Behavioral Health Policies, Standards, and Billing References
- Abbreviations and Acronyms
- Third Party Liability (TPL) [07/01/2022]
- Telehealth Policy [01/01/2021]
- Service Documentation Standards [01/01/2022]
- Treatment Plan Standards [07/01/2018]
- Neuro/Psychological Testing Policy [01/01/2022]
- Medicaid Providers [01/07/2018]
- Room and Board
- Court-Ordered Services
- Definition of Medical Necessity
- Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
- Covered Diagnoses
- Claiming Medicaid Services
- Outpatient Hospital Services
- Licensed Provider Claiming Under a Supervisor
- Missed Appointments
- Health First Colorado Behavioral Health Rendering Provider Oversight (RPO) Policy
- Time Documentation Standards/Rules
- Current Procedural Terminology (CPT) Service Categories
- Medicaid State Plan Services
- Medicaid 1915(B)(3) Waiver Services
- Medicaid Place of Service Codes
- Medicaid Billing Provider Types Who Can Bill Under The Capitated Behavioral Health Benefit
- Modifiers for Medicaid Capitated Behavioral Health Benefit
- Targeted Case Management
- Behavioral Health Peer Support Policy
- Clinical Laboratory Improvement Amendments (CLIA)
- FAQs on Urine Collection and Analysis [07/01/2018]
- Essential Safety Net Provider Alignment Guide
- Colorado System of Care (CO-SOC)
- Directed Payment Policy
- Colorado Medically Unlikely Edits and Procedure to Procedure (CO MUEs and CO PTP)
- National Correct Coding Initiative (NCCI) edits
- Behavioral Health Secure Transport Place of Service
- Senate Bill 23-174: Coverage Policy
- Prior Authorization and Retrospective Reviews for Outpatient Psychotherapy
This contains common abbreviations or acronyms not elsewhere explained in other resources.
Term/Acronym | Definition |
|---|---|
| ACT | Assertive Community Treatment |
| ADL | Activities of Daily Living |
| AHA | American Hospital Association |
| AHIMA | American Health Information Management Association |
| AMA | American Medical Association OR Against Medical Advice |
| AOD | Alcohol and/or Other Drugs |
| APA | American Psychological Association |
| APR | Advanced Practice Registry |
| ASAM | American Society of Addiction Medicine |
| (b)(3)/B3 | 1915(b)(3) Waiver |
| BH | Behavioral Health |
| BHA | Behavioral Health Administration |
| CARF | Commission on Accreditation of Rehabilitation Facilities |
CASASTARTSM | The National Center on Addiction & Substance Abuse at Columbia University Striving Together to Achieve Rewarding Tomorrows |
| CBH | Community Behavioral Health |
| CCAR | Colorado Client Assessment Record |
| CCR | Colorado Code of Regulations |
| CDHS | Colorado Department of Human Services |
| CDPHE | Colorado Department of Public Health and Environment |
| CFR | Code of Federal Regulations |
| CLIA | Clinical Laboratory Improvements Amendment |
| CM | Case Management |
| CMB | Colorado Medical Board |
| CMS | Centers for Medicare and Medicaid Services |
| CNA | Certified Nurse Aide |
| CNM | Certified Nurse Midwife |
CPT® | Current Procedural Terminology |
| CYMHTA | Children and Youth Mental Health Treatment Act |
| DD | Developmental Disability(ies) |
| DME | Durable Medical Equipment |
| DOC | Department of Corrections |
| DORA | Department of Regulatory Agencies |
| DRG | Diagnosis-Related Group |
| DSM-5 | Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition |
| DYS | Division of Youth Services |
| EHR | Electronic Health Record |
| EI | Early Intervention |
| E/M | Evaluation and Management |
| EOB | Explanation of Benefits |
| EPSDT | Early Periodic Screening Diagnosis and Treatment Program |
| ER | Emergency Room |
| FARS/DFARS | Federal Acquisition Regulation System/Defense Federal Acquisition Regulation Supplement |
| FFP | Federal Financial Participation |
| FFS | Fee-For-Service |
| FQHC | Federally Qualified Health Center |
| FTE | Full-Time Equivalent |
| FY | Fiscal Year |
| HCBS | Home and Community-Based Services |
| HCPCS | Healthcare Common Procedure Coding System |
| HCPF | Department of Health Care Policy and Financing |
| HHS | US Department of Health and Human Services |
| HIPAA | Health Insurance Portability and Accountability Act of 1996 |
| ICD-10-CM | International Classification of Diseases, Tenth Revision, Clinical Modification |
| ICF | Intermediate Care Facility |
| ICF-MR | Intermediate Care Facility for the Mentally Retarded |
| ICM | Intensive Case Management |
| IEP | Individualized Education Program |
| IMD | Institute(s) for Mental Disease |
| Inpt Hosp | Inpatient Hospital |
| Inpt PF | Inpatient Psychiatric Facility |
| IOP | Intensive Outpatient Psychiatric/Program |
| JCAHO | Joint Commission on Accreditation of Healthcare Organizations (The Joint Commission) |
| LMHP | Licensed Mental Health Professional |
| LOC | Level of Care |
| LSW | Licensed Social Worker |
| MAP | Medical Assistance Program |
| MCE | Managed Care Entity |
| MCO | Managed Care Organization |
| MCR | Mobile Crisis Response |
| MH | Mental Health |
| MHP | Mental Health Professional |
| MI | Mental Illness |
| MST | Multi-Systemic Therapy |
| NAMI | National Alliance on Mental Illness |
| NF | Nursing Facility |
| NH | Nursing Home |
| NP | Nurse Practitioner |
| NPI | National Provider Identifier |
| NPP | Non-Physician Practitioner |
| NOS | Not Otherwise Specified |
| OTP | Opioid Treatment Provider |
| PCMP | Primary Care Medical Provider |
| PCP | Primary Care Physician |
| PF - PHP | Psychiatric Facility – Partial Hospital |
| PHP | Partial Hospital Program |
| POS | Place of Service |
| PPS | Prospective Payment System |
| Prison/CF | Prison/Correctional Facility |
| PRTF | Psychiatric Residential Treatment Facility |
| PSR | Psychosocial Rehabilitation |
| QRTP | Qualified Residential Treatment Program |
| RCCF | Residential Child Care Facility |
| RAE | Regional Accountable Entity |
| RxN | Advanced Practice Nurse with Prescriptive Authority |
| SAMHSA | Substance Abuse and Mental Health Services Administration |
| SDOH | Social Determinants of Health |
| SED | Serious Emotional Disturbance(s) |
| SI | Suicidal Ideation |
| SMI | Serious/Severe Mental Illness |
| SNF | Skilled Nursing Facility |
| SSA | Single State Agency |
| SSN | Social Security Number |
| SUD | Substance Use Disorder |
| TBI | Traumatic Brain Injury |
| TCM | Targeted Case Management |
| TIN | Tax Identification Number |
| TOB | Type of Bill |
| UA | Urine Analysis/Urinalysis |
| UB | Uniform Bill |
| WRAP | Wellness Recovery Action Plan |
Third Party Liability (TPL) [07/01/2022]
Providers are responsible for billing the payor who has primary responsibility for a service. There is a hierarchy to payers when a member has multiple insurances or is eligible for multiple benefit coverages. In general, private insurance should be billed first and then federal or state payers would be secondary. Medicaid is called the payer of last resort because Federal regulations require that all available health insurance benefits be used before Medicaid considers payment. With few exceptions, claims for members with health insurance resources are denied when the claim does not show insurance payment or denial information.
When a Medicaid practitioner serves a member who is covered by both Medicare and Medicaid [i.e. considered dually eligible], they must submit claims for processing by Medicare before billing the MCE. Medicaid practitioners who serve dually eligible members must be enrolled with Medicare to bill the responsible primary payor. Effective April 1, LPCs, LMFTs and LACs who serve Medicare members are required to enroll as Medicare providers. Claims for behavioral health services provided by a pre-licensed clinician or an unlicensed professional under the oversight of a Medicare-enrolled provider submitting claims as the Rendering Provider can be submitted directly to the MCE. These claims must include the HO modifier in the first available position after any required modifiers, to indicate the practitioner performing the service is not eligible to be covered by Medicare. Claims for services not covered by Medicare can be submitted directly to the MCE.
Medicaid does not automatically pay commercial health insurance co-pays, coinsurance, or deductibles. If the commercial health insurance benefit is the same or more than the Health First Colorado benefit allowance, no additional payment will be made. Providers cannot bill members for the difference between commercial health insurance payments and their billed charges when Medicaid does not make additional payment. The provider also cannot bill members for co- pay/deductibles assessed by the TPL. A provider must be contracted with all coverages a member has in order to comply with TPL policies. A provider cannot use a primary coverage denial resulting from being an out-of-network provider as appropriate TPL documentation when billing Medicaid. For additional information on TPL, please refer to the FAQ below.
Third Party Liability and Coordination of Benefits Frequently Asked Questions
Version 1.0, Created 7/1/2024
This FAQ is intended to provide guidance to providers serving Medicaid Members who have additional sources of insurance coverage.
Q1. What is Third Party Liability (TPL)?
A1. Under Federal regulation (See 42 CFR Part 433 Subpart D), “Third Party Liability” (TPL) means that payment is the responsibility of a third party other than the individual or the Medicaid Program. Medicaid is the payor of last resort. By law, virtually all other sources of health coverage must pay claims under their policies before Medicaid will pay for the care of an eligible individual.
Q2. What is Coordination of Benefits (COB) and how does it work in general?
A2. Coordination of Benefits refers to the practice of ensuring that a claim is paid by the payor that is legally responsible for paying a claim as Primary with any secondary parties paying Secondary. Coordinating benefits makes sure that the correct party pays first by, 1) cost-avoiding (aka denying) claims where a known other party should be paying and/or 2) cost-recovering a claim that Medicaid erroneously paid that should have been paid by another party.
Q3. Where can I find all of the coverages where a Medicaid Member is enrolled?
A3. Providers have multiple options for establishing a Member's coverage. A Medicaid Member has a primary responsibility for disclosing all coverages in which they are enrolled. Additionally, a provider should verify both Medicaid and other coverage in the Medicaid Provider Portal (See Accessing Eligibility Verification Information).
The Medicaid Provider Portal captures other coverage information from the Medicaid Management Information System (MMIS), the Department of Health Care Policy & Financing’s (HCPF) system of record for TPL. TPL data is added to the MMIS from multiple sources under a hierarchy defined by HCPF and sources populate data into the system in different cadences.
Any additions of coverage or updates to existing coverage that are manually entered into the Provider Portal by providers are reviewed by HCPF’s Fiscal Agent staff before changes are accepted. The Fiscal Agent, Gainwell Technologies, is responsible for enrolling providers, providing billing assistance, etc. (See Fiscal Agent Responsibilities). The manual review occurs weekly so providers will not immediately see changes they have made. HCPF is working on enhancements to the Provider Portal processes to increase the frequency of manual reviews and to automate additions and updates of the TPL information.
Q4. Are Children’s Health Plan (CHP), MCOs and other “Medicaid” Plans treated the same as “Medicaid - Title XIX” for purposes of TPL and coordination of Benefits?
A4. All programs and benefit aid types shown in the Medicaid Provider Portal are subject to coordination of benefits and remain the payor of last resort. Generally, Members with Title XIX Medicaid are able to have commercial insurance and/or Medicare.
If there is no other coverage for a Member, providers should follow standard Medicaid billing practices. Providers can find additional guidance regarding specific coverage types by viewing the Verifying Specific Coverage Types document. Providers can also reference this Verifying Eligibility Quick Guide for additional information on Member eligibility.
Q5. What can I do if I discover a Member has additional coverage after a service is provided?
A5. A provider should bill the Primary payor first under standard TPL policies. If the provider has already received payment from Gainwell or the Managed Care Entity (MCE) prior to learning of the other coverage, the provider should immediately bill the other coverage for payment as Primary. If the provider receives payment from the other carrier, they need to return their Primary payment from Gainwell or the MCE. The provider should then rebill Gainwell or the MCE as Secondary.
*If the provider receives a denial for being out of network with the Primary payor, they should not submit the claim for full payment to Gainwell or the MCE. Please see the response to Question 9 below.
Providers contracted with an MCE should follow the applicable published timely filing guidelines for that MCE when resubmitting a claim. Providers can resubmit a Primary or Secondary fee-for-service claim to Gainwell for payment within 60 days from the date of a void or retraction. (See Timely Filing and Resubmissions)
Q6. Am I allowed/required to collect a deductible, coinsurance, and/or copayments for the Primary Insurance from a Member who also has Medicaid coverage?
A6. No. A provider is only allowed to collect appropriate Medicaid copays. There are no Medicaid copays for behavioral health services.
Providers cannot bill Members for the difference between commercial health insurance payments and their billed charges when Health First Colorado or an MCE does not make additional payment. The provider also cannot bill Members for copay/deductibles assessed by another payor.
Q7. Can I bill a Member for services that are not covered by Medicaid?
A7. A Medicaid Member may choose to privately pay for services that are NOT covered by Medicaid, including services determined not to be medically necessary. Failure by the provider to follow the proper process to obtain a prior authorization does not mean that a service is not covered by Medicaid or medically necessary. Additionally, if a provider chooses not to enroll with Medicaid or contract with an MCE, that does not qualify as documentation to bill a Member for services, nor does it deem a service as uncovered or not medically necessary.
A Member is responsible for payment for the items provided or services rendered only when there is a written agreement in place. This written agreement is distinct from the standard consent form included in documentation a Member completes when they establish care with a provider. This agreement should, at a minimum, be signed prior to services being rendered and include a statement of the specific services being rendered, an explanation that the services are not covered by Medicaid, and that Medicaid cannot reimburse the Member for those services directly, and the full amount the Member will be responsible for paying. See C.R.S. § 25.5-4-301(1)(a)(1).
Q8. What if I am contracted with an MCE but not contracted with the Primary Insurance?
A8. A provider must be contracted with a Member’s Primary Insurance in order to comply with TPL standards. A provider is required to bill the Primary Insurance and cannot submit claims to Gainwell or the MCE without TPL documentation. Claims that are submitted without TPL documentation will be denied by both Gainwell and an MCE.
Q9. Can a provider who ‘Opts Out’ of Medicare with CMS serve Members who are dually eligible with Medicare and Medicaid?
A9. No. A provider must be contracted with a Member’s Primary Insurance in order to comply with TPL standards. A provider who ‘Opts Out’ of Medicare would not be able to properly bill Medicare for covered services as the Primary coverage. Additionally, this provider would not be able to bill Medicaid without the appropriate TPL documentation, and the provider would not be able to bill the Member.
Q10. What steps should I take once I have identified all of a Medicaid Member’s coverages?
A10. There are three (3) steps to getting reimbursement for services provided to a Medicaid Member with multiple health insurance coverages:
- Bill the Primary Insurance for payment.
- Bill the Secondary for payment with the Primary Insurance TPL payment and cost sharing information.
- Store the other coverage information within the provider’s Member record and claim payment system(s) for use in future claim submissions.
- Add the other coverage to the Medicaid Provider Portal. (See the Provider Web Portal Quick Guide: Adding and Updating Third-Party Liability (TPL) Information).
- Update the provider records and Medicaid Provider Portal as coverages change.
Example:
| Provider submits claim to Primary Insurance | $200.00 |
| Primary Insurance pays provider | $80.00 |
| Provider submits same claim to Gainwell or MCE - Includes TPL information with claim showing total paid to provider by Primary Insurance | $200.00 $80.00 |
| Gainwell refers to fee schedule MCE refers to contracted rate amount | $84.00 |
| Provider is paid the allowed rate less the TPL payment | $4.00 |
| Provider receives total reimbursement from Gainwell/MCE | $4.00 |
Provider stores the other coverage for future billings | |
*This illustrates a provider underbilling for services but receiving the full Directed Payment amount as required.
Q11. What happens when Medicaid has issued a Directed Payment for a service?
