Lactation Support Services Billing Manual
The Lactation Support Services benefit program is administered by the Colorado Department of Health Care Policy & Financing (the Department). This billing manual provides information regarding coverage, policy and billing requirements. The information in this manual is subject to change as the Department periodically modifies the Lactation Support Services program’s benefits and services. The manual will be updated as new policies are implemented.
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for general information about Health First Colorado (Colorado’s Medicaid program). The General Provider Information Manual provides information about billing Health First Colorado, reimbursement policies, provider participation, eligibility requirements and other useful information.
- Program Overview
- Provider Qualifications and Enrollment
- Supervision Requirement
- Billing Information
- Third-Party Liability (TPL)
- Covered Lactation Support Services
- Coding Table for Lactation Support Services
- Determining What Time Counts Towards Time Codes
- National Correct Coding Initiative (NCCI)
- Recommendation for Lactation Support Services
- Documentation Requirements
- Physical Health Managed Care
- Outpatient Hospital
- Inpatient Hospital and Freestanding Birth Center Services
- Place of Service Codes
- Contact Information
- CMS 1500 Paper Claim Reference Table
- UB-04 Paper Claim Reference Table
- Timely Filing
- Lactation Support Services Revision Log
Return to Billing Manuals Web Page
Program Overview
On December 1, 2024, the Colorado Department of Health Care Policy and Financing (the Department) implemented a Lactation Support Services benefit for Health First Colorado members. This program is based on legislation HB22-1289.
Rules and Regulations
The Lactation Support Services benefit program is administered by the Department. Rules governing the program are outlined in the Code of Colorado Regulations 10 C.C.R. 2505-10 8.732.7. Providers are required to comply with all rules and guidance provided by the Department and are encouraged to contact the Department’s policy specialists with any questions at HCPF_MaternalChildHealth@state.co.us. Updates to policy and guidance will be published in this manual. Providers will be given notice of updates through the Department’s monthly Provider Bulletin.
This program gives people access to Lactation Support Services, including training and counseling the breastfeeding (or lactating) member about breastfeeding and human lactation. It provides comprehensive, skilled care and evidence-based information for breastfeeding and human lactation.
To be eligible for the program, a member must meet the following criteria:
- Be eligible for Health First Colorado
- Be a pregnant, postpartum or pediatric member who is breastfeeding
Member Eligibility
Before rendering services, the provider should verify the member's eligibility to ensure that the member is eligible for benefits. Providers should retain documentation of the verified eligibility for billing purposes. In order to be eligible for reimbursement for services provided to Child Health Plan Plus (CHP+) members, all CHP+ providers must have an active contract with a CHP+ Managed Care Organization (MCO) and maintain current enrollment in Health First Colorado. Providers should submit claims to the MCO once a CHP+ member is enrolled into an MCO. Refer to the Child Health Plan Plus (CHP+) web page for further guidance.
Back to Top
Provider Qualifications and Enrollment
Providers must be enrolled as Health First Colorado providers to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
Visit the Provider Enrollment web page if interested in becoming a Health First Colorado provider.
Eligible Rendering Providers
Lactation Support Services may only be provided by enrolled individual providers with training in advanced lactation support. Providers may not bill for services provided by un-enrolled providers, such as supervised interns or persons undergoing training to become a Certified Lactation Educator (CLE), Certified Lactation Counselor (CLC), or International Board-Certified Lactation Consultant (IBCLC).
The following enrolled provider types (PT) may provide Lactation Support Services:
- International Board-Certified Lactation Consultant (IBCLC) – PT 70
- Certified Lactation Counselor (CLC) - PT 71
- Certified Lactation Educator (CLE) - PT 71
The following enrolled provider types (PT) may provide Lactation Support Services if it is within their scope of practice according to state licensing requirements and laws and the provider has training in advanced lactation support:
- Certified Professional Midwife (CPM)/Direct Entry Midwife (DEM) - PT 69
- Certified Midwife (CM) - PT 80
- Certified Nurse Midwife (CNM) - PT 22
- Licensed Physician (MD) – PT 05
- Licensed Osteopath (DO) - PT 26
- Licensed Physician Assistant (PA) – PT 39
- Licensed Advanced Practice Nurse (APN) – PT 41
- Licensed Registered Nurse (RN) – PT 24 (enrolled as a Non-Physician Practitioner-Individual)
- Certified Registered Nurse Anesthetist (CRNA) – PT 40
- Occupational Therapist (OT) – PT 28
- Speech Therapist (SLP) – PT 27
Providers who are currently enrolled with the Department as one of the provider types listed above may render Lactation Support Services under their existing provider enrollment.
Providers must maintain an active lactation certification and submit documentation of current certification through the Provider Web Portal. Acceptable certifications include the following:
- Certified International Board-Certified Lactation Consultant (IBCLC) with current certification by the International Board of Lactation Consultant Examiners (IBLCE)
- Certified Lactation Counselor (CLC) with current certification by the Academy of Lactation Policy and Practice, Inc. (ALPP)
- Certified Lactation Educator (CLE) with current certification by the Childbirth and Postpartum Professional Association (CAPPA).
Eligible Billing Providers
Facility Provider Types
The only facility provider type that may bill for Lactation Support Services is:
- Supply – PT 14
Supply (PT 14)
When claims are submitted using a supplier as the billing provider, the rendering provider’s National Provider Identifier (NPI) listed on the claim must be the individual provider who rendered the service. The rendering provider does not need to be formally affiliated with the group in order for the claim to be processed.
