Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS)
- Program Overview
- Eligible Providers
- Prescribing Providers
- Billing Providers
- Covered Benefits
- Durable Medical Equipment
- Transcutaneous or Neuromuscular Electrical Nerve Stimulators (TENS or NMES)
- Osteogenic Stimulators
- Lymphedema Pumps and Compressors
- Continuous Passive Motion (CPM) Devices
- Speech Generating Devices (SGDs)
- Cochlear Implant/ Bone-Anchored Hearing Aid (BAHA) Replacements
- Oxygen Contents and Oxygen Delivery Systems
- Continuous and Bilevel Positive Airway Pressure Devices (CPAP/BiPAP)
- Mobility Equipment (Manual Wheelchairs, Power Wheelchairs and Scooters)
- Complex Rehabilitation Technology (CRT)
- Enclosed/Safety Bed Criteria
- Bed Rails
- Vocational Items
- Hip Kits
- Prosthetics and Orthotics (P&O)
- Supplies
- Special Considerations
- Pricing
- Durable Medical Equipment
- Prior Authorization Requests (PARs)
- Return of Incorrect Equipment
- Record Keeping
- General Billing Information
- Using Modifiers
- Procedure/HCPCS Codes Overview
- Paper PAR Instructional Reference
- Paper Claim Reference Table
- Column Instructions for HCPCS Code Table
- HCPCS Code Table
- CRT HCPCS Code Table
- Retired DMEPOS Policies
- DMEPOS Revisions Log
Return to Billing Manuals Web Page
Program Overview
Health First Colorado (Colorado's Medicaid program) covers Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) as described in this manual. Durable Medical Equipment (DME) is defined as equipment that can withstand repeated use and that generally would be of no value to the member in the absence of a disability, illness or injury. Prosthetics and Orthotics (P&O or O&P) are defined as replacement, corrective, or supportive devices that artificially replace a missing portion of the body, prevent or correct physical deformity or malfunction, or support a weak or deformed portion of the body. Disposable Medical Supplies (Supplies) are defined as supplies that are specifically related to the active treatment or therapy for an illness or physical condition, they are non-durable, disposable, consumable and/or expendable. This manual gives a summary of the covered DMEPOS benefits. It is periodically modified as new billing or policy information is implemented, therefore, the information in this manual is subject to change. The DMEPOS benefit may also be referred to as 'DME' or 'Supply'.
The list of open Supply Healthcare Common Procedure Coding System (HCPCS) Codes is provided in this manual, which Health First Colorado updates and makes available to all enrolled DME providers at least annually. Refer to the HCPCS Code Table section in this manual for updated benefit coverage, limitations, and prior authorization request (PAR) requirements. Providers may refer to the Code of Colorado Regulations, Program Rules (10 CCR 2505-10 Section 8.590), for specific regulations and guidance on providing the DMEPOS benefit.
Eligible Providers
Providers must be enrolled as a Health First Colorado provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
Note: For members with primary insurance refer to the PAR submission instructions below.
Prescribing Providers
DMEPOS must be prescribed by a physician, physician assistant, nurse practitioner, occupational therapist (effective 08/06/2025), or physical therapist (effective 08/06/2024). The prescription must be within the scope of the prescribing provider's license.
Over-the-counter rapid COVID tests may also be prescribed by a pharmacist.
Breast pumps may also be prescribed by a certified nurse midwife, effective 12/01/2022.
Billing Providers
Billing Providers (the provider that bills/submits the claim) must acquire and retain Medicare DME accreditation and must be enrolled with the Department of Health Care Policy & Financing (the Department) as a Supply Provider. At the time of enrollment, the Department requires proof of Medicare accreditation. The following exceptions apply:
- Pharmacies with less than 5% of total revenue received from DMEPOS are not required to obtain Medicare accreditation.
- Pharmacies and Prosthetic and Orthotic only providers are not required to provide proof of Medicare DME accreditation.
Mail order and out of state pharmacies do not qualify to provide DMEPOS though they may separately enroll as a Supply provider.
Out of state DMEPOS providers may only provide services for crossover Medicare/Health First Colorado members or have a specialized product that cannot be obtained through an in-state DMEPOS provider.
The Billing Provider must retain the member's prescription and related documentation for services for at least six (6) years and make it available for audit by the Department and its agents or representatives.
Covered Benefits
DMEPOS must be medically necessary and prescribed by an authorized prescriptive authority for use by an eligible member. The following are categories of covered benefits and are further outlined in this section. Additional DMEPOS items are listed in the DMEPOS HCPCS Code section of this manual.
Durable Medical Equipment
DME refers to equipment and appliances that are primarily and customarily used to serve a medical purpose, generally are not useful to an individual in the absence of a disability, illness or injury, can withstand repeated use, and can be reusable or removable. DME may be rented or purchased.
Purchase: These items are purchased for a member.
