Managed Care Encounters Reporting Guide
- Section 1.0 - Introduction
- Section 2.0 – Terms and Definitions
- Section 3.0 – Submitting Encounters
- Section 4.0 – Reporting Encounter Data
- Section 5.0 - Billing Manuals and Fee Schedules
- Section 6.0 – Department Reporting
- Section 7.0 – Encounter Claims Adjudication
- Section 8.0 – Additional Support
- Managed Care Encounters Reporting Guide Version History
Section 1.0 – Introduction
Purpose
The purpose of the Managed Care Encounter Reporting Guide is to provide a comprehensive program resource and tool kit to support the Department of Health Care Policy & Financing's (the Department) contracted Managed Care Entities' (Regional Accountable Entities [RAEs] and Managed Care Organizations [MCOs]) claims encounter reporting responsibilities.
Scope
The scope of this document includes resources for the Department's contracted Managed Care Entity (MCEs) to support their claims encounter reporting responsibilities. While much of the information provided within may also be applicable to other program entities, such as Dental or Program of All-Inclusive Care for the Elderly (PACE), the document is not currently intended to be comprehensive for these programs; however, future versions will be inclusive of all Department programs. Pharmacy encounter submissions are not covered in this guide. Managed Care enrollment and capitation payments are not covered in this guide. Fee-For-Service (FFS) claims are not covered in this guide. This guide is not intended to be used as a billing manual. This guide is not legally binding and the contracts between the Department and the MCEs take precedence in the case of any discrepancies.
Section 2.0 – Terms and Definitions
Accountable Care Collaborative (ACC) The primary Colorado Medicaid health care service delivery method which seeks to leverage the proven successes of Colorado Medicaid's programs to enhance the Health First Colorado (Colorado's Medicaid program) member and provider experience.
All Payer Claims Database (APCD) - The state's most comprehensive health care claims database representing the majority of covered lives and payers.
Behavioral Health Incentive Payment (BHIP) – To qualify for incentive payments, a RAE must meet the following minimum performance requirements during the contract year: timely submission and completion of a corrective action plan submissions and activities; and timely and accurate submission of monthly encounter data.
Centers for Medicare & Medicaid Services (CMS) – CMS is the federal oversight/partner agency that provides guidance and financial participation to Health First Colorado.
Child Health Plan Plus (CHP+) – CHP+ is public low-cost health insurance for certain children and pregnant women. It is for people who earn too much to qualify for Health First Colorado but not enough to pay for private health insurance.
Coordination of Benefits (COB) – COB is a system which makes sure that the correct party pays first by, 1) cost-avoiding claims where a known other party should be paying or 2) cost-recovering from a claim Health First Colorado paid that should have been paid by someone else.
Elevate Medicaid Choice (EMC) – one (1) of two (2) Managed Care Organizations operating within the ACC program. This closed health care network primarily serves Denver county.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT) – The EPSDT benefit provides comprehensive and preventive health care services for children and youth ages 20 and under including adults who are pregnant, who are enrolled in Health First Colorado.
Electronic Data Interchange (EDI) – EDI is the intercompany communication of business documents in a standard format.
Enhanced Ambulatory Patient Groups (EAPG) – EAPG is a payment grouping system using weight tables the Department uses to reimburse hospitals for outpatient services.
Evaluation and Management (E&M) – E&M is a set of services and procedure codes in which a physician or other qualified healthcare professional diagnoses and treats illness or injury.
Federally Qualified Health Center (FQHC) – FQHC providers are certified by the U.S. Department of Health and Human Services that may be either freestanding or federally defined as "provider based" providing services that must be medically necessary and provided in outpatient settings only. Inpatient hospital stays are not included.
Health First Colorado - Health First Colorado is public health insurance for Coloradans who qualify for Medicaid. Medicaid is funded jointly by the federal government and Colorado state government and is administered by the Department.
Health Insurance Portability and Accountability Act (HIPAA) – HIPAA was signed into federal law in 1996 as Public Law 104-191. One (1) purpose of the law is to protect the portability of health insurance coverage for employees and their families if they change or lose their jobs. Also, part of the legislation collectively known as Administrative Simplification is designed to protect sensitive health care information and reduce the administrative burden of health care for health care providers.
Indian Health Service (IHS) – IHS is an agency within the Department of Health and Human Services responsible for providing federal health services to American Indians and Alaska Natives.
interChange (iC) – The Colorado interChange is the state of Colorado's Medicaid Management Information System (MMIS). The system processes provider enrollments and health care claims, and reimburses providers for Health First Colorado, CHP+, PACE, dental and behavioral health services.
Key Performance Indicator (KPI) – A KPI is a set of metrics developed to measure key performance areas in the work delivered by the RAEs and MCOs.
Managed Care Accuracy Audit Reporting (MCAAR) – A periodic FQHC Data Section and Attestation Statement is required at least quarterly to the Department to confirm complete payment.