Group Provider Types
The only group provider types that may bill for Lactation Support Services are:
- Federally Qualified Health Center (FQHC) – PT 32
- Rural Health Clinic (RHC) – PT 45
- Indian Health Services (IHS) – PT 61
- Clinic – PT 16
- Non-Physician Practitioner Group – PT 25
- Lactation/Doula Professional Group – PT 72
Federally Qualified Health Centers and Rural Health Clinics (PT 32 and 45)
Refer to the Federally Qualified Health Center (FQHC)/Rural Health Clinic (RHC) billing manual for details regarding billing Lactation Support Services in an FQHC/RHC setting. Lactation Support Services provided by an employee at an FQHC/RHC site are billed as part of the encounter rate for the FQHC/RHC and may result in a payment when delivered by a provider included in the FQHC/RHC visit definition (10 CCR 8.700 & 8.740). Lactation Support Services are not billed separately on professional claim forms (CMS 1500). Lactation Support Services provided by an employee at an FQHC/RHC site that are not included in the FQHC/RHC visit definition should be included in the FQHC/RHC cost report.
Lactation support service providers who provide Lactation Support Services at a FQHC or RHC but are not employed by the FQHC/RHC can bill for services separately on a professional claim form (CMS 1500) and use the applicable Place of Service codes. These claims are reimbursed at the Health First Colorado Fee Schedule rate.
Indian Health Services (PT 61)
Refer to the Indian Health Services (IHS) billing manual for details regarding billing Lactation Support Services in an outpatient setting. Lactation Support Services provided at an IHS site are billed per encounter as part of the all-inclusive rate. They are not billed separately on professional claim forms (CMS 1500).
Back to Top
Clinics and Non-Physician Practitioner Groups (PT 16 and 25)
When claims are submitted using Clinics and Non-Physician Practitioner Groups as the billing provider, the rendering provider’s National Provider Identifier (NPI) listed on the claim must be the individual provider who rendered the service. The rendering provider must be formally affiliated with the group in order for the claim to be processed.
Lactation/Doula Professional Groups (PT 72)
When claims are submitted using the Lactation/Doula Professional Group as the billing provider, the rendering provider’s NPI listed on the claim must be the individual provider who rendered the service. The rendering provider must be formally affiliated with the group in order for the claim to be processed.
A Lactation/Doula Professional Group consists of any of the following professionals who are enrolled with the Department as approved providers:
- International Board-Certified Lactation Consultant (IBCLC) – PT 70
- Certified Lactation Counselor – PT 71
- Certified Lactation Educator – PT 71
- Doula – PT 79
This billing provider type must have at least one (1) IBCLC or Doula affiliated with the group.
Individual Billing Providers
Individual providers may choose to be their own billing provider for Lactation Support Services. The following list of providers can have billing status when enrolling with Health First Colorado:
- International Board-Certified Lactation Consultant (IBCLC) – PT 70
- Certified Midwife (CM) – PT 80
- Certified Nurse Midwife (CNM) – PT 22
- Licensed Physician (MD) – PT 05
- Licensed Osteopath (DO) - PT 26
- Licensed Advanced Practice Nurse (APN) – PT 41
- Certified Registered Nurse Anesthetist (CRNA) – PT 40
- Occupational Therapist (OT) – PT 28
- Speech Therapist (SLP) – PT 27
Doula-Lactation Cross-Billing
Enrolled Doula providers who meet IBCLC, CLC or CLE qualifications per 10 C.C.R. 2505-10 8.732.9 may provide lactation support without separate PT 70 or 71 enrollment.
Doula providers are required to submit a copy of their current lactation certification to the Department for verification prior to rendering or billing for Lactation Support Services.
Enrolled doula providers are required to submit a copy of their current certification through the Provider Web Portal as one of the following:
- International Board-Certified Lactation Consultant (IBCLC) with current certification by the International Board of Lactation Consultant Examiners (IBLCE)
- Certified Lactation Counselor (CLC) with current certification by the Academy of Lactation Policy and Practice, Inc. (ALPP)
- Certified Lactation Educator (CLE) with current certification by the Childbirth and Postpartum Professional Association (CAPPA)
This verification process ensures compliance with program standards and protects continued access to reimbursement. Providers who do not complete this step will be subject to enforcement actions in accordance with Section 25.5-4-301, C.R.S., and 10 C.C.R. 2505-10, Section 8.076.
Enrolled Lactation Support Service providers (IBCLC, CLC, or CLE) who meet doula qualifications per 10 C.C.R. 2505-10 8.734.4 may provide doula services without separate provider type 79 enrollment. Refer to the Doula billing manual for further guidance.
Supervision Requirements
International Board-Certified Lactation Consultants (IBCLCs) with current certification by the International Board of Lactation Consultant Examiners (IBLCE) may provide Lactation Support Services without supervision.
Certified Lactation Counselors (CLCs) with current certification by the Academy of Lactation Policy and Practice, Inc. (ALPP) and Certified Lactation Educators (CLEs) with current certification by the Childbirth and Postpartum Professional Association (CAPPA) may only provide Lactation Support Services under the general supervision of enrolled:
- Physicians (MDs) – PT 05/65
- Osteopaths (DOs) – PT 26
- Physician Assistants (PAs) – PT 39
- Advanced Practice Nurses (APNs) - PT 41
- Certified Nurse Midwives (CNMs) – PT 22
- International-Board Certified Lactation Consultants (IBCLCs) – PT 70
A Certified Lactation Counselor (CLC)/Certified Lactation Educator (CLE) may render services but does not bill directly. Claims must be submitted through the enrolled group. Claims must identify the CLC/CLE with their NPI number as the rendering provider.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for general information.
