Verify Member Eligibility and Co-Pay
Table of Contents
- Verifying Member Eligibility
- Verifying Co-Pay Amount
- Verifying Remaining Service Units - PT/OT
- Verifying Remaining Service Units - Behavioral Health
- Verifying Child Health Plan Plus (CHP+) Coverage
- Verifying Managed Care Assignment
- Benefit Plans and Billing Instructions
- Verifying Third-Party Liability Coverage
Verifying Member Eligibility
- Log in to the Provider Web Portal.
- Click the Eligibility tab.
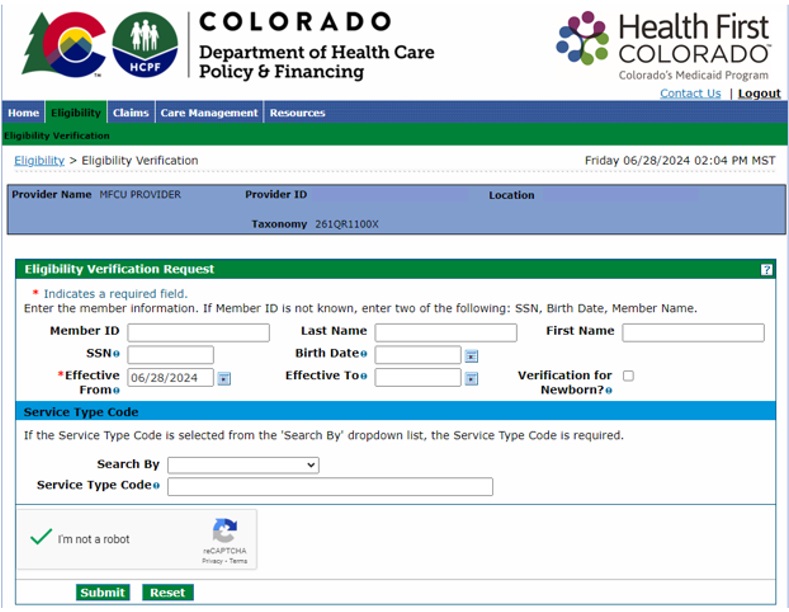
- Click the Eligibility Verification link.

Enter search criteria (including the date of service), complete the CAPTCHA verification and click "Submit." Effective search criteria include one of the following combinations of member information:
- Member ID
- Last Name, First Name and Birth Date
- Last Name, First Name and Social Security Number
- Birth Date and Social Security Number
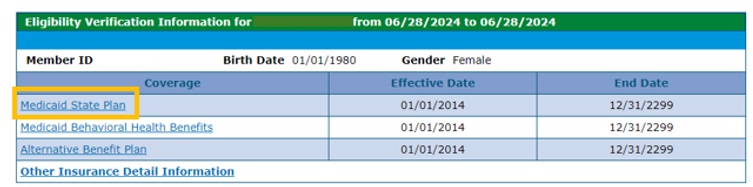
Confirm coverage types before rendering any services or submitting claims. Look carefully at effective and end dates. Eligibility coverage types listed in the Provider Web Portal include (but are not limited to):
- Medicaid: "Medicaid State Plan" and "TXIX" (Title XIX [Title 19])
- Behavioral Health Coverage through the Regional Accountable Entities (RAEs): "Medicaid Behavioral Health Benefits" and "BHO+B"
- Home and Community-Based Services Waiver: “HCBS ___ Waiver”
- Child Health Plan Plus: “Child Health Plan Plus” and “CHP+B”
- Medicare: “Qualified Medicare Beneficiary” and “QMB”
- If a member has QMB coverage but does not have Medicaid State Plan (TXIX) coverage, Health First Colorado will not provide payment unless Medicare pays first.
- If a member has QMB and Medicaid State Plan (TXIX) coverage, then Health First Colorado is the secondary payer.
- Health First Colorado is always the payer of last resort. Providers must be enrolled with and bill Medicare before submitting claims to Health First Colorado through the fiscal agent Gainwell Technologies. Providers have 120 days from the Medicare Explanation of Benefits (EOB) date to submit claims to Gainwell Technologies.
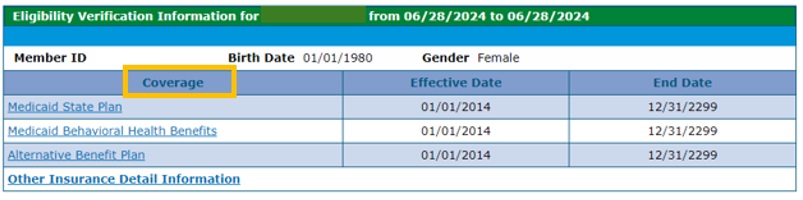
- To identify any Third-Party Liability (TPL), or commercial insurance, click on “Other Insurance Detail Information.” Providers are able to add TPL information here as well.