Managed Care Entity (MCE) – An MCE enters into a contract to provide services in a managed care delivery system, including but not limited to managed care organizations, prepaid MCEs, primary care case managers and Coordinated Care Organizations.
Managed Care Organization (MCO) - MCOs are integrated entities in the healthcare system, which endeavor to reduce healthcare expenditures costs.
Medicaid Management Information System (MMIS) – The MMIS is a mechanized claims processing and information retrieval system that State Medicaid programs must have to be eligible for Federal funding.
Medically Unlikely Edit (MUE) – The MUE is a set of edits developed by CMS in 2007 to reduce paid claims errors for Medicare claims which specify the maximum units of service that a provider can submit in most circumstances for a client on a single date of service.
National Correct Coding Initiative (NCCI) – policies originally implemented within Medicare in 1996 for claims submitted by physicians.
National Provider Identifier (NPI) – The NPI is a unique identification number for covered health care providers. Covered health care providers and all health plans and health care clearinghouses must use the NPIs in the administrative and financial transactions adopted under HIPAA. The NPI is a 10-position, intelligence-free numeric identifier (10-digit number).
Program for All-Inclusive Care for the Elderly (PACE) – The PACE program provides comprehensive medical and social services to certain frail individuals 55 years of age and older.
Provider Web Portal – The Provider Web Portal is an online tool used by a Provider to enroll with Health First Colorado or CHP+ and to manage provider network and perform claims activities.
Regional Accountable Entity (RAE) – A RAE is an organization in each of the four (4) regions of the State that manages both physical and behavioral health care for the eligible Members in the region.
Rocky Mountain Health Plans Prime (Prime) – One (1) of two (2) Managed Care Organizations operating within the ACC program. This health care network exists within RMHP serving Delta, Garfield, Gunnison, Mesa, Montrose, Ouray, Pitkin, Rio Blanco and San Miguel counties.
Rural Health Clinic (RHC) – provider certified by Medicare located in rural area that are either freestanding or hospital affiliated. RHCs cannot be rehabilitation facilities or facilities primarily for the care and treatment of mental illness.
Secure File Transfer Protocol (SFTP) – The SFTP secure version of file transfer protocol which facilitates data access and data transfer between organizations.
Third Party Liability (TPL) - circumstances when a Health First Colorado Member has health insurance or other potential resources in addition to the Health First Colorado program that may pay for medical services.
Trading Partner - An entity which sends and/or receives electronic health care transactions to/from EDISS. (i.e., provider, billing group, billing service, clearinghouse or payer.)
Technical Report Type 3 (TR3) -The TR3 is a guide for health care electronic data interchange.
Transformed Medicaid Statistical Information System (TMSIS) - a critical data and systems component of the CMS Medicaid and CHIP Business Information Solution (MACBIS).
X12 - a standard for Electronic Data Interchange (EDI) that governs the exchange of business documents (e.g., purchase orders, invoices, healthcare claims, etc.)
Section 3.0 – Submitting Encounters
General Encounter Submission Requirements
All MCEs that provide services to Health First Colorado Members are required to submit encounter data. This includes the RAEs and the MCOs that operate within the ACC program, i.e., EMC and Prime as well as MCEs participating in the CHP+ program. MCEs are required to submit managed care encounter claims once a month at a minimum. Specific program requirements for Medicaid or CHP+ may require more frequent submission.
All managed care encounters are reported to the Department on the appropriate HIPAA 837 X12N transaction for the service being reported. The Department processes the 837 transactions immediately, and a weekly proprietary Encounter Response File is generated and sent back to the reporting entity. MCEs are required to enforce the Department's Payer of Last Resort policy, whereby Medicare or commercial payers should process claims and pay for a covered member's services before the encounter is submitted to the Department. All COB data is required to be submitted on the encounter to the Department, including the COB of the managed care entity itself and any payers that processed the claim prior to the encounter being submitted to the Department.
Electronic Data Interchange (EDI) and X12 Translation
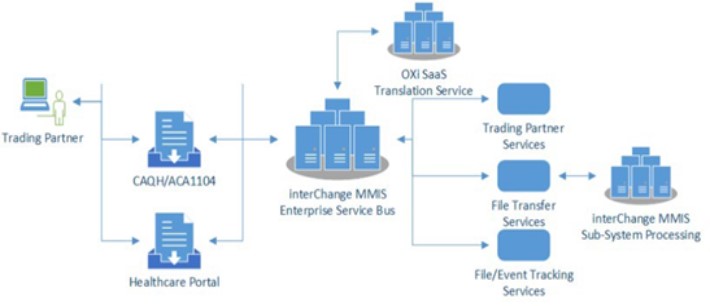
The Electronic Data Interchange (EDI) system in the Colorado interChange interfaces with OXi translation software to translate inbound and outbound HIPAA X12N transaction data between trading partners and the Colorado interChange.
Inbound 837 File Processing
During processing, each submitted file is assigned a file tracking number. As processing continues, the trading partner is validated and the submitted file headers are evaluated. If a failure of the initial validation occurs, file/event tracking table entries are generated, and the file is rejected. For batch files, a TA1 X12 transaction is created and returned to submitting trading partner.
For validated HIPAA X12 transaction files, the process continues to HIPAA X12 Compliance validation, including SNIP Levels 1-4. If a file fails compliance validation, a HIPAA X12 999 (transaction set level errors) and optionally a HIPAA X12 TA1 (interChange header level errors) transaction file indicating validation failure is returned. If a file passes validation, a HIPAA X12 999 transaction file indicating validation success is returned and the file is translated into the iC for claims adjudication.
Encounter Response File
MCEs that submit 837 X12N HIPAA transactions to the Colorado iC will receive a weekly Encounter Response File every Sunday. The Encounter Response File is a proprietary file and is not a HIPAA X12N transaction. The Colorado Proprietary Encounter File Layout is located on the Department's Health Plan Systems SharePoint site under the Resources section.
Trading Partners
An approved trading partner enrollment is required to exchange 837 transactions and receive Encounter Response Report.
- Visit the EDI Support web page for information about Trading Partner enrollment and testing process.
- Trading Partners must complete the testing packet (10 compliant claims) before they can be approved to submit 837 claims into the iC production environment.
Note: Perspective Trading Partners should select ENCOUNTER CLAIMS ONLY option for the "Type of Business" during Trading Partner enrollment.
- Trading Partners that submit 837 transaction files need to review 999 responses to ensure 837 transactions files were accepted.
- For 837 transaction files that are rejected (did not pass compliance) or partially accepted (portion of file passed compliance and portion of file did not pass compliance), Trading Partners need to review 999 responses and correct compliance errors associated with 837 transaction files. There is also a hypertext markup (HTM) file that gets generated that is a readable version of compliance errors.
TR3 and Companion Guides
Trading Partners must build 837 test and production transactions referencing the TR3 and Companion Guides for transactions they are exchanging.
- TR3 Guides can be purchased on the X12 website.
- Visit the EDI Support web page for Colorado Companion Guides.
- Trading Partners building 837 test and production transactions for encounter claims should review Four Key Reminders for Managed Care Entities submitting Encounter claims.
- Once Trading Partner enrollment has passed testing and been approved, providers will need to delegate any approved 837 transactions to the Trading Partner(s) that will be submitting their encounter claims.
- MCEs should refer to the Provider Web Portal Quick Guide - Linking the TPID and Pulling an 835 Quick Guide to do the delegation (made specifically for 835 transactions but applies to any of the transactions).
Note: If a provider wants to change a transaction delegation from one (1)Trading Partner to another, they will first need to remove delegation from existing Trading Partner, then they will be able to delegate transaction to new Trading Partner.
- MCEs should refer to the Provider Web Portal Quick Guide - Linking the TPID and Pulling an 835 Quick Guide to do the delegation (made specifically for 835 transactions but applies to any of the transactions).
SFTP Submission
The Department provides Secure File Transfer Protocol (SFTP) to Health Plans and Trading Partners to allow entities to exchange files with the Colorado IC in a secure format. Refer to the Connectivity Guide located under the Companion Guides and Instructions section of the EDI Support web page for more information about connecting to the Health First Colorado MOVEit SFTP site.
Section 4.0 – Reporting Encounter Data
Managed Care Entity (MCE) Reporting Requirements
Specific encounter data reporting requirements are located in the individual RAE, MCO and CHP+ contracts. Refer to Section 15. DATA, ANALYTICS AND CLAIMS PROCESSING SYSTEMS in the respective contract linked below:
Visit the Health First Colorado Managed Care Contracts web page for RAE, Prime (included in RAE 1) and Elevate Medical Plan Contracts.
The CHP+ contracts are located on the Child Health Plans Plus Managed Care Contracts web page.
Coordination of Benefits (COB)
The Department is expecting to see how the MCE to which the Member is enrolled ultimately paid the claim and whether the MCE was the primary payer, secondary etc. The MCE will be submitted on the encounter transaction with the 'ZZ' claim filing indicator as per the companion guide. When a crossover encounter claim is submitted the Medicare COB should be included in the reported encounter. When a commercial carrier has processed the claim prior to the encounter being submitted, the COB for the commercial carrier should also be reported on the encounter. MCEs and Trading Partners should reference the TR3 and Department Companion Guides for 837 X12N reporting information.
Resubmission Adjustments and Void of Encounter Data
MCEs are required to submit all claims that are paid, denied or adjusted as per contractual agreement. When a claim is submitted that is not considered 'clean', the MCE is expected to make necessary updates or adjustments to the claim and resubmit the claim until is it considered 'clean'. MCEs should resubmit claims as far back as two (2) prior fiscal years from the current fiscal year.
A paid claim can be adjusted or voided. Regardless of whether a claim is being adjusted or voided the original claim is not changed, it is "replaced" by the adjusted/voided claim.
