Report to the Community
Report to the Community
Fiscal Year 2021-2022
The Department administers Health First Colorado (Colorado’s Medicaid program), Child Health Plan Plus (CHP+), and other public health care programs for Coloradans who qualify.
Our mission is to improve health care equity, access and outcomes for the people we serve while saving Coloradans money on health care and driving value for Colorado.
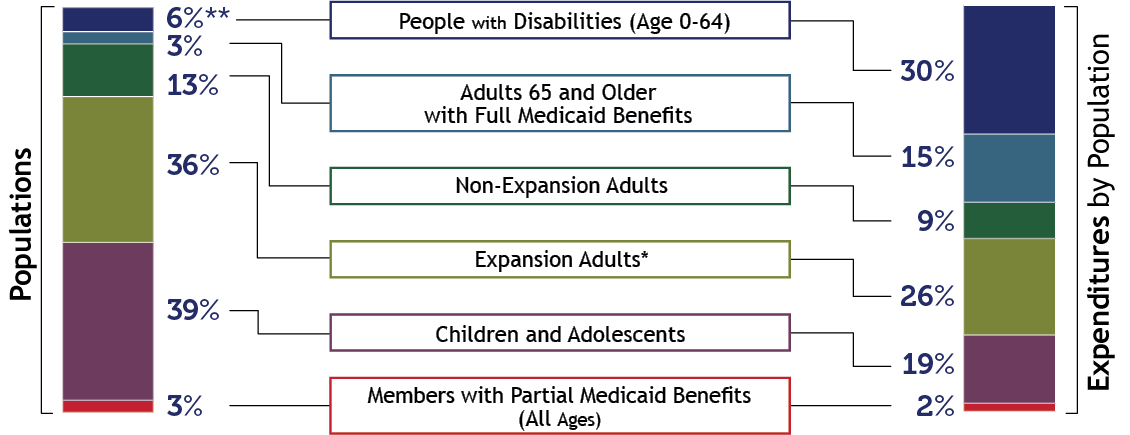
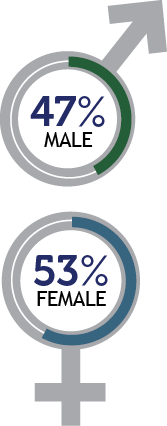
Who we serve
 |
 |
||
 |
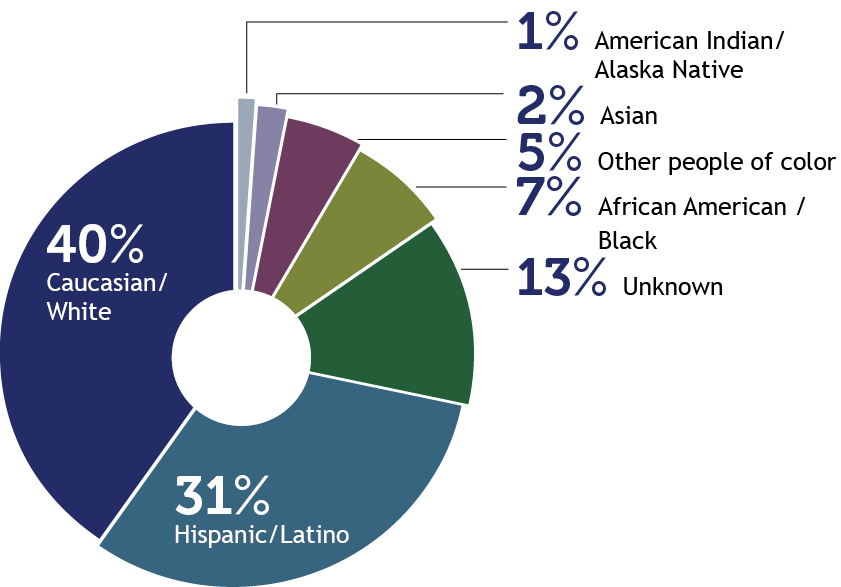 Due to rounding, percentages may not total 100%. Due to rounding, percentages may not total 100%. |
||
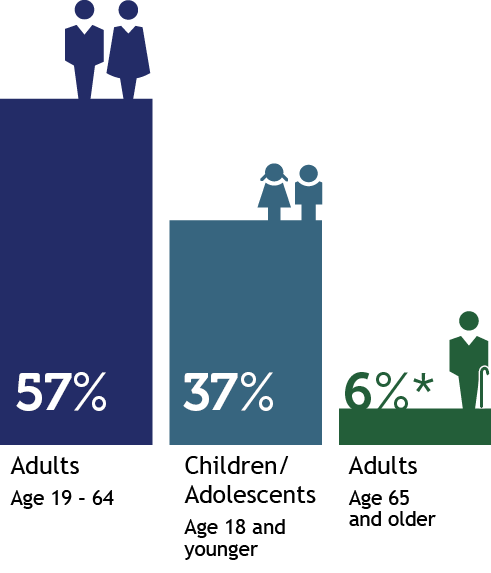 *Adults age 65 and older includes people partially eligible for Health First Colorado. |
 |
||
 |
|||
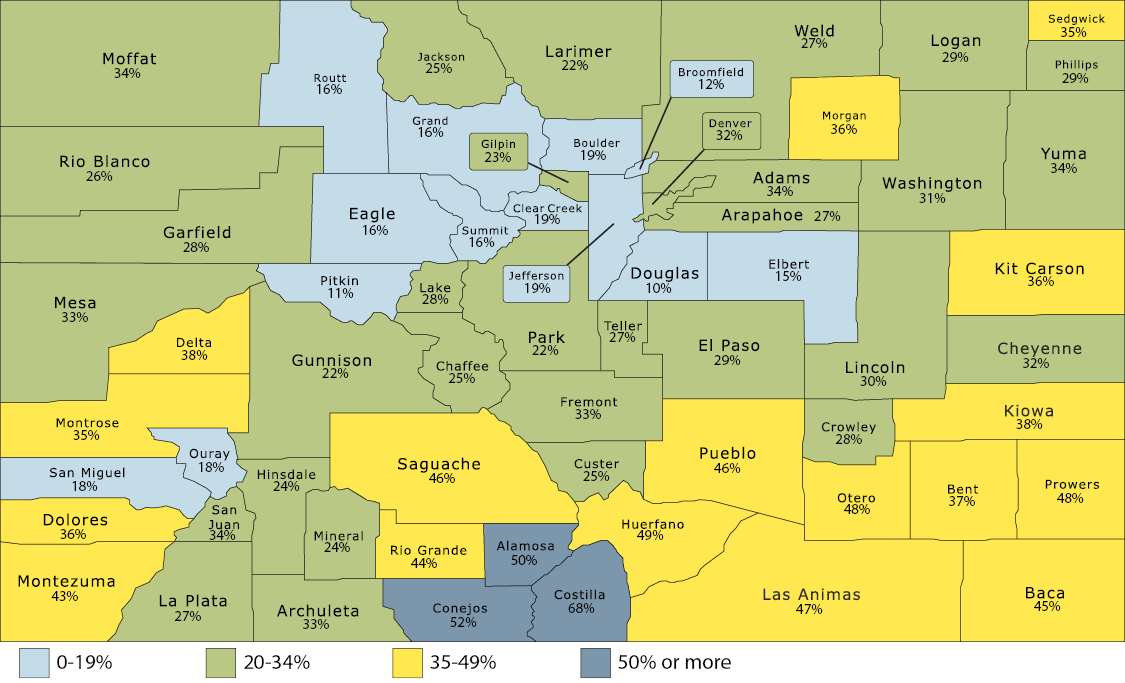
Percentage of Total Population Enrolled in Health First Colorado and Child Health Plan Plus, by County
How we deliver care
|
Health First Colorado |
Child Health Plan Plus (CHP+) |
Colorado Indigent Care Program |
|
511,620 Dental Programs |
15,424 Buy-In Programs |
Long-Term Services & Supports (LTSS)
|
Accountable Care CollaborativeThe Accountable Care Collaborative (ACC) is at the core of Health First Colorado. Launched in 2011, it creates Regional Accountable Entities (RAEs) that deliver the programs that will improve member health and reduce costs across the state. Learn more about the ACC. |
||
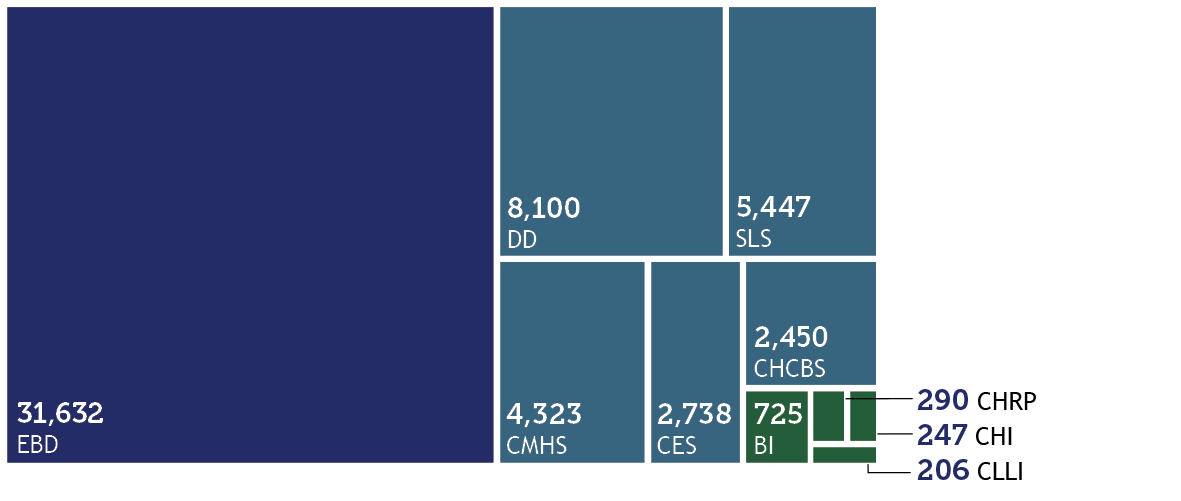
Members Served by Waivers
Who is covered and what does it cost?
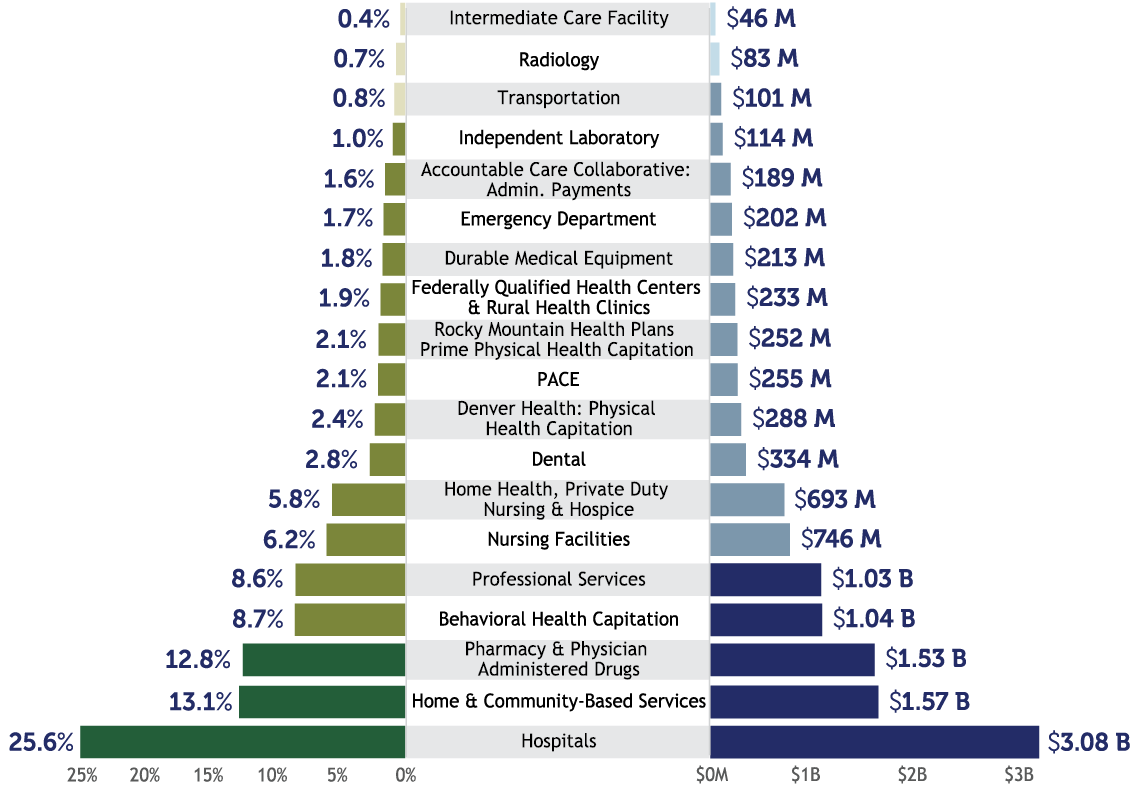
| In Fiscal Year 2021-22, the Department Paid: | 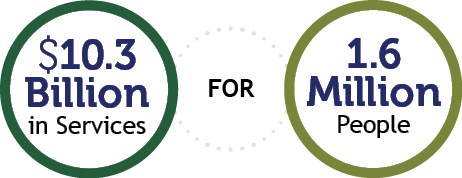 |
