Stabilizing Long-Term Services and Supports (LTSS)
Purpose
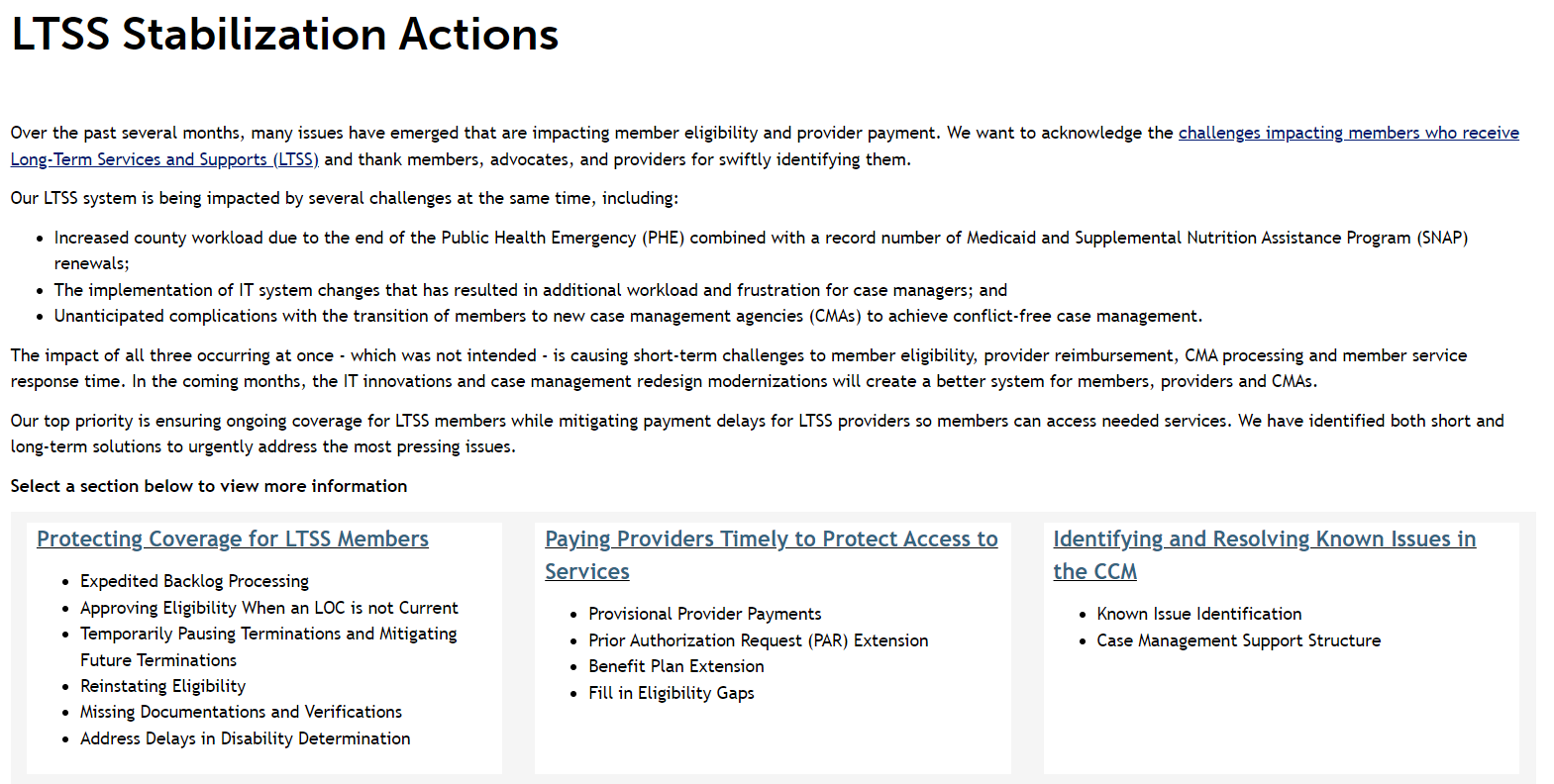
Over the past several months, many issues have emerged that are impacting member eligibility and provider payment. We want to acknowledge the challenges impacting members who receive Long-Term Services and Supports (LTSS) and thank members, advocates, and providers for swiftly identifying them.
Our LTSS system is being impacted by several challenges at the same time, including:
- Increased county workload due to the end of the Public Health Emergency (PHE) combined with a record number of Medicaid and Supplemental Nutrition Assistance Program (SNAP) renewals;
- The implementation of IT system changes that has resulted in additional workload and frustration for case managers; and
- Unanticipated complications with the transition of members to new case management agencies (CMAs) to achieve conflict-free case management.
The impact of all three occurring at once - which was not intended - is causing short-term challenges to member eligibility, provider reimbursement, CMA processing and member service response time. In the coming months, the IT innovations and case management redesign modernizations will create a better system for members, providers and CMAs.
Our top priority is ensuring ongoing coverage for LTSS members while mitigating payment delays for LTSS providers so members can access needed services. We have identified both short and long-term solutions to urgently address the most pressing issues.
Through this process we are working on:
- Protecting Coverage for LTSS Members
- Paying Providers Timely to Protect Access to Services
- Identifying and Resolving Known IT Issues
- Reducing Case Management and County Backlog
- Addressing Appeals and Escalations Backlog
View more information about this work on the LTSS Stabilizing Actions page
Past Communications
LTSS Strategies Joint Meeting
This joint meeting is for leadership staff from case management agencies, county eligibility sites, and disability advocates to meet in partnership with HCPF to discuss current challenges related to the Long-Term Services and Supports (LTSS) Stabilization Efforts. This quarterly meeting offers an opportunity for shared learning, collaboration, and relationship-building across these entities.
Meeting Materials
November 4, 2025
July 31, 2025
April 3, 2025
January 9, 2025
December 12, 2024
November 14, 2024
LTSS Stabilizing Actions
Get information about work that is occurring to address the many issues and challenges impacting members who receive long-term services and supports.
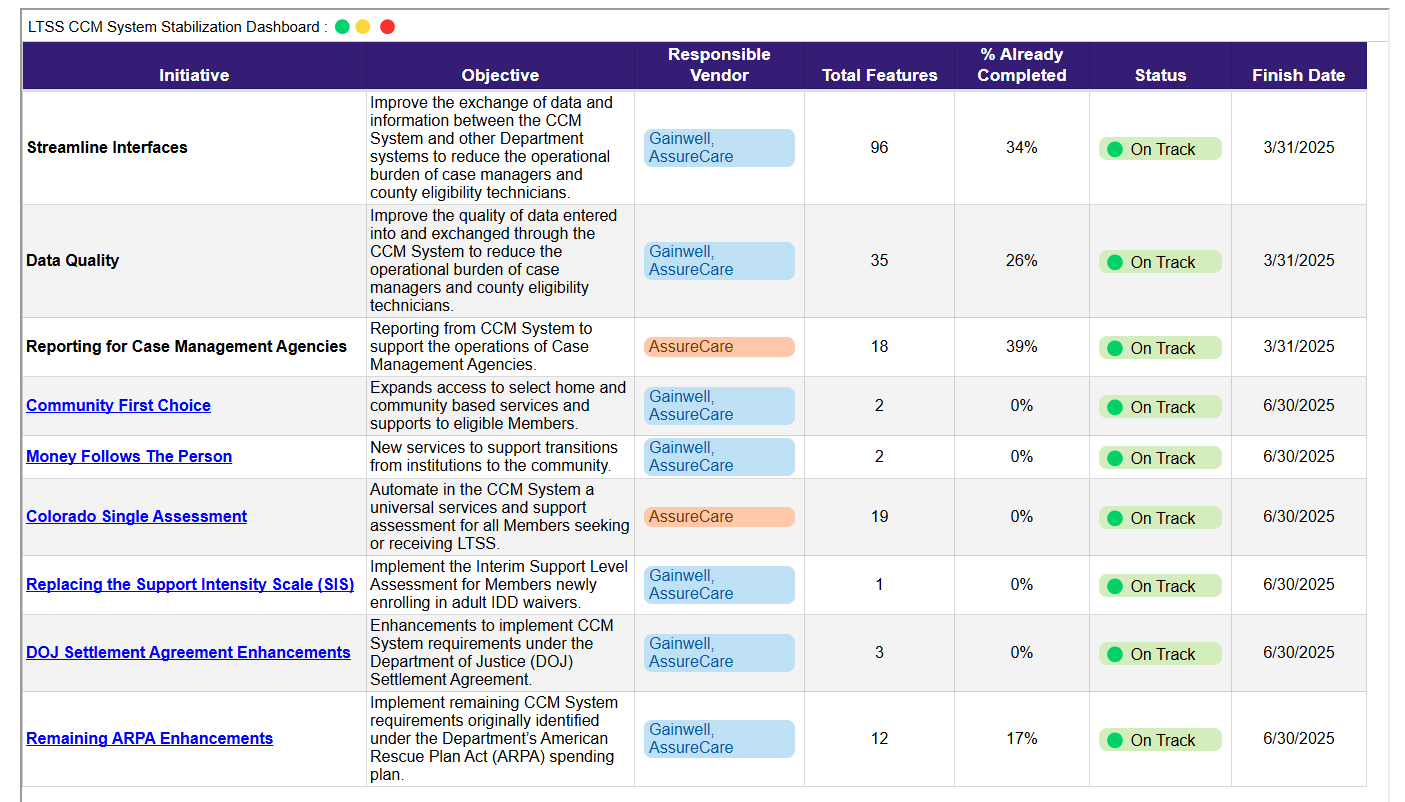
Care and Case Management (CCM) System Stabilization & Enhancement Dashboard
HCPF made significant progress in 2024 to stabilize the CCM System. As work continues, HCPF acknowledges remaining issues across the CCM System in three key areas including Streamlining Interfaces, Data Quality, and Reporting for Case Management Agencies. This dashboard conveys the progress being made toward each of the stabilization areas and key initiatives.
My HCBS Case Management
Members can learn about how changes to the case management system will impact them.
Watch informational videos about LTSS programs and view an interactive map showing the new case management service areas.
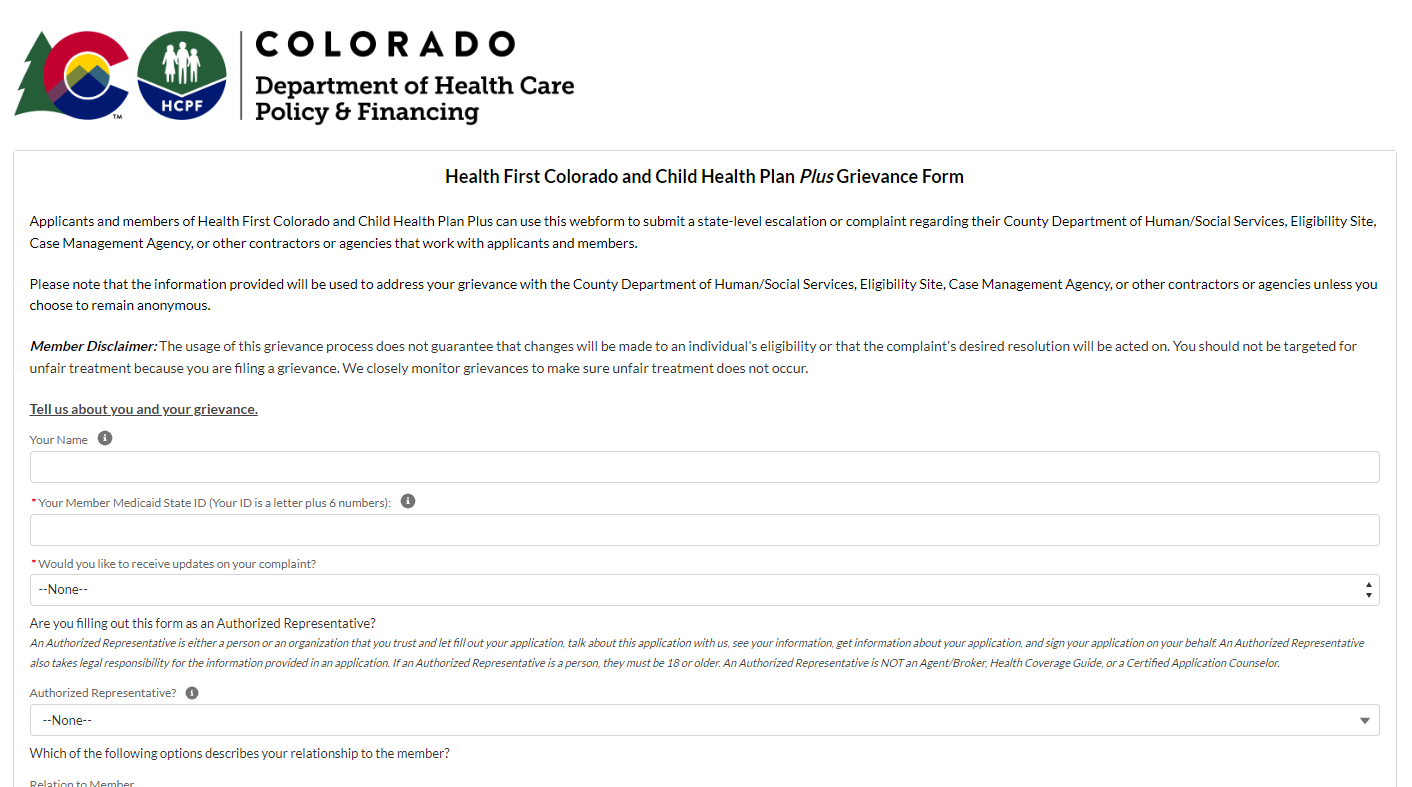
Escalation Form
Case managers can help you as you submit paperwork for your HCBS program to ensure you meet level of care and other requirements, counties help determine if you are eligible based on financial program rules. If you have been working with your case manager or county and are having trouble, you can submit a state-level escalation or complaint regarding issues with County Department of Human/Social Services, Eligibility Site, Case Management Agency, or other contractors or agencies that work with applicants and members.
