Report to the Community
Report to the Community
Fiscal Year 2024-25
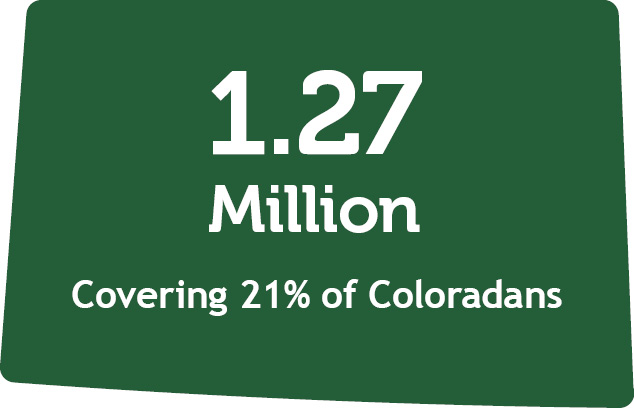
The Colorado Department of Health Care Policy and Financing (HCPF) administers Health First Colorado (Colorado Medicaid), Child Health Plan Plus (CHP+), and other public health care programs for Coloradans who qualify.
Our mission is to improve health care equity, access and outcomes for the people we serve while saving Coloradans money on health care and driving value for Colorado.
Who we serve
Source of enrollment data is Medicaid Management Information System (MMIS). Figures represent average monthly enrollment in Health First Colorado and CHP+ during Fiscal Year 2024-2025.
 |  | ||
 | 
| ||
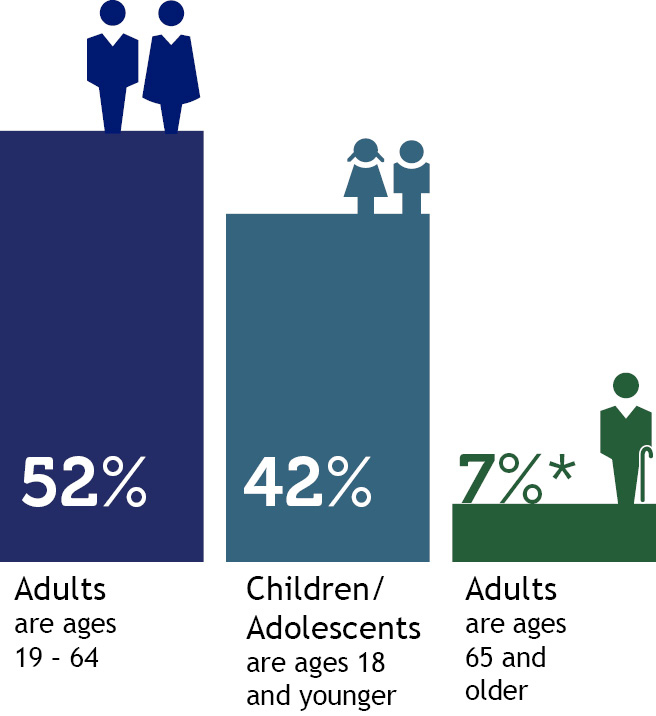 *Adults age 65 and older includes people partially eligible for Health First Colorado. |  | ||
 | |||
Percentage of total population enrolled in Health First Colorado and Child Health Plan Plus, by county
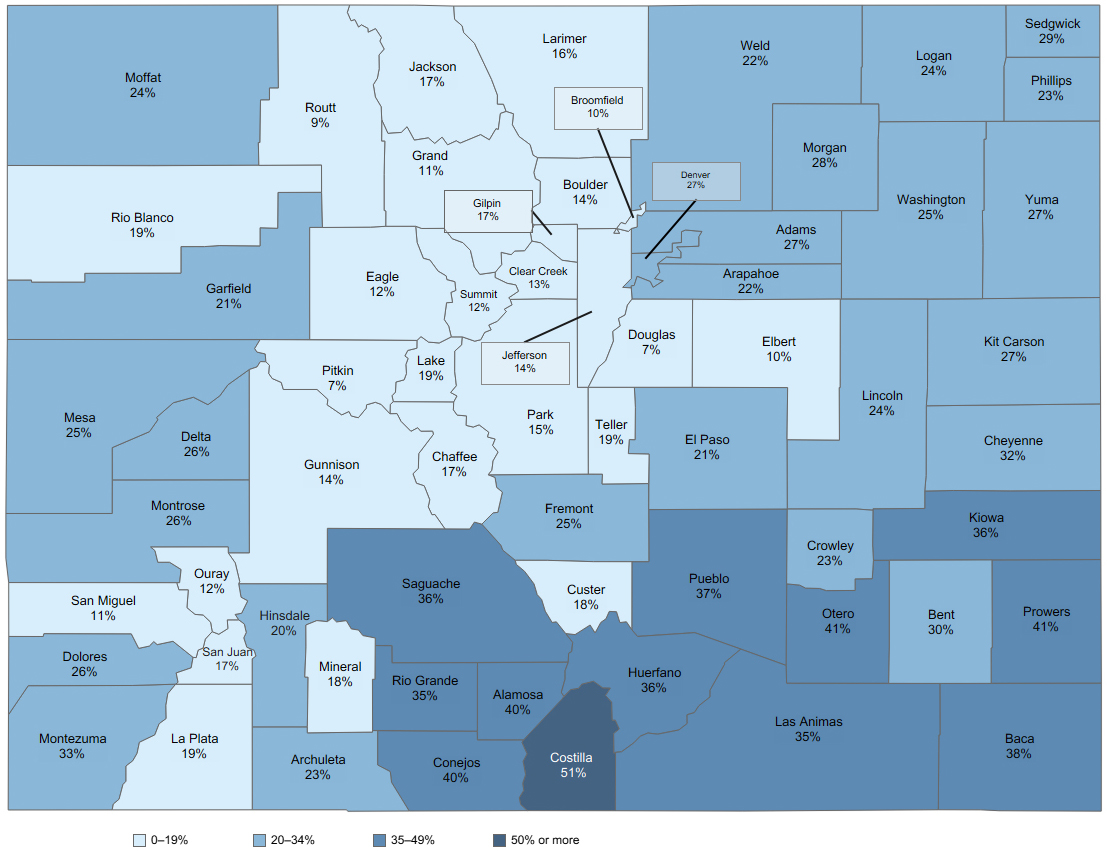
2025 population data as forecasted by the state demographer.
How we deliver care
1.18 M members Health First Colorado (Colorado's Medicaid program) Medicaid provides access to physical and behavioral health care, hospitalization, nursing facility care, prescription drugs, dental care and other benefits. |
88,636 members Child Health Plan Plus (CHP+) CHP+ provides comprehensive health care benefits, including dental care, to uninsured children 18 and younger, and pregnant people who meet income criteria but do not qualify for Health First Colorado. |
67,500 served Colorado Indigent Care Program (CICP) and Hospital Discounted Care Approximately 67,500 Coloradans with incomes up to 250% of the Federal Poverty Level qualified for discounted health care services at CICP participating hospitals, community health centers and clinics, and hospitals that fall under the Hospital Discounted Care law. Hospital Discounted Care sets minimum standards for all hospitals’ financial assistance programs, and eligibility is determined for Hospital Discounted Care and CICP simultaneously. The CICP program ended June 30, 2025. Coloradans can continue to access discounted care through area hospitals subject to the Hospital Discounted Care law. | ||
Accountable Care CollaborativeThe Accountable Care Collaborative (ACC) is at the core of Medicaid. Launched in 2011, it creates Regional Accountable Entities (RAEs) that deliver innovations, programs and supports that improve care access, equity, and care outcomes while better controlling Medicaid cost trends. Learn more about the ACC. |
619,778 served Dental Programs Health First Colorado offers dental benefits to children and adults. In FY 2024-25, Health First Colorado provided dental services to 553,785 Coloradans and CHP+ provided dental care to 65,993 Coloradans. |
26,240 served Buy-In Programs The Health First Colorado Buy-In programs allow members with disabilities to pay a premium for Health First Colorado if they earn too much to qualify, so they don’t have to choose between work and health coverage. Learn more about Buy-In programs for adults and children. | ||
93,294 served Long-Term Services and Supports (LTSS)
| ||||
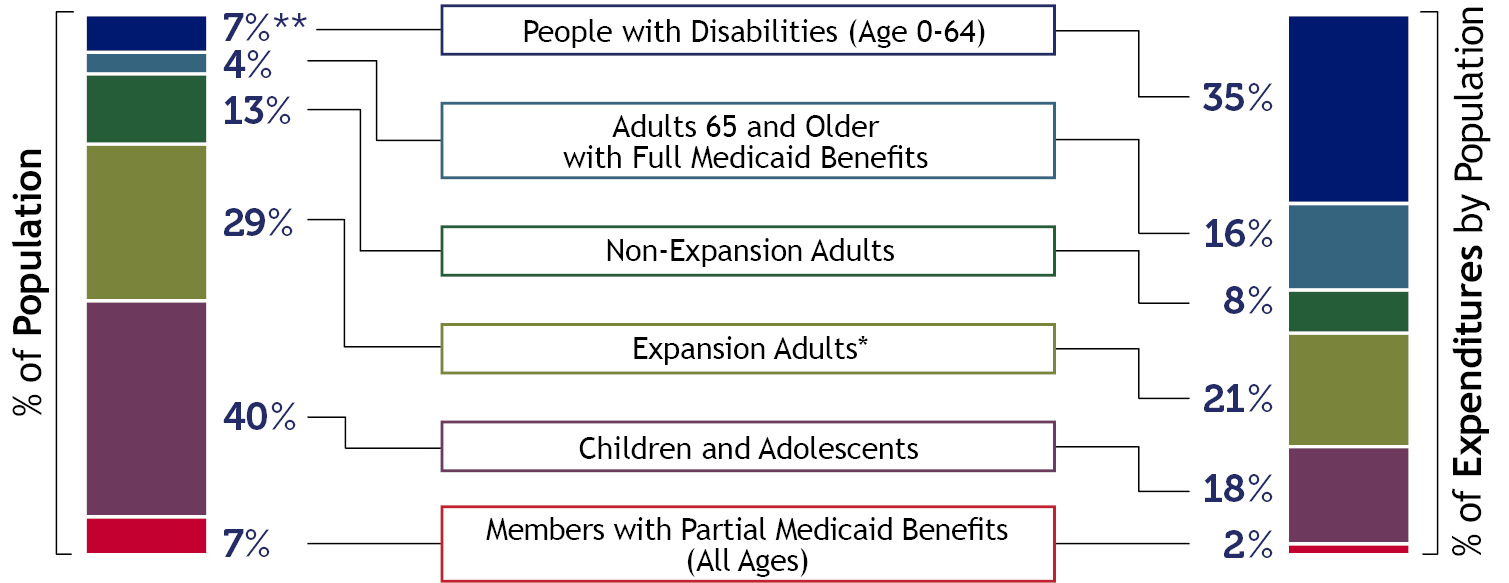
Who is covered and what does it cost?
Patient Protection and Affordable Care Act (ACA) Medicaid Expansion. |
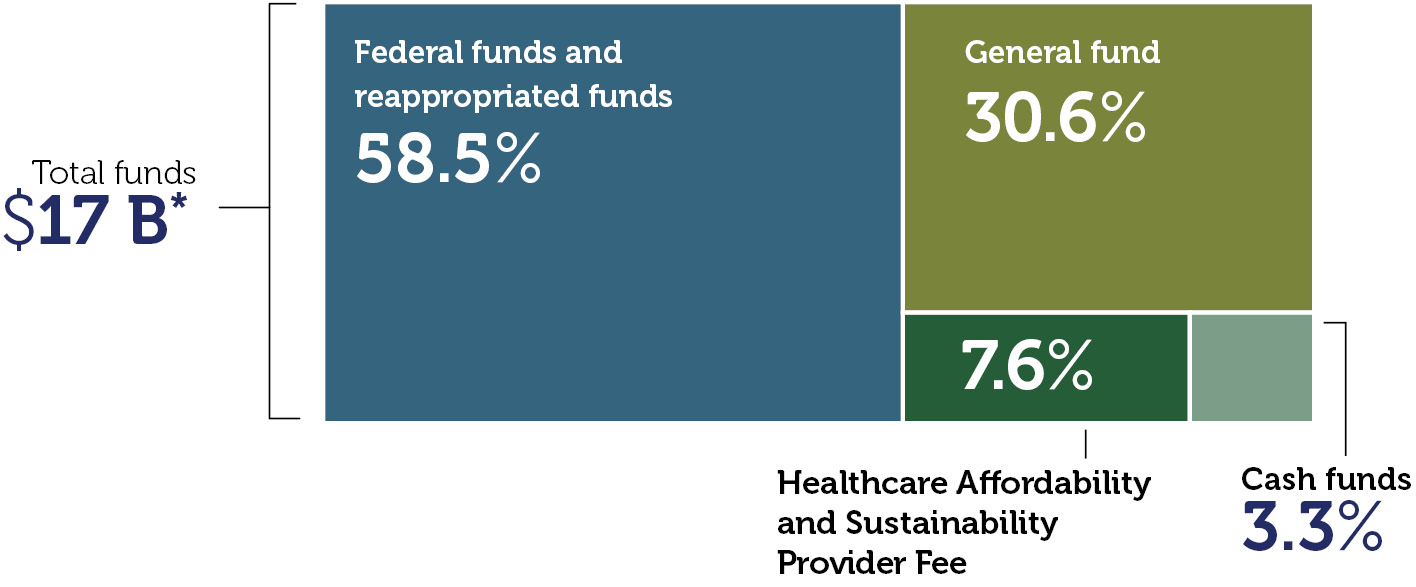
HCPF expenditures by fund
*Includes all services and administrative line items, including Colorado Indigent Care Program and Old Age Pension. |
Payment breakdown to Health First Colorado partners
This chart refers to medical services cost only, not total HCPF spending. It is based on claims data by date of service and will differ from data calculated on a cash accounting basis. Due to rounding, percentages do not total 100%. |
Some of our accomplishments in FY 2024-25
- Completed or on track with 84% of our 99 projects supporting 45 HCPF goals.
- Leveraged $566M one-time ARPA federal funding for long-term and community-based services, rural communities, behavioral health advances.
- Increased federal funding to support health related social needs work and hospitals.
- Launched ACC Phase III to improve Medicaid cost control, quality, access and equity.
- Developed and improved upon the delivery of Intensive Behavioral Health Services.
- Launched Cover All Coloradans, covering 22,000+ children and pregnant Coloradans.
- Improved automation and digitization of eligibility systems.
- Significantly reduced large county call center speed of answer.
- Achieved 95% timeliness for processing new eligibility applications and renewals.
- Completed the Statewide Supportive Housing Expansion Pilot Grant for Medicaid members with a history of chronic homelessness and high system utilization.
- Developed the Colorado System of Care plan to improve community behavioral health access for high acuity children and youth.
- Expanded the number of behavioral health access sites to over 13,000.
- Implemented a Direct Entry Midwife provider type to improve access for members who want to give birth at home or at a freestanding birth center.
- Implemented a new doula benefit, created a Doula Advisory Committee, and provided scholarship money to train new doulas.
- Overhauled Non-Emergent Medical Transportation benefit provider enrollment, credentialing and management processes to better detect and mitigate provider fraud, waste and abuse.
- Created an eConsult program to enable primary care providers to secure consultation from
specialists, increasing care access and improving health outcomes. - Increased provider adoption of the Prescriber Tool to more than 66% of Medicaid providers,
improving affordability and health outcomes, while enhancing the service experience for members and providers. - Redesigned the Recovery Audit Contractor program to reduce improper payments, improve
collections of overpayments, reduce provider administrative burden and improve provider billing education.