Numbers are approximate. Health First Colorado and Child Health Plan Plus expenditures only. |
|
Patient Protection and Affordable Care Act (ACA) Medicaid Expansion. Due to rounding, percentages may not total 100%. *The majority of funding for Expansion Adults is federal dollars, with the state fund source funded by the Healthcare Affordability and Sustainability Fee. |
||
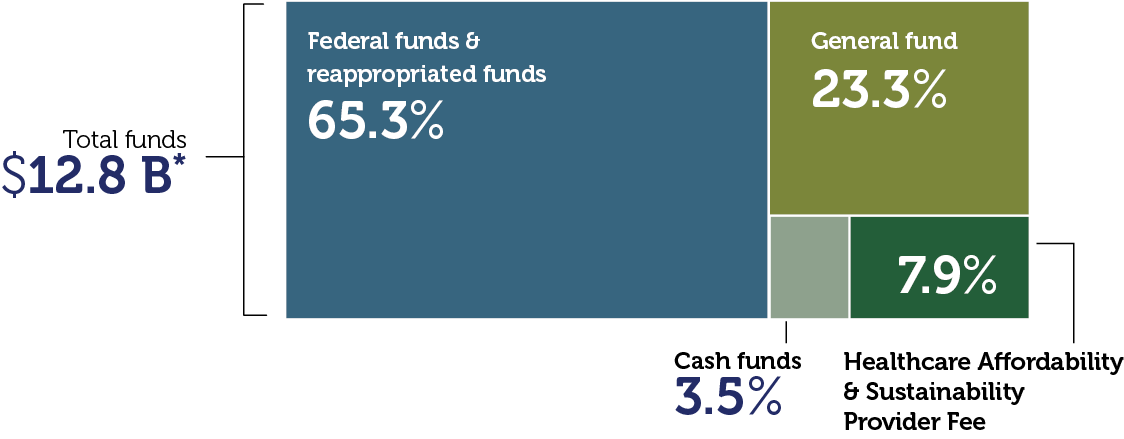
Department Expenditures by Fund
|
*Includes all services and administrative line items, including Colorado Indigent Care Program and Old Age Pension. |
||
Payment Breakdown to Health First Colorado Partners
This chart refers to medical services cost only, not total Department spending. It is based on claims data by date of service and will differ from data calculated on a cash accounting basis. Due to rounding, percentages may not total 100%. |
||
What we accomplished in FY 21-22
To support our mission, we focused on several priority areas:
| Transforming home & community-based care We received state and federal approval to leverage $530 million of American Rescue Plan Act (ARPA) federal stimulus to implement lasting transformation for people with disabilities and long-term care needs. Our initiatives enhance, expand and strengthen home and community-based services (HCBS) in Colorado through the end of 2024. There are currently 63 projects in progress to support recipients of long-term services and supports (LTSS), their families, providers and the health care workforce. Our most recent quarterly reports are available on our website. |