- A void claim is denied, so it cannot be adjusted or voided, once voided a new claim would need to be submitted.
- An adjusted claim can either be paid or denied, if it is denied it cannot be adjusted or voided again, if it is paid then it can be adjusted or voided. A paid claim can only be adjusted once before having to be voided and resubmitted.
- All of the 'mother' and 'child' relationships can be seen in the interChange
Clean Encounter Claim Definition
The Department considers an Encounter claim clean when the claim can be processed in the MMIS without obtaining additional information from the provider of the service or from a third party. A clean Encounter claim may include errors originating in the MCO or Department's claims system. The Department does not expect that an Encounter claim is dispositioned to "PAY" in order for the Encounter claim to be considered "clean".
The following are characteristics of clean Encounter claims:
- Clean Encounter claims are submitted to the MMIS using standard 837 HIPAA X12 transactions.
- Clean Encounter claims are submitted to the MMIS on a post-payment basis, with all information necessary to processes the claim and in accordance with the Department's published filing requirements.
- Clean Encounter claims are filed in a timely manner per contractual agreement with the Department.
- 95% of Encounter claims should be submitted to the Department within 30 days of payment of services by the MCE. 100% of adjudicated Encounter claims should be submitted within 120 days.
- A clean Encounter claim does not require the Department to review on a pre- payment basis, however if medical review is required and all documentation for review is attached or included with the Encounter claim, it is considered 'clean'.
Reporting Denied Services in Encounters
When a Health Plan denies a service, the denial must be reported using the CAS (Claim Adjustment Segment). Within this segment, Health Plans should include the most appropriate Claim Adjustment Reason Code (CARC) and the group code PI (Payor-Initiated Adjustment), along with the corresponding adjustment amount. The group code PI is the required indicator used by interChange, regardless of the specific CARC reported. This information may be reported in either the claim header or service line level.
Services reported with these adjustments will be automatically denied in interChange to ensure consistent alignment of dispositions and reporting between the Health Plan and interChange systems.
Upon processing, Edit 1097 – “Service Denied by Health Plan” will be applied to the affected services and reflected in the encounter response file.
Claims receiving this edit are considered accurate and complete. No resubmission is required as this represents the correct disposition. These denials do not negatively affect accuracy Service Level Agreements (SLAs) and will prevent the claim from receiving additional error codes.
Encounter Resubmission Guidelines
- MCE Denies the Service → Department Denies the Service
- This would not need to be resubmitted, both MCE and Department are denying and in alignment.
- MCE Pays the Service → Department Pays the Service
- This would not need to be resubmitted, both MCE and Department are paying and in alignment.
- MCE Denies the Service → Department Pays the Service
- MCE should review and determine why there is a misalignment of billing policy with the Department; updates made, reprocess and resubmit claims, if needed.
- MCE Pays the Service → Department Denies the Service
- MCE should review and determine why there is a misalignment of billing policy with the Department; updates made, reprocess and resubmit claims, if needed.
If there is a misalignment of billing policy, typically one (1) of the following issues is applicable:
- Service is not being submitted per the billing policy (provider should submit claim per billing policy)
- System is not configured per the billing policy (MCE or Department System configuration update is needed)
- MCE Data is not in sync with iC Data (MCE System Data updates are needed)
- Example: Member Data is not up to date with iC (MCEs ensure 834s processing are up to date)
- Example: Provider Data is not up to date with iC (MCEs ensure All Provider with MCO Affiliation report processing is up to date.)
InterChange User Acceptance Testing (UAT) and Support Process
The Department has made the iC UAT environment available to all MCEs to test 837 X12 and Encounter Response File transactions. When the Department or MCEs make system or billing configuration changes that an MCE would like to test, the MCE can submit a test plan to the Department according to process defined in the HPS UAT Request and Support Processes Guide located on the Health Plan Systems SharePoint site. Look for the iC UAT folder under the Resources section to download the process guide and test plan request form.
Section 5.0 - Billing Manuals and Fee Schedules
Billing Manuals and Guides
The Department provides a comprehensive set of billing manuals for all covered services. The Colorado interChange is configured to adjudicate claims according to the published billing manuals located on the Department's Billing Manual web page. The following list represents some of the billing manuals found on the public website.
General Provider Information Manual
The General Provider Information Manual is designed as a guide for all providers enrolled with Health First Colorado and includes guidance on provider participation and enrollment, reimbursement policies, co-pay, member eligibility, billing information, TPL coordination of benefits, Medicare, timely filing, financial cycles and claims processing.
Appendix T and Universal Services Coding Standards
Appendix T and Universal Services Coding Standards are located on the Accountable Care Collaborative Phase III – Provider and Stakeholder Resource Center web page. These resources support standardized billing of services covered under the Colorado Behavioral Health Program 1915(b)(3) including information about covered diagnoses, covered services, billing guidelines, coding responsibilities and specific claim type instructions.
National Correct Coding Initiative (NCCI)
NCCI policies are based on correct coding conventions defined by the American Medical Association's (AMA) Current Procedural Terminology (CPT) Manual, national and local Medicare policies and editing and standard medical and surgical practice. Visit the Department's NCCI reference web page for information about the purpose, background, general process and methodology related to NCCI.
Child Health Plan Plus (CHP+)
The Department's CHP+ Billing Manual is being developed. A link to the billing manual will be provided here when available.
Fee Schedules and Pricing
Health First Colorado Fee Schedule
The current fee schedule for Health First Colorado is located on the Provider Rates and Fee Schedules web page. This reference provides an index to all the current published fee schedules across the Health First Colorado programs.
CHP+ Fee Schedule
The Department's CHP+ Fee Schedule is located on the Provider Rates and Fee Schedules web page.
Inpatient Pricing
Outpatient Pricing
- Enhanced Ambulatory Patient Groups (EAPG) Pricing
- Federally Qualified Health Center (FQHC), Rural Health Clinic (RHC) Pricing
- Indian Health Services (IHS) Pricing
- Home Health
Medicare Crossover Pricing
- General Billing Manual Medicare Crossover Benefits and Payments
- Colorado Medicaid State Plan Amendment CO-14-0042
Section 6.0 – Department Reporting
Department Use of Encounter Data
- Managed Care encounter data at a service claim level is an integral part of determining managed care capitated rates each year. The Department will be moving to the use of encounter data submitted to the MMIS for rate-setting in the near future to comply with Federal regulations.
- Performance measurement which includes but is not limited to KPI, BHIP, performance pool, etc. rely heavily on Managed Care encounter data to ensure that measurement of Department programs is both complete and accurate.
- Regular reporting on utilization, costs, members and services is highly important to monitor ongoing Department policy and programs. Managed Care encounter data is incorporated into monthly, quarterly, annual reporting as well as multiple dashboard projects utilized throughout the Department.
- Ad hoc, legislative, external data requests often require use of Managed Care encounter data to complete the data request and/or answer the specific need of the requestor.
- Audits at the state and federal level will often require encounter data as part of the official audit request. This includes the Managed Care Accuracy Audit Reporting (MCAAR) for FQHCs.
- Federal reporting requirements and measurement such as those from CMS will frequently require the need for Managed Care encounter data. This includes reporting related to various waivers including the 1915(b) and 1115 waivers.
- Data extracts to Federal and State entities such as All Payer Claims Database (APCD) and Transformed Medicaid Statistical Information System (TMSIS) require reporting of Managed Care encounter data.
Section 7.0 – Encounter Claims Adjudication
Claims Editing and Adjudication
All 837 HIPAA transactions that pass compliance editing are accepted and adjudicated in the Colorado interChange claims subsystem. The managed care encounter adjudication process validates claims data and then evaluates that claims data for alignment with correct coding standards and Department policies. The Colorado interChange is configured to align Federal and State regulations and with the Department's published billing manuals.
CO MMIS Encounter Claims Processing
The Colorado iC processes all claims in a specific order. Validation of critical claims data is completed first, some examples include provider enrollment validation, member eligibility validation, timely filing validation and header reference data validation such as type of bill and diagnosis codes. If the claim passes the initial validation editing without posting an error to deny the claim, the adjudication process continues; the claim is assigned the provider contract and contract billing and reimbursement rules are processed, while concurrently the Member's assignment plans and eligibility are determined, and related coverage rules are processed. If the claim passes the business policy rule processing, the claim services are priced. At this point, any services that are dispositioned to pay are processed against NCCI rules as required, and the claim is audited for duplicate billing or limits against previously adjudicated and paid services. A weekly batch process identifies all Encounter claims that were processed in the last week; the adjudication data, including disposition, pricing and errors, are reported in the Encounter Response File to MCEs.
Appendix R Explanation of Benefits (EOB) List
Refer to Appendix R: Remittance Advice (RA) Messages on the Billing Manual web page for a list of EOB codes that are reported on provider RA.
Validation Editing
Validation editing ensures that the data submitted on the claim is usable for adjudication; is the data found in the system, is the data active in the system, is the data in a valid format? Some examples of validation editing include:
- Does the Member ID exist? If so, is the member eligible for any Benefit Plan on the Date of Service (DOS)?
- Does the Provider ID exist? Can the specific service location be determined? Is the provider enrolled on the DOS?
- Does the diagnosis exist? If so, is the diagnosis code active?
- Is the Type of Bill (TOB) active on the DOS?
- Is the Through Date of Service (TDOS) after the From Date of Service (FDOS)?
The following EOB codes are for common validation edits that the iC system posts and reports. Some EOBs can be associated to multiple error codes within the iC. When an EOB is reported to an MCE, this does not indicate that the claim or service has denied, Encounter claim error codes may be dispositioned to pay or deny.
Date of Service Validation
EOB 1702 - THE ICD SURGICAL PROCEDURE DATE IS NOT WITHIN THE HEADER DATES OF SERVICE. THE PROCEDURE MUST FALL WITHIN THESE DATES. CORRECT THE SURGICAL PROCEDURE/HEADER DATES.
All Institutional Claim Types
Edit 575 - SURGERY DATE CANNOT BE OUTSIDE HEADER FDOS/TDOS
Edit posts at the header.
Resolution for Claim Types O, C, L: Ensure that for all ICD procedures, the date is not prior to the header FDOS and not after the header TDOS.
Resolution for Claim Types I and A: Ensure that the ICD surgical procedure is not more than one (1) day prior to the Header FDOS and not more than one (1) day after the TDOS.
EOB 1920 – THE MEDICAL LEAVE DAYS/NON-COVERED DAYS ARE MISSING OR INVALID. ENTER/CORRECT THE NUMBER OF MEDICAL LEAVE DAYS AND/OR THE NON-COVERED DAYS.
All Claim Types
Edit 313 - MISSING INVALID COVERED-NON-COVERED DAYS
Edit posts at the header.
Resolution: Ensure that the total number of days from the Admit Date to the TDOS is equal to the Total Covered Days + Total Non-Covered Days.
EOB 1930 – THE COVERED/NON-COVERED DAYS ARE MISSING OR INVALID. ENTER /CORRECT THE NUMBER OF COVERED/NON-COVERED DAYS.
Inpatient, Inpatient Crossover and Long-Term Care Claim Types
Edit 570- HEADER TOTAL DAYS LESS THAN COVERED DAYS
Edit posts at the header.
Resolution: Ensure the Total Header Days reported on the claim are not less than the Total Covered Days on the Claim.
EOB 4455 – EAPG-UNITS OF ANCILLARY OBSERVATION REPORTED EXCEEDS 48 HOURS.
Outpatient Claims Only
Edit 4455 – EAPG-OBSERVATION UNIT EXCEEDS 48 HOURS
Edit posts at the detail.
Resolution: observation hours reported cannot be greater than 48 hours.
Type of Bill Validation
EOB 4100 – TYPE OF BILL MISSING OR INVALID
All Institutional Claim Types
Edit 274 – Type of Bill Code Invalid
Edit posts at the header.
Resolution: Ensure the Type of Bill submitted on the claim is valid.
EOB 4100 – ITYPE OF BILL MISSING OR INVALID
All Institutional Claim Types
Edit 801 – Type of Bill/Claim Type Invalid
Edit posts at the header.
Resolution: Ensure the Type of Bill submitted on the claim is valid for the Claim Type.
Provider Data and NPI Validation
EOB 0352 - THE BILLING PROVIDER NUMBER IS NOT ON FILE.
All Claim Types
Edits 1000 and 1004 - BILLING PROVIDER ID NOT ON FILE
Edits posts at the header.
Resolution: Submit a billing provider ID for an enrolled provider.
EOB 0956- NO BILLING PROVIDER LOCATION STATUS FOUND FOR DATE OF SERVICE RANGE. PLEASE MAKE SURE THE BILLING PROVIDER HAS BEEN REVALIDATED AND THAT YOU ARE USING THE CORRECT PROVIDE ID.
All Claim Types
Edit 1956 – NO BILLING PROVIDER LOCATION STATUS FOUND
Edits posts at the Detail.
Resolution: Ensure the provider is currently enrolled.
EOB 1026 - A VALID ENROLLED FACILITY PROVIDER NPI IS REQUIRED.
All Claim Types
Edit 1006 – FACILITY PROV NOT ELIG AT SERV LOC
Edit posts on the detail.
Resolution: Ensure the Service Facility Provider submitted on the claim is enrolled on the FDOS.
EOB 1045 – NPI SUBMITTED IN THE FACILITY ID FIELD IS END DATED FOR DOS BILLED.
All Claim Types
Edit 1082 – NPI for Facility ID End Dated for DOS Billing
Edit posts at the header.
Resolution: submit NPI in the facility ID field that is active on the first date of service billed.
EOB 1046– NPI SUBMITTED IN THE BILLING ID FIELD IS END DATED FOR THE DOS.
All Claim Types
Edit 1084 – NPI for Billing ID End Dated or DOS Billing
Edit posts at the header.
Resolution: Submit NPI in the billing provider ID field that is active on the first date of service billed.
EOB 1112– A NATIONAL PROVIDER IDENTIFIER (NPI) IS REQUIRED FOR THE RENDERING PROVIDER LISTED IN THE HEADER.
All Claim Types
Edit 1811 –Rendering NPI Required
Edit posts at the detail.
Resolution: Provide an NPI for the rendering provider listed./p>
EOB 1208- MULTIPLE SERVICE LOCATION FOUND FOR THE BILLING PROVIDER NPI.
All Claim Types
Edit 1970 – MULTI SVC LOCATIONS – BILLING PROVIDER NPI
Edits posts at the Detail.
Resolution: Submit the Billing Provider NPI along with a unique taxonomy or zip+4. When this error occurs, it can result in the wrong iC provider record being identified and assigned to the claim.
EOB 1210 - THE BILLING PROVIDER NUMBER OR THE NPI ARE MISSING OR IN CONFLICT. VERIFY THE MEDICAID BILLING PROVIDER NUMBER, THE NATIONAL PROVIDER IDENTIFICATION (NPI), THE TAXONOMY CODE, AND THE 9-DIGIT ZIP CODE ARE ENTERED CORRECTLY AND HAVE BEEN REGISTERED.
All Claim Types
Edit 201 - BILLING PROVIDER ID MISSING
Edits posts at the header.
Resolution: Ensure the billing provider's ID or NPI is included and accurate on the claim.
EOB 1345 - SUBMITTED REFERRING PROVIDER NPI IN THE HEADER IS INVALID.
All Claim Types
Edit 1026 – HEADER REFERRING PROVIDER NPI INVALID
Edit posts at the header.
Resolution: Ensure the Referring Provider is enrolled during the service dates on the claim.
EOB 1390 – THE ATTENDING PHYSICIAN NUMBER IS MISSING OR INVALID. ENTER OR VERIFY THE ATTENDING PHYSICIAN’S 10-DIGIT NPI NUMBER.
All Institutional Claim Types
Edit 381 – Attending provider ID missing – HDR
Edit posts at the header.
Resolution: Include attending provider ID when submitting claim types I, A, O, C, L. Does not apply to out of state providers.
EOB 1503 – A RENDERING PROVIDER NUMBER IS REQUIRED.
All Claim Types
Edit 1965–Rendering required and rendering is not present
Edit posts at the detail.
Resolution: Rendering national provider identifier is required when submitting claims electronically.
EOB 1508 - MULTIPLE PROVIDER LOCATIONS WERE FOUND FOR RENDERING PROVIDER. PLEASE SUBMIT NPI WITH TAXONOMY. PLEASE MAKE SURE THAT THE RENDERING PROVIDER HAS BEEN REVALIDATED, THAT THE RENDERING PROVIDER IS AFFILIATED WITH YOUR BILLING GROUP AND THAT YOU ARE USING THE CORRECT RENDERING PROVIDER ID.
All Claim Types
Edit 1972 – Multi service Locations for facility provider NPI.
Edit posts at the header.
Resolution: The system is not able to identify the NPI as a unique NPI, ensure the NPI is unique on the FDOS or submit a unique taxonomy for the rendering provider. When this error occurs, it may result in the wrong rendering provider record being selected and assigned to the claim.
EOB 1958- BILLING PROVIDER INDICATED IS NOT CERTIFIED AS A BILLING PROVIDER.
All Claim Types
Edit 1964 – BILLING PROVIDER NOT DESIGNATED AS A "BILLER"
Edits posts at the Detail.
Resolution: Ensure the provider is enrolled as a Biller.
EOB 2220 – POLICY NOT CURRENTLY ENFORCED – DELTA
All Claim Types
Edit 382 – Attending provider ID missing – DTL
Edit posts at the header.
Resolution: Include attending provider ID when submitting claim types I, A, O, C, L for each detail. Does not apply to out of state providers.
EOB 2220 – POLICY NOT CURRENTLY ENFORCED – DELTA
All Claim Types
Edit 1029 – DETAIL REFERRING PROVIDER NPI INVALID
Edit posts at the detail.
Resolution: Ensure the detail Referring Provider is enrolled during the service dates on the claim.
EOB 2222 - POLICY NOT CURRENTLY ENFORCED.
All Claim Types
Edit 1020 – REFERRRING PROVIDER NUMBER NOT ON FILE
Edit posts at the header.
Resolution: Ensure referring provider NPI matches the referring provider ID on the claim.
EOB 9999 – PROCESSED PER POLICY.
All Claim Types
Edit 1021 – REFERRING NPI INACTIVE
Edit posts on the detail
Resolution: Ensure the referring provider's NPI is active on the first date of service on the claim.
EOB 9999 – PROCESSED PER POLICY.
All Claim Types
Edit 1022 – REFERRING NPI REQUIRED
Edit posts on the header.
Resolution: Include referring provider's NPI on the claim.
Member Validation Edits
EOB 0248 - BIRTH DATE DOES NOT MATCH MEMBER'S STATE ID NUMBER. CORRECT THE BIRTH DATE/STATE ID NUMBER. IF BILLING FOR NEWBORN CARE WITH THE MOTHER’S DOB AND STATE ID NUMBER FOR DAT AFTER 11/30/2003 USE MODIFIER UK. IF BILLING PRIOR TO 11/30/003 USE MODIFIER XN.
All Claim Types
Edit 2008 - CLIENT ID AND DOB MISMATCH
Edit posts at the detail.
Resolution: Ensure the date of birth submitted on the claim matches the client file. If the data in iC is believed to be inaccurate, the member must update their DOB information with CBMS through their PEAK website account or with the appropriate county.
EOB 2500 - THE MEMBER'S STATE ID NUMBER IS NOT ON FILE. ENTER THE CLIENT STATE ID NUMBER AS IT APPEARS ON THE ELIGIBILITY INQUIRY.
All Claim Types
Edit 2001 - CLIENT ID NUMBER NOT ON FILE
Edit posts at the header.
Resolution: Ensure that the member ID submitted on the claim is correct, if the ID is correct, the member is not found in the iC system and is not eligible for services. Providers are required to perform eligibility verification before rendering services. The member should follow up with CBMS if they believe this is error is not reporting correctly.
EOB 2520 – THE DATES OF SERVICE OVERLAP ELIGIBILITY SPAN. MEMBER IS NOT ELIGIBLE ON EACH DATE OF THE SPLAN BILLED ON THE CLAIM. REFER TO THE ELEGIBILITY DATES ON THE ELIBILITY INQUIRY AND SPLIT THE CLAIM.
All Claim Types
Edit 2003 - MEMBER INELIGIBLE ON DTL DOS
Edit posts at the detail.
Resolution: Ensure that the member is eligible on the date that services are rendered. All providers are required to perform eligibility verification on the date that any services are performed, before performing the service.
EOB 3041 – SUBMITTING HMO IS NOT THE ENROLLED HMO OF CLIENT
All Claim Types
Edit 3367 – SUBMITTING HMO IS NOT THE ENROLLED HMO OF CLIENT
Edit posts at the detail.
Resolution: Ensure that the Managed Care Submitter is the Managed Care Plan that the member is enrolled to on the date(s) of service.
EOB 3361 – SERVICE BILLED IS CARVED OUT OF MANAGED CARE AND SHOULD BE BILLED AS FFS
All Claim Types
Edit 3361 – DENY ENCOUNTER FOR SVCS CARVED OUT OF MANAGED CARE
Edit posts at the detail.
When an Encounter does not find a match under the assignment plan rules (AP) and the assignment plan is in Benefit Plan Group Type 2010 (Assignment and OI Plans Configured as Inclusions), post the edit.
OR
When an Encounter finds a match under the assignment plan rules (AP) and the assignment plan is NOT in Benefit Plan Group Type 2010 (Assignment and OI Plans Configured as Inclusions), post the edit.
Along with 3361 some informational edits are posted. Refer to the guidance document below for additional help on informational edits.
Edits 3361 Informational Edits Guidance
Other Edits
EOB 1097 – SERVICE DENIED BY HEALTH PLAN
All Claim Types
Edit 1097 – SERVICE DENIED BY HEALTH PLAN
Edit posts at the detail.
Resolution: Edit will post when an Encounter is submitted with CARC Group Code PI, at the header or detail, regardless of the adjustment group and amount. Edit will not apply to Pharmacy claims.
Section 8.0 – Additional Support
The Department's website is a great resource for MCEs, and important links are included below where information can be found to resolve questions without the need for additional support. Please note that the Health Plans Systems mailbox is not the first tier of support for most reported issues. The references below should help get support needs addressed as quickly as possible.
Trading Partner and EDI Support
Visit the EDI Support web page for Trading Partner Support for setting up new trading partners, accessing the transaction companion guides, setting up new files or to report missing files.
For support with Provider Enrollment, Revalidation or any Provider Web Portal questions:
- Call Us at 1-833-721-0024
- Email: CO.EDW.Support@conduent.com
Eligibility, Enrollment and Capitation Support
Contact the individual listed below or your Program's Department Contract Manager:
| Contract | Benefit Manager | |
|---|---|---|
| ACC RAEs | Matthew Lanphier | Matthew.Lanphier@state.co.us |
| ACC MCOs (DHMC and RMHP Prime) | Tim Gaub | Tim.Gaub@state.co.us |
| PACE | Christopher Gutierrez | Christopher.Gutierrez@state.co.us |
| CHP+ | Christine Martinez | Christine.Martinez@state.co.us |
| Dental (TXIX and CHP+) | Yvonne Castillo | Yvonne.Castillo@state.co.us |
Encounter Claims Processing Support (HCPF_HPSystemSupport@state.co.us)
Before submitting claims questions to the Department please ensure that the claims in question have been reviewed, that they have been submitted according to Department Policy, and that the services billed are covered under the Program that submitted the Encounter claim.
If contacting the Department to escalate an issue that has been reported to the Provider Call Center or with EDI Support, please include the Help Desk Ticket Number so that we can properly follow up with the Medicaid Operations Office and the iC vendor as needed. We will not be able to provide help on EDI or Portal related issues without a ticket number.
Please include your Program's Department Contract Manager on all emails to the Department's Health Plans Systems mailbox.
Managed Care Encounters Reporting Guide Version History
| Version | Description | Version Date |
|---|---|---|
| 1.0 | Version 1.0 Release | 7/1/2021 |
| 2.0 | Version 2.0 Release | 3/30/2023 |
| 3.0 | Version 3.0 Release | 11/24/2025 |