Third-Party Liability (TPL)
The term Third-Party Liability (TPL) describes circumstances when a Health First Colorado member has health insurance or other potential resources - in addition to the Health First Colorado program - that may pay for medical services.
An estimated 10% of Health First Colorado members have other health insurance resources available to pay for medical expenses.
While most benefits require a process by which Medicaid would be the payer of last resort because Federal regulations require that all available health insurance benefits be used before Health First Colorado considers payment, Third Party Liability (TPL) edits will be automatically bypassed for both commercial insurance and Medicare when claims are submitted by the following provider types:
- PT 70 - Lactation Consultant
- PT 72 - Lactation/Doula Professional Group
- PT 79 – Doula
For more information on TPL, please visit the general provider billing manual section that discusses these rules in greater depth.
Covered Lactation Support Services
Lactation Support Services are billed using a single Healthcare Common Procedure Coding System (HCPCS) procedure code (S9443), one (1) of two (2) modifier codes indicating individual (U1) or group settings (U2) and one (1) of eight (8) modifier codes (U3, U4, U5, U6, U7, U8, U9, UA) to indicate the number of minutes spent providing direct contact services to the member. Add an additional modifier code if services are delivered via telemedicine (FQ, FR, 93, 95), as shown in the tables below. Refer to the current Fee Schedule for rates
Prior authorization requests are not required. There are no amount, duration or scope limitations for the Lactation Support Services benefit.
Appropriate diagnosis codes must be utilized when billing for Lactation Support Services (e.g., Z39.1: encounter for care and examination of a lactating mother, O92.70: unspecified disorders of lactation). If billing a claim for a breastfeeding child, use a child lactation-related code (e.g., R63.31: pediatric feeding difficulty, P92.5: neonatal feeding difficulties at breast).
Services for the lactating member and child must be billed on one (1) claim. Both the lactating member and the breastfeeding child must not have claims submitted for the same service and the same date of service. The provider should bill the claim under the eligible member for whom the visit was scheduled, or most closely aligns with the provider’s scope of practice. For example, a pediatrician would bill under the Health First Colorado enrolled breastfeeding child, and an obstetrician would bill under the Health First Colorado enrolled lactating member.
When billing for Lactation Support Services for twins, multiple infants or tandem breastfeeding, providers have two options:
- Bill for extended time spent with the lactating member; OR
- Bill separately for time spent with each breastfeeding child. Providers will need to ensure to bill for distinct and separate identifiable amounts of time for each pediatric member.
A lactation support provider who renders services to more than one (1) member at a time must bill appropriately using the approved group session modifier U2. The group session must be an instructor-led breastfeeding education group. Not all participants in the group need to be members of Health First Colorado, but a claim for payment may only be submitted for each enrolled Health First Colorado member who received services in the group session. Such claims must be coded using S9443 with the U2 modifier.
Coding Table for Lactation Support Services
| Procedure Code | Description | First Position Modifier | second position Modifier |
|---|---|---|---|
| S9443 | Lactation Support Services
Telemedicine service delivery is allowed. | U1 = individual session
U2 = group session | U3 = 8-22 minutes U4 = 23-37 minutes U5 = 38-52 minutes U6 = 53-67 minutes U7 = 68-82 minutes U8 = 83-97 minutes U9 = 98-112 minutes UA = 113-127 minutes |
Example: A member received a total of 90 minutes of individual in-person Lactation Support Services on a given date of service. The provider should report S9443 with the U1 modifier to indicate individual setting and the U8 modifier to indicate 90 minutes of direct member contact services provided.
Important Notes on S9443
Although the formal definition of HCPCS procedure code S9443 is “Lactation classes, non-physician provider, per session,” the Department instructs providers to use this procedure code under the direction detailed in this billing manual. Key differences are:
- This procedure code should be reported for Lactation Support Services by any eligible provider, including physicians, rather than just “non-physicians.”
| Modifier Codes for Telemedicine Service Delivery for S9443 | Description |
|---|---|
| FQ | The service was furnished using audio-only communication technology. |
| FR | The supervising practitioner was present through two-way audio/video communication technology. |
| 93 | Synchronous telemedicine service was rendered via telephone or other real-time interactive audio-only telecommunications system. |
| 95 | Synchronous telemedicine service was rendered via real-time interactive audio and video telecommunications system. |
Determining What Time Counts Towards Timed Codes
Providers report the code for the time spent in direct member treatment. Pre- and post-delivery services are not to be counted in determining the treatment service time. In other words, the time counted as "intra-service care" begins when the lactation provider is directly working with the member to deliver treatment services. Record-keeping documentation and travel time is not reimbursable. Time spent for preparation, report writing, processing of claims, or documentation regarding billing or service provision is not reimbursable.
National Correct Coding Initiative (NCCI)
When multiple services, including lactation support, are provided during a single visit, providers should not bill for overlapping time spent on different activities. Each billed procedure code must correspond to a distinct and separately identifiable amount of time and work for each service. For example, if during a visit both preventive medicine services and Lactation Support Services are provided, the provider may bill each code only if the time spent on each is separately identifiable and does not overlap.
NCCI Procedure-To-Procedure (PTP) and Medically Unlikely Edits (MUE) may apply to certain combinations of procedure codes. Visit the Centers for Medicare & Medicaid Services (CMS) NCCI web page for a complete list of impacted codes, guidance on bypass modifier uses, and general information.