Rental/Purchase: In general, these items are rented or purchased as follows:
- The item is rented if the physician, physician assistant, nurse practitioner or occupational therapist documents that the anticipated need is six (6) months or less.
- The item may be rented or purchased if the physician, physician assistant, nurse practitioner or occupational therapist documents that the anticipated need exceeds six (6) months.
- Some items are required to be rented or purchased as indicated within this manual.
Once rental is initiated on an item, a subsequent request for prior approval of purchase of that item must be accompanied by additional supporting documentation validating the need for purchase. Rental reimbursements may not exceed the purchase price of the item. Once the purchase price of the item is reached, the rental will be considered purchased and no additional reimbursement will be made.
Example: If the monthly rental for an item is $30 and the new purchase price is $200, Health First Colorado will pay six (6) full months of rental, plus no more than $20 in the seventh month of rental. At that time, the item becomes the property of the member, and no more rental payments are made.
Continuous Rental: Most rented equipment will convert to purchase when the purchase price is met. The following are exceptions to this policy and may be rented indefinitely as they require frequent and/or substantial servicing:
- Oxygen Equipment
- Ventilators
Transcutaneous or Neuromuscular Electrical Nerve Stimulators (TENS or NMES)
A prior authorization request (PAR) that includes a completed Questionnaire #9 is required for rental and purchase. A TENS or NMES unit must be trialed for at least a two (2) month rental period before a request for purchase will be considered.
- All rental months must include the RR modifier on both PARs and claims.
- In addition to the RR modifier, claims for the first month of rental must also include the KH modifier.
- In addition to the RR modifier, claims for the second month (and if applicable, the third month) of rental must also include the KI modifier.
- The purchase price is equivalent to 10 months of rental, requests for more than 10 months of rental will not be approved. The unit is considered owned by the member once the purchase price has been reached.
- All supplies (i.e., lead wires, electrodes, batteries, etc.) are inclusive of the rental reimbursement and cannot be billed for separately while the unit is rented.
Osteogenic Stimulators
The following criteria applies to osteogenic stimulators effective for prior authorization requests submitted on or after February 1, 2024.
This equipment is considered medically necessary in the treatment of nonunion fractures, when:
- A minimum of two (2) sets of radiographs are obtained at least 90 days apart, prior to starting treatment with the equipment. Each radiograph set must include multiple views of the fracture site accompanied with a written interpretation by a physician stating that there has been no clinically significant evidence of fracture healing between the two (2) sets of radiographs; and,
- Documentation that the member had a least one (1) unsuccessful surgical intervention for the treatment of the fracture.
- For Adults with nonunion fractures of the skull, vertebrae, and those that are tumor-related are excluded from coverage.
- Ultrasonic osteogenic stimulators may not be used concurrently with other non-invasive osteogenic devices.
Lymphedema Pumps and Compressors
Advanced compression devices may be covered only when all other interventions have failed.
Continuous Passive Motion (CPM) Devices
CPM devices may be medically necessary only when requested for total knee replacements. Please see procedure code E0935.
Speech Generating Devices (SGDs)
Health First Colorado covers Augmentative and Alternative Communication Devices (AACD) which allows a client with an expressive speech language disorder to electronically represent vocabulary and express thoughts or ideas to meet the client’s speech needs, as an in-home benefit.
AACD are covered for members who have a condition that inhibits communication. AACDs are provided upon recommendation by a speech-language pathologist after the client has completed a comprehensive assessment and medical necessity for the device has been well documented.
They may be approved to support communication and improve health outcomes for clients with severe dysarthria, apraxia, aphasia, and other conditions that severely inhibit communication.
A speech-language pathology assessment must provide evidence that alternative, natural communication methods have been ineffective before an AACD will be considered. The assessment documentation should support the recommended AACD by including the client’s medical need, ability to operate the device both cognitively and physically, and expected improvement in the following.
- Ability to communicate medical needs;
- Ability to express basic needs;
- Ability to provide feedback on treatment or therapy programs;
- Prevention of secondary impairments;
- Independence and personal safety.
Digitized speech devices, synthesized speech devices and tablet computers are described below. Certain speech-generating software and necessary accessories are also covered once a client is approved for an AACD.
Digitized Speech Devices (Procedure Codes E2500, E2502, E2504, and E2506)
Digitized speech devices, sometimes referred to as “whole message” speech output devices, use words or phrases that have been recorded by someone other than the AACD system user. The following four (4) options describe the types of digitized speech devices available:
- A speech generating device using pre-recorded messages, less than or equal to eight (8) minutes recording time.
- A speech generating device using pre-recorded messages, greater than eight (8) minutes but less than or equal to 20 minutes recording time.
- A speech generating device using pre-recorded messages, greater than 20 minutes but less than or equal to 40 minutes recording time.
- A speech generating device using pre-recorded messages, greater than 40 minutes recording time.