A11. The MCE is required to reimburse a provider a minimum of the Directed Payment published rate. The Directed Payment reimbursement will still follow general TPL guidelines where all payments from other coverage will be deducted from the amount of the Directed Payment rate.
Example:
| Provider submits claim to Primary Insurance | $200.00 |
| Primary Insurance pays provider | $80.00 |
| Provider submits same claim to Gainwell or MCE - Includes TPL information with claim showing total paid to provider by Primary Insurance | $200.00 $80.00 |
| Gainwell refers to fee schedule MCE refers to Directed Payment rate amount | $250.00* |
| Provider is paid the allowed rate less the TPL payment | $170.00 |
| Provider receives total reimbursement from Gainwell/MCE to ensure provider receives the PPS/Directed Payment amount | $170.00 |
Provider stores the other coverage for future billings | |
*This illustrates a provider underbilling for services but receiving the full Directed Payment amount as required.
Q12. Are there any instances when a provider should not bill the Primary
Insurance first?
A12. Providers should always bill a Member’s Primary Insurance prior to billing Medicaid or the MCE. Covered services for Primary Insurance policies vary by plan design. Billing the Primary Insurance allows a provider the opportunity to collect a higher reimbursement for covered services and also facilitates proper coordination of benefits, especially if the service’s coverage is questionable. When the Primary Insurance does not cover the service provided, a provider can submit the claim to Gainwell or the MCE.
HCPF recognizes that some behavioral health services are not routinely covered by Primary Insurance policies and may only be covered by Medicaid or the MCE. Behavioral health providers can review services determined to be covered by Medicare, Medicaid and commercial insurances in Appendix I in the State Behavioral Health Services (SBHS) Billing Manual.
For additional questions regarding TPL and COB policies, please send your inquiries to thirdparty_liability@state.co.us.
Telehealth Policy [01/01/2021]
Telehealth is the use of telecommunications and information technology to provide access to health assessment, diagnosis, intervention, consultation, supervision, and information across distance. At one time, telehealth in Medicaid had been referred to as telemedicine. Under the Medicaid Capitated Behavioral Health Benefit MCEs have the flexibility to authorize the use of outpatient treatment services to be delivered via audiovisual and telephone modalities when it is clinically viable and appropriate. The BHA does not limit the use of telehealth at licensed and designated facilities. Services provided via telehealth should be indicated by Place of Service 02 – “Telehealth Provided Other than in Member’s Home” or 10 – “Telehealth Provided in Member’s Home”. These place of service codes are not included on any coding page but should be used per each MCEs policy guidance.
Other standard requirements for telehealth services provided to a member include:
- All services must be synchronous.
- Any health benefits provided through telehealth shall meet the same standard of care as in- person care.
- The availability of services through telehealth in no way alters the scope of practice of any health care provider; nor does it authorize the delivery of health care services in a setting or manner not otherwise authorized by law.
- Services may be delivered by telephone only when it is clinically appropriate, no other form of service delivery is possible, and this is documented in the clinical record. When a service is provided by telephone (Audio Only) modifier FQ should be used in the first available position on a claim.
- Members that are new to a provider must contact the provider to initiate services.
- Services for established members must be consistent with the members’ treatment plan.
- Providers must document the member’s consent, either verbal or written, to receive telehealth services.
- Record-keeping and member privacy standards should comply with normal BHA and Medicaid requirements, HIPAA and 42 CFR Part 2 requirements.
- Services not otherwise covered by the BHA, or Health First Colorado are not covered when delivered via telehealth.
- Providers may only bill procedure codes which they are contracted with a MCE to bill.
Service Documentation Standards [01/01/2022]
Providers have the discretion to design the format of a service note that captures documentation in line with these guidelines and general professional standards for clinical care. Documenting clinical encounters is essential to quality clinical care and lays the foundation for coding and billing, as well as telling the story of the person’s treatment over time. Documentation is also evidence of several important factors:
- That a service was provided.
- That there is clinical rationale and medical necessity for the service.
- That the service code utilized is appropriate to the encounter.
- Whether the individual served is engaged and/or benefiting form the service.
The following information must be documented for all clinical encounters submitted for reimbursement:
- Date of Service (DOS)
- Start and end time/duration of session and total contact time with person-served or collateral(s)
- Session setting/place of service
- Reason for the encounter, description of services provided, and interventions utilized
- Provider’s dated signature and relevant qualifying credential. A title should be included where no credential is held.
Depending on the purpose and details of the encounter, including the type of service, duration and mode of delivery, details are included to indicate medical necessity of the services provided, including (as appropriate):
- Documentation of consent to participate in the service (e.g. consenting to Telehealth)
- The individual’s response to the service and/or demonstrated benefit from the service provided
- Assessments, which may include treatment history, results of screening and/or diagnostic tools, Mental Status Exam (MSE), and clinical impressions.
- Relevance to the treatment/service plan, once implemented.
- Plan(s) for follow-up, including coordination of care, referrals, and recommendations
Shift Notes Documentation should include a description of all individual and group services rendered during the course of the shift/day. These can all be included in the same documentation or in a separate note as applicable (e.g. skills training group, individual therapy, med administration services, although included in the per diem, should be identified separately.)
Treatment Plan Standards [07/01/2018]
Clinical standards and best practice recommend that quality care should begin with a diagnostic evaluation or assessment of a member which would then inform a treatment/service plan. Outside of correct coding and appropriate documentation standards, Medicaid does not have any rules or guidelines that govern when an evaluation/assessment is completed, how frequently it is repeated, or what details are included. Additionally, while MCEs will audit providers and determine that assessments and treatment plans are documented and billed appropriately, there are no billing rules that require certain services to be billed or completed before other services. For example, practitioners do not have to provide service codes 90791 or H0032 before they bill 90834.
Neuro/Psychological Testing Policy [01/01/2022]
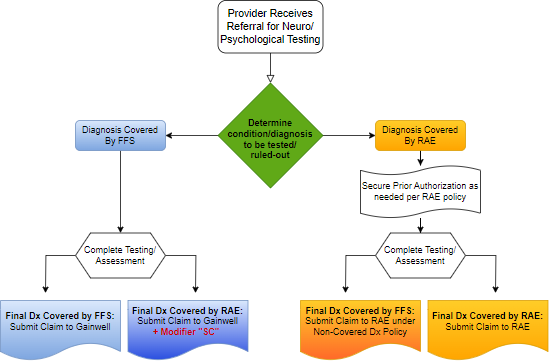
When a provider receives a referral for neuro/psychological testing the provider will determine the scope of testing needed based on a review of available member history and existing clinical documentation. Based on the primary condition being assessed or ruled out, a provider will identify the primary payer (RAE or FFS).
- RAE - If the referring diagnosis is part of the Capitated Behavioral Health Benefit (responsibility of the RAE), the provider should first seek Prior Authorization according to RAE policy. If the concluding diagnosis is a non-covered RAE diagnosis, the provider should still submit the claim to the RAE.
- FFS - If the referring diagnosis is part of the FFS benefit, then the provider needs to submit their claim to Gainwell for reimbursement. If the testing yields a diagnosis which is part of the Capitated Behavioral Health Benefit (responsibility of the RAE), the provider should still submit the claim to Gainwell and additionally use modifier code ‘SC’ to indicate it is an exception.
Medicaid Providers [01/07/2018]
Medicaid has two categories of providers with separate requirements addressing each. The Medicaid Provider is the provider agency or independent practitioner who has a direct relationship with the state. It has a signed agreement with the state and MCE, when appropriate. The Medicaid Provider is documented as overseeing the member’s course of treatment, and can order, prescribe, or refer a member for services. This is the provider that can bill for services. The state specifies the requirements to be a Medicaid provider and the qualifications to enroll with Medicaid.
Medicaid Providers must enroll with Medicaid as a defined provider type (PT). A PT is distinct from a license, credential, or service category since some of our PTs are for groups of providers or do not require a specific professional license. For example, an LPC, LCSW, or LAC in private practice would enroll as PT 38 - “Licensed Behavioral Health Clinician”. Each PT also has specialty types - additional information/qualifications on the PT. For example, an SUD Continuum (PT 64) has different Specialty Types for the ASAM level of treatment offered. Many of our PTs have the same PT and Specialty Type. For example, a Licensed Psychologist (PT 37) has a specialty type of Licensed Psychologist. A list of Medicaid PTs that can bill for Medicaid services can be found on HCPF's website under the Medicaid Billing Provider Types Who Can Bill Under The Capitated Behavioral Health Benefit: in Appendix L.
Service Providers
The Medicaid Provider may in turn establish a relationship with a clinician, therapist, program staff, or paraprofessional who provides hands-on care to the Medicaid member. These are known as Service Providers. Any non-licensed professional that delivers Medicaid billable services must operate under the clinical supervision of a licensed professional, and the name of that licensed professional appears on the claim as the Rendering Provider.
Each coding page in the State Behavioral Health Services (SBHS) Billing Manual identifies the service providers that are acceptable to provide hands-on care if the service is within the scope of practice for the practitioner. Scope of Practice “means the extent of the authorization to provide health services granted to a health practitioner by a license issued to the practitioner in the state in which the principal part of the practitioner’s services is rendered, including any conditions imposed by the licensing authority (§ 12-245-101).”
Depending on the type of Medicaid service (physician services or BH services) and whether a professional practice act applies, there may be very specific requirements associated with who is eligible to provide hands-on care. If this is the case, such requirements must be followed for the service to be properly provided and reimbursed.
This is a list of practitioners who can provide hands-on care of behavioral health services. The services performed must be within the scope of the practitioner’s practice and license. This list is not meant to indicate who can enroll with or submit claims to Medicaid.
| Acronym | Full Description | Regulatory Reference |
|---|---|---|
| APN | Advanced Practice Nurse. Professional nurse licensed by the CO Board of Nursing who is recognized and included on the Advanced Practice Registry by the CO Board of Nursing. | CRS 12-38-111.5; 3 CCR 716-1; SB 15- 197 |
| Bach Level | Bachelor's Degree. Bachelor's degree in social work, counseling, psychology, or related field from an accredited institution. Providers with a bachelor’s degree or higher in a non-related field may perform the functions of a bachelor’s degree level staff person if they have one year in the behavioral health field. | 10 CCR 2505-10 |
| CAC | Certified Addiction Counselor. A CAC is an individual who has a certificate issued by the board authorizing the individual to practice addiction counseling commensurate with his or her certification level and scope of practice. | CRS 12-245-801(7) |
| CAS | Certified Addiction Specialist. A CAS is an addiction counselor who may independently treat substance use and co-occurring disorders; conduct clinical assessments including diagnostic impression; provide treatment planning; coordinate referral and discharge planning; provide service coordination and case management; provide addiction counseling for individuals, families, and groups; and facilitate member, family, and community psychoeducation. A CAS may provide clinical supervision to individuals pursuing CAT and CAS. | 2 CCR 502-1; CRS 12-245-804(3.5)(b) |
| CAT | Certified Addiction Technician. A CAT is an entry-level counselor who may collect biopsychosocial screening data; provide service coordination and case management; monitor compliance with case management plans; provide skill-based education; co-facilitate therapy groups with certified addiction specialists or licensed addiction counselors; provide member, family, and community addiction education; and coordinate referral and discharge resourcing and planning. Staff in the process of obtaining addiction technician credentials or certified addiction technicians must have all clinical documentation reviewed and co-signed by their clinical supervisor. CAT staff can only account for a maximum of one quarter or 25% of the counseling staff for all licensed programs. | 10 CCR 2505-10 8.746; CRS 12-245-805(3)(a), |
| Certified/Registered Medical Assistant | Certified/Registered Medical Assistant. The U.S. Bureau of Labor identifies a medical assistant as an individual who completes administrative and clinical tasks in the offices of physicians, hospitals, and other healthcare facilities. Certification as a Certified Medical Assistant or a Registered Medical Assistant should be obtained through an accredited school | CRS 12-36-106 |
| CPS | Certified Prevention Specialist. Credentialed by the CO Prevention Certification Board, under guidelines set by the International Certification and Reciprocity Consortium. Pass the IC&RC Examination for Prevention Specialists | |
| CRNA | Certified Registered Nurse Anesthetist. Licensed by the CO Board of Nursing | CRS 12-38-111.5 |
| DO | Doctor of Osteopathy who is licensed by the CO Board of Medical Examiners | CRS 12-36-101 |
| Intern | An intern must be from the clinical program of study that meets minimum credentials for service provided or code billed. Clinical programs of study are Masters, Doctoral, or Prescriber programs. Prescriber programs for APNs include preceptorships and mentorships. Bachelors-level programs are not clinical programs of study, and students in a bachelor's- level program will not be classified as interns under this definition. Interns will perform duties under the direct clinical supervision of appropriately licensed staff | |
| LAC | Licensed Addiction Counselor - holds a master's degree or higher in a clinical Behavioral Health specialization from an accredited college or university. Licensed by the Board of Addiction Counselor Examiners | CRS 12-245-801; 4 CCR 744-1; HB 19- 1172 |
| LCSW | Licensed Clinical Social Worker - provider with master's or Doctoral degree from an accredited program offering full time course work approved by the Council on Social Work Education (CSWE). Provider is licensed by the Colorado Board of Social Work Examiners | CRS 12-43-403 |
| Licensed EdD, PhD, PsyD | Licensed Doctor of Education with a doctoral degree from an accredited program and who is licensed by the Colorado Board of Psychologist Examiners Licensed Doctor of Philosophy with a doctoral degree from an accredited program and who is licensed by the Colorado Board of Psychologist Examiners Licensed Doctor of Psychology with a doctoral degree from an accredited program and who is licensed by the Colorado Board of Psychologist Examiners | CRS 12-43-303 and 12-43-3043; CCR 721-1 |
| LMFT | Licensed Marriage and Family Therapist - provider possesses a master's degree or higher from a graduate program with course study accredited by the Commission on Accreditation for Marriage and Family Therapy Education (CAMFTE). Licensed by the CO Board of Marriage and Family Therapist Examiners. | CRS 12-43-504 |
| LPC | Licensed Professional Counselor - provider possesses a master's degree or higher in professional counseling from an accredited college or university. Licensed by the Colorado Board of Licensed Professional Counselor Examiners to practice professional counseling or mental health counseling | CRS 12-43-603; 4 CCR 737-1 |
| LPN/LVN | Licensed Practical Nurse and Licensed Vocational Nurse. Graduated from an approved program of practical nursing. Licensed as a Practical Nurse from the CO Board of Nursing | CRS 12-38-103 |
| LPT | Licensed Psychiatric Technician – provider performs selected acts requiring interpersonal and technical skills and includes the administering of selected treatments and selected medications prescribed by a licensed physician or dentist, in the care of and in the observation and recognition of symptoms and reactions of a patient with a behavioral or mental health disorder or an intellectual and developmental disability under the direction of a licensed physician and the supervision of a registered professional nurse. The selected acts in the care of a patient with a behavioral or mental health disorder or an intellectual and developmental disability must not require the substantial specialized skill, judgment, and knowledge required in professional nursing. | CRS 12-295-103 |
| MD | Doctor of Medicine who is licensed by the CO Board of Medical Examiners | CRS 12-36-101 |
| PA | Physician Assistant. Successfully completed the national certifying examination for PA's and is licensed by the CO Board of Medical Examiners | CRS 12-36-106; SB 01-128 |
| PSP | Peer Support Professional. A Peer Support Professional (PSP) may also be referred to as a peer support specialist, recovery coach, peer and family recovery support specialist, peer mentor, family advocate or family systems navigator. A PSP “is a person who uses his or her lived experience of recovery from mental illness and/or addiction, plus skills learned in formal training, to deliver services in BH settings to promote mind-body recovery and resiliency.” A family advocate is a person whose “lived experience” is defined as having a family member who has a mental illness or substance use disorder and the knowledge of the BH care system gained through navigation and support of their family member. PSPs perform a wide variety of non-clinical tasks to assist members “in regaining control over their own lives and recovery”6 processes. The following is a useful overview of the four major types of recovery support services: (1) peer mentoring or coaching, (2) recovery resource connecting, (3) facilitating and leading recovery groups, and (4) building community.8 PSPs assist members in navigating treatment systems for mental health and substance use disorders. PSPs “promote self-determination, personal responsibility and the empowerment inherent in self-directed recovery.” | Colorado does not require a Peer Support Professional to be certified or licensed by DORA but to have formal training in specific content areas as outlined in Appendix P. |
| QBHA | Qualified Behavioral Health Assistant. This support professional, non-clinical role works under supervision to carry out activities such as wellness promotion and education, community needs assessment, screening, referrals, crisis management, case management, orientation to services & care navigation, and individual and group interventions.