Back to Top
Recommendation for Lactation Support Services
Lactation Support Services are provided as preventative services and require a recommendation by a physician or other licensed practitioner of the healing arts acting within their scope of practice in accordance with 42 CFR 440.130(c).
- The lactating individual-child dyad requires a recommendation on file from a physician or other licensed practitioner of the healing arts. This recommendation authorizes Lactation Support Services from pregnancy through the duration of breastfeeding. The recommendation can come from the licensed healthcare provider of either the lactating individual or the child.
- All claims for Lactation Support Services must have the NPI number of the enrolled provider who recommended the items to be indicated on the claim in the appropriate Ordering, Prescribing and Referring (OPR) field on the claim. The enrolled provider types who may recommend these services are:
- Physician – PT 05/65
- Osteopath – PT 26
- Physician Assistant – PT 39
- Advanced Practice Nurse – PT 41
- Nurse Midwife – PT 22
- Certified Midwife (CM) – PT 80
- Certified Professional Midwife (CPM)/Direct Entry Midwife (DEM) - PT 69
- Non-Physician Practitioner-Individual – PT 24
- The recommending provider indicated on the claim must be actively enrolled with Health First Colorado (42 CFR 455.410(b)). The claim will be denied if the indicated provider is not actively enrolled. Reference the Ordering, Prescribing, and Referring Claim Project Identifier for further details.
- If a licensed provider listed in this manual renders a service under their own ordering authority, then that rendering licensed provider's NPI number should be placed in the applicable OPR field on the claim. This does not apply to providers enrolled as IBCLC, CLC and CLEs.
Professional Claims
- Paper claims use field 17.b.
- Electronic submissions use loop 2420 with qualifier DK (Ordering), DN (Referring) or DQ (Supervising).
- Claims submitted through the Provider Web Portal use the “Referring Provider” field.
Institutional Claims
- The Attending Provider field (#76) or the Other ID fields (#78 or #79) for both paper and electronic claims.
- Providers may refer to their applicable UB-04 billing manuals for guidance on how each field is used.
Documentation Requirements
The provider must maintain documentation in accordance with 10 CCR 2505-10 8.130.2 that complies with state and federal regulations. The provider must retain records that specifically record the dates and precise times at which direct services provided to a member began and ended, among other general requirements for documentation. These timestamps are critical for validating the second position modifier billed.
Physical Health Managed Care
Lactation Support Services are not included in Health First Colorado physical health managed care plans. Lactation Support Services are still covered benefits for members enrolled in those plans as “wrap-around” benefits of the plan.
All claims for Lactation Support Services should be billed to the Department’s Fiscal Agent, Gainwell Technologies, even if the member is attributed to a Health First Colorado physical health managed care plan.
Outpatient Hospital
Lactation Support Services provided at an Outpatient Hospital are reported on the institutional claim type and are reimbursed as part of the hospital's EAPG payment.
Inpatient Hospital and Freestanding Birth Center Services
Professional services provided by a Lactation Support Services provider associated with newborn deliveries and immediate postnatal breastfeeding support care for the lactating individual are part of the hospital’s facility All Patient Refined-Diagnosis Related Group (APR-DRG) payment and the Freestanding Birth Center’s delivery payment. Such circumstances are not eligible for billing through the Lactation Support Services benefit. Place of Service codes 21 (Inpatient Hospital) and 25 (Freestanding Birth Center) are not available for billing use. HCPCS codes for Lactation Support Services cannot be billed for dates on or during the date span of the delivery and inpatient stay. Refer to the Obstetrical Care Billing Manual.
Place of Service Coding
Providers may provide Lactation Support Services in a variety of settings, including the member’s home, clinics, provider offices or via telehealth. The visit setting should be indicated on the claim using the Place of Service code. A full list of allowable places of service for Lactation Support Services is indicated below.
Lactation Support Services can be provided via telemedicine with Place of Service codes 02 or 10. Telehealth services must adhere to the Telemedicine Billing Manual.
Official descriptors of the Place of Service can be found on the Centers for Medicare and Medicaid Services (CMS) website.
The following Place of Service codes are allowed:
| Allowed Place of Service Code | Description (short) |
|---|---|
| 02 | Telehealth Provided Other than in Patient’s Home |
| 04 | Homeless Shelter |
| 10 | Telehealth Provided in Patient’s Home |
| 11 | Office |
| 12 | Home |
| 15 | Mobile Unit |
| 19 | Off Campus-Outpatient Hospital |
| 20 | Urgent Care Facility |
| 22 | On Campus-Outpatient Hospital |
| 49 | Independent Clinic |
| 50 | Federally Qualified Health Center |
| 71 | Public Health Clinic |
| 72 | Rural Health Clinic |
Contact Information
Contact the Provider Services Call Center with billing inquiries.
Contact the Department’s Lactation Support Services policy specialist at HCPF_MaternalChildHealth@state.co.us for all other inquiries.