Transforming behavioral health Thanks to General Assembly support of transformative legislation, the Department is partnering with the new Behavioral Health Administration to expand behavioral health services for our members. This includes adding residential beds, expanding the provider network, improving transparency and reporting, and catalyzing care coordination. To support this work, the Department has increased our investment in behavioral health by $400 million since FY 2018-19, now totaling over $1 billion annually, and has expanded the provider network to include 10,300 active behavioral health providers, including 1,000 added from September 2021 through August 2022. |
| Expanding the health care workforce The Department is part of a multi-agency state effort, with providers, advocates, members, families and workers, to expand and support the health care workforce. The General Assembly approved Health First Colorado rate increases for providers and certain health care workers, including a $15/hr minimum for direct care workers and those working in nursing facilities. The Department is investing in telemedicine, expanding data infrastructure, supporting the existing workforce, partnering on training, recruitment, and career pathway creation and helping identify geographic differences in the health care workforce. |
Leading on affordability The Department is working to save people money on health care, focused on the top two drivers of health care costs: prescription drugs and hospital prices. To bring down prescription drug costs, the Department has made progress on value-based contracts and payments, drug importation where federally permitted, and the Prescriber Tool, driving to implement the affordability recommendations in our report: Reducing Prescription Drug Costs in Colorado. To make hospital services more affordable, the Department is partnering with hospitals to recognize where we are outliers in the nation, asking hospitals to make meaningful pricing changes. As part of that effort, the Department published nationally leading hospital price, cost and profit transparency reporting. Value-based payments are being implemented across the spectrum of care — hospital care, primary care, maternity care, behavioral health, prescription drugs and more — to reward quality outcomes and affordability. |
| Committing to health equity We updated our mission in 2021 to highlight our commitment to “improve health care equity, access and outcomes for the people we serve while saving Coloradans money on health care and driving value for Colorado.” While the Department is working hard to apply a health equity lens across all our programs and initiatives, we have identified four initial health disparity areas of focus within Health First Colorado, including: vaccination rates, maternal care, behavioral health and prevention. Read more about this in our first Health Equity Plan. |
Ensuring continuous coverage At the beginning of the COVID-19 pandemic, the federal government declared a public health emergency (PHE) which required states to continue Health First Colorado coverage, even if someone becomes ineligible, among other things. Health First Colorado and CHP+ grew by more than 440,000 members (35%) and now serve 1.69 million Coloradans. That’s 1 in 4 Coloradans. As a result, together, we kept the uninsured rate steady at about 6.6% through the pandemic. With the economy rebounding and the federal PHE expected to end, the Department has a 14-month plan to make sure that people who are eligible stay covered and those who aren’t can find reduced cost coverage on the Connect for Health Colorado marketplace. |
| Improving member & provider experience The members who participate in our programs are at the center of everything we do. We track several metrics to ensure we’re improving their experience and collect real-time feedback from our Member Experience Advisory Council. In the past year, our Member Call Center answered calls in less than 30 seconds on average. Eligibility system innovations and automation have driven our automatic approval rate to approximately 34% for all members renewing. This means there is no member or eligibility worker activity needed for these approvals. These system innovations have also enabled us to process 97% of applications within 45 days. For our providers, claims were processed in less than four days and calls were answered in well under one minute on average through the last half of the year. Together, we have handled the 35% membership growth without any major operational issues and expanded the Health First Colorado provider network by 28% over the past few years, with 96,800 providers now enrolled. |
|
A message from the Executive Director
I am extremely proud of our accomplishments together over the past fiscal year (July 2021-June 2022), which is reflected in this annual report. Thank you for your partnership in another unprecedented year for health care. Together, we successfully served an additional 440,000 Coloradans in need — an increase of 35% — since the start of the pandemic.
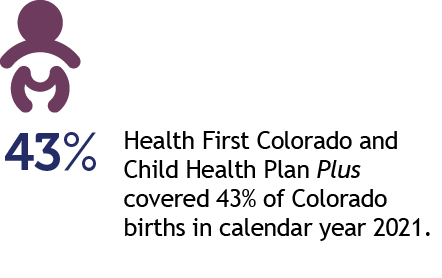
We are covering 1.69 million, or one in four, Coloradans — including more than 40% of Colorado’s children and more than 40% of births in the state.
This support during the pandemic has been a lifeline for Coloradans. Our safety net programs have helped keep Coloradans covered through the COVID-19-induced economic downturn, maintaining a steady 6.6% uninsured rate. This annual report shows how we not only grew our provider network to meet the needs of members, but also how we invested in health care delivery to improve care quality, service, equity and affordability. We appreciate our partners who worked with us through this pandemic. For more detailed information on what we accomplished together, please see our Performance Plan.
Looking ahead, there is still much work to do to help Coloradans thrive. We’re focusing our efforts on several key areas in the coming months.
- Continuity of coverage after the end of the COVID-19 public health emergency (PHE). Once the PHE ends, each member of Health First Colorado and Child Health Plan Plus (CHP+) will need to return to the annual renewal process. Our revamped renewal process will smooth the process for members. Thanks to HB 22-1289, we also waived the CHP+ enrollment fee so children who qualify for CHP+ can auto-enroll if they no longer qualify for Health First Colorado. We are also working closely with Connect for Health Colorado to improve Coloradans’ awareness of coverage programs and the financial assistance available for those who no longer qualify for our programs.
- Driving affordability and quality care. Amidst the unprecedented growth in membership, we kept Health First Colorado cost trends flat while evolving innovations that improve quality, reduce disparities and improve the health of our members. Our leadership in prescription drug and hospital affordability will continue to help us manage our own budget (about 1/3 of the state’s overall budget), while helping save Coloradans and employers money on health care as well.
- To further impact affordability transformation, we continue to prioritize value-based payments in primary care, maternity care, prescription drugs, behavioral health, and hospital care that reward improved access to quality care, health equity and affordability. Value-based payments reduce disparities and are a benchmark of our Health Equity Plan. We also ensured that health equity plans are now part of each Regional Accountable Entity (RAE) and Managed Care Entity (MCE) contract. This important lever is foundational in achieving better health and reduced health care disparities. Advances in member care coordination and support, cost and quality indicators, the Prescriber Tool and other innovations will further improve care access, quality outcomes and overall affordability.
- Life changing opportunities. Current economic conditions are difficult. It’s pivotal that we offer a range of solutions to help people rise and thrive in Colorado. We’re partnering with other state agencies to promote several unique funding opportunities that can help our members thrive. Among the most significant are the Colorado Cash Back Refund, Child Tax Credit and Earned Income Tax Credit and free health care workforce training through Care Forward Colorado. These programs offer life-changing opportunities to help lift up Coloradans.
Thank you again for your ongoing partnership in transforming health care for the betterment of our members and all Coloradans. I hope you enjoy this annual report.

Kim Bimestefer, Executive Director, HCPF

 Live in a setting they choose with the supports they need
Live in a setting they choose with the supports they need Participate in communities that value their contributions
Participate in communities that value their contributions Access services in a simple, timely & streamlined manner
Access services in a simple, timely & streamlined manner Get the highest quality services
Get the highest quality services