| SB 22-181 Colorado does not require a Qualified Behavioral Health Assistant to be certified or licensed by DORA, but to have formal training through the Colorado Community College System (CCCS). |
| QMAP | Qualified Medication Administration Person. Successful completion of a State-approved medication administration course qualifies a QMAP to administer medications in settings authorized by law. A QMAP is employed by a licensed facility on a contractual, full- or part-time basis to provide direct care services, including medication administration to residents upon written order of a licensed physician or other licensed authorized practitioner. A QMAP may also be a person employed by a home health agency who functions as permanent direct care staff to licensed facilities, who is trained in medication administration, and who administers medication only to the residents of the licensed facility. | 6 CCR 1011-1, 24,2 |
| RN | Registered Nurse. Graduated from an approved program of professional nursing and is licensed as a Professional Nurse by the CO Board of Nursing | CRS 12-38-103 |
| RxN | Advanced Practice Nurse with Prescriptive Authority. Professional Nurse licensed by the CO Board of Nursing and who has been granted Prescriptive Authority by the CO Board of Nursing | 3 CCR 716-1-14, 1.14; CRS 12-38-111.5 and 12-38-111.6; |
| Unlicensed Ed/D, PhD, PsyD | Unlicensed Doctor of Education - provider possesses a Ed. D degree, doctoral level credentials. Received extensive training in research and/or clinical psychology but have not attained licensure by the CO Board of Psychologist Examiners Unlicensed Doctor of Psychology - provider possesses a Psy.D degree, doctoral level credentials. Received extensive training in research and/or clinical psychology but have not attained licensure by the CO Board of Psychologist Examiners Unlicensed Doctor of Philosophy - provider possesses a Ph. D degree, doctoral level credentials. Ph. D in philosophy signifies mastery of a broad discipline of learning together with demonstrated competence in a special field within that discipline | HB 21-1305 12-245-218 |
| Unlicensed Master Level | Unlicensed Master's Degree - provider has master's degree in a mental health field from an accredited college or university. Must be supervised in the provision of services by a Licensed Provider. Includes unlicensed psychotherapist | HB 19-1172 |
Room and Board services (lodging and meals) are provided to members residing in a facility for at least 24 hours. Room and board is not a covered Medicaid benefit and is not included in any per diem rate. Room and board are included in reimbursement when services are rendered in a hospital or PRTF and billed using a revenue code. BHA covers room and board for some Medicaid members when a facility is contracted with BHA for reimbursement. For example, RSATFs bill room and board to BHA or their designee for Medicaid members. BHA covers room and board for uninsured/ underinsured members in some settings when all contractual and safety net criteria is met by a provider. Check your BHA contract for more details.
Services that are ordered by a court (to include psychological testing, SUD treatment, residential care, etc.) are not automatically covered or excluded by Medicaid. Services must be covered under the Capitated BH Benefit and meet Medical Necessity criteria to be reimbursed by Medicaid.
Definition Of Medical Necessity
According to 10 CCR 2505-10 section 8.076.1.8, a service is considered medically necessary when it:
- Will, or is reasonably expected to prevent, diagnose, cure, correct, reduce, or ameliorate the pain and suffering, or the physical, mental, cognitive, or developmental effects of an illness, condition, injury, or disability. This may include a course of treatment that includes mere observation or no treatment at all. For members under age 21, per section 8.280.4E, this includes a reasonable expectation that the service will assist the member to achieve or maintain maximum functional capacity in performing one or more Activities of Daily Living.
- Is provided in accordance with generally accepted professional standards for healthcare in the United States.
- Is clinically appropriate in terms of type, frequency, extent, site, and duration.
- Is not primarily for the economic benefit of the provider or primarily for the convenience of the member, caretaker, or provider.\
- Is delivered in the most appropriate setting(s) required by the member's condition.
- Is not experimental or investigational; and
- Is not more costly than other equally effective treatment options.
Learn more about Medicaid Necessity.
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
Federal Medicaid law, 42 U.S.C.§ 1396d(r), requires state Medicaid programs to provide EPSDT benefits for members under 21 years of age. This means Medicaid is required to cover any service for members aged 20 or younger that is medically necessary “to correct or ameliorate a defect, physical or mental illness, or a condition identified by screening,” whether or not the service is covered under the Colorado State Medicaid Plan. “Ameliorate” means to “make more tolerable” or in other words, to improve or maintain the member’s health in the best condition possible, compensate for a health problem, prevent it from worsening, or prevent the development of additional health problems. Even if the service will not cure the member’s condition, it must be covered if it is medically necessary to improve or maintain the member’s overall health. The services covered under EPSDT are limited to those within the scope of the category of services listed in federal law at 42 U.S.C. § 1396d(a).
This means that EPSDT benefits include medically necessary treatments that a recipient under 21 years of age needs to stay as healthy as possible, and Medicaid must provide or arrange for (directly or through referral to appropriate agencies, organizations, or individuals) corrective treatment. EPSDT benefits are more robust than the adult Medicaid benefit package and include a separate medical necessity definition for services rendered to or requested for members under the age of 21, see 10 CCR 2505-10 § 8.280.4.E.
EPSDT makes short-term and long-term services available to all members under 21 years of age without many of the limits Medicaid imposes for services for members over the age of 21. The services must be prescribed by the member’s treating provider(s) and prior authorization may be required for some services.
The Medicaid Capitated Behavioral Health Benefit identifies covered diagnoses using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). The ICD-10-CM is the official system of assigning codes to diagnoses and procedures used by all health care settings, including hospitals, physicians, nursing homes (NH), home health agencies and other providers. ICD-10-CM code selection follows the Official ICD-10-CM Guidelines for Coding and Reporting, developed cooperatively by the American Hospital Association (AHA), the American Health Information Management Association (AHIMA), CMS, and the National Center for Health Statistics (NCHS). These guidelines are a companion document to the ICD-10-CM, and while not exhaustive, assist the user in situations where the ICD-10-CM does not provide direction. The ICD10-CM is updated annually, effective October 1st. The ICD-10-CM does not include diagnostic criteria, primarily because its principal function as an international system is to define categories that aid in the collection of basic health statistics. The Official ICD-10-CM Guidelines must be followed when submitting claims for payment. It is important to check all diagnosis codes for appropriate guidelines before submitting a claim. For example, diagnosis codes may have a required number of digits (must be coded to greatest specificity). While most diagnosis codes will not include diagnostic criteria, others will provide guidelines according to some clinical criteria (for example, F10.1 and F10.2, alcohol dependence vs. alcohol abuse which have distinct definitions and clinical indications).
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5), on the other hand, is the universal authority in the United States for diagnosing psychiatric disorders. Clinicians are encouraged to base their diagnostic decisions on DSM-5 criteria, and reference tables in the DSM-5 for ICD-10-CM insurance billing information. DSM-5 and the ICD are compatible with one another, and the DSM-5 contains a crosswalk to both ICD-9 and ICD-10 codes. The ICD–10-CM was implemented on October 1, 2015.
- Primary/Principal Diagnosis
Identifying the appropriate diagnosis that drives clinical treatment or other BH services is essential for many reasons. Beyond clinical considerations, as it relates to billing and coding, the diagnosis in the first position of a claim has significant impact. If an intervention is provided for a diagnosis not related to the condition indicated in the first position, it is possible the claim could be denied if the diagnosis is not covered under the Capitated Behavioral Health Benefit. A member may have a pervasive condition, a genetic disorder, or a chronic condition, as well as an episodic BH need. The diagnosis listed in the first position of a claim should be directly related to the service being provided regardless of any other co-occurring diagnosis.
- A Primary Diagnosis is the diagnosis the provider either conducted an evaluation for or was the reason for the specific treatment that is requested or submitted for reimbursement on a CMS 1500.
- A Principal Diagnosis is the condition established after study to be chiefly responsible for a member's admission to the hospital. It is always the first-listed diagnosis on the health record and the UB-04 claim form.
- Non-Covered Diagnoses
A covered diagnosis is required for reimbursement, unless it falls in one of the following categories: Screening, Assessment, Crisis, or Prevention/Early Intervention. (See Appendix I for specific codes allowed without a covered diagnosis.) For these services, a non-covered diagnosis may be reported when these services have been rendered to a Medicaid member for the purpose of evaluating and assessing to determine the presence of and/or diagnose a BH disorder(s). When no other diagnosis has been determined, R69 or Z03.89 may be used. These codes are specifically intended for use when persons without a diagnosis are suspected of having an abnormal condition, without signs or symptoms, which requires study, but after examination and observation, is found not to exist. - Covered Diagnoses
The tables below list the covered diagnoses under the Medicaid Capitated Behavioral Health Benefit. Codes that are not covered may be billed to a member’s MCO, or to FFS if the member is not enrolled with an MCO. BHA also covers the diagnosis codes in these tables, as well as additional codes. Contact your BHA program manager for the most current version of the CCAR Manual where additional BHA covered diagnosis codes can be found.
Effective January 1, 2024, for members under 21 years old, Autism Spectrum Disorder (F84.0-F84.9) are covered diagnoses for psychotherapy services only (90785, 90791, 90792, 90832, 90833, 90834, 90836, 90837, 90838, 90846, 90847, 90849,90853)
Covered Mental Health Diagnoses
Start Value | End Value |
| F20.0 | F69 |
| F90.0 | F98.4 |
| F98.8 | F99 |
| R45.1 | R45.2 |
| R45.5 | R45.82 |
Covered SUD Diagnoses
Start Value | End Value |
| F10.10 | F19.99 |
Covered SDOH Diagnoses for Members Under 21 when billing services covered under SB23-174 Coverage (see Appendix I for codes highlighted in BLUE)
Start Value | End Value |
| R45.0 | R45.75 |
| R45.81 | R45.84 |
| R45.850 | R45.89 |
R69 and Z03.89 | |
| Z55.0 | Z55.9 |
| Z56.0 | Z56.6 |
| Z56.81 | Z56.9 |
| Z58.81 | Z58.9 |
| Z59.00 | Z59.02 |
| Z59.10 | Z59.3 |
| Z59.41 | Z59.7 |
| Z59.811 | Z59.9 |
| Z60.0 | Z60.9 |
| Z62.0 | Z62.1 |
| Z62.21 | Z62.6 |
| Z62.810 | Z62.819 |
| Z62.820 | Z62.823 |
| Z62.831 | Z62.833 |
| Z62.890 | Z62.9 |
| Z63.0 | Z63.1 |
| Z63.31 | Z63.6 |
| Z63.71 | Z63.9 |
| Z64.0 | Z64.4 |
| Z65.0 | Z65.9 |
Claiming For Medicaid Services
This section outlines claim information for the Colorado Medicaid Capitated Behavioral Health
Benefit and is designed to assist providers with the key details to obtain Medicaid reimbursement. For more specific claiming instructions refer to the following RAE links:
| Colorado Regional Accountable Entities (RAEs) | ||
| Region 1 | Rocky Mountain Health Plans | https://www.rmhp.org |
| Region 2 | Northeast Health Partners | https://www.northeasthealthpartners.org/ |
| Region 3 | Colorado Community Health Alliance | https://www.cchacares.com |
| Region 4 | Colorado Access Denver Health | https://www.coaccess.com https://www.dhha.org |
- Responsibility for Code Assignments
Coding consistency is a major initiative in the quest to improve quality reporting and accurate claims submission for BH services. Adherence to industry standards and approved coding principles ensures quality along with consistency in the reporting of these services. The ultimate responsibility for procedure code assignment lies with the rendering provider. Policies and procedures may document instances where procedure codes may be selected and assigned by authorized individuals (i.e. coders), who may change a procedure code to more accurately reflect the provider’s documentation. However, collaboration with the provider is required, as the provider is ultimately responsible for the coding and documentation. - Approved Claim Formats
All claims for services must be submitted in an approved claim format. The two (2) approved claim formats are:- Institutional Claims - UB-04/837I (Also known as CMS-1450)
Institutional claims are submitted on the UB-04 paper format. The 837I is the electronic equivalent of the UB-04 and is subject to all HIPAA standards (transactions, privacy, and security). The UB-04 is used for all institutional provider billing with the exception of the professional component of physician’s services (see CO-1500 below). The following provider types use the UB-04/837I claim form:- Inpatient Hospital
- Nursing Facility
- Home Health/Private Duty Nursing
- Hospice
- Psychiatric Residential Treatment Facility
- Dialysis Center
- Outpatient Hospital
- Outpatient Laboratory
- Hospital-Based Transportation
- Rural Health Clinic
- Federally Qualified Health Center
- Professional Claims - CO-1500/837P (Formerly known as CMS-1500)
The 1500 claim form was developed primarily for outpatient services. These professional health service claims are submitted on a paper CMS-1500 claim form or in the electronic 837 Professional 4010A1 (837P) format. Paper CMS-1500 forms must be submitted using the scanned, red ink version. The following services are billed on the CO-1500/837P claim format:- Practitioner Services
- Independent Laboratory Services
- Durable Medical Equipment and Supplies (DME)
- Non-Hospital Based Transportation
- Home and Community-Based Services (HCBS)
- Residential services described in Appendix C and billed using a code with a Residential primary category listed in Appendix I. [Although these are not outpatient services, they do not include room and board and are viewed as professional services]
For detailed instructions on completing the CMS-1500, refer to the Colorado MAP Billing Manuals;8 the National Uniform Claim Committee (NUCC) 1500 Claim Form Map to the X12 837 Health Care Claim: Professional.9 the 837P Transaction Data Guide; the 837P Implementation Guide or the Web Portal User Guide; and/or the appropriate RAE provider manual.
For detailed instructions on completing the UB-04, refer to the Colorado MAP Billing Manuals; the 837I Transaction Data Guide; the 837I Implementation Guide or the Web Portal User Guide; and/or the appropriate RAE provider manual.
All services provided to the same member on the same day at the same location (enrolled with HCPF under a common NPI) shall be billed on a single claim. Each line/service on a claim can indicate a distinct rendering provider as appropriate.
To document the place of service (POS) on a CMS 1500 when a clinician provides services in a community setting, Box 24B "Place of Service" should contain the most precise CMS POS indicator. When the community setting has no NPI (i.e. city park, restaurant, etc.) Box 32 "Service Facility Location Information" should contain the address and NPI of the clinician's office/home location. If the Service Facility location is the same address as that reported in the Billing Provider Name, the Service Facility Location must not be sent.
- Institutional Claims - UB-04/837I (Also known as CMS-1450)
Hospital services provided to a Medicaid member attributed to an MCE for a primary BH Diagnosis covered by an MCE are covered under the Capitated Behavioral Health Benefit according to the following parameters. MCEs have the responsibility to ensure these services are medically necessary and may deny a claim for this reason. Providers are able to appeal any claims denials.
- Professional services provided in an inpatient hospital, outpatient hospital, or emergency room setting billed on a CMS-1500/ANSI 837-P claim form when the procedure(s) is listed in the State Behavioral Health Services (SBHS) Billing Manual.
- Outpatient hospital services billed on a UB-04/ANSI 837-I X12 claim form that do not include a behavioral health service but are for a primary behavioral health diagnosis.
