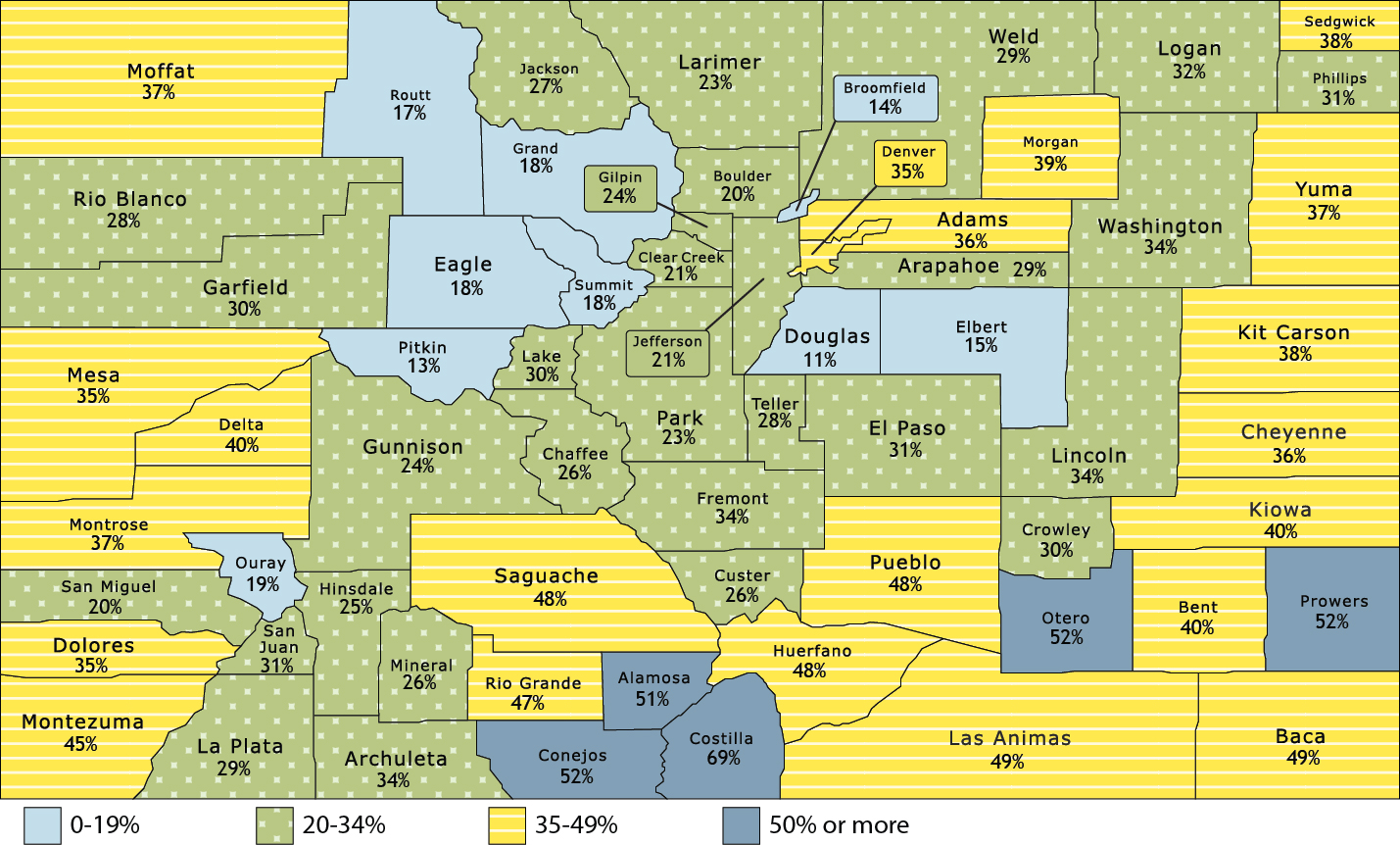
Percentage of Total Population Enrolled in Health First Colorado and Child Health Plan Plus, by County
How we deliver care
Health First Colorado |
Child Health Plan Plus (CHP+) |
Colorado Indigent Care Program |
675,264 Dental Programs |
19,200 Buy-In Programs |
Long-Term Services and Supports (LTSS)
|
Accountable Care CollaborativeThe Accountable Care Collaborative (ACC) is at the core of Health First Colorado. Launched in 2011, it creates Regional Accountable Entities (RAEs) that deliver the programs that will improve member health and reduce costs across the state. Learn more about the ACC. | ||
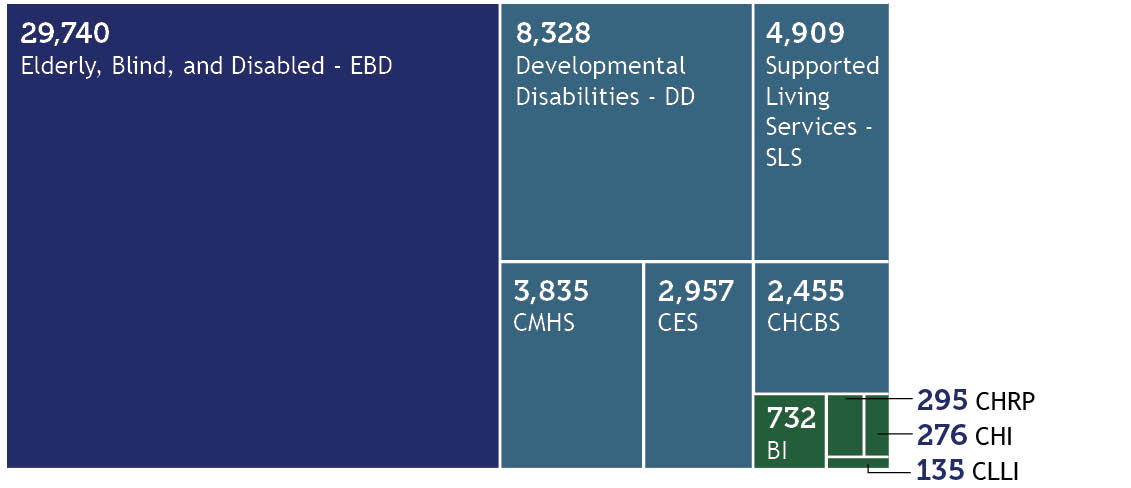
Members Served by Waivers
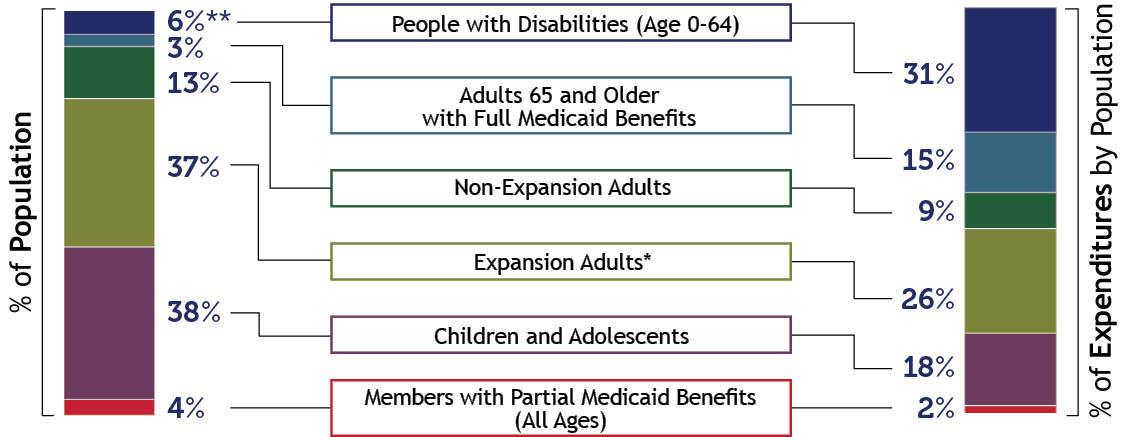
Who is covered and what does it cost?
| In Fiscal Year 2022-23, the Department Paid: |  | Numbers are approximate. Health First Colorado and Child Health Plan Plus expenditures only. |
Patient Protection and Affordable Care Act (ACA) Medicaid Expansion. Due to rounding, percentages may not total 100%. *The majority of funding for Expansion Adults is federal dollars, with the state fund source funded by the Healthcare Affordability and Sustainability Fee. | ||
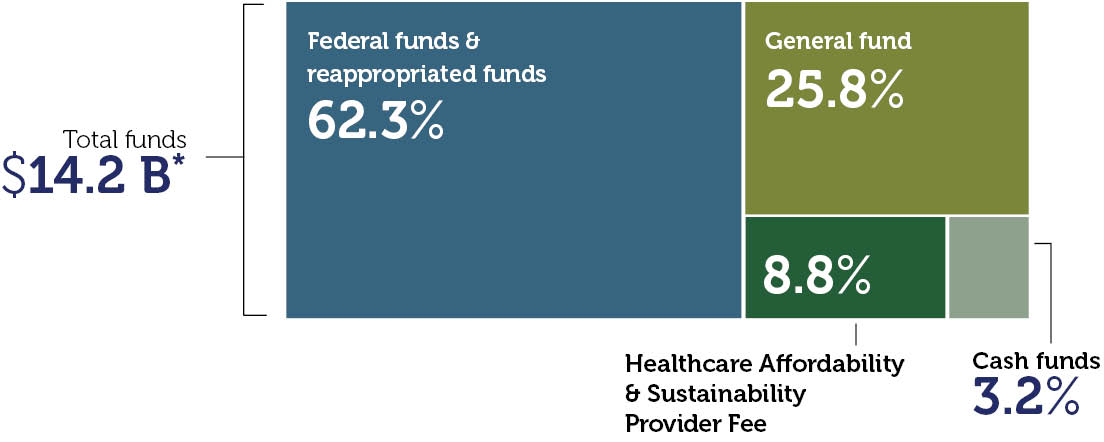
Department Expenditures by Fund
*Includes all services and administrative line items, including Colorado Indigent Care Program and Old Age Pension. Due to rounding, percentages may not total 100%. | ||
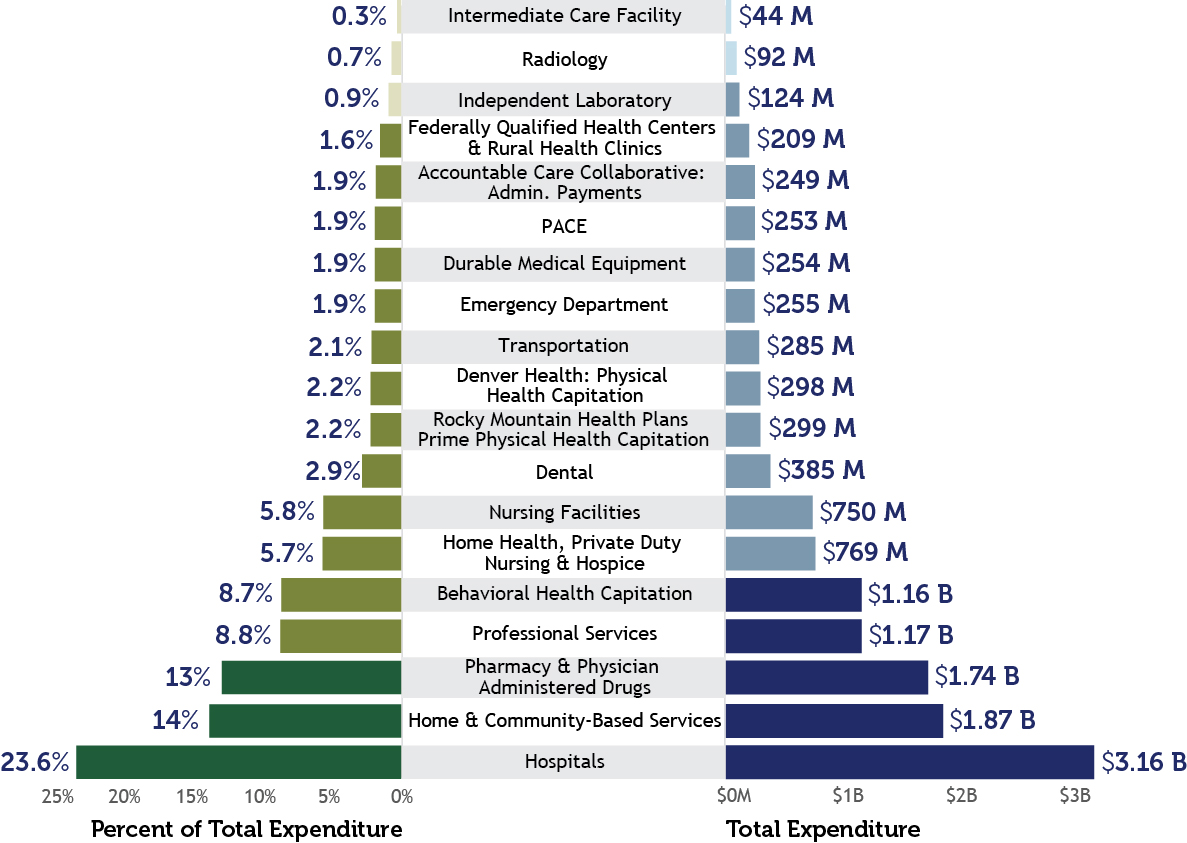
Payment Breakdown to Health First Colorado Partners
This chart refers to medical services cost only, not total Department spending. It is based on claims data by date of service and will differ from data calculated on a cash accounting basis. Due to rounding, percentages may not total 100%. | ||
What we accomplished in FY 2022-23
To support our mission, we focused on several priority areas:
| Transforming home & community-based care We are leveraging $550 million of American Rescue Plan Act (ARPA) federal stimulus funds to implement lasting transformation for older adults and people with disabilities. The initiatives we’ve undertaken will enhance, expand and strengthen home and community-based services (HCBS) in Colorado. We are currently implementing about 60 projects to support recipients of HCBS or people with behavioral health needs, their families, providers, and the health care workforce. Our most recent quarterly reports are available on our website. | Transforming behavioral health Thanks to General Assembly support of transformative legislation, HCPF is closely partnering with the Behavioral Health Administration to expand behavioral health access and services for our members. This includes expanding services, adding residential beds, growing the provider network, improving transparency and reporting, and catalyzing care coordination. To support this work, HCPF increased our investment in behavioral health by more than $600 million since FY 2018-19, now totaling $1.2 billion annually, and has expanded the provider network by adding 2,200 behavioral health providers (an increase of 25%) from April 2021 to March 2023. The Governor’s Budget also has carved out just under $30 million for a comprehensive expansion of services for children and youth with high needs, using the System Care model. |