Health First Colorado is always the payer of last resort. Providers must be enrolled with and bill the TPL as the primary payer before submitting claims to Health First Colorado through the fiscal agent Gainwell Technologies. Claims must be submitted to Gainwell Technologies with the TPL’s Explanation of Benefits (EOB) date within 365 days from the date of service.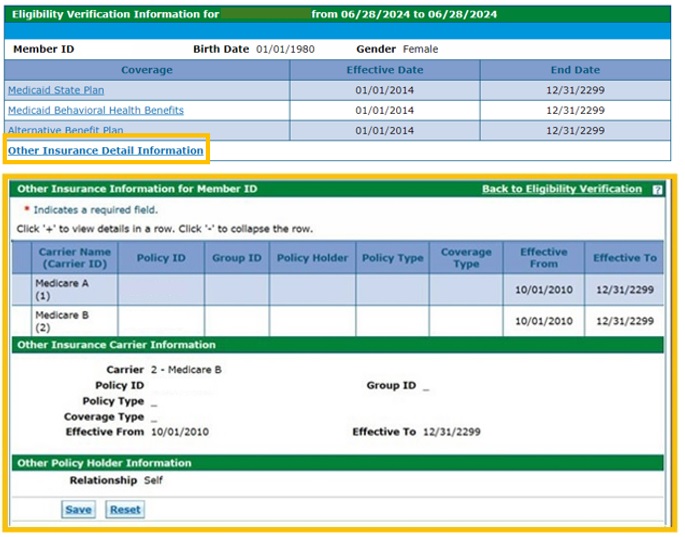
- For more information about a Coverage type, click on the title of the Coverage.
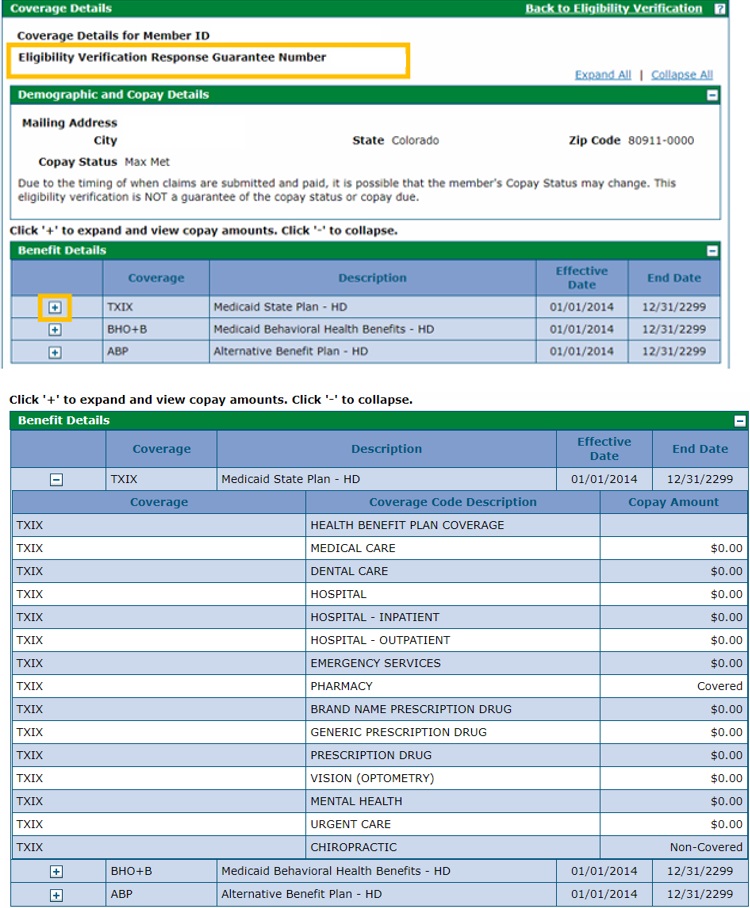
Note the Eligibility Verification Response Guarantee Number at the top of the screen. Click the + symbol next to a Coverage type for more information on coverage and co-pays.
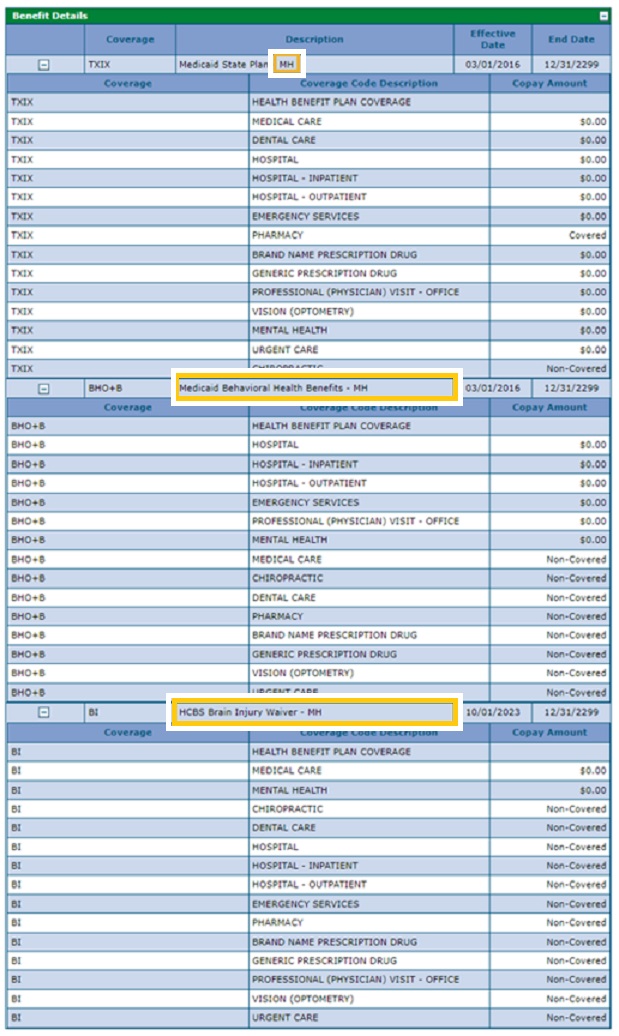
The screenshot below shows Coverage details for a member covered by the Home and Community-Based Services (HCBS) benefit, indicated by the modifier "MH"
- Brain Injury: "BI"
- Community Mental Health Supports: "CMHS"
- Complementary and Integrative Health: "CIH"
- Developmental Disabilities: "DD"
- Elderly, Blind and Disabled: "EBD"
- Supported Living Services: "SLS"
- Children with Life Limiting Illness: "CLLI"
- Children’s Extensive Support: "CES"
- Children’s Habilitation Residential Program: "CHRP"
- Children’s Home and Community-Based Services: "CHCBS"
Members must show a benefit plan as well as the MH code for claims to process correctly. If the benefit plan is missing, HCBS providers may submit a request via this form to update a benefit plan. HCBS providers should not contact the county or the case manager to update the benefit plan.
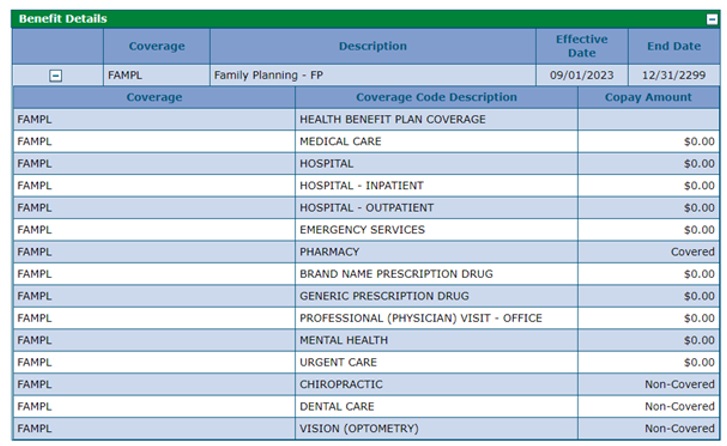
The screenshot below shows benefit details for a member covered by the Family Planning (FAMPL) benefit. A member with FAMPL is eligible for family planning services or family planning-related services when the intent of the service is to delay, prevent or plan for a pregnancy.
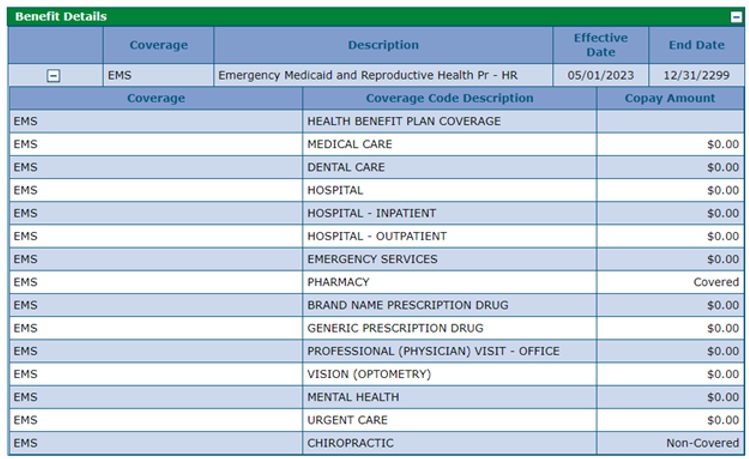
The screenshot below shows benefit details for a member covered by the Emergency Medicaid and Reproductive Health Program (EMS). EMS is a limited benefit that covers emergency, family planning and family planning-related services.
Verifying Co-Pay Amount
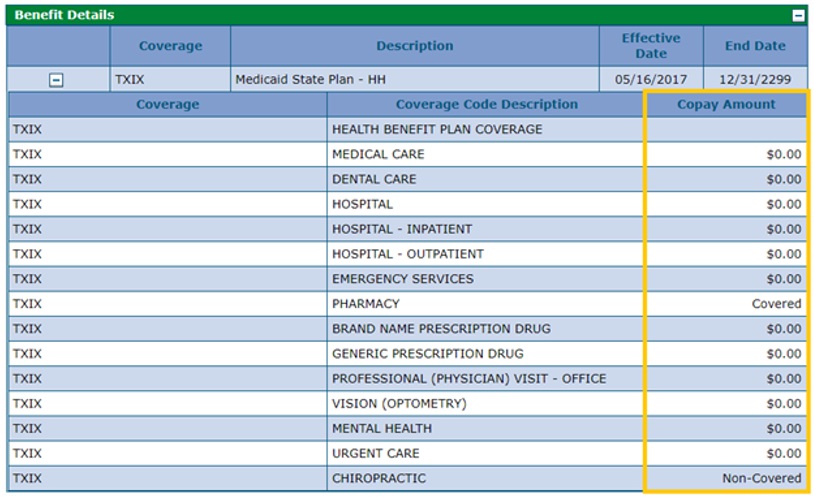
Verify member co-pay requirements by referring to the "Copay Amount" column under the Benefit Details section.
Members may not be required to pay a co-pay for every visit, so it is important that providers check the co-pay amount every time they see a Health First Colorado member.
If a member has already reached their 5% co-pay maximum for a given month, or they are exempt, the “Copay Amount” field will display $0. “Non-Covered” will show when the coverage code is inactive for the member's associated coverage during the Coverage effective dates.
The Pharmacy Coverage Code Description (CCD) will be used in conjunction with the “Brand Name Prescription Drug” and “Generic Prescription Drug” CCDs. If a value of “Covered” for Pharmacy services is received, the base co-pay due will reside in values next to “Brand Name Prescription Drug” and/or “Generic Prescription Drug.”
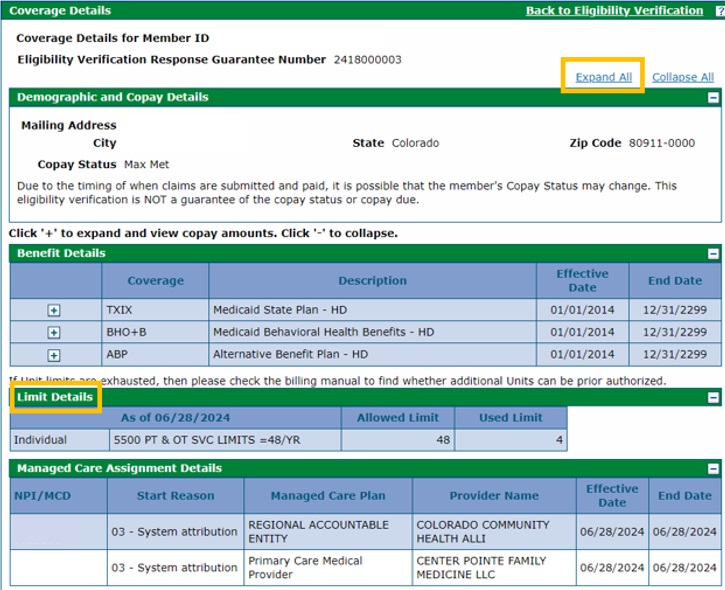
Verifying Remaining Service Units – PT/OT
- Click “Expand All” at the top of the screen to view Limit Details. Refer to the Verifying Remaining Service Units Quick Guide for more information regarding Physical or Occupational Therapy remaining units.
Verifying Remaining Service Units - Behavioral Health
- If applicable, check the member's available units of short-term behavioral health services under the Limit Details section.
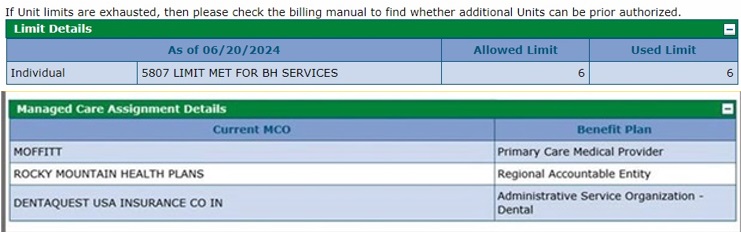
"5807 LIMIT MET FOR BH SERVICES" references the system audit that will post when the service unit limit is exceeded.
This used benefit amount is calculated by subtracting all the paid units of service for short-term behavioral health a member has incurred within the current state fiscal year from the limit. Once the unit limit has been reached for the state fiscal year, a Prior Authorization Request (PAR) cannot be used to exceed it.
Additional visits beyond the unit limit during a state fiscal year may be eligible for reimbursement by the Regional Accountable Entity (RAE) in accordance with their provider credentialing and utilization management policies and procedures. At the beginning of the next state fiscal year, the total units for that fiscal year will be available.
Verifying Child Health Plan Plus (CHP+) Coverage
When a member is enrolled with CHP+, they are assigned one of four (4) Managed Care Organizations (MCOS). However, the original CHP+ eligibility is in the system before the MCO gets assigned. In this gap, they will bill claims directly to Gainwell as "fee for service (FFS)". Providers must bill claims directly to the MCO directly once the member is assigned.
Claims for members who are eligible for CHP+ but are not yet enrolled in a CHP+ MCO should be submitted to Gainwell Technologies, the Department of Health Care Policy & Financing’s (the Department’s) fiscal agent, for reimbursement or Prime Therapeutics for pharmacy services.
The Benefit Details Effective Date must be set prior to the CHP+ Managed Care Assignment Effective Date. For example, in the following screenshot, any services provided from May 1, 2021, through July 14, 2021, would be billed as fee-for-service claims to Gainwell Technologies. Services provided on and after July 15, 2021, would be billed directly to the MCO. Providers must be enrolled with the MCO.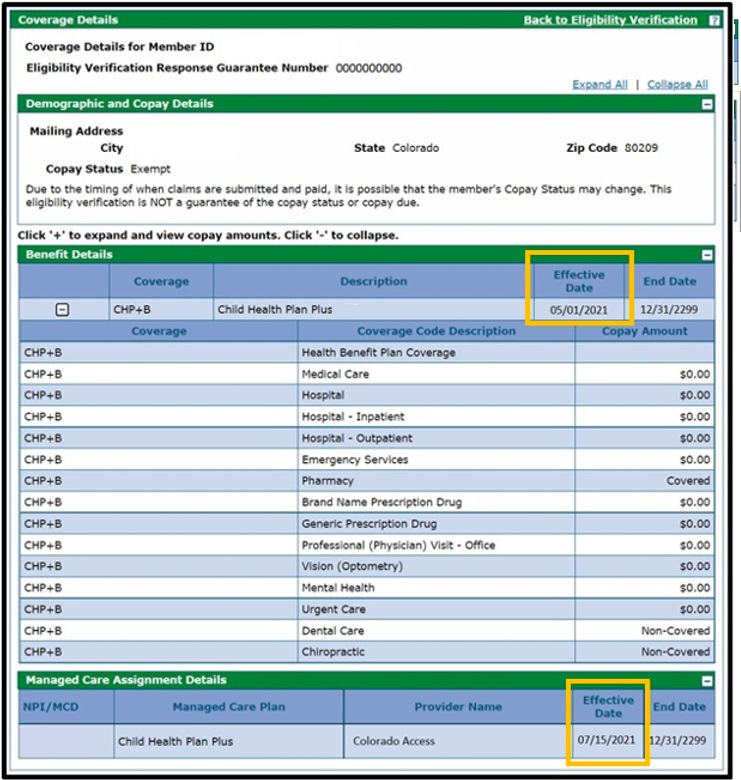
CHP+ Managed Care Organizations include:
- Colorado Access (also serves as a Regional Accountable Entity for Health First Colorado)
- Denver Health (closed network)
- Kaiser Permanente (closed network)
- Rocky Mountain Health Plans (also serves as a Regional Accountable Entity for Health First Colorado)
Verifying Managed Care Assignment
Click “Expand All” at the top of the screen to view Managed Care Assignment Details. This panel will display only if the member is assigned to a managed care plan. It will show all of the plans the member is assigned to, as well as their effective dates of coverage. Refer to the “Benefit Plans and Billing Instructions” table below for more information on how to verify co-pay amounts and submit claims. Managed Care Organizations (MCOs) process all of their own claims.
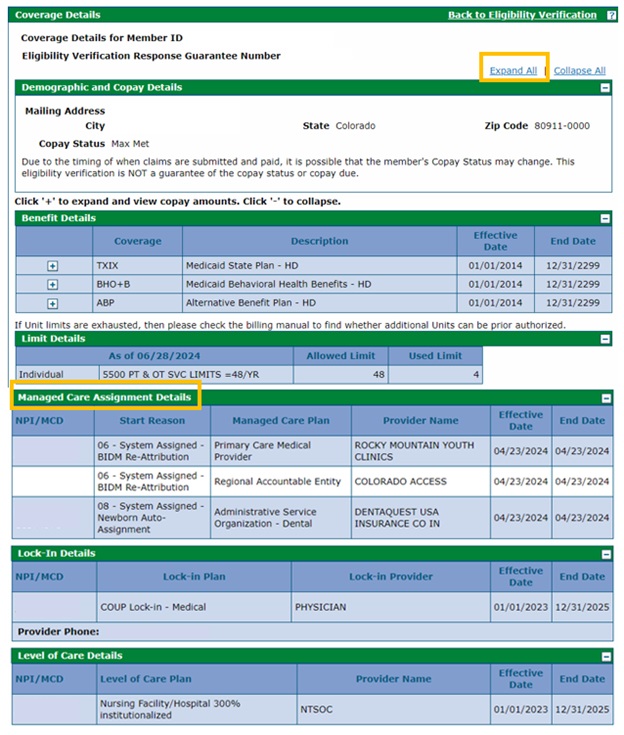
The coverage information will include the name or type of coverage and the effective and end dates of that coverage. Additional information returned in the eligibility response may display the following details panels in addition to the Managed Care Assignment Details:
- Lock-in Details is displayed when a member is locked in or restricted to a specific provider known as a “lock-in plan.” To authorize services delivered for a member by a provider other than the designated Lock-in Plan Provider, claims must include the referring provider's National Provider Identifier (NPI). The Lock-in Details panel provides the Lock-in Provider's Doing Business As (DBA) Name and Provider Phone information.
- Level of Care Details is displayed when a member resides in a nursing home and reports their level of care within that facility.
Benefit Plans and Billing Instructions
See the table below for a complete list of all possible benefit plans along with billing instructions and co-pay notes.
Benefit Plan | Billing Medical Claims | Billing Behavioral Health Claims | Co-Pay |
Health First Colorado Managed Care Organizations (MCOs): Medical Claims | |||
Note: Span must show "Active."
Denver Health also serves as a Child Health Plan Plus (CHP+) MCO | Denver Health | Colorado Access (even if Denver Health Medical Plan shows as the Regional Accountable Entity [RAE]) | Most services, such as office visits, medications and hospital visits have a co-pay. Services for pregnant women, children 18 and under, American Indians and Alaska Natives do not require a co-pay. |
Rocky Mountain Health Plans Prime Rocky Mountain Health Plans also serves as a Regional Accountable Entity (RAE) and as a Child Health Plan Plus (CHP+) MCO | Rocky Mountain Health Plans Prime | Rocky Mountain Health Plans Prime | Contact Rocky Mountain Health Plans Prime for co-pay details. |
PACE | PACE | There are no co-pay amounts or out-of-pocket expenses for services covered under this program. | |
Regional Accountable Entities (RAEs): Behavioral Health Claims | |||
Accountable Care Collaborative (ACC)
Note: ACC will only appear for dates of service prior to 7/1/18. | Gainwell Technologies | Appropriate Regional Accountable Entity (RAE) | Not applicable |
Regional Accountable Entities (RAEs) (formerly known as Behavioral Health Organizations [BHOs] and Regional Care Collaborative Organizations [RCCOs]) | Gainwell Technologies, unless the member has Denver Health Public Health Intervention Program (PHIP) or Rocky Mountain Health Plans Prime | Appropriate Regional Accountable Entity (RAE)
Behavioral therapy is an exception and should be billed directly to Gainwell Technologies. | There are no co-pay amounts for Health First Colorado behavioral health services. However, if the member has other insurance, they must use that insurance first before using Health First Colorado benefits. |
RAE: Colorado Access Behavioral Health for Denver Health Medical Choice | Denver Health Medical Choice | Colorado Access
Behavioral therapy is an exception and should be billed directly to Gainwell Technologies. | There are no co-pay amounts for Health First Colorado behavioral health services. However, if the member has other insurance, they must use that insurance first before using Health First Colorado benefits. |
| Current contracts with the RAEs, referred to as Phase II, will end on June 30, 2025. New contracts, referred to as Phase III, will launch on July 1, 2025. As part of this transition, the number of RAEs will be reduced from seven (7) to the following four (4) regions. | |||
RAE, Region 1: Rocky Mountain Health Plans Rocky Mountain Health Plans also serves as a Health First Colorado Managed Care Organization (MCO) and as a Child Health Plan Plus (CHP+) MCO | Gainwell Technologies, unless the member belongs to a Managed Care Organization (MCO) | Rocky Mountain Health Plans
Behavioral therapy is an exception and should be billed directly to Gainwell Technologies. | There are no co-pay amounts for Health First Colorado behavioral health services. However, if the member has other insurance, they must use that insurance first before using Health First Colorado benefits. |
RAE, Region 2: Northeast Health Partners (NHP) | Gainwell Technologies, unless the member belongs to a Managed Care Organization (MCO) | Northeast Health Partners (NHP)
Behavioral therapy is an exception and should be billed directly to Gainwell Technologies. | There are no co-pay amounts for Health First Colorado behavioral health services. However, if the member has other insurance, they must use that insurance first before using Health First Colorado benefits. |
RAE, Region 3: Colorado Community Health Alliance
| Gainwell Technologies, unless the member belongs to a Managed Care Organization (MCO) | Colorado Community Health Alliance (CCHA)
Behavioral therapy is an exception and should be billed directly to Gainwell Technologies. | There are no co-pay amounts for Health First Colorado behavioral health services. However, if the member has other insurance, they must use that insurance first before using Health First Colorado benefits. |
RAE, Region 4: Colorado Access Colorado Access also serves as a Child Health Plan Plus (CHP+) Managed Care Organization (MCO) | Gainwell Technologies, unless the member belongs to a Managed Care Organization (MCO) | Colorado Access
Behavioral therapy is an exception and should be billed directly to Gainwell Technologies. | There are no co-pay amounts for Health First Colorado behavioral health services. However, if the member has other insurance, they must use that insurance first before using Health First Colorado benefits. |
Primary Care Medical Providers (PCMPs) | |||
Denver Health and Hospital Authority-Primary Care Medical Provider (PCMP) | Gainwell Technologies | Appropriate Regional Accountable Entity (RAE) | Not applicable |
Primary Care Medical Provider (PCMP) | Gainwell Technologies | Appropriate Regional Accountable Entity (RAE) | Not applicable |
Dental Claims | |||
Administrative Service Organization - Dental | DentaQuest |
| Contact DentaQuest for co-pay details. |
Child Health Plan Plus (CHP+) Dental
Note: The CHP+ State Managed Care Network (SMCN) will no longer be available to pay for health care services for CHP+ members delivered after 6/30/21. | Providers should bill the CHP+ Managed Care Organization (MCO). If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to a CHP+ MCO, providers should bill fee-for-service claims for services directly to Gainwell Technologies. |
| Some CHP+ members may also have to pay a co-pay to their health care provider at the time of service. There is no co-pay for preventative care, such as prenatal care and check-ups. Other services may require a co-pay based on member income. Native Americans and Alaskan Natives do not have to pay co-pay amounts.
|
Child Health Plan Plus (CHP+): Medical and Behavioral Health Claims | |||
Note: The CHP+ State Managed Care Network (SMCN) will no longer be available to pay for health care services for CHP+ members delivered after 6/30/21. | Providers should bill the CHP+ Managed Care Organization (MCO). If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to a CHP+ MCO, providers should bill fee-for-service claims for services directly to Gainwell Technologies. | Providers should bill the CHP+ Managed Care Organization (MCO). If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to a CHP+ MCO, providers should bill fee-for-service claims for services directly to Gainwell Technologies. | Some CHP+ members may also have to pay a co-pay to their health care provider at the time of service. There is no co-pay for preventative care, such as prenatal care and check-ups. Other services may require a co-pay based on member income. Native Americans and Alaskan Natives do not have to pay co-pay amounts. |
Colorado Access – CHP+ Managed Care Organization (MCO) Colorado Access also serves as a Regional Accountable Entity (RAE) | Providers should bill Colorado Access. If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to Colorado Access, providers should bill fee-for-service claims directly to Gainwell Technologies. | Providers should bill Colorado Access. If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to Colorado Access, providers should bill fee-for-service claims directly to Gainwell Technologies. | Contact Colorado Access for co-pay details. |
CHP+ by Denver Health Medical Plan – CHP+ Managed Care Organization (MCO) Denver Health also serves as a Health First Colorado MCO | Providers should bill Denver Health. If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to Denver Health, providers should bill fee-for-service claims directly to Gainwell Technologies. | Providers should bill Denver Health. If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to Denver Health, providers should bill fee-for-service claims directly to Gainwell Technologies. | Contact Denver Health Medical Plan for co-pay details. |
Kaiser Permanente – CHP+ Managed Care Organization (MCO) | Providers should bill Kaiser Permanente. If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to Kaiser Permanente, providers should bill fee-for-service claims directly to Gainwell Technologies. | Providers should bill Kaiser Permanente. If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to Kaiser Permanente, providers should bill fee-for-service claims directly to Gainwell Technologies. | Contact Kaiser Permanente for co-pay details. |
Rocky Mountain Health Plans – CHP+ Managed Care Organization (MCO) Rocky Mountain Health Plans also serves as a Health First Colorado MCO and as a Regional Accountable Entity (RAE) | Providers should bill Rocky Mountain Health Plans. If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to Rocky Mountain Health Plans, providers should bill fee-for-service claims directly to Gainwell Technologies. | Providers should bill Rocky Mountain Health Plans. If a CHP+ member’s eligibility start date occurs prior to the member’s assignment to Rocky Mountain Health Plans, providers should bill fee-for-service claims directly to Gainwell Technologies. | Contact Rocky Mountain Health Plans for co-pay details. |
Verifying Third-Party Liability Coverage
- To see Third Party Liability (TPL) coverage (including Medicare), return to the Eligibility Verification page.

- Scroll to the bottom of the page and click "Other Insurance Detail Information."
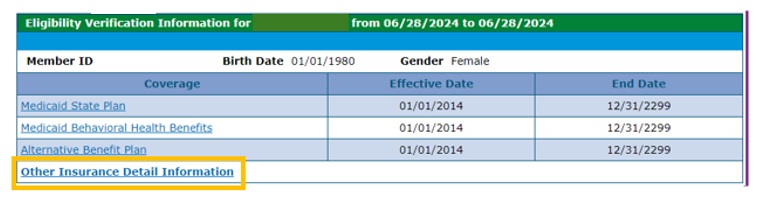
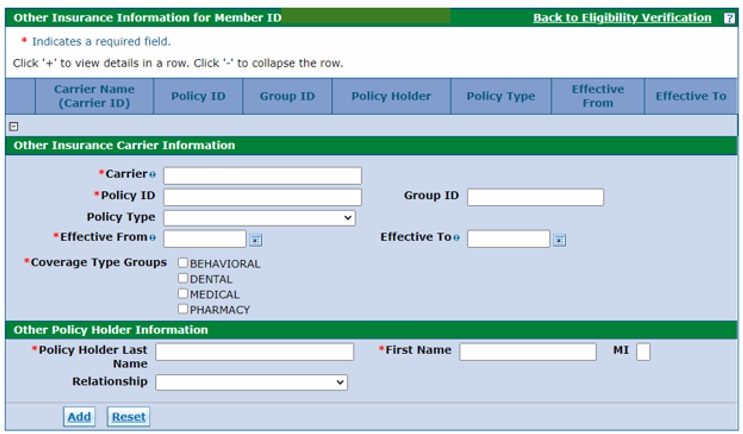
This is where other insurance coverage (including Medicare coverage) is displayed:
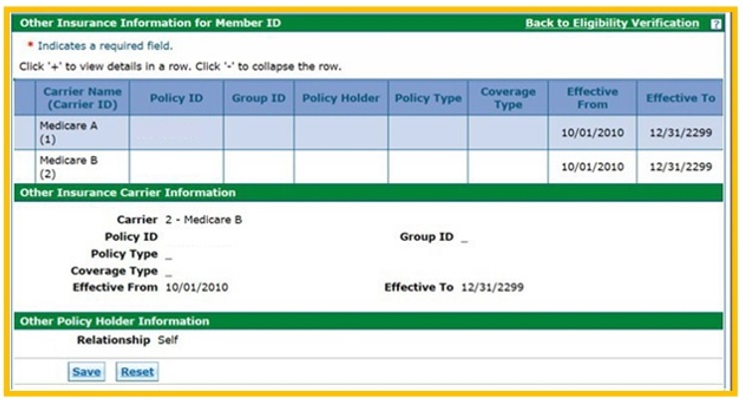
Add additional Third-Party Liability (TPL) information as needed.
Refer to the "Adding and Updating Additional TPL Information Provider Web Portal Quick Guide" for step-by-step instructions on how to add TPL information for a member with TPL coverage that isn't already listed.
For Medicare, Health First Colorado is always the payer of last resort. Providers must be enrolled with and bill Medicare before submitting claims to Health First Colorado through the fiscal agent Gainwell Technologies. Providers have 120 days from the Medicare Explanation of Benefits (EOB) date to submit claims to Gainwell Technologies.
For Commercial Insurance, Health First Colorado is always the payer of last resort. Providers must be enrolled with and bill the commercial insurance as the primary payer before submitting claims to Health First Colorado.
Need More Help?
Visit the Quick Guides web page to find all the Provider Web Portal Quick Guides.