A message from the Executive Director
I am pleased to share the fiscal year July 2024 through June 2025 annual report for the Colorado Department of Health Care Policy & Financing (HCPF). We were honored to cover and serve an average of 1.2 million Coloradans at any one time throughout this period, including more than 40% of Colorado’s children and more than 40% of births.
During this past fiscal year, and into this current year, we have continued our focus on several key areas.
- Medicaid sustainability efforts. Controlling Medicaid cost trends is essential to better align our claim expenses with revenues available to cover them, especially given the significant and growing fiscal impacts of H.R. 1. The HCPF Medicaid Sustainability Framework seeks to: organize emerging budget reduction concepts and strategies; thoughtfully navigate Medicaid’s multi-year, fiscal challenges; avoid draconian cuts to our safety net program; and foster alignment, partnership and collaboration in completing this difficult work.
- Leverage ARPA dollars to advance Home and Community-Based Services. In March 2025, HCPF closed out all American Rescue Plan Act (ARPA) Home and Community-Based Services (HCBS) projects, which made historic investments and fueled transformational work across these services that support people with disabilities. Since 2021, HCPF invested a total of $566 million across 61 initiatives aimed at expanding and improving care access, modernizing infrastructure, and strengthening the direct care workforce. Learn more by visiting the ARPA website and accomplishments to review project summaries. Thank you to the more than 12,000 stakeholders who engaged with us on these projects over the past several years. During the current fiscal year, we continue to take actions to stabilize the LTSS ecosystem, including identifying and resolving issues in the new Care and Case Management Tool (CCM), implementing the new single Nurse Assessment Tool, and resolving case management agency backlogs.
- Advance the Medicaid delivery system. The Accountable Care Collaborative (ACC) is the primary delivery system for our Medicaid program. The third phase of the ACC, effective July 1, 2025, included selecting four RAE partners, down from seven, and preparing to implement key advances, including: increasing accountability and transparency; enhancing care and case management and health improvement programs; creating Accountable Care Organization (ACO)-like primary care performance with a special focus on better supporting rural primary care providers and rural health clinics to advance their infrastructure to drive quality of care, affordability and their sustainability; and advancing technology across the board. Designing the ACC Phase III has been a multi-year, stakeholder-informed effort with 135 stakeholder meetings and more than 5,700 attendees over 18 months.
- Build a lasting foundation for behavioral health care. In partnership with the Behavioral Health Administration (BHA), we continue strengthening Colorado’s Behavioral Health Safety Net System. Significant state and federal investments, updated policies, higher reimbursements, new payment models, and strong stakeholder collaboration have significantly expanded access to care, better whole-person care and benefits. Given state fiscal challenges and reductions in federal funding, HCPF has shifted from expanding the system to implementing strategies that curb outlier trends to sustain and protect key enhancements and vital services for Coloradans covered by our programs. We continue working to evolve Medicaid payment models that drive affordability and quality, and implement a system of care for children and youth.
- Drive affordability and outcomes through innovations. We continued to innovate to mitigate cost trends, drive quality and reduce disparities to improve the health of our members. Over 50% of Medicaid payments are in the form of value-based payments across primary care, maternity care, prescription drugs, behavioral health, and hospital care. These advanced payment models reward improved access to high-quality, equitable and affordable care for our members. The Prescriber Tool, eConsults, Providers of Distinction and the Colorado Social Health Information Exchange are innovations that improve affordability and quality outcomes, while making it easier to connect members to the care and supports they need. At the same time, HCPF leverages our health care experts to lead prescription drug and hospital affordability policies, tools and innovations that help save all Coloradans and employers money on health care.
For more on what we accomplished together in this past fiscal year, please see our Performance Plan. Thank you again for your ongoing partnership in transforming health care for the betterment of our members and all Coloradans. I hope you enjoy this annual report.

Kim Bimestefer, Executive Director, HCPF

 Live in a setting they choose with the supports they need
Live in a setting they choose with the supports they need Participate in communities that value their contributions
Participate in communities that value their contributions Access services in a simple, timely and streamlined manner
Access services in a simple, timely and streamlined manner Access needed supports and services
Access needed supports and services