If an LTSS Member is experiencing issues with their eligibility, use this form to ensure the most prompt resolution.
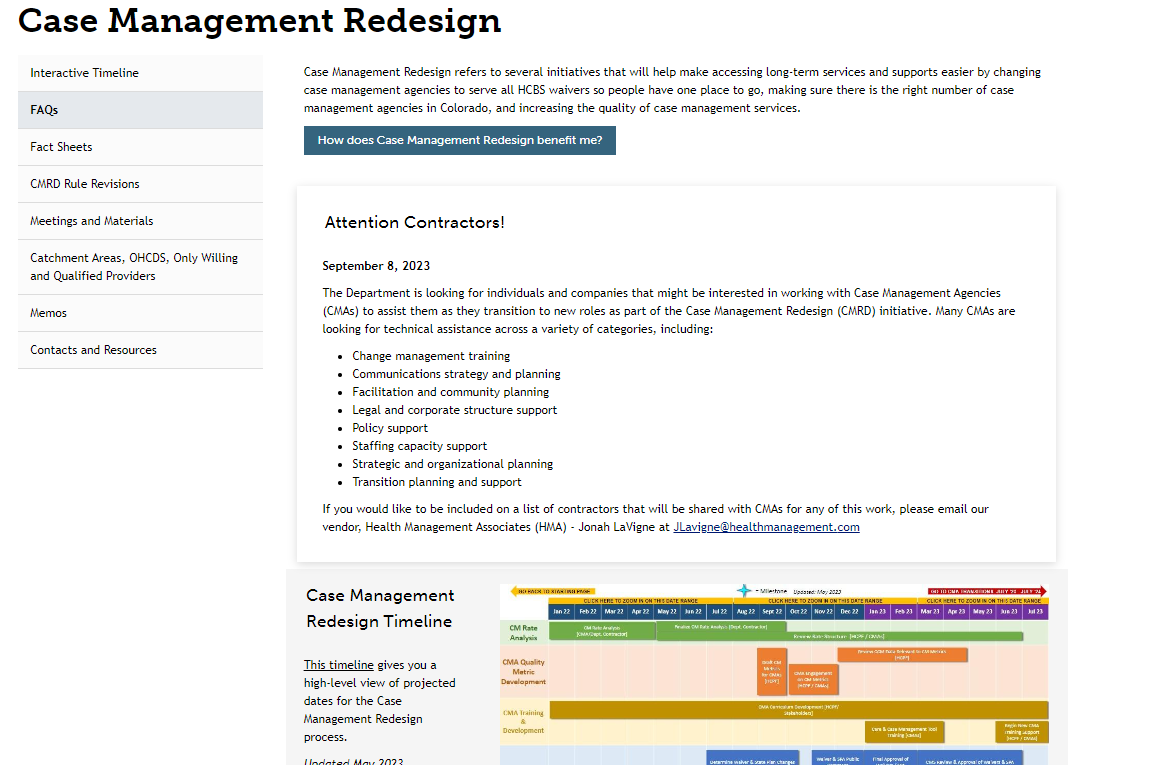
Case Management Redesign
A resource for all stakeholders to learn about the Case Management Redesign (CMRD) initiative.
View an interactive timeline, frequently asked questions, rule revision updates, historical meeting materials and recordings, and an archive of memos about CMRD.
Annual Renewal Process Videos
A series of short informational videos in English and Spanish to provide members with information about the annual renewal process.
Topics include:
- updating your mailing address
- basics of the annual renewal process for Medicaid and CHP+
- transitioning from CHP+ to the health insurance marketplace
Case Management Agency Resources
Case Manager's Corner Newsletters
| 2026 | 2025 |
|---|---|
|
For newsletters older than 2025, please contact hcpf_ccm_stakeholder@state.co.us