Back to Top
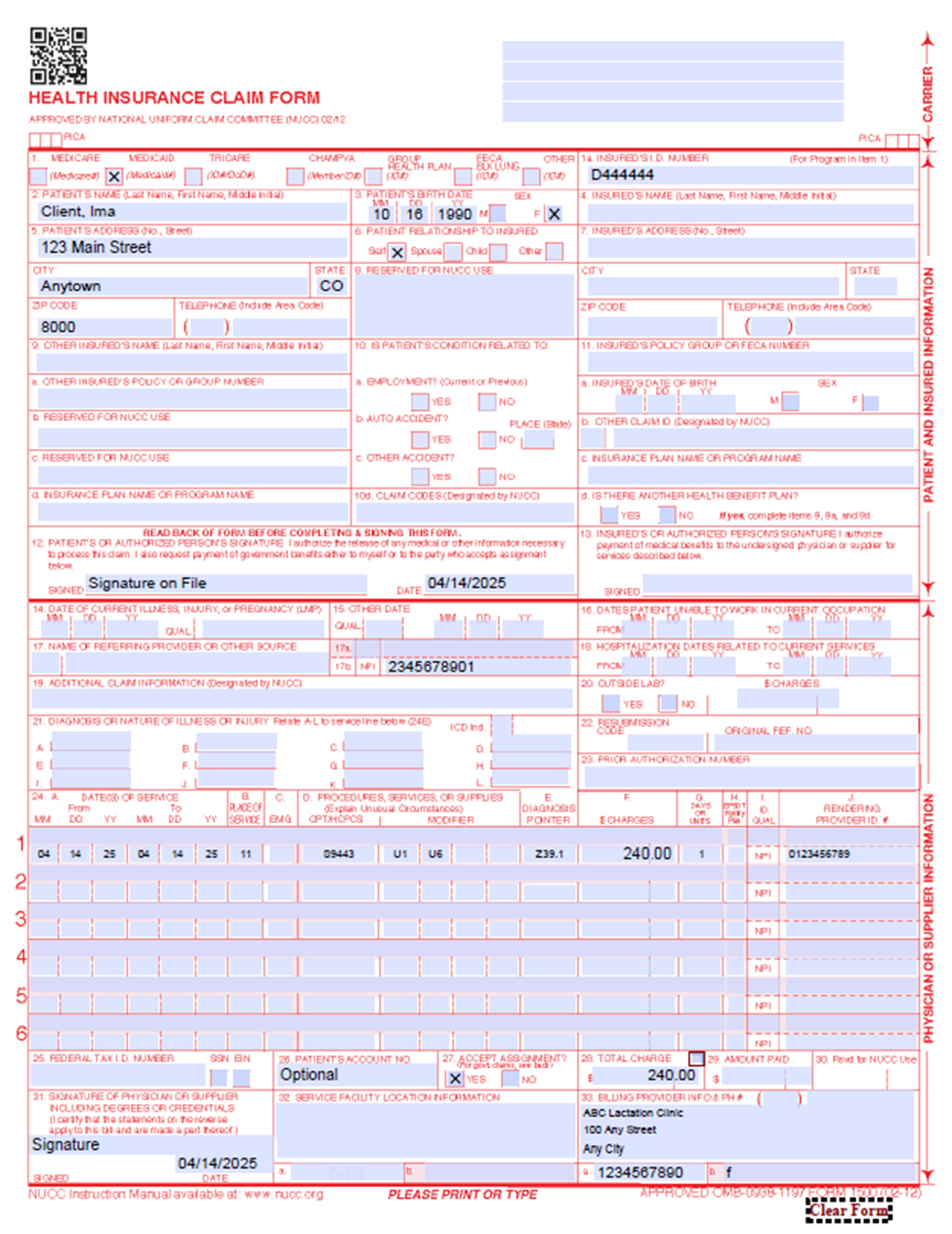
CMS 1500 Paper Claim Reference Table
The following paper claim form reference table shows required, optional and conditional fields and detailed field completion instructions for the CMS 1500 professional claim form.
| CMS Field Number & Label | Field is? | Instructions | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven (7)-digit Health First Colorado ID number as it appears on the Medicaid Identification card. Example: A123456. | ||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name and middle initial. | ||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES," enter the insured's last name, first name and middle initial. | ||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES," enter the policy or group number. | ||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES" enter the insurance plan or program name. | ||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES," complete 9, 9a and 9d. | ||||||||||||
| 12. Patient's or Authorized Person's Signature | Required | Enter "Signature on File," "SOF" or legal signature. If there is no signature on file, leave blank or enter "No Signature on File." Enter the date the claim form was signed. | ||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||
| 14. Date of Current Illness, Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||
| 17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. | ||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left-hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use with original claim submissions. | ||||||||||||
| 23. Prior Authorization | Not Required | Prior Authorization Enter the six (6)-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. | ||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||
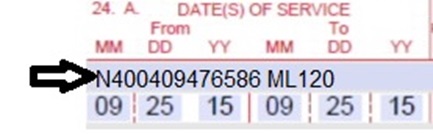
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019.