Synthesized Speech Devices (Procedure Codes E2508 and E2510)
Synthesized speech devices utilize technology that allows input from the AACD system user in order to generate speech. These devices are not limited to pre-recorded messages, allowing the AACD system user to independently create messages. The following two (2) options describe the types of synthesized speech devices available:
- A speech generating device that formulates messages through letters and requires direct selection with the device.
- A speech generating device that formulates messages through multiple methods of message creation and device access.
- Message creation capabilities of the device must include two (2) or more of the following: letters, words, pictures or symbols; and
- Device access must be through direct selection with a keyboard or touch screen and one (1) of more of the following indirect selection techniques: joystick/switches, head mouse, touch-enter, optical head pointer, light pointer, infrared pointed, scanning device or morse code.
Tablet Computers (Procedure Code E1399 with AV Modifier)
For this policy, “tablet computer” refers to a portable, integrated speech-generating device contained in a single panel that utilizes touch screen technology as the primary input for operation. As technology advances and becomes available, other primary input capabilities developed for tablet computers will be considered, e.g. operation by eye gaze/eye control.
- Tablet computers are a benefit when all AACD medical necessity criteria defined in this policy have been met.
- The speech language pathologist will determine the AACD features necessary for effective communication through the assessment. The client must trial a minimum of three (3) devices that have the necessary capabilities determined in the assessment before the recommendation for a tablet computer is submitted.
- The assessment documentation must support the trial findings and the final recommendation for a tablet computer.
- Tablet computer requests must specify that the device has a primary use as an AACD and that the client or client’s caretaker/representative acknowledges and agrees with the usage requirement.
- Prior authorization requests must be submitted using the designated modifier. Requests should also include the recommended software or application, and any necessary accessories designated for the protection and effective use of the device such as a protective case, head pointer, mounting device, etc.
- Note: tablet computers approved for the integrated use as an AACD should be received by the recommended provider/speech language pathologist who can assist the client with loading the approved software and instructing the client on its proper use.
- The minimum replacement timeline for a tablet computer is five (5) years.
- Stolen devices may be replaced within the five (5)-year timeline; however, the client is limited to one (1)-time replacement due to theft, and a police report must be provided for verification of the incident.
- Replacement will not be granted within the five (5)-year timeline for devices that are damaged, lost, misused, abused, or neglected.
- Devices may not be sold or given away during the expected lifetime of use.
Software (Procedure Code E2511)
- Speech generating software and applications are a covered benefit upon approval for an AACD and for client-owned equipment that will primarily be used as a communication device.
- The appropriate software or application must be determined by the speech language pathologist in the assessment with a supporting diagnosis; and
- The recommended software or application must be compatible with the personal computer, tablet computer or personal digital mobile device being used as the client’s AACD.
- The software or application being requested for a client-owned equipment should be supported by detailed trial information as outlined in the previous Tablet Computers section of this policy.
Accessories (Procedure Codes A4601 E1902, E2511, E2512, E2599, and L9900)
- Replacement lithium-ion batteries.
- Non-electric AACD communication board.
- Mounting systems designated for securing the AACD within reach of the client.
- Safety and protection accessories designated to maintain the life expectancy of the device.
- Accessories not otherwise classified may be approved to enhance the use of the AACD system as the client’s condition changes.
- Orthotic and prosthetic supplies and accessories, and/or service components of another HCPCS L code.
Non-Covered Services and General Limitations
Equipment, accessories and supplies that do not have a primary medical use will not be covered, which includes any items that are unnecessary for operation of the AACD or are unrelated to the AACD.
Items that will not be covered include but are not limited to the following:
- Printers
- Laptop or desktop computers
- Other portable, electronic devices that are not designated to have a primary use as an AACD
- Modems, routers or other items used for internet utility services
- Internet, phone or data services
- Accessories that are not designated to have a primary purpose of protecting the AACD
- Applications, software or programs that have not been recommended by the speech language pathologist or are not designated to have a primary use as a communication tool
Prior Authorization Requirements
Prior authorizations for these devices should follow standard PAR practices, as outlined in this manual. There is no required format, form, or questionnaire for submitting prior authorization requests; but the documentation should be inclusive of the following:
- A prescription and recommendation for an AACD, AACD accessories and or AACD software by the client’s physician and licenses speech language pathologist.
- Speech assessment documentation supporting the AACD recommendations, which includes but is not limited to the following:
- Medical diagnosis and description of the current functional needs, communication skills/limitations, and prognosis for improvement or deterioration
- History of communication-related therapies
- Alternative, natural communication methods were proven ineffective
- Evidence of cognitive and physical ability to operate the device
- Medical justification for the recommended device and software
- Description of any trials required for the recommended device, including how each device trial met or failed to meet the client’s functional communication needs
- The recommended device should be capable of modification to meet the needs for anticipated improvement or deterioration of functional communication when possible
- A statement that affirms that the device has a primary use as an AACD and that the client or client’s caretaker/representative acknowledges and agrees with the usage requirement.
SGDs allow a member with an expressive communication disorder (e.g., severe dysarthria, apraxