Verifying Remaining Therapy Service Units
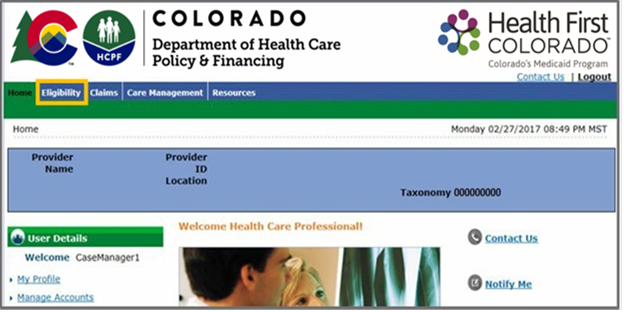
- Log in to the Provider Web Portal.
- Click the Eligibility tab.
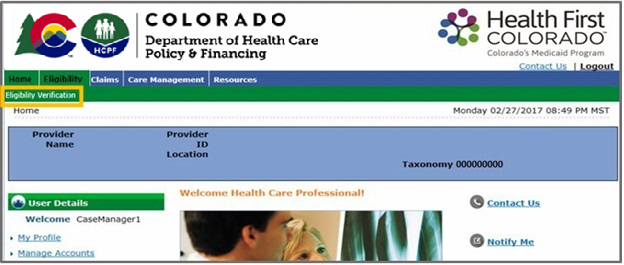
- Click the Eligibility Verification link.
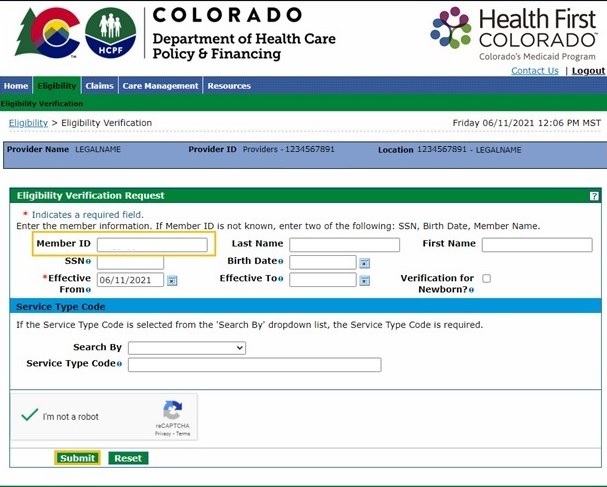
- Enter search criteria, then click "Submit."
Check the member's available units of physical/occupational therapy (PT/OT) services under the Limit Details section by clicking “Expand All” at the top of the screen.
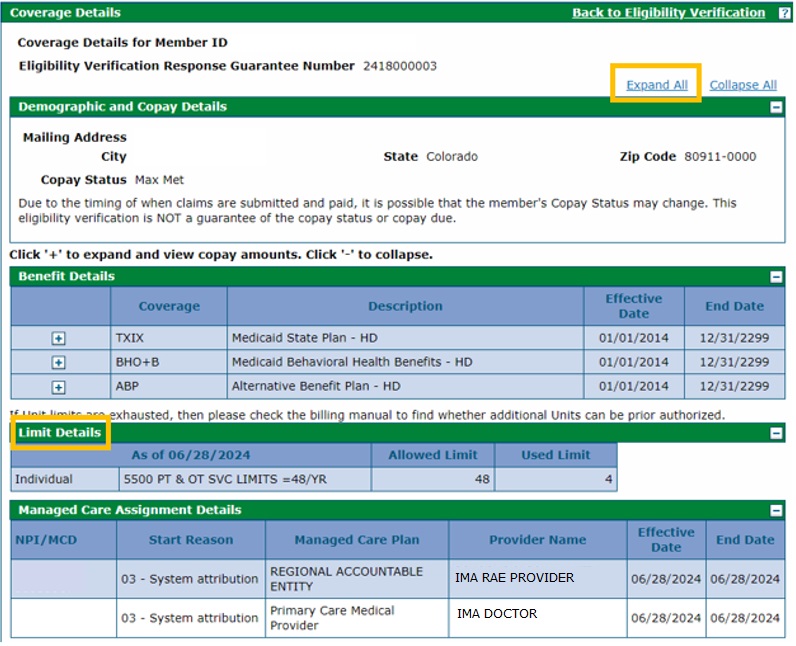
The remaining benefit amount for each member represents PT/OT units of service that have been billed and paid in the previous rolling 365 days. An approved Prior Authorization Request (PAR) is required for additional units.
The function will calculate PT/OT units regardless of whether they were paid with a PAR on file.
Refer to the Benefit Limitation Frequently Asked Questions, located on the Outpatient PT/OT Benefits web page, for more information.
The allowed billing provider is reimbursed for covered speech therapy services so that Title XIX (TXIX) and Alternative Benefit Plan (ABP) members can receive Speech Therapy service within the limit and beyond the limit with prior authorization.
Need More Help?
Visit the Quick Guides web page to find all the Provider Web Portal Quick Guides.