| ||||||||||||
| 24B. Place of Service | Required | Reference the billing policy found in this manual for allowed Place of Service codes. | ||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom unshaded area of the field to indicate the service was rendered for a life-threatening condition or one that requires immediate medical intervention. | ||||||||||||
24D.Procedures, Services, or Supplies
| Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested: S9443 All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. Please reference the billing policy detailed in this manual for specific modifier code use. | ||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first and other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado-covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only. Do not enter fractions or decimals. | ||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early & Periodic Screening, Diagnosis and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available- Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) If the service is Family Planning (e.g., contraception, sterilization), enter "Y" for YES or "N" for NO in the bottom unshaded area of the field. | ||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the National Provider Identifier (NPI) or the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. Unacceptable signature alternatives: Claim preparation personnel may not sign the enrolled provider's name. Initials are not acceptable as a signature. Typed or computer printed names are not acceptable as a signature. "Signature on file" notation is not acceptable in place of an authorized signature. | ||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line: Name 2nd Line: Address 3rd Line: City, State and ZIP Code If the PT is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line: Name 2nd Line: Address 3rd Line: City, State and ZIP Code | ||||||||||||
| 33a- NPI Number | Required | |||||||||||||
| 33b- Other ID # | If the PT is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||
CMS 1500 Lactation Support Service Example
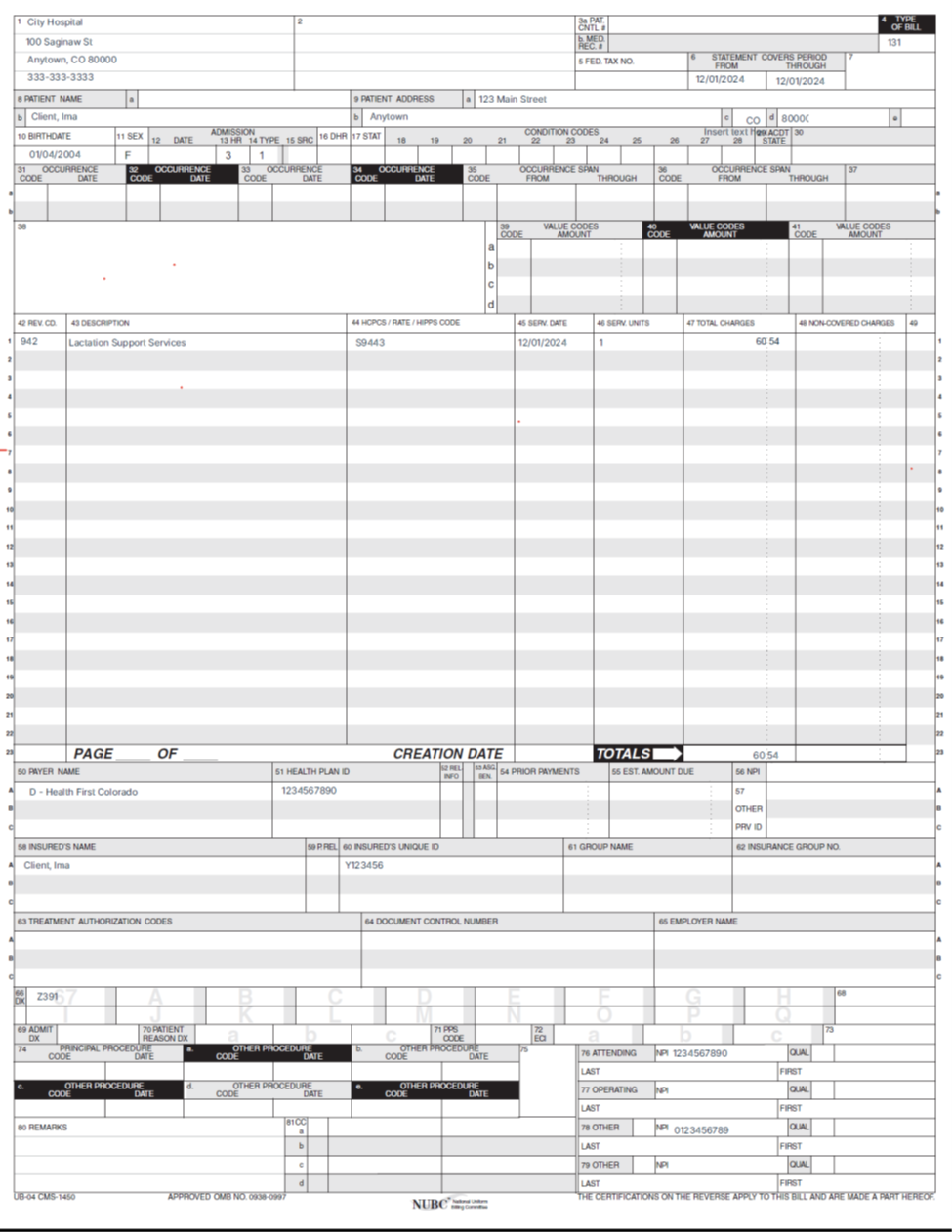
UB-04 Paper Claim Reference Table
Lactation Support Services outpatient hospital paper claims must be submitted on the UB-04 claim form.
The information in the following table provides instructions for completing form locators (FL) as they appear on the paper UB-04 claim form. Instructions for completing the UB-04 claim form are based on the current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data form locators on the UB-04 have the same attributes (specifications) for Health First Colorado as those indicated in the NUBC UB-04 Reference Manual.
All code values listed in the NUBC UB-04 Reference Manual for each form locator may not be used for submitting paper claims to Health First Colorado. The appropriate code values listed in this manual must be used when billing Health First Colorado.
The UB-04 Certification document must be completed and attached to all claims submitted on the paper UB-04. Completed UB-04 paper Health First Colorado claims, including hardcopy Medicare claims, should be mailed to the correct fiscal agent address listed in Appendix A, under the Appendices drop-down section on the Billing Manuals web page.
Do not submit "continuation" claims. Each claim form has a set number of billing lines available for completion. Do not crowd more lines on the form.
Billing lines in excess of the designated number are not processed or acknowledged. Claims with more than one page may be submitted through the Provider Web Portal.
Bill with a date span (From and To dates of service) only if the service was provided every consecutive day within the span. The From and To dates must be in the same month.
The Paper Claim Reference Table below lists the required, optional and/or conditional form locators for submitting the paper UB-04 claim form to Health First Colorado for nursing facility services.
| Form Locator and labels | Completion format | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Billing Provider Name, Address, Telephone Number | Text | Required
Abbreviate the state using standard post office abbreviations. Enter the telephone number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Pay-to Name, Address, City, State | Text | Required only if different from FL 1.