- Intensive Outpatient Program (IOP) services performed in an outpatient hospital setting when the procedure is billed on a UB-04/ANSI 837-I X12 claim form.
- Emergency room services for a primary mental health diagnosis billed on a UB-04/ANSI 837-I X12 claim form.
- All inpatient services for a primary mental health diagnosis billed on a UB-04/ANSI 837-I X12 claim form, this includes all psychiatric and associated medical and facility services, labs, x-rays, supplies, occupational, physical, and speech therapy services, and other ancillary services. Split billing for behavioral health services provided in an inpatient setting is not permitted.
Exclusions:
- Outpatient emergency room services for a primary SUD diagnosis billed on a UB-04/ANSI 837-I X12 claim form are billed fee-for-services (FFS).
- All inpatient services for a primary SUD diagnosis billed on a UB-04/ANSI 837-I X12 claim form for ASAM level 4 criteria are billed FFS.
- Hospital services billed on a UB-04/ANSI 837-I X12 claim form for a primary diagnosis of Autism Spectrum Disorder (F84.0-F84.9) are billed FFS. ASD is only considered a RAE-covered diagnosis for psychotherapy services for members under 21 years old.
- Hospital services billed on a UB-04/ANSI 837-I X12 claim form for a primary diagnosis of Gender Dysphoria (F64.0-F64.9) are billed FFS. This is addressed in the Gender Affirming Care billing manual here.
- Occupational Therapy (OT), Physical Therapy (PT), and Speech Therapy (ST) billed on a CMS1500/ANSI 837-P claim form are billed FFS regardless of diagnosis.
Licensed Provider Claiming Under a Supervisor
Practitioners who are enrolled with Medicaid and have applied for credentials with a Regional Accountable Entity (RAE) may submit claims under a supervising provider for a maximum of 90 days while completing contracting with a RAE. This policy applies to:
- Newly licensed BH providers who were providing services to members under clinical supervision while they were working toward licensure.
- Licensed BH providers who are hired by a group practice.
Medicaid cost sharing is only permitted as specified in sections 1902(a)(14), 1916 and 1916A of the Social Security Act and their implementing regulations at 42 CFR 447.50-57. Cost sharing under those statutes and regulations is only permissible for services under the state plan. There are no procedure codes for missed appointments (i.e. cancellations and/or “no shows”). A missed appointment is a “non-service” and is not reimbursable or reportable. From a risk management perspective, however, missed appointments should be documented in the clinical record.
Health First Colorado Behavioral Health Rendering Provider Oversight (RPO) Policy
This policy was updated on December 5, 2025.
The Department of Health Care Policy and Financing (HCPF) has developed standards and practices to permit pre-licensed clinicians and unlicensed professionals to deliver behavioral health services to Health First Colorado (Colorado’s Medicaid program) members and seek reimbursement from a Health First Colorado Regional Accountable Entity (RAE) or reimbursement from HCPF in the case of certain services covered by the 1115 Waiver. This policy promotes quality member care, while supporting efforts to expand the workforce, reduce burnout, and improve access to care.
Under federal Medicaid policies, pre-licensed clinicians and unlicensed professionals are not able to independently deliver Medicaid reimbursable behavioral health services because they do not hold a valid active license in Colorado. In order to reimburse for care delivered by these individuals, their services must be billed under a Rendering Provider.
From July - September 2025, more than 600 stakeholders and advocates shared valuable suggestions, observations, and recommendations regarding the draft Supervision Policy for Medicaid Billable Behavioral Health Services. The Summary of Stakeholder Feedback on the Supervision Policy for Medicaid Billable Behavioral Health Services outlines suggestions, observations and recommendations that HCPF received. HCPF appreciates all of the feedback that was provided and has integrated recommendations from each category into the revised policy. Based on one of the most common recommendations, HCPF renamed the policy to better reflect its purpose and scope. The final policy is linked below:
Health First Colorado Behavioral Health Rendering Provider Oversight (RPO) Policy
FAQ Regarding Rendering Provider Oversight of Medicaid Billable Services
All Medicaid enrolled providers who are subject to this policy must submit this attestation annually by January 1st to any RAE the billing provider is contracted with, confirming adherence to rules and standards outlined in the policy.
Providers delivering 1115 Waiver services that are billed fee-for-service should submit the attestation to HCPF via email: hcpf_bhbenefits@state.co.us
Time Documentation Standards/Rules
When documenting, reporting and/or billing CPT® or HCPCS procedure codes, the units of service should be consistent with the time component defined in the procedure code description. CPT® and HCPCS procedure codes include both “timed” and “untimed” procedure codes.
“Timed” procedure codes specify a direct time increment in the procedure code description. The direct time component is only that time spent with the member and/or family in a billable activity. Non-direct time (i.e., pre-, and post-encounter time, drive time with the member to an encounter, etc.) is not included in the calculation of the time component. Examples of time-specific services are psychological testing (1 hour), psychotherapy (from 20 – 30 minutes up to 70 – 80 minutes), and case management (15 minutes).
“Untimed” procedure codes do not include specific direct time increments in the procedure code description. These procedure codes represent a service or procedure without regard to the length of the encounter. If there is no designated time in the procedure code description, the procedure code is reported or billed as one (1) unit (i.e., session, encounter), regardless of the number of minutes spent rendering the service. Examples of “untimed” services are psychiatric diagnostic interview exam, and medication management.
A unit of time is attained when the mid-point is passed. For example, an hour is attained when 31 minutes have elapsed (more than midway between zero and sixty minutes). A second hour is attained when a total of 91 minutes has elapsed.
Fifteen (15) Minute Time-Based Procedure Codes
Some CPT® and HCPCS procedure codes specify that the direct time spent in member contact is 15 minutes. The provider reports or bills these procedure codes with the appropriate number of 15-minute units of service using the following time intervals:Determining Billing Units for 15 Minute Timed Procedure Codes # of 15 Minute Units Duration 1 unit Greater than or equal to 8 minutes and less than 23 minutes 2 units Greater than or equal to 23 minutes and less than 38 minutes 3 units Greater than or equal to 38 minutes and less than 53 minutes 4 units Greater than or equal to 53 minutes and less than 68 minutes 5 units Greater than or equal to 68 minutes and less than 83 minutes 6 units Greater than or equal to 83 minutes and less than 98 minutes 7 units Greater than or equal to 98 minutes and less than 113 minutes 8 units Greater than or equal to 113 minutes and less than 127 minutes The pattern continues in the same way for service times in excess of two (2) hours. For all services, providers should not report, or bill services rendered for less than eight (8) minutes. For case management services (T1017 and H0006) providers may not bill services rendered for less than eight (8) minutes, however bundling of these services is acceptable.
While the above table provides guidance in rounding time into 15-minute increments, it does not imply that any minute until the eighth should be excluded from the total count. The time of direct treatment includes all time spent in member contact. The start and end time of the treatment service should be routinely documented in the member’s clinical record as part of the progress note.
One-Hour Time-Based Procedure Codes
Some CPT and HCPCS procedure codes specify that the direct time spent in member contact is 1 hour. The provider reports or bills these procedure codes with the appropriate number of 1-hour units of service using the example time intervals given in the table below. The pattern continues in this manner.Determining Billing Units for 1-hour or 60 Minutes Timed Procedure Codes # of 60 Minute Units Duration 1 unit Greater than or equal to 31 minutes and less than 91 minutes 2 units Greater than or equal to 91 minutes and less than 151 minutes 3 units Greater than or equal to 151 minutes and less than 211 minutes 4 units Greater than or equal to 211 minutes and less than 271 minutes 5 units Greater than or equal to 271 minutes and less than 331 minutes 6 units Greater than or equal to 331 minutes and less than 391 minutes 7 units Greater than or equal to 391 minutes and less than 451 minutes - Encounter Time-Based Procedure Codes
Some CPT® and HCPCS procedure codes are reported as encounters (1 unit), but also specify an approximate amount of direct time in the procedure code description. For example, the CPT® procedure codes 90832 – 90838 for individual psychotherapy state “approximately ‘x’ minutes direct contact with the member.” HCPCS procedure codes G0176 – G0177 for partial hospitalization program (PHP) activity therapy and training and education services parenthetically state “45 minutes or more.” The actual start and stop time or the total amount of time (i.e. duration) spent with a member must be documented to support coding for encounters based on time. - Per Diem Procedure Codes
Some CPT® and HCPCS procedure codes are reported by “day” units (per diem). This is defined by a calendar day and may or may not have a minimum duration indicated on the coding page. A per diem code should be claimed for the date of admission even if the member discharged the same day, and regardless of the amount of time the member was actually at the facility/program. A per diem code should not be claimed for the date of discharge unless it was the same date as the admission.
Current Procedural Terminology (CPT) Service Categories
Each CPT code falls into one of ten primary categories of service, or “Service categories”. These categories are not listed on the individual SBHS Billing Manual pages but can be found in Appendix I.
Prevention/Early Intervention Services
Prevention and Early Intervention Services include “screening and outreach to identify at-risk populations, proactive efforts to educate and empower Members to choose and maintain healthy life behaviors and lifestyles that promote behavioral health. Services can be population-based, including peer, and group interventions, and are not restricted to face-to-face interventions.” Prevention and Early Intervention Services include:
- Mental health (MH) screenings
- Nurturing Parent Program
- Educational programs (safe and stable families)
- Senior workshops (common aging disorders)
- “Love and Logic” (healthy parenting skills)
- CASASTART (children at high risk for substance abuse (SA), delinquency, and academic failure)
Crisis Services
Crisis/Emergency Services are “provided during a MH emergency, which can involve unscheduled, immediate, or special interventions in response to a crisis with a member, including associated laboratory services, as indicated.” Services are designed to:
- Improve or minimize an acute crisis episode
- Assist the member in maintaining or recovering his/her level of functioning (LOF) by providing immediate intervention and/or treatment in a location most appropriate to the needs of the member and in the least restrictive environment available
- Prevent further exacerbation or deterioration and/or inpatient hospitalization, where possible
- Prevent injury to the member and/or others
- Stabilization is emphasized so that the member can actively participate in needs assessment and treatment/ service planning. Services are characterized by the need for highly coordinated services across a range of service systems. Crisis/Emergency Services are available on a 24-hour, 7-day a week basis.
Screening Services
Screening is provided to address the needs of those seeking BH treatment services in a timely manner. This brief assessment involves an initial appraisal of an individual’s need for services. If there are sufficient indications of a MI and/or substance-related disorder, further diagnostic assessment is warranted to determine the individual’s eligibility for admission to BH treatment services, as well as appropriate referrals and preliminary recommendations. Additionally, substance use screening can be used as a part of treatment. Screening services are often performed through specimen collection to test for the presence of alcohol and/or drugs. Results are discussed with the member during a Substance Use counseling session. Screenings often provide members with personal feedback about their increased risks due to substance use and may identify problems that can prompt individuals to change their substance use behavior.
Assessment Services
Assessment Services are the process, both initial and ongoing, of collecting and evaluating information about a member for developing a profile on which to base treatment/service planning and referral (2 CCR 502-1, 190.1). An Assessment may also use a diagnostic tool to gather the information necessary in the Assessment Services process. These can include services related to Diagnosis, Psychological Testing/Neuropsychological Testing, or Treatment/Service Planning.
Treatment Services
Treatment services utilize a variety of methods to treat mental, behavioral, and substance use disorders. The goal is to alleviate emotional disturbances and reverse or change maladaptive patterns of behavior in order to encourage a member’s personal growth and development. Treatment services often utilize assessments to formulate and implement an individualized comprehensive written treatment/service plan that is used to promote the member’s highest possible level of independent functioning. For SUD diagnoses, treatment can include relapse planning, information about the process of addiction, and assist members to understand some of the underlying issues that lead them to use substances. Services that can be provided under this category can include Psychotherapy (individual, group, or family), Medication Management, Substance Use Treatment Services, Rehabilitation Services, Inpatient Services, Targeted Case Management (TCM) Services, Vocational Services, Intensive Treatment Services, Consultation Services, Medical Team Conference, or Other Professional Services.
Evaluation and Management (E/M) Services
E/M codes cover a broad range of services for members in both inpatient and outpatient settings. They are generic in the sense that they are intended to be used by all physicians, nurse practitioners, and physician assistants and to be used in primary and specialty care alike. For E/M codes covered under the Capitated BH Benefit see Appendix E in the SBHS Billing Manual.
DEFINITIONS:
- New patient: A new patient is defined as one who has not received any professional services from the prescriber or another prescriber of the exact same specialty and subspecialty who belongs to the same group within the past 3 years.
- Established patient: An established patient is one who has received professional services from the prescriber or another prescriber of the exact same specialty and subspecialty who belongs to the same group within the past 3 years.
There is no distinction made between new and established patients in the emergency Department.
Residential Services
Residential Services are any type of 24-hour care, excluding room and board, provided in a nonhospital, non-nursing home (NH) setting, where the contractor provides supervision in a therapeutic environment. Residential Services are appropriate for children, youth, adults and older adults whose MH issues and symptoms are severe enough to require a 24-hour structured program, but do not require hospitalization.”
Respite Care Services
Respite Care Services are Temporary or short-term care of a child, adolescent or adult provided by adults other than the birth parents, foster parents, adoptive parents, family members or caregivers with whom the Member normally resides, designed to give the usual caregivers some time away from the Member to allow them to emotionally recharge and become better prepared to handle the normal day-to-day challenges.” This service acknowledges that, while the services of primary caregivers may keep a member out of more intensive levels of care (i.e., inpatient hospital), there are occasional needs to substitute for these caregivers. Respite Care Services may be rendered when:
- The member’s primary caregivers are unable to provide the necessary illness-management support and thus the member is in need of additional support or relief
- The member and his/her primary caregivers experience the need for therapeutic relief from the stresses of their mutual cohabitation
- The member is experiencing a behavioral crisis and needs structured, short-term support
- Relief care giving is necessitated by unavoidable circumstances, such as a family emergency
Peer Support/Recovery Services
Peer Support/Recovery Services are “designed to provide choices and opportunities for adults with SMIs, youth with SEDs, or individuals with SUDs. Recovery-oriented services promote self-management of psychiatric symptoms, relapse prevention, treatment choices, mutual support, enrichment, and rights protection. Peer Support/Recovery Services also provide social supports and a lifeline for individuals who have difficulties developing and maintaining relationships. These services can be provided at schools, churches, or other community locations. Most recovery services are provided by BH peers or family members, whose qualifications are having a diagnosis of MI or substance use or being a family member of a person with MI and/or substance use.” Peer Support/Recovery Services include:
- Peer counseling and support services
- Peer-run drop-in centers
- Peer-run employment services
- Peer mentoring for children and adolescents
- Bipolar Education and Skills Training (BEST) courses
- National Alliance on Mental Illness (NAMI) courses
- Wellness Recovery Action Plan (WRAP) groups
- Member and family support groups
- Warm lines
- Advocacy services
Support Services
Support Services are not clinical but help facilitate a psychotherapy encounter and include such supports as childcare for a member receiving clinical care, Non-Emergent Medical Transportation (NEMT), and sign language services.
The Medicaid State Plan is the document by which the State of Colorado certifies that it will comply with all Federal requirements for Medicaid. Some of the requirements are identical for all states, and some permit the State to choose certain options. To be eligible to receive federal matching funds (Federal Financial Participation or FFP) to operate its Medicaid program, the State must agree to comply with all parts of the Medicaid State Plan on file with the Centers for Medicare and Medicaid Services (CMS).
Inpatient Services include:
- Inpatient hospital – under 21: a program of care for members under age twenty-one (21) in which the member remains twenty-four (24) hours a day in a psychiatric hospital, or other facility licensed as a hospital by the state. Members who are inpatient on their twenty-first birthday are entitled to receive inpatient benefits until discharged from the facility or until their twenty-second (22) birthday, whichever is earlier, as outlined in 42 CFR 441.151.
- Inpatient hospital – adult 21-64: a program of psychiatric care in which the member remains twenty-four (24) hours a day in a facility licensed as a hospital by the state, excluding state institutions for mental disease (IMDs).
- Inpatient hospital – 65 and over: a program of care for members age sixty-five (65) and over in which the member remains twenty-four (24) hours a day in institutions for mental diseases (IMD) or other facility licensed as a hospital by the state.
SUD Inpatient and Residential Services are Substance Use Disorder (SUD) treatment and withdrawal management services, including services along the continuum of care defined by the American Society of Addiction Medicine (ASAM). Services are provided to Medicaid beneficiaries with one or more diagnosed SUD(s). Services are determined according to medical necessity which include an assessment of level of clinical severity and function.
Outpatient Services are a program of care in which the member receives services in a hospital or other health care facility/office, but does not remain in the facility twenty-four (24) hours a day,
including:
- Physician Services, including psychiatric care: BH services provided within the scope of practice of medicine as defined by State law.
- Rehabilitative Services: Any remedial services recommended by a physician or other licensed practitioner of the healing arts, within the scope of his/her practice under State law, for maximum reduction of behavioral/emotional disability and restoration of a member to his/her best possible functional level, including:
- Individual BH Therapy: Therapeutic contact with one member.
- Individual Brief BH Therapy: Therapeutic contact with one member.
- Group BH Therapy: Therapeutic contact with more than one member.
- Family BH Therapy: Therapeutic contact with a member and family member(s), or other persons significant to the member, for improving member-family functioning.
- Family BH therapy is appropriate when intervention in the family interactions is expected to improve the member’s emotional/BH. The primary purpose of family BH therapy is treatment of the member.
- Behavioral Health Assessment: Clinical assessment of a member by a BH professional that determines the nature of the member’s problem(s), factors contributing to the problem(s), a member’s strengths, abilities, and resources to help solve the problem(s), and any existing diagnoses.
- Pharmacologic Management: Monitoring of medications prescribed, and consultation provided to members by a physician or other medical practitioner authorized to prescribe medications as defined by State law, including associated laboratory services, as indicated
- Outpatient Day Treatment: Therapeutic contact with a member in a structured, nonresidential program of therapeutic activities. Services include assessment and monitoring; individual/ group/ family therapy; medical/nursing support; psychosocial education; skill development and socialization training focused on improving functional and behavioral deficits; medication management; expressive and activity therapies; and coordination of needed services with other agencies. When provided in an outpatient hospital program, may be called "partial hospitalization."
- Emergency/Crisis Services: Services provided during a BH emergency which involve unscheduled,immediate, or special interventions in response to crisis situation with a member/family, including associated laboratory services, as indicated.
- Pharmacy Services: Prescribed drugs when used in accordance with 10 CCR 2505-10 Section 8.800, Pharmaceuticals.
- Targeted Case Management: Case management services furnished to assist individuals, eligible under the State Plan, in gaining access to needed medical, social, educational, and other services.
- School-Based BH Services: BH services provided to school-aged children and adolescents onsite in their schools with the cooperation of the schools.
- Drug Screening and Monitoring: Substance use disorder counseling services provided along with screening results to be discussed with member.
- Medication-Assisted Treatment: Administration of Methadone or another approved controlled substance to an opiate-dependent person for the purpose of decreasing or eliminating dependence on opiate substances.
Medicaid 1915(B)(3) Waiver Services
Colorado’s Medicaid Capitated Behavioral Health Benefit is operated under a 1915(b)(3) waiver. This waiver allows Colorado to offer alternative services (in addition to those identified under the State Plan) under a regional Managed Care model. These alternative services and the waiver itself are subject to approval by CMS.
1915 B3 Waiver Services are also called “alternative” services because these are alternatives to inpatient level of care. Alternative services are intended to serve adults with Serious Mental Illness (SMI) diagnoses or children/adolescents with a Serious Emotional Disturbance (SED) diagnosis in order to keep them supported and living in the community. Alternative services are BH services not included in our State Plan. However, each State must ensure that all BH services covered under the State Plan are available and accessible to enrollees of the 1915 B3 Waiver Program. Alternative services are broken down into 8 categories:
- Prevention/Early Intervention services are proactive efforts to educate and empower individuals to choose and maintain healthy life behaviors and lifestyles that promote positive psychological health.
- Prevention and early intervention efforts include services such as BH screenings, the Nurturing Parent Program, educational programs promoting safe and stable families, senior workshops related to common aging disorders, and Love and Logic classes for healthy parenting skills.
- Respite Care is temporary or short-term care of a child, youth or adult client that is provided by adults other than the birth parents, foster parents, adoptive parents, family members or caregivers that the client normally resides with, that is designed to give the parents, family members or caregivers some time away from the client, to allow them to emotionally recharge and become better prepared to handle the normal day-to-day challenges.
- Intensive Case Management describes community-based services averaging more than one hour per week, provided to adults with serious behavioral health diagnoses who are at risk of hospitalization, incarceration and/or homelessness due to multiple needs and impaired level of functioning. Services are designed to provide adequate supports to ensure community living.
- Services are assessment, service plan development, multi-system referrals, assistance with obtaining wrap-around services and supportive living services, monitoring and follow-up.
- Vocational Services are services designed to assist adults and adolescents who are ineligible for state vocational rehabilitation services and require long-term services and supports in developing skills consistent with maintaining employment and/or in obtaining employment.
- Services are skill and support development interventions, vocational assessment, and job coaching.
- Recovery Services are designed to provide choices and opportunities for adults with serious behavioral health disorders. Recovery-oriented services promote self-management of psychiatric symptoms, focus on relapse prevention, treatment choices, mutual support, enrichment, and rights protection. Recovery services also provide social supports and a lifeline for individuals who have difficulties developing and maintaining relationships. These services can be provided at schools, churches, or other community locations.
- Recovery services are peer counseling and support services, peer-run drop-in centers, peer-run employment services, peer mentoring for children and adolescents, Bipolar Education and Skills Training (BEST) courses, National Alliance for the Mentally Ill (NAMI) courses, Wellness Recovery Action Planning (WRAP) groups, consumer and family support groups, warm lines, and advocacy services.
- Clubhouses and drop-in center services are peer support services for people who have BH disorders, provided in Clubhouses and drop-in centers. In Clubhouses, individuals (members) utilize their skills for clerical work, data input, meal preparation, providing resource information or reaching out to fellow members. Staff and members work side by side, in a unique partnership.
- In drop-in centers, members plan and conduct programs and activities in a club-like setting. There are planned activities and opportunities for individuals to interact with social groups.
- Assertive Community Treatment (ACT) is a service-delivery model that provides comprehensive, community-based treatment to adults with a serious behavioral health diagnosis. Services are highly individualized and are available 24 hours a day, seven days a week, 365 days a year to clients who need significant assistance and support to overcome the barriers and obstacles that confront them.
- ACT teams provide case management, initial and ongoing BH assessments, psychiatric services, employment and housing assistance, family support and education, and substance use disorder services.
- Residential Services are defined as twenty-four (24) hour care, excluding room and board, provided in a non-hospital, non-nursing home setting, and are appropriate for individuals members) whose BH issues and symptoms are severe enough to require a 24-hour structured program but do not require hospitalization. Residential services are a variety of clinical interventions that, individually, may appear to be similar to traditional state plan services. By virtue of being provided in a setting where the client is living, in real-time (i.e. with immediate intervention possible), residential services become a unique and valuable service in their own right that cannot be duplicated in a non-structured community setting. These clinical interventions, coupled together, in real-time, in the setting where a client is living, become a tool for treating individuals in the most cost-effective manner and in the least restrictive setting.
- Clinical interventions provided in this setting are: assessment and monitoring of mental and physical health status; assessment and monitoring of safety, including suicidal ideation and other BH issues; assessment of level and quality of social interactions; assessment of/support for motivation for treatment; assessment of ability to provide for daily living needs; observation and assessment of group interactions; behavioral interventions to build effective social behaviors and coping strategies; behavioral interventions to reduce social withdrawal and inappropriate behaviors or thought processes; individual therapy; group therapy; family therapy; and medication management.
Medicaid Place of Service Codes
Code | Name | Description |
|---|---|---|
01 | Pharmacy | A facility or location where drugs and other medically related items and services are sold, dispensed, or otherwise provided directly to members. |
02 | Telehealth Provided Other than in Member’s Home | The location where health services and health related services are provided or received, through telecommunication technology. Member is not located in their home when receiving health services or health related services through telecommunication technology. |
03 | School | A facility whose primary purpose is education. |
04 | Homeless Shelter | A facility or location whose primary purpose is to provide temporary housing to homeless individuals (e.g., emergency shelters, individual or family shelters). |
05 | Indian Health Service (IHS) Free- Standing Facility | A facility or location, owned and operated by the Indian Health Service (IHS), which provides diagnostic, therapeutic (surgical and non- surgical), and rehabilitation services to American Indians and Alaska Natives who do not require hospitalization. |
06 | Indian Health Service (IHS) Provider- Based Facility | A facility or location, owned and operated by the IHS, which provides diagnostic, therapeutic (surgical and non-surgical), and rehabilitation services rendered by, or under the supervision of, physicians to American Indians and Alaska Natives admitted as inpatients or outpatients. |
07 | Tribal 638 Free- Standing Facility | A facility or location owned and operated by a federally recognized American Indian or Alaska Native tribe or tribal organization under a 638 agreement, which provides diagnostic, therapeutic (surgical and non-surgical), and rehabilitation services to tribal members who do not require hospitalization. |
08 | Tribal 638 Provider-Based Facility | A facility or location owned and operated by a federally recognized American Indian or Alaska Native tribe or tribal organization under a 638 agreement, which provides diagnostic, therapeutic (surgical and non-surgical), and rehabilitation services to tribal members admitted as inpatients or outpatients. |
09 | Prison/Correction al Facility | A prison, jail, reformatory, work farm, detention center, or any other similar facility maintained by either federal, State or local authorities for the purpose of confinement or rehabilitation of adult or juvenile criminal offenders. Medicaid will not reimburse for services provided to a person living in a public institution that is the responsibility of a governmental unit or over which a governmental unit exercises administrative control (42 CFR 435.1010). Public institutions include correctional institutions. |
| 10 | Telehealth Provided in Member’s Home | The location where health services and health related services are provided or received through telecommunication technology. Member is located in their home (which is a location other than a hospital or other facility where the member receives care in a private residence) when receiving health services or health related services through telecommunication technology. |
| 11 | Office | Location, other than a hospital, skilled nursing facility (SNF), military treatment facility, community health center, State or local public health clinic, or intermediate care facility (ICF), where the health professional routinely provides health examinations, diagnosis, and treatment of illness or injury on an ambulatory basis. |
| 12 | Home | Location, other than a hospital or other facility, where the member receives care in a private residence. |
| 13 | Assisted Living Facility (ALF) | Congregate residential facility with self-contained living units providing assessment of each resident’s needs and on-site support 24-hours a day, 7 days a week, with the capacity to deliver or arrange for services, including some health care and other services. |
| 14 | Group Home | A residence, with shared living areas, where members receive supervision and other services, such as social and/or behavioral services, custodial service, and minimal services (e.g., medication administration). |
| 15 | Mobile Unit | A facility/unit that moves from place-to-place equipped to provide preventive, screening, diagnostic, and/or treatment services. |
| 16 | Temporary Lodging | A short-term accommodation such as a hotel, campground, hostel, cruise ship or resort where the member receives care, and which is not identified by any other POS code. |
| 17 | Walk-in Retail Health Clinic | A walk-in health clinic, other than an office, urgent care facility, pharmacy or independent clinic and not described by any other Place of Service code, that is located within a retail operation and provides, on an ambulatory basis, preventive, and primary care services |
| 18 | Place of Employment- Worksite | A location, not described by any other POS code, owned, or operated by a public or private entity where the member is employed, and where a health professional provides on-going or episodic occupational medical, therapeutic, or rehabilitative services to the individual |
| 19 | Off Campus- Outpatient Hospital | A portion of an off-campus hospital provider-based department which provides diagnostic, therapeutic (both surgical and nonsurgical), and rehabilitation services to sick or injured persons who do not require hospitalization or institutionalization |
| 20 | Urgent Care Facility | A location, distinct from a hospital emergency room, an office or a clinic, whose purpose is to diagnose and treat illness or injury for unscheduled, ambulatory members seeking immediate medical attention. |
| 21 | Inpatient Hospital | A facility, other than psychiatric, which primarily provides diagnostic, therapeutic (both surgical and non-surgical), and rehabilitation services by, or under the supervision of physicians to members admitted for a variety of medical conditions. |
| 22 | Outpatient Hospital | A portion of a hospital which provides diagnostic, therapeutic (both surgical and non-surgical), and rehabilitation services to sick or injured persons who do not require hospitalization or institutionalization. |
| 23 | Emergency Room - Hospital | A portion of a hospital where emergency diagnosis and treatment of illness or injury is provided. |
| 24 | Ambulatory Surgical Center | A free-standing facility, other than a physician’s office, where surgical and diagnostic services are provided on an ambulatory basis. |
| 25 | Birthing Center | A facility, other than a hospital’s maternity facilities or a physician’s office, which provides a setting for labor, delivery, and immediate post-partum care, as well as immediate care of newborn infants. |
| 26 | Military Treatment Facility (MTF) | A medical facility operated by one or more of the Uniformed Services. MTF also refers to certain former US Public Health Service (USPHS) facilities now designated as Uniformed Service Treatment Facilities (USTF). |
| 27 | Outreach Site/Street | A non-permanent location on the street or found environment, not described by any other POS code, where health professionals provide preventive, screening, diagnostic, and/or treatment services to unsheltered homeless individuals. |
28-30 | Unassigned | N/A |
31 | Skilled Nursing Facility (SNF) | A facility which primarily provides inpatient skilled nursing care and related services to members who require medical, nursing, or rehabilitative services, but does not provide the level of care or treatment available in a hospital. |
32 | Nursing Facility (NF) | A facility which primarily provides to residents skilled nursing care and related services for the rehabilitation of injured, disabled, or sick persons, or on a regular basis health-related care services above the level of custodial care to other than individuals with mental retardation. |
33 | Custodial Care Facility (CCF) | A facility which provides room, board, and other personal assistance services, generally on a long-term basis, and which does not include a medical component. |
34 | Hospice | A facility, other than a member’s home, in which palliative and supportive care for terminally ill members and their families are provided. |
35-40 | Unassigned | N/A |
41 | Ambulance – Land | A land vehicle specifically designed, equipped, and staffed for lifesaving and transporting the sick or injured. |
42 | Ambulance – Air or Water | An air or water vehicle specifically designed, equipped, and staffed for lifesaving and transporting the sick or injured. |
43-48 | Unassigned | N/A |
49 | Independent Clinic | A location, not part of a hospital and not described by any other POS code, that is organized and operated to provide preventive, diagnostic, therapeutic, rehabilitative, or palliative services to outpatients only. |
50 | Federally Qualified Health Center (FQHC) | A facility located in a medically underserved area that provides Medicare beneficiaries preventive primary medical care under the general direction of a physician. |
51 | Inpatient Psychiatric Facility (IPF) | A facility that provides inpatient psychiatric services for the diagnosis and treatment of mental illness on a 24-hour basis, by or under the supervision of a physician. |
52 | Psychiatric Facility – Partial Hospitalization (PF – PHP) | A facility for the diagnosis and treatment of mental illness that provides a planned therapeutic program for members who do not require full- time hospitalization, but who need broader programs than are possible from outpatient visits to a hospital-based or hospital-affiliated facility. |
53 | Community Mental Health Center/ Clinic (CMHC) | A facility that provides the following services: outpatient services, including specialized outpatient services for children, the elderly, individuals who are chronically ill, and residents of the CMHC’s mental health services area who have been discharged from inpatient treatment at a mental health facility; 24-hours a day emergency care services; day treatment, other partial hospitalization services, or psychosocial rehabilitation services; screening for members being considered for admission to State mental health facilities to determine the appropriateness of such admission; and consultation and education services. Effective 7/1/2024 Comprehensive Safety Net Providers (PT 78) should use POS 53 when the location of service is not described by any other POS code. |
54 | Intermediate Care Facility – Mentally Retarded (ICF-MR) | A facility which primarily provides health-related care and services above the level of custodial care to individuals with MR but does not provide the level of care or treatment available in a hospital or SNF. |
55 | Residential Substance Abuse Treatment Facility (RSATF) | A facility which provides treatment for substance (alcohol and drug) abuse to live-in residents who do not require acute medical care. Services include individual and group therapy and counseling, family counseling, laboratory tests, medications and supplies, psychological testing, and room and board. |
56 | Psychiatric Residential Treatment Center (PRTC) | A facility or distinct part of a facility for psychiatric care which provides a total 24-hour therapeutically planned and professionally staffed group living and learning environment. |
57 | Non-Residential Substance Abuse Treatment Center (NRSATC) | A location which provides treatment for substance (alcohol and drug) abuse on an ambulatory basis. Services include individual and group therapy and counseling, family counseling, laboratory tests, medications and supplies, and psychological testing. |
58-59 | Unassigned | N/A |
60 | Mass Immunization Center | A location where providers administer pneumococcal pneumonia influenza virus vaccinations and submit these services as electronic media claims, paper claims, or using the roster billing method. This generally takes place in a mass immunization setting, such as a public health center, pharmacy, or mall, but may include a physician office setting. |
61 | Comprehensive Inpatient Rehabilitation Facility (CIRF) | A facility that provides comprehensive rehabilitation services under the supervision of a physician to inpatients with physical disabilities. Services include physical therapy, occupational therapy, speech pathology, social or psychological services, and orthotics and prosthetics services. |
62 | Comprehensive Outpatient Rehabilitation Facility | A facility that provides comprehensive rehabilitation services under the supervision of a physician to outpatients with physical disabilities. Services include physical therapy, occupational therapy, and speech pathology services. |
63-64 | Unassigned | N/A |
65 | End-Stage Renal Disease Treatment Facility | A facility, other than a hospital, which provides dialysis treatment, maintenance, and/or training to members or caregivers on an ambulatory or home-care basis. |
66-70 | Unassigned | N/A |
71 | Public Health Clinic | A facility maintained by either State or local health departments that provides ambulatory primary medical care under the general direction of a physician. |
72 | Rural Health Clinic (RHC) | A certified facility which is located in a rural medically under-served area that provides ambulatory primary medical care under the general direction of a physician. |
73-80 | Unassigned | N/A |
81 | Independent Laboratory | A laboratory certified to perform diagnostic and/or clinical tests independent of an institution or a physician’s office. |
82-98 | Unassigned | N/A |
99 | Other Place of Service | Other place of service (POS) not identified above. |
Medicaid Billing Provider Types Who Can Bill Under The Capitated Behavioral Health Benefit
Code | Provider Types | Code | Specialty Types | Can Be Essential Provider |
|---|---|---|---|---|
| 1 | Hospital - General | 301 | Hospital - General |
|
| 2 | Hospital - Mental | 302 | Hospital - Mental | X |
| 5 | Physician | 505 | Physician | X |
| 13 | Transportation | 124 | County agency, Non-Metro area | |
| 13 | Transportation | 324 | Emergency | |
| 16 | Clinic - Practitioner | 351 | Clinic - Practitioner | X |
| 24 | Non-Physician Practitioner - Individual | 440 | Non-Physician Practitioner - Individual | X |
| 25 | Non-Physician Practitioner - Group | 441 | Non-Physician Practitioner - Group | X |
| 26 | Osteopath | 501 | Osteopath | X |
| 30 | Psychiatric Residential Treatment Facility | 476 | Psychiatric Residential Treatment Facility | X |
| 32 | Federally Qualified Health Center | 150 | Freestanding |
|
| 32 | Federally Qualified Health Center | 160 | Hospital Based |
|
| 32 | Federally Qualified Health Center | 199 | Denver Health Hosp School Based Clinics |
|
| 37 | Licensed Psychologist | 520 | Licensed Psychologist | X |
| 38 | Licensed Behavioral Health Clinician | 521 | Licensed Behavioral Health Clinician | X |
| 39 | Physician Assistant | 510 | Physician Assistant | X |
| 41 | Nurse Practitioner | 034 | Pediatric | X |
| 41 | Nurse Practitioner | 035 | Family | X |
| 41 | Nurse Practitioner | 335 | General | X |
| 45 | Rural Health Clinic | 398 | Hospital Based |
|
| 45 | Rural Health Clinic | 472 | Freestanding |
|
| 52 | Residential Childcare Facility | 471 | Mental Health Program |
|
| 64 | Substance Use Continuum | 371 | ASAM 1.0 | X |
| 64 | Substance Use Continuum | 372 | ASAM 1 WM | X |
| 64 | Substance Use Continuum | 213 | Opioid Treatment Provider (OTP) – Moderate Risk | X |
| 64 | Substance Use Continuum | 214 | Opioid Treatment Provider (OTP) – High Risk | X |
| 64 | Substance Use Continuum | 373 | ASAM 2.1 IOP | X |
| 64 | Substance Use Continuum | 212 | ASAM 2.5 PHP | X |
| 64 | Substance Use Continuum | 374 | ASAM 2WM | X |
| 64 | Substance Use Continuum | 871 | ASAM level 3.1 | X |
| 64 | Substance Use Continuum | 872 | ASAM level 3.3 | X |
| 64 | Substance Use Continuum | 873 | ASAM level 3.5 | X |
| 64 | Substance Use Continuum | 874 | ASAM level 3.7 | X |
| 64 | Substance Use Continuum | 875 | ASAM level 3.2 WM | X |
| 64 | Substance Use Continuum | 876 | ASAM level 3.7 WM | X |
| 68 | Qualified Residential Treatment Program | 689 | Qualified Residential Treatment Program | X |
| 77 | Behavioral Health Group | 388 | With Prescriber | X |
| 77 | Behavioral Health Group | 389 | Without Prescriber | X |
| 78 | Comprehensive Safety Net Provider | 887 | Comprehensive Community Behavioral Health Provider |
|
| 88 | Behavioral Health Crisis Line | 880 | Behavioral Health Crisis Line |
|
| 89 | Community Support Services Provider | 889 | Recovery Support Services Organization |
|
| 89 | Community Support Services Provider | 208 | Supportive Housing Provider |
|
| 95 | Crisis Provider | 772 | Mobile Crisis Response | X |
| 95 | Crisis Provider | 386 | Acute Treatment Unit | X |
| 95 | Crisis Provider | 387 | Crisis Stabilization Unit | X |
| 96 | Adult Mental Health Residential | 561 | Support Therapeutic Transitional Living | X |
| 97 | Behavioral Health Transportation | 773 | Secure Transportation |
Modifiers For Medicaid Capitated Behavioral Health Benefit
Effective January 1, 2024, HCPF removed the requirement for a first position modifier to identify a service as either a State Plan or B3 service on all codes. As a result, these modifiers were removed from this table.
Select Residential codes require a modifier to distinguish a service or level of care. These modifiers should be used in the first position on a claim.
The following modifiers should be added in the first available position on a claim when applicable.
Modifier | Category | Description |
|---|---|---|
76 | Repeat Services | Repeat procedure or service by same physician or other qualified health care professional on the same date. |
77 | Repeat Services | Repeat procedure or service by another physician or other qualified health care professional on the same date. |
ET | Emergency Services | Indicates a rendered emergency service/procedure. Services provided through Colorado Crisis Services should include the ET modifier. For Medicaid, providers should refer to their RAE contracts to determine which crisis codes they can provide. |
FQ | Audio Only | Indicates a service was provided by telephone. |
HA | Member Under 21 | Indicates a service was modified/specific to a member under 21 y.o. and allowed due to coverage under EPSDT. |
HD | Special Connections | Indicates services provided as part of the Special Connections program. This should be added to all services provided to pregnant women and/or women with dependent children by approved Special Connections providers. |
HO | Ineligible Medicare Provider | Indicates when an enrolled Medicaid provider is providing services to a Medicare member with Medicaid (Dual Eligible) and the provider is not eligible to enroll in Medicare. |
NOTE: This table lists modifiers that can be used when billing Managed Care Entities under the Capitated Behavioral Health Benefit. There may be other modifiers required for billing Fee-For-Service or the Behavioral Health Administration (BHA).
According to the Colorado State Plan, Targeted Case Management (TCM) is a covered benefit for an identified Target Group: "Medicaid clients enrolled in the [Capitated Behavioral Health Benefit] (a Section 1915(b) waiver program) who have or are being assessed for a mental health diagnosis(es) covered under the [Capitated Behavioral Health Benefit]."
Case management services are services furnished to assist individuals, eligible under the State Plan, in gaining access to needed medical, social, educational and other services. Case management does not include activities integral to the administration of foster care programs, or for which third parties are liable to pay.
Examples of Case Management
Assessment of service needs:
- Comprehensive assessment/periodic reassessment of the individual’s need for medical, educational, social, or other services.
- Activities/Interventions to gather/confirm information coming from the Individual, family, and other sources in order to complete assessment.
- Determining with the individual/family/supports their ability to access and effectively link to these services and supports on their own and what type of help they will need, including how intensely and for how long case management services will be needed.
- Assisting the Individual and their Family/Supports in understanding what case management services include their limitations so that they can better participate in the case management assessment and treatment/service planning process
Development of a specific service plan that includes:
- Prioritizing with the Individual and their Family/Supports the referrals and linkages needed so the treatment/service plan reflects the case management assessment. As a result of the assessment, the case management plan will have a timeline for referral and linkage as well as the expected outcomes of the interventions.
- Specifies goals and actions to address the medical, social, educational, and other services needed by the individual.
- Identifies a course of action to respond to assessed needs.
- Developing, in conjunction with the Individual, a list of agreed upon case management interventions that will be used to help the Individual successfully link to services and supports.
- Develop with the Individual and Family/Supports the role of the persons providing case management services in coordinating care among treatment providers, other services, and natural/community supports.
- Develop with the Individual an agreed upon structure for regular meetings with the person(s) providing case management services to review progress and determine necessary changes to the treatment/service plan.
Referral and related activities to obtain needed services:
- To help an individual obtain needed service including activities that link them to medical, social, or educational providers or other services capable of providing services and assisting in referral/scheduling.
- Follow-up post appointments to ensure that the person providing case management services understands any changes or recommendations to treatment or to the content of the supports that will be provided, and that this information is also understood and able to be acted on effectively by the Individual/Family/Supports.
Monitoring and follow-up:
- Meeting via phone or face-to-face (all services can take place face-to-face or via phone) on a regularly scheduled basis with the individual and their Family/Supports to ensure that services are being provided according to the treatment/service plan, that the individual believes they are effective, and wishes to continue according to the current treatment/service plan to ensure the member is getting the services they need.
- Talking/meeting with Providers and Supports, with or without the Individual present, to coordinate care, assess the effectiveness of service, progress of the Individual towards goals and objectives on any treatment/service plan, and soliciting ideas for changes that will allow for more rapid progress towards the Individual’s recovery goals. Again, the overall purpose of these activities is to ensure the member is getting the services they need.
Case Management does not include the following:
- Case management activities that are an integral component of another covered Medicaid service.
- Direct delivery of medical, educational, social, or other services to which a Medicaid eligible member has been referred.
- Activities integral to the administration of foster care programs.
- Activities, for which a Medicaid eligible member may be eligible, but are integral to the administration of another non-medical program.
Behavioral Health Peer Support Policy
This policy was updated on December 5, 2025
According to 2 CCR 502-1, “‘Peer Support’ means recovery-oriented services provided by peer support professionals that promote self-management of psychiatric symptoms, relapse prevention, treatment choices, mutual support, enrichment, and rights protection. Peer support also provides social support and a lifeline for individuals who have difficulties developing and maintaining relationships.”
The SMD letter #07-011 indicates that states must determine the minimum training and certification criteria for professionals delivering peer support services in a behavioral health context. HCPF follows the definitions of training and certification requirements for Peer Support Professionals in Behavioral Health Administration (BHA) rule. In alignment with the Medicaid Sustainability Memo published in June 2025, HCPF is implementing the following policy for Peer Support Professionals delivering behavioral health services billable to a Regional Accountable Entity (RAE) (henceforth referred to as Behavioral Health Peer Support Professionals).
Effective January 1, 2026, all Behavioral Health Peer Support Professionals must either be certified or be in the process of becoming certified in order for the services they deliver to be reimbursable by a Health First Colorado Regional Accountable Entity (RAE).
In the process of becoming certified is defined as: Peers who have completed all 60 hours of required training and are in the process of completing their hours of experience and working towards certification. Services delivered by Behavioral Health Peer Support Professionals in the process of becoming certified are reimbursable for up to 6 months following the completion of required training.
Agencies must sign and submit this attestation to their Regional Accountable Entity (RAE) or RAEs by January 1st annually, indicating that all Behavioral Health Peer Support Professionals are either certified or are in the process of becoming certified.
Like all other unlicensed professionals delivering behavioral health services, Behavioral Health Peer Support Professionals deliver services under the oversight of a Rendering Provider. Effective January 1, 2026, oversight must be in alignment with the Health First Colorado Behavioral Health Rendering Provider Oversight (RPO) Policy.
In compliance with Centers for Medicare and Medicaid Services (CMS) guidance, behavioral health Peer Support Services must tie to measurable goals specified on an individualized service plan.
In response to budget adjustments authorized by the state legislature, effective July 1, 2025, HCPF updated the services that can be billed for when delivered by a Behavioral Health Peer Support Professional, in addition to the providers that can bill for services delivered by a Behavioral Health Peer Support Professional. Behavioral Health Peer Support Professionals are encouraged to continue to participate in team-based treatment, however, their individual contributions are limited as outlined below.
Effective July 1, 2025, HCPF limited the codes that can be billed for individual contributions by Behavioral Health Peer Support Professionals to the following:
- H0038: Self-help/Peer Services
- H0023: Behavioral Health Outreach Service
HCPF is limiting the providers that can bill for H0038: Self-help/Peer Services to the following provider types:
- Comprehensive Safety Net Providers - Provider Type (PT) 78 / Specialty Type (ST) 887
- Substance Use Disorder Clinics - PT 64 / ST 371
- Recovery Support Services Organizations - PT 89/ST 889
Additionally, Behavioral Health Peer Support Professionals can only deliver H0023: Behavioral Health Outreach Service when employed by the above provider types.
Effective July 1, 2025, Colorado MUEs (CO MUEs) for H0038 and H0023 are as follows:
- H0038: Self-help/peer services - 12 units per day (3 hours)
- H0023: Behavioral Health Outreach Service - 8 units* per day (2 hours) (*Please note: The NCCI MUE for H0023 is 1, 15 minute unit per day. HCPF will continue to review this policy)
Service billed in excess of the CO MUE will have a denial message regarding the MUE limit being exceeded; providers have a right to appeal and submit any necessary clinical documentation, in order to determine if more units should be allotted.
CSNPs (PT 78/887) & SUD providers (PT 64/371) can also use Peer Support Professionals to deliver:
- H2017/H2018: Psychosocial rehabilitation services
- H2023/H2024: Supported employment
- H2025/H2026: Ongoing support to maintain employment
Behavioral Health Peer Support Professionals may deliver services within their scope as part of a multidisciplinary team for individuals with behavioral health needs. As part of a multidisciplinary team, Peers may participate in the delivery of the following team-based services:
- H0015: Alcohol and/or drug services. Intensive Outpatient Program (IOP), ASAM level 2.1
- H0016: Alcohol and/or drug services; less than 24 hours, Partial Hospitalization Program (PHP), ASAM level 2.5
- H0035: Mental Health Partial Hospitalization Program (PHP)
- H2030/H2031: Mental Health Clubhouse services
- H0046: Drop-In Center
- H2001: Rehabilitation program
- H2015/H2016: Comprehensive community support services
- H2017/H2018: Psychosocial rehabilitation services
- H2023/H2024: Supported employment
- H2025/H2026: Ongoing support to maintain employment
- H2011 ET: Crisis intervention service
- H0039/H0040: Assertive Community Treatment
Resources:
CMS Guidance on Medicaid Coverage of Peer Support Services
SMDL #07-011 (August 15, 2007)
Frequently Asked Questions on Medicaid and CHIP Coverage of Peer Support Services (June 5, 2024)
SAMHSA Core Competencies for Peer Workers
Core Competencies for Peer Workers in Behavioral Health Services (December 13, 2018)
Clinical Laboratory Improvement Amendments (CLIA)
Explanation of CLIA waiver: SUD providers can deliver some laboratory testing services through a CLIA Certificate of Waiver. CLIA stands for Clinical Laboratory Improvement Amendments, and by the CLIA law, waived tests are those tests that are determined by CDC or FDA to be so simple that there is little risk of error. Some testing methods for glucose and cholesterol are waived, along with pregnancy tests, fecal occult blood tests, some urine tests, etc. For more information, please see the How to Obtain a CLIA Certificate of Waiver brochure, as well as the list of CLIA waived CPT codes.
All claims for laboratory services, including those rendered by non-laboratory providers such as physicians, must have the NPI number of the provider who ordered the items to be indicated on the claim. In the Provider Web Portal, this field is labeled "Referring Provider".
The provider types who may order these services are physician (05), physician assistant (39), osteopath (26), certified nurse-midwife (22), advanced practice nurse (41), and pharmacist (75). Reference the Laboratory Services Billing Manual for further details.
FAQs on Urine Collection and Analysis [07/01/2018]
Q1. Are urine collection and analysis tests reimbursed by Health First Colorado (Colorado’s Medicaid program)?
A1. There are three components to a urinalysis (UA): collection, analysis, and counseling.
- Collection of a urine specimen alone is not reimbursable.
- The analysis of the specimen is billed fee-for-service by the laboratory. According to rule and Laboratory billing guidelines, a physician’s order is required for a lab to bill for analysis.
- The review of results and counseling provided to a member can be billed to a Managed Care Entity (MCE) by using HCPCS code S9445.
Q2. Are strip tests, or other testing that does not require a lab analysis, reimbursed by Health First Colorado?
A2. Health First Colorado does not reimburse for strip tests, dip sticks, or any other methodology considered “Direct Optical Observation”. Providers contracted with the Behavioral Health Administration can submit these services in their client-level encounter reporting using CPT Code 80305.
Q3. Are monthly UAs as a part of recovery support services reimbursable by Health First Colorado?
A3. If a physician orders the UA and a behavioral health practitioner offers counseling based on the testing results, then the UA can be reimbursed as described in question #1.
Q4. Does Health First Colorado reimburse court-ordered UAs (e.g. DUI treatment requirements, “Drug Court”, requirements for child visitation by county human services department, controlled substance monitoring, etc.)?
A4. A court order is not a factor that determines Health First Colorado reimbursement. A service is reimbursed if it is covered under the Capitated Behavioral Health Benefit and considered medically necessary.
Q5. Is there a limit to the number of UAs that can be ordered for an individual?
A5. There are no limitations on the number of UAs reimbursed as long as the service is medically necessary.
Essential Safety Net Provider Alignment Guide
Effective July 1, 2025
HCPF Provider Type
| BHA Essential Approval Paperwork Options
|
|---|---|
| Hospital - Mental (PT 2/302) |
|
| Psychiatric Residential Treatment Facility (PT 30/476) |
|
| Substance Use Continuum - Opioid Treatment Provider (OTP) – Moderate Risk (PT 64/213) |
|
| Substance Use Continuum - Opioid Treatment Provider (OTP) – High Risk (PT 64/214) |
|
| Substance Use Continuum - ASAM level 3.1 (PT 64/871) |
|
| Substance Use Continuum - ASAM level 3.3 (PT 64/872) |
|
| Substance Use Continuum - ASAM level 3.5 (PT 64/873) |
|
| Substance Use Continuum - ASAM level 3.7 (PT 64/874) |
|
| Substance Use Continuum - ASAM level 3.2 WM (PT 64/875) |
|
| Substance Use Continuum - ASAM level 3.7 WM (PT 64/876) |
|
| Qualified Residential Treatment Program (PT 68/689) |
|
| Crisis Provider - Mobile Crisis Response (PT 95/772) |
|
| Crisis Provider - Acute Treatment Unit (PT 95/386) |
|
| Crisis Provider - Crisis Stabilization Unit (PT 95/387) |
|
| Adult Mental Health Residential - Supported Therapeutic Transitional Living (PT 96/561) |
|
Effective July 1, 2025
Colorado System of Care (CO-SOC) [effective 07/01/2025]
HCPF has developed a CO-SOC Provider Enrollment & Billing Guidance document. Additional information regarding Medical Necessity Criteria, Exclusion Criteria, Continued Stay Criteria, and Discharge Criteria is published below.
Enhanced Multi-Systemic Therapy (EMST)
- Medical Necessity Criteria
Youth must meet the following criteria for admission to MST:- The youth has an assessment completed that shows evidence of symptoms and functional impairment that the youth has met criteria for a primary diagnosis consistent with the most recent version of Diagnostic and Statistical Manual that falls within the categories of disruptive behavior, mood, substance use or trauma and stressor-related disorders.
- Within the past 30 calendar days, the youth has demonstrated at least one of the following that puts the youth at risk of an out-of-home placement:
- Persistent and deliberate attempts to intentionally inflict serious injury on another person.
- Ongoing dangerous or destructive behavior that is evidenced by repeated occurrences of behaviors that are endangering to self or others are difficult to control, cause distress, or negatively affect the youth’s health.
- Increasing and persistent symptoms associated with depression or anxiety in combination with externalizing problems (e.g. physical and verbal aggression, truancy, stealing, property destruction, lying, etc.) that have contributed to decreased functioning in the community.
- Ongoing substance use or dependency that interfere with the youth’s interpersonal relationships and functioning in the community.
- OR,
The youth is returning home from an out-of-home placement and EMST is needed as step down service from an out-of-home placement.- The youth’s successful reintegration or maintenance in the community is dependent upon an integrated and coordinated treatment approach that involves intensive family/caregiver partnership through the MST model.;
- There is a family member or other committed caregiver available to participate in this intensive service.
- Arrangements for supervision at home/community are adequate to ensure a reasonable degree of safety and a safety plan has been established or will be quickly established by the EMST program as clinically indicated
- Exclusion Criteria:
Youth who meet any one of the criteria below are not eligible to receive EMST:- The youth is currently experiencing active suicidal, homicidal or psychotic behavior that requires continuous supervision that is NOT available through the provision of EMST.
- The youth is living independently, or the provider cannot identify a primary caregiver for participation despite extensive efforts to locate all extended family, adult friends and other potential surrogate caregivers.
- The youth’s presenting problem is limited to sexually harmful or dangerous behavior in the absence of other externalizing behaviors.
- Continued Stay Criteria
- Within the past thirty (30) calendar days, EMST continues to be the appropriate level of care for the youth as evidenced by at least one of the following:
- The youth’s symptoms/behaviors and functional impairment persist at a level of severity adequate to meet admission criteria;
The youth has manifested new symptoms that meet admission criteria and those have been documented in the treatment plan
Progress toward identified treatment plan goal(s) is evident and has been documented based upon the objectives defined for each goal, but not all of the treatment goal(s) have been achieved.
- The youth’s symptoms/behaviors and functional impairment persist at a level of severity adequate to meet admission criteria;
- Within the past thirty (30) calendar days, EMST continues to be the appropriate level of care for the youth as evidenced by at least one of the following:
- Discharge Criteria
- The youth meets discharge criteria if any of the following are met:
- The youth’s documented treatment plan goals have been met and the discharge plan has been successfully implemented
- The youth and family are not engaged in treatment despite documented efforts to engage and there is no reasonable expectation of progress at this level of care;
- The youth is placed in an out of home placement, including, but not limited to a hospital, skilled nursing facility, psychiatric residential treatment facility, or therapeutic group home and is not ready for discharge within 30 consecutive calendar days to a family home environment or a community setting with community-based support.
- Required consent for treatment is withdrawn.
- The youth meets discharge criteria if any of the following are met:
Enhanced Functional Family Therapy (EFFT)
- Medical Necessity Criteria
- Youth must meet the following criteria for admission to EFFT:
- The initial assessment provides evidence of symptoms and functional impairment that the youth has met criteria for a primary diagnosis consistent with the most recent version of Diagnostic and Statistical Manual that falls within the categories of disruptive behavior, mood, substance use or trauma and stressor-related disorders.
- Within the past 30 calendar days, the youth has demonstrated at least one of the following that puts the youth at risk of out of home placement:
- Persistent and deliberate attempts to intentionally inflict serious injury on another person;
- Ongoing dangerous or destructive behavior that is evidenced by repeated occurrences of behaviors that are endangering to self or others are difficult to control, cause distress, or negatively affect the youth’s health;
- Increasing and persistent symptoms associated with depression or anxiety in combination with externalizing problems (e.g. physical and verbal aggression, truancy, stealing, property destruction, lying, etc.) that have contributed to decreased functioning in the community;
- Ongoing substance use or dependency that interfere with the youth’s interpersonal relationships and functioning in the community.
- OR,
The youth is returning home from out-of-home placement and EFFT is needed as step down service from an out-of-home placement.- The youth’s successful reintegration or maintenance in the community is dependent upon an integrated and coordinated treatment approach that involves intensive family/caregiver partnership through the FFT model.
- There is a family member or other committed caregiver available to participate in this intensive service.
- Arrangements for supervision at home/community are adequate to ensure a reasonable degree of safety and a safety plan has been established or will be quickly established by the EFFT program as clinically indicated.
- Youth must meet the following criteria for admission to EFFT:
- Exclusion Criteria
Youth who meet any one of the criteria below are not eligible to receive EFFT:- The youth is currently experiencing active suicidal, homicidal or psychotic behavior that requires continuous supervision that is NOT available through the provision of EFFT.
- The youth is living independently, or a provider cannot identify a primary caregiver for participation despite extensive efforts to locate all extended family, adult friends and other potential surrogate caregivers.
- The youth’s presenting problem is limited to sexually harmful or dangerous behavior in the absence of other externalizing behaviors.
- Continued Stay Criteria
Within the past thirty (30) calendar days, EFFT continues to be the appropriate level of care for the youth as evidenced by at least one of the following:- The youth’s symptoms/behaviors and functional impairment persist at a level of severity adequate to meet admission criteria;
- The youth has manifested new symptoms that meet admission criteria and those have been documented in the treatment plan.
- Progress toward identified treatment plan goal(s) is evident and has been documented based upon the objectives defined for each goal, but not all of the treatment goal(s) have been achieved.
- Discharge Criteria
The youth meets discharge criteria if any of the following are met:- The youth’s documented treatment plan goals and objectives have been substantially met and all EFFT phases have been completed;
- The youth no longer meets admission criteria due to the following:
- The youth’s needs can be met at a lower level of care;
- The youth’s current level of function requires a higher level of care
- The youth or the youth’s family have not benefited from EFFT despite multiple documented efforts to engage the youth or family and there is no reasonable expectation of progress at this level of care despite treatment plan changes or the youth or the youth’s family has achieved maximal benefit from this level of care;
- The youth is placed in a hospital, skilled nursing facility, residential treatment facility, or other residential treatment setting and is not ready for discharge within 30 consecutive calendar days to a family home environment or a community setting with community-based support;
- Required consent for treatment is withdrawn;
Enhanced High Fidelity Wraparound (EHFW)
The National Wraparound Implementation Center (NWIC) Model for evidenced based Intensive Care Coordination intervention is not duplicative of case management provided by the QRTP, PRTFs and OHIRT in their daily rates.
- Medical Necessity Admission Criteria
All of the following are necessary for admission to this level of care:- Part I and II of the criteria below.
- Part I: The youth currently has, or at any time during the past year has had, a diagnosable mental, behavioral, or emotional disorder to meet the diagnostic criteria specified within ICD -10 or DSM –V-TR (and subsequent revisions) of the American Psychiatric Association with the exception of other V codes, substance use, and developmental disorders, unless these disorders co-occur with another diagnosable disturbance. All of these disorders have episodic, recurrent, or persistent features; however, they vary in terms of severity and disabling effects.
- The diagnosable disorder identified above has resulted in functional impairment that substantially interferes with or limits the youth’s role or functioning in family, school, or community activities. Functional impairment is defined as difficulties that substantially interfere with or limit the youth in achieving or maintaining developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills. Functional impairments of episodic, recurrent, and continuous duration are included unless they are temporary and expected responses to stressful events in the environment.
- Youth who would have met functional impairment criteria during the referenced year without the benefit of treatment or other support services are included in this definition.
- Additionally:
The youth is multi-system involved, including but not limited to receiving services at school, DYS, treatment centers, hospitals, residential or day treatment centers , of any combination thereof.- The youth is multi-system involved, including but not limited to receiving services at school, DYS, treatment centers, hospitals, residential or day treatment centers , of any combination thereof.
- The person(s) with authority to consent to medical treatment for the youth voluntarily agrees to participate in HFW. The assent of a youth who is not authorized under applicable law to consent to medical treatment is desirable but not required.
- For youth in a hospital, skilled nursing facility, psychiatric residential treatment facility or other residential treatment setting who meet the above criteria, the admission to HFW may occur 30 days prior to discharge from the above settings.
- Part I and II of the criteria below.
- Exclusion Criteria
Any of the following criteria is sufficient for exclusion from EHFW:- The person(s) with authority to consent to medical treatment for the youth does not voluntarily consent to participate in HFW.
- The youth is in a hospital, skilled nursing facility, psychiatric residential treatment facility, DYS, or other residential treatment setting at the time of referral and is unable to return to a family home environment or community setting with community-based support.
- Continued Stay Criteria
The following criteria must be met for continued treatment at this level of care:- The youth’s clinical condition(s) continues to warrant EHFW services in order to coordinate the youth’s involvement with state agencies and special education or multiple service providers.
AND - Progress toward Individualized Care Plan (ICP) identified goals is evident and has been documented based upon the objectives defined for each goal, but the goals have not yet been substantially achieved.
OR - Progress has not been made, and the Care Plan Team (CPT) has identified and implemented changes and revisions to the ICP to support the goals of the youth and family.
- The youth’s clinical condition(s) continues to warrant EHFW services in order to coordinate the youth’s involvement with state agencies and special education or multiple service providers.
- Discharge criteria
Any of the following criteria is sufficient for discharge from this level of care:- The youth no longer meets the criteria for HFW.
- The CPT determines that the youth’s documented ICP goals and objectives have been substantially met and continued services are not necessary to prevent worsening of the youth’s behavioral health condition.
- Consent for treatment is withdrawn.
- The youth and parent/caregiver are not engaged in treatment. Despite a minimum of 3 documented attempts to address engagement, the lack of engagement is of such a degree that it implies withdrawn consent or treatment at this level of care becomes ineffective or unsafe.
- The youth is placed in a hospital, skilled nursing facility, psychiatric residential treatment facility, committed to DYS or other residential treatment setting and is unable to return to a family home environment or a community setting with community-based supports, or unable to continue the HFW process.
- The youth turns 21
- Provider Qualifications
Individuals are eligible to provide Enhanced High Fidelity Wraparound (EHFW) and supervise EHFW within their professional scope of practice those services certified by the training through the workforce capacity center.- Bach Level
- Intern
- Unlicensed Master’s Level
- Unlicensed EdD/ PhD/PsyD
- LCSW
- LPC
- LMFT
- Licensed EdD/PhD/PsyD
- LAC
- The provider's training plan must include provisions for ongoing training specific to the identified training needs of the staff as it relates to the population served, including attention to cultural competency, changing demographics, trauma informed care, new knowledge or research, and other areas identified by the agency.
The provider must demonstrate that each Enhanced High Fidelity Wraparound supervisor receives training specific to the clinical and administrative supervision of the service.
The provider shall obtain satisfactory fidelity reviews based on the NWIC model of HFW criteria every twelve months. This will be documented on a fidelity scoring instrument. - Wraparound Facilitator
Must have, at minimum, a bachelor’s in social services, human services, or an equivalent field.- All new wraparound staff (facilitators, family support partners, youth support partners, coaches, and supervisors) are required to complete the NWIC Model training;
- Phase 1: Orientation Phase
- Basic history and overview of wraparound
- Introduction to skills/ competencies
- Intensive review of the process
- Ends when tell, show, practice is complete
- Phase 2: Apprenticeship Phase (carries a full caseload)
- Observation by the apprentice
- Observation of the apprentice
- Observations are completed with a score that exceeds threshold on a knowledge test
- Phase 3: Ongoing coaching and supervision
- Ongoing coaching, informed by data
- Periodic observation
- Document review
- Ongoing as needed.
- Wraparound supervisor
- Must complete all the above requirements; and NWIC supervisor training;and
- Have a bachelor’s degree in social services, human services, or an equivalent field with a minimum of two (2) years’ experience working with the target population and/or HFW program and supervision.
- Wraparound coach
- Must complete all the above requirements; and NWIC coaching training;and
- Have a bachelor’s degree in social services, human services, or an equivalent field with a minimum of two (3) years’ experience working with the target population and/or HFW program and supervision.
Enhanced Standardized Assessment (ESA)
- Service Description (including example activities):
The Enhanced Standardized Assessment (ESA) is a non-medical encounter conducted by a non-physician licensed or licensure candidate behavioral health professional. The SA is a comprehensive, clinical assessment process completed by a behavioral health provider to assist in determining appropriate treatment/service recommendations for children, youth, and families. This process must include the following components and activities:- Face-to face clinical assessment of the child/youth
- CO CANS Assessment Tool
- CO CANS Decision Support Model upon availability
- Review of records (see notes)
- Collateral interviews & information (see notes)
- DSM-5 diagnosis
- Completion of the BHA-provided and approved Enhanced Standardized Assessment Narrative Template which includes, but is not limited to, the following elements:
- Child/Youth Identifying Information & Demographics
- Tools used during the Assessment (e.g., required CO CANS, Columbia, PHQ-A, GAD-7, etc.)
- Documentation Review
- Date(s) and name(s) or all individuals interviewed or outreached for the ESA (complete list is in the ESA Template)
- Chief Complaint/Presenting Problem Narrative
- Life Functioning Narrative
- Intellectual/Developmental Narrative
- School Behaviors and Educational Information
- Youth Behavioral/Emotional Narrative and Symptom Profile
- Traumatic/Stressful Life Events Narrative
- Adjustment to Trauma/Traumatic Stress Symptoms Narrative
- Substance Use Disorder Narrative
- Danger to Self Risk Behaviors Narrative
- Danger to Others Risk Behaviors Narrative
- Cultural Factors Narrative
- Youth Strengths Narrative
- Early Childhood Narrative (as applicable)
- Transition Age Youth Narrative (as applicable)
- Mental Status Exam
- Caregiver Resources and Needs Narrative
- Current/Previous Medications
- History of or current child welfare involvement and DYS commitment, including prior placement
- Psychiatric Hospitalization(s)
- Current and Previous Behavioral Health Services
- Current or Pending Legal or Juvenile Justice Concerns
- Diagnosis History
- Current Barriers to Treatment
- Risk of being a victim of human trafficking
- Current diagnosis/diagnoses
- Significant Findings of the Child and Adolescent Needs and Strengths (CANS) Tool
- Recommendations of and clinical justifications for recommended treatment/services (including but not limited to unsuccessful treatment history, barriers to treatment, caregiver involvement history, caregiver needs, risk factors, environmental factors, etc.)
- The provider shall make reasonable documented efforts to obtain and review the following documents/records including but not limited to:
- Critical documents from Trails
- Juvenile Assessment Center (JAC) assessment
- Individualized Education Program (IEP) documents
- 504 plans
- Educational records
- Applicable child welfare case notes and court orders
- Behavioral health treatment notes
- Behavioral health assessments
- Parent-child interactional assessments
- Trauma screen or assessment
- DYS assessment reports and documents
- All referral information
- RAE records
- Team meeting notes
- Any hospitalization records from the last year
- Probable cause statements and other judicial assessments that were completed within the last year.
- The provider shall make reasonable documented efforts to interview the following individuals and integrate information disclosed in the SA:
- Child/youth
- Parents/caregivers
- County Department of Human Services caseworker
- DYS client manager
- RAE care coordinator
- Primary behavioral health treatment provider
- Psychiatrist or person authorized to prescribe medications
- Other relevant individuals, if they are a part of the child/youth’s team: Court Appointed Special Advocate (CASA), Guardian ad Litem (GAL), Counsel For Youth (CFY), Mentor, Probation Officer, Diversion Officer etc.
- The provider shall make reasonable documented efforts to obtain, review, and integrate information gathered from the following sources in the SA:
- Previous behavioral health treatment providers
- Other natural supports and/or family members identified by the child/youth and family,
- School staff
- Mentors/behavioral coaches,
- Guardian ad litem (GAL)
- Counsel for Youth (CYF)
- Court Appointed Special Advocate (CASA)
- Any recent (past twelve (12) months) foster parents or guardians
- Other collateral information as relevant to the case
- Additional items for inclusion in documentation where information is available and applicable (pursuant to following CCR 502-1 Rules CR 502.1.21.200.14 & CCR 502.1.190.3)
- Additional assessment requirements may be required for specific BHA programs that utilize the SA.
Under the Capitated Behavioral Health Benefit, Regional Accountable Entities (RAEs) have sole responsibility and discretion to contract with service providers, as well as to set provider rates. However, there are occasionally reasons that HCPF establishes a Directed Payment as a minimum reimbursement rate for specific services, or services delivered to a specific population, that RAEs must pay. Directed Payments help ensure that the RAEs are investing in specific state priority areas. RAEs are required to update provider contracts and claims systems to reflect a rate no less than the rates outlined by HCPF. Directed payments are time-limited investments that are reviewed on a regular basis to monitor their effectiveness and are not a sustainable ongoing funding mechanism within a managed care model. Directed Payments are not exclusively for the purpose of a rate review/increase. Please refer to the Statewide Behavioral Health Billing Manual Appendix D for rates associated with Directed Payments.
The factors that inform when a Directed Payment is necessary:
- When a service is new or is being underutilized across the state.
- When there are identified access issues related to a specific service.
As a Directed Payment is phased out, RAEs may negotiate provider reimbursement rates based on quality metrics, network adequacy, and regional service needs. HCPF expects RAEs to use available funds to maintain access to services in alignment with required timeliness standards.
Safety Net Directed Payments
When launching the safety net in 2024, Directed Payments were utilized as a time-limited method to infuse funds into the behavioral health safety net system to support providers through the transition to the new system, support network access, and create growth for specific services.
Effective July 1, 2025, HCPF will no longer set Directed Payments for outpatient behavioral health essential safety net services, except those for Mobile Crisis Response services and Opioid Treatment Programs. Directed Payments for essential safety net services in a bedded facility will remain in place until June 30, 2026.
Directed Payments for behavioral health safety net services as of July 1, 2025, include:
- Comprehensive Safety Net Providers
- Prospective Payment System (PPS)
- Essential Safety Net Providers (ESNP)
- Mobile Crisis Response (MCR) services
- Opioid Treatment Program (OTP) services
- Services in a bedded facility (Until June 30, 2026)
Directed Payments for Targeted Populations
Directed Payments for services for Targeted Populations (non-Safety Net) are limited unique situations where targeted action is necessary to support network access and growth for specific services. In such circumstances, HCPF may establish a Directed Payment as a minimum reimbursement rate for specific services that RAEs must pay to non-Safety Net providers.
Current Directed Payments for Targeted Populations serve youth receiving the following services:
- Functional Family Therapy (FFT)
- Multisystemic Therapy (MST)
- Wraparound Services
- Community Support Services
These directed payments will also be reviewed on a regular basis to monitor their effectiveness and are not a sustainable ongoing funding mechanism within a managed care model.
Colorado Medically Unlikely Edits and Procedure to Procedure (CO MUEs and CO PTP)
Effective October 1, 2025, HCPF is requiring Regional Accountable Entities (RAEs) to implement Colorado specific medically unlikely edits (MUEs) and Colorado specific procedure to procedure (PTP) edits. Services billed in excess of the CO MUE will have a denial message regarding the MUE limit being exceeded; providers have a right to appeal and submit any necessary clinical documentation, in order to determine if more units should be allotted.
- Medically Unlikely Edits (MUEs) prevent inappropriate payments when services are reported with an unusually high number of units of service.
- Procedure to Procedure (PTP) edits prevent code pairs that should not be reported together on the same date of service.
| code | title & units | CO MUE Units allowed (per day) | CO PTP |
|---|---|---|---|
| H0004 | Individual/family counseling and therapy | 4 units per day | |
| H0023 | Behavioral Health Outreach Service | 8 units per day | |
| H0033 | Oral medication administration, direct observation, per diem | 2 units per day | |
| H0034 | Medication training and support, per 15 mins | 1 unit per day | |
| H0038 | Self-help/peer services | 12 units per day | |
| H2014 | Skills training and development | 12 units per day | |
| H2015 | Comprehensive community support services | 16 units per day | Cannot be billed on the same day as H2014, H2016, H2017, H2018, H2021, or H2022 |
| H2016 | Comprehensive community support services | 1 unit per day | Cannot be billed on the same day as H2014, H2015, H2017, H2018, H2021, or H2022 |
| H2017 | Psychosocial rehabilitation services | 16 units per day | Cannot be billed on the same day as H2014, H2015, H2016, H2018, H2021, or H2022 |
| H2018 | Psychosocial rehabilitation services, per diem | 1 per day | Cannot be billed on the same day as H2014, H2015, H2016 H2017, H2021, or H2022 |
| H2021 | Community-based wrap-around services, 15 mins | 16 units per day | Cannot be billed on the same day as H2014, H2015, H2016 H2017, H2018, or H2022 |
| H2022 | Community-based wrap-around services | 1 unit per day | H2016 H2017, H2018, or H2021 |
| H2027 | Psychoeducational service, per 15 mins | 4 units per day | |
| H2032 | Activity therapy, per 15 mins | 12 units per day | |
| S9454 | Stress management classes, non-physician provider | 1 unit per day | |
| T1017 | Targeted Case Management | 4 units per day | Cannot be billed on the same day as H0006 |
National Correct Coding Initiative (NCCI) edits
The National Correct Coding Initiative
Beginning July 1, 2025, HCPF is requiring RAEs to implement all National Correct Coding Initiative (NCCI) edits. The Centers for Medicare and Medicaid Services (CMS) created the NCCI to reduce improper payments stemming from incorrect coding and billing practices. NCCI prevents reimbursement for inappropriate combinations of Current Procedural Terminology (CPT) codes. The following are the three types of NCCI Edits:
- Add-on Code (AOC) edits ensure add-on codes are not billed without a primary procedure code.
- Medically Unlikely Edits (MUEs) prevent inappropriate payments when services are reported with an unusually high number of units of service.
- Procedure to Procedure (PTP) edits prevent code pairs that should not be reported together on the same date of service.
Visit the CMS NCCI for Medicaid webpage for more information on NCCI edits.
For additional information on NCCI Edits and CO MUEs, please refer to the NCCI and CO MUEs Frequently Asked Questions
Document PDF attached: Frequently Asked Questions for NCCI & CO MUEs
Behavioral Health Secure Transport Place of Service
Behavioral Health Secure Transportation (BHST) is a benefit for all Health First Colorado (Colorado's Medicaid program) members who are experiencing a behavioral health crisis and require urgent transportation for behavioral health stabilization and treatment. Behavioral Health Secure Transportation (BHST) pick-up may occur from the following place of service (POS) listed below.
- 01 Pharmacy
- 03 School
- 04 Homeless Shelter
- 05 Indian Health Service (HIS) – Free Standing Facility
- 06 Indian Health Service (HIS) –Based Facility
- 07 Tribal 638 Free-Standing Facility
- 08 Tribal 638 Provider-Based Facility
- 11 Office
- 12 Home
- 13 Assisted Living Facility (ALF)
- 14 Group Home
- 15 Mobile
- 16 Temporary Lodging
- 17 Walk-in Retail Health Clinic
- 18 Place of Employment – Worksite
- 19 Off Campus – Outpatient Hospital
- 20 Urgent Care Facility
- 22 Outpatient Hospital
- 23 Emergency Room – Hospital
- 24 Ambulatory Surgical Center
- 25 Birthing Center
- 26 Military Treatment Facility (MTF)
- 27 Outreach Site/Street
- 31 Skilled Nursing Facility (SNF)
- 32 Nursing Facility (NF)
- 33 Custodial Care Facility (CCF)
- 34 Hospice
- 49 Independent Clinic
- 50 Federally Qualified Health Center (FQHC)
- 52 Psychiatric Facility – Partial Hospitalization (PF-PHP)
- 53 Community Mental Health Center/Clinic (CMHC)
- 54 Intermediate Care Facility – Mentally Retarded (ICF-MR)
- 55 Residential Substance Abuse Treatment Facility (RSATF)
- 56 Psychiatric Residential Treatment Center (PRTC)
- 57 Non-Residential Substance Abuse Treatment Center (NRSATC)
- 60 Mass Immunization Center
- 62 Comprehensive Outpatient Rehabilitation Facility
- 65 End-Stage Renal Disease Treatment Facility
- 71 Public Health Clinic
- 72 Rural Health Clinic (RHC)
- 81 Independent Laboratory
- 99 Other Place of Service (POS) not identified above
Pick-up is not allowable if a behavioral health crisis is not established, regardless of the listed POS. Transportation arranged for member convenience, routine medical needs, or any other non-crisis scenario does not meet criteria for BHST coverage.
For Fee for Service information please go here.
Senate Bill 23-174: Coverage Policy
Select Behavioral Health Services for Members Under 21
In 2023, the Colorado Legislature passed Senate Bill 23-174 that required the Department of Health Care Policy and Financing (HCPF) to provide access to a limited set of behavioral health services to members under the age of 21 without a covered diagnosis. The legislation detailed service categories that must be included under this coverage, and HCPF engaged stakeholders to identify the specific service codes that are included. This coverage policy goes into effect July 1, 2024.
There are eighteen (18) services covered under the “174 Coverage Policy”. These are listed below and are indicated in the State Behavioral Health Services (SBHS) Billing Manual, Appendix I, highlighted in blue, as well as the School Health Services (SHS) Program Manual Section 2 and the SHS Billing Manual.
When a practitioner provides any of the included services to a member under the age of 21 they are allowed to use one of the listed symptomology or Social Determinant of Health (SDOH) codes in the diagnosis box of a claim. If a member meets the criteria for a Behavioral Health condition it is best practice to use the clinical diagnosis on a claim for services provided.
- References and Resources
Prior Authorization and Retrospective Reviews for Outpatient Psychotherapy
This policy was updated on December 22, 2025.
Effective January 1, 2026, Regional Accountable Entities (RAEs) are permitted to prior authorize psychotherapy services beyond 24 sessions per member in a given state fiscal year (July 1 - June 30), in any combination of the impacted psychotherapy codes (with the exception of crisis codes) and across all provider types. The Department of Health Care Policy and Financing (HCPF) affirms that RAEs will remain in compliance with all federal and state parity regulations as they implement these new utilization management mandates.
This policy change was authorized following the 2025 Special Legislative Session and the passage of Senate Bill 25B-001.
Please refer to the FAQ below.