| Expanding the health care workforce HCPF is part of a multi-agency state effort, with providers, advocates, members, families and workers, to expand and support the health care workforce. The General Assembly approved an additional 3% across the board provider reimbursement rate increase for FY 23-24, as well as a 2% increase in FY 22-23. The General Assembly also approved targeted rate increases to support rural care, care for people with disabilities, and for value-based payment programs and support. HCPF is embracing and encouraging telemedicine, expanding data infrastructure, supporting the existing workforce, and partnering on training, recruitment and career pathway creation, while collaborating with the industry to address violence against health care workers. HCPF is also helping identify geographic differences in the health care workforce. Additionally, HCPF has invested in critical direct care workers who serve our aging and older adults and people with disabilities by increasing the base wage. | Leading on affordability HCPF is working to Save People Money on Health Care, focused on the top two drivers of health care costs: prescription drugs and hospital prices. HCPF submitted our state Canadian drug importation plan, advanced legislation (HB 23-1201) that eliminates the practice of prescription drug “spread pricing” or up-charging of prescription drugs by middlemen insurance carriers and Pharmacy Benefit Managers (PBMs) on individual or group policies, made progress on value-based contracts and payments, and advanced the Prescriber Tool, thereby implementing the affordability recommendations made in our report: Reducing Prescription Drug Costs in Colorado. To make hospital services more affordable, HCPF is partnering with hospitals to make pricing more transparent and make meaningful changes. As part of that effort, HCPF published nationally leading hospital price, cost and profit transparency reports and analyses, supported key policies (HB23-1226 Financial Transparency, SB23-252 Price Transparency, HB23-1243 Community Benefit, SB23-298 Allowing Rural Hospital Cooperation and launched multiple tools to help inform and drive increased hospital transparency and affordability. |
| Committing to health equity HCPF created a robust and comprehensive health equity plan to address health outcomes and disparity indicators in three areas: prevention (which includes COVID vaccinations and many other areas), maternal health, and behavioral health in Health First Colorado and CHP+ programs. As part of this focus, HCPF led a statewide health equity task force of more than 60+ ambassadors, applied sophisticated analytics and insights to track health equity core measures and indicators, as well as required vendors to have health equity plans in their contracts; hosted 20 community town halls with over 2,500 members, providers, and other key stakeholders to inform department priorities and initiatives; and published the 2020 Maternity report (April 2023) highlighting birthing experiences of members, which informed HCPF’s roadmap to improve maternal health care and equity, which covers over 40% of all Colorado births. | Ensuring continuous coverage At the beginning of the COVID-19 pandemic, the federal government declared a public health emergency (PHE), which required states to continue Health First Colorado coverage, even if someone became ineligible. The PHE continued from March 2020 through May 2023. Health First Colorado and CHP+ membership peaked in April 2023 at 1.8 million members, an increase of 550,000 members or 44%, thereby covering 1 in 4 Coloradans, including over 40% of children and over 40% of births. Together we kept the uninsured rate steady at about 6% through the pandemic. With the economy rebounding and the federal PHE over, HCPF is working with partners to help people who are eligible stay covered while supporting those who lose coverage connect to affordable coverage through employer-sponsored, Medicare, or individual coverage through Connect for Health Colorado marketplace. For more information on this important work, visit KeepCOcovered.com. |
| Improving the member and provider service experience The members who participate in our programs are at the center of everything we do. We track several metrics to ensure we’re improving their service experience and collect real-time feedback from our Member Experience Advisory Council. In the past year, both our member and provider call centers answered calls in well under one minute, on average. Eligibility system innovations and automation have driven our automatic approval rate to approximately one-third of all renewals. This means there is no member or eligibility worker activity needed for these approvals. These system innovations have also enabled us to provide “real-time eligibility” for about 80% of eligible renewals, allowing members to receive an eligibility decision in real-time. Recent improvements to our PEAK environment have substantially improved access and member satisfaction, with more enhancements in process. We’ve revised renewal packets based on member and advocate feedback that mirror enhancements made by our SNAP peers to ensure members know they are official state mail and significantly reduce the number of pages. For our providers, claims were processed in less than four days and calls were answered in well under one minute on average. Together, we navigated the 44% membership growth without major operational issues and expanded the Health First Colorado provider network by 26% over the past few years, adding over 21,500 providers, 490 pharmacists (+30%), and 2,220 behavioral health providers (+25%) to increase member access to care. | |
A message from the Executive Director
I am extremely proud of our accomplishments together over the past fiscal year (July 2022-June 2023), which is reflected in this annual report. Thank you for your partnership in another unprecedented year for health care. This past fiscal year, we covered 1.72 million people, or one in four, Coloradans — including more than 40% of Colorado’s children and more than 40% of births in the state.
This annual report shows how we not only grew our provider network to better meet the access needs of members, but also how we invested in health care delivery to improve care quality, service, equity and affordability. We appreciate our partners who worked with us through the year, through the public health emergency and through the COVID-19 pandemic. For more detailed information on what we accomplished together, please see our Performance Plan.
Looking ahead, there is still much work to do in pursuit of our mission and to help Coloradans rise and thrive. We’re focusing our efforts on several key areas in the coming months.
- Keep Coloradans Covered. Now that the COVID-19 public health emergency has ended, all states – including Colorado – were required to return to the regular, annual renewal process for each member of Health First Colorado (Colorado’s Medicaid program) and Child Health Plan Plus (CHP+). To make renewals easier for members, we revamped the renewal process and received authority to discontinue the CHP+ enrollment fee so children who qualify for CHP+ can be auto-enrolled if they no longer qualify for Health First Colorado. We are also working closely with Connect for Health Colorado to improve Coloradans’ awareness of coverage programs and the financial assistance available for those who no longer qualify for our programs. Further, we are working with insurance carriers in the commercial space, while collaborating with Chambers of Commerce and purchasing organizations to help employers understand how they can connect their employees who are being disenrolled from Health First Colorado to employer-sponsored coverage. For more information on this important effort, please visit KeepCOcovered.com.
- Driving affordability and quality care. Amidst the unprecedented growth in membership, we kept Health First Colorado per member per month cost trends to 2% – largely paralleling the respective across-the-board provider reimbursement rate increase – while evolving innovations that drive quality and reduce health disparities to improve the health of our members. Our leadership in prescription drug and hospital affordability will continue to help us manage our own budget (about a third of the state’s overall budget), while helping save Coloradans and employers money on health care.
- To further impact affordability and health equity transformation, we continue to prioritize value-based payments in primary care, maternity care, prescription drugs, behavioral health, and hospital care that reward improved access to high-quality, equitable and affordable care. Because value-based payments reduce disparities and are a benchmark of our Health Equity Plan, we also ensured that health equity plans are now part of each Regional Accountable Entity (RAE) and Managed Care Entity (MCE) contract to reduce disparities. Advances in member care coordination and support, cost and quality indicators, the Prescriber Tool, eConsults, and other innovations will further improve access, quality outcomes, health equity, and overall affordability. Phase II of the Prescriber Tool, sometimes called the Social Health Information Exchange, or SHIE, will connect Health First Colorado members to state programs like the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), payer programs like Regional Accountable Entity prenatal or diabetic supports, and community social determinants of care like food banks, homeless shelters or housing vouchers for those who are food or housing insecure.
- Redesigning the Medicaid delivery system for tomorrow. The Accountable Care Collaborative (ACC) is the Health First Colorado care delivery model, designed to cost-effectively provide access to quality health care services while improving member health. The model in place today, referred to as ACC Phase II, has been in effect since July 1, 2018, and was developed based on substantial stakeholder engagement. HCPF is now in the process of creating the next generation of the ACC, Phase III, which will build on what works well while making improvements to both modernize and address opportunities. The goals of Phase III, which will go into effect July 2025, are to improve quality care for members, close health disparities and promote health equity, improve care access, improve the member and provider service experience, and manage costs to protect member coverage and benefits, as well as provider reimbursements.
Thank you again for your ongoing partnership in transforming health care for the betterment of our members and all Coloradans. I hope you enjoy this annual report.

Kim Bimestefer, Executive Director, HCPF

 Live in a setting they choose with the supports they need
Live in a setting they choose with the supports they need Participate in communities that value their contributions
Participate in communities that value their contributions Access services in a simple, timely and streamlined manner
Access services in a simple, timely and streamlined manner Get the highest quality services
Get the highest quality services