Abbreviate the state using standard post office abbreviations. Enter the telephone number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3a. Patient Control Number | Up to 20 characters: Letters, numbers or hyphens | Optional Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3b. Medical Record Number | 17 digits | Optional Enter the number assigned to the member to assist in retrieval of medical records. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Type of Bill | 3 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Federal Tax Number | None | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Statement covers period From/Through | From:6 digits MMDDYY Through: 6 digits MMDDYY | Required This form locator must reflect the beginning and ending dates of service. When span billing for multiple dates of service and multiple procedures, complete FL 45 (Service Date). Providers not wishing to span bill following these guidelines, must submit one claim per date of service. "From" and "Through" dates must be the same. All line item entries must represent the same date of service. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8a. Patient Identifier | Text | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8b. Patient Name | Up to 25 characters, letters & spaces | Required Enter the member's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Patient Address - Street | Characters Letters & numbers | Required Enter the member's street/post office box as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Patient Address - City | Text | Required Enter the member's city as determined at the time of admission | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Patient Address - State | Text | Required Enter the member's state as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Patient Address - ZIP | Text | Required Enter the member's zip code as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9e. Patient Address - Country Code | Digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10. Birthdate | 8 digits (MMDDCCYY) | Required Enter the member's birthdate using two digits for the month, two digits for the date, and four digits for the year (MMDDCCYY format). Example: 01012010 for January 1, 2010. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Patient Sex | 1 letter | Required Enter an M (male) or F (female) to indicate the member's sex. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Admission Date | 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Admission Hour | 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Admission Type | 1 digit | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Source of Admission | 1 digit | Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Discharge Hour | 2 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Patient Discharge Status | 2 digits | Required Dialysis must use code 01. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18-28. Conditions Codes | 2 digits | Conditional Complete with as many codes necessary to identify conditions related to this bill. Condition Codes Renal dialysis settings | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Accident State | 2 digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31-34. Occurrence Code/Date | 2 digits & 6 digits | Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35-36. Occurrence Span Code From/ Through | Digits | Leave blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38. Responsible Party Name/Address | None | Leave blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39-41. Value Codes and Amounts | 2 characters and up to 9 digits | Conditional
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 42. Revenue Code | 4 digits | Required Enter the revenue code which identifies the specific service provided. List revenue codes in ascending order. These codes are listed in Appendix Q, under the Appendices drop-down section on the Billing Manuals web page, for valid dialysis revenue codes. A revenue code must appear only once per date of service.* If more than one of the same service is provided on the same day, combine the units and charges on one line accordingly. Complete with as many codes necessary to identify conditions related to this bill. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 43. Revenue code Description | Text | Required
Example:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 44. HCPCS/Rates/ HIPPS Rate Codes | 5 digits | Conditional Enter only the HCPCS code for each detail line. Use approved modifiers listed in this section for hospital based transportation services. Complete for laboratory, radiology, physical therapy, occupational therapy and hospital based transportation. When billing HCPCS codes, the appropriate revenue code must also be billed. Services Requiring HCPCS Enter HCPCS and revenue codes for each radiology line. The only valid modifier for OP radiology is TC. Refer to the annual HCPCS bulletin for instructions in the Provider Services Bulletins section of the website. With the exception of outpatient lab and hospital-based transportation, outpatient radiology services can be billed with other outpatient services. HCPCS codes must be identified for the following revenue codes:
HCPCS codes cannot be repeated for the same date of service. Combine the units in FL 46 (Units) to report multiple services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 45. Service Date | 6 digits | For span bills only Each date of service must fall within the date span entered in the "Statement Covers Period" field (FL 6). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 46. Service Units | 3 digits | Required For span bills, the units of service reflect only those visits, miles or treatments provided on dates of service in FL 45. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 47. Total Charges | 9 digits | Required Enter the total charge for each line item. Calculate the total charge as the number of units multiplied by the unit charge. Do not subtract Medicare or third-party payments from line charge entries. Do not enter negative amounts. A grand total on line 23 is required for all charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 48. Non-covered Charges | Up to 9 digits | Conditional Enter incurred charges that are not payable by Health First Colorado. Non-covered charges must be entered in both FL 47 (Total Charges) and FL 48 (Non-Covered Charges.) Each column requires a grand total on line 23. Non-covered charges cannot be billed for outpatient hospital laboratory or hospital based transportation services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 50. Payer Name | 1 letter and text | Required Enter the payment source code followed by name of each payer organization from which the provider might expect payment.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 51. Health Plan ID | 10 digits | Required Enter the NPI number assigned to the billing provider. Payment is made to the enrolled provider or agency that is assigned this number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 52. Release of Information | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 53. Assignment of Benefits | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 54. Prior Payments | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter third party and/or Medicare payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 55. Estimated Amount Due | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter the net amount due from Health First Colorado after provider has received other third party, Medicare or member liability amount. Medicare Crossovers Enter the sum of the Medicare coinsurance plus Medicare deductible less third-party payments and member payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 56. National Provider Identifier (NPI) | 10 digits | Required Enter the billing provider's 10-digit National Provider Identifier (NPI). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 57. Other Provider ID | Optional Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 58. Insured's Name | Up to 30 characters | Required Enter the member's name on the Health First Colorado line. Other Insurance/Medicare Complete additional lines when there is third party coverage. Enter the policyholder's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 60. Insured's Unique ID | Up to 20 characters | Required Enter the insured's unique identification number assigned by the payer organization exactly as it appears on the health insurance card. Include letter prefixes or suffixes shown on the card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 61. Insurance Group Name | 14 letters | Conditional Enter the name of the group or plan providing the insurance to the insured exactly as it appears on the health insurance card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 62. Insurance Group Number | 17 digits | Conditional Enter the identification number, control number or code assigned by the carrier or fund administrator identifying the group under which the individual is carried. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 63. Treatment Authorization Code | Up to 18 characters | Conditional Complete when the service requires a PAR. Enter the authorization number in this FL if a PAR is required and has been approved for services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 64. Document Control Number | None | Conditional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 65. Employer Name | Text | Conditional Complete when there is third party coverage. Enter the name of the employer that provides health care coverage for the individual identified in FL 58 (Insured Name). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 66. Diagnosis Version Qualifier | Submitted information is not entered into the claim processing system. Enter applicable ICD indicator to identify which version of ICD codes is being reported. 0ICD-10-CM (DOS 10/1/15 and after) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67. Principal Diagnosis Code | Up to 6 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67A.-67Q. - Other Diagnosis | 6 digits | Optional Enter the exact diagnosis code corresponding to additional conditions that co-exist at the time of admission or develop subsequently and which effect the treatment received or the length of stay. Do not add extra zeros to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 69. Admitting Diagnosis Code | 6 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 70. Patient Reason Diagnosis | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 71. PPS Code | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 72. External Cause of Injury code (E-Code) | 6 digits | Optional Enter the diagnosis code for the external cause of an injury, poisoning or adverse effect. This code must begin with an "E". | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74. Principal Procedure Code/Date | 7 characters and 6 digits | Conditional Enter the ICD-10-CM procedure code for the principal procedure performed during this billing period and the date on which procedure was performed. Enter the date using MMDDYY format. Apply the following criteria to determine the principal procedure: The principal procedure is not performed for diagnostic or exploratory purposes. This code is related to definitive treatment, and The principal procedure is most related to the primary diagnosis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74A. Other Procedure Code/Date | 7 characters and 6 digits | Conditional Complete when there are additional significant procedure codes. Enter the procedure codes identifying all significant procedures other than the principal procedure and the dates on which the procedures were performed. Report those that are most important for the episode of care and specifically any therapeutic procedures closely related to the principal diagnosis. Enter the date using MMDDYY format. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 76. Attending NPI - Required | NPI - 10 digits | Health First Colorado ID Required NPI - Enter the 10-digit NPI number assigned to the physician having primary responsibility for the member's medical care and treatment. This number is obtained from the physician and cannot be a clinic or group number. (If the attending physician is not enrolled in the Health First Colorado or if the member leaves the ER before being seen by a physician, the hospital may enter their individual numbers.) Hospitals and FQHCs may enter the member's regular physician's 10-digit NPI in the Attending Physician ID form locator if the locum tenens physician is not enrolled in the Health First Colorado. QUAL - Enter "1D" for Health First Colorado Enter the attending physician's last and first name. This form locator must be completed for all services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 77. Operating NPI | Not required Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 78-79. Other ID | NPI - 10 digits | Conditional Complete when attending physician is not the PCP or to identify additional physicians. Ordering, Prescribing or Referring NPI - when applicable NPI - Enter up to two 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attending physician is not the PCP or if a clinic is a PCP agent, enter the PCP NPI number as the referring physician. The name of the Health First Colorado member's PCP appears on the eligibility verification. Review either for eligibility or PCP. Health First Colorado does not require that the PCP number appear more than once on each claim submitted. The attending physician's last and first name are optional. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 80. Remarks | Text | Enter specific additional information necessary to process the claim or fulfill reporting requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 81. Code - QUAL/CODE/VALUE (a-d) | Qualifier: 2 digits Taxonomy Code: 10 digits | Optional Complete both the qualifier and the taxonomy code for the billing provider in field 81CC-a. Field 81CC-a must be billed with qualifier B3 for the taxonomy code to be captured in the claims processing system. If B3 is missing, no taxonomy code will be captured in the claims processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
UB-04 Lactation Support Service Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Lactation Support Specialist Billing Manual Revision Log
Revision Date | Addition/Changes | Made by |
|---|---|---|
| 11/12/2024 | Creation of Manual | HCPF |
| 02/03/2025 | Added information for Lactation Support Services provided by a dually-qualified Doula; added fee schedule information; updated billing information for twins (multiple infants); added information for determining what time counts towards 15-minute time codes; added information about National Correct Coding Initiative (NCCI); updated OPR policy information. | HCPF |
| 04/30/2025 | Updated billing information for Lactation Support Services. Updated CMS 1500 Lactation Support Services claim example. | HCPF |
| 05/20/2025 | Added Supply PT 14 to eligible billing providers; updated diagnosis code information; updated billing guidance for submitting claims under lactating member or breastfeeding child; added information for outpatient hospital; added UB-04 paper claim reference table; added UB-04 Lactation Support Services example. | HCPF |
| 07/16/2025 | Updated the Ordering, Prescribing, and Referring (OPR) provider types who may recommend Lactation Support Services. | HCPF |
| 08/21/2025 | Added Third-Party Liability (TPL) information. | HCPF |
| 10/15/2025 | Updated Lactation-Doula Cross-Billing guidance. | HCPF |
| 01/27/2026 | Updated eligible rendering and individual billing providers. Updated policy guidance for enrolled individual providers with training in advanced lactation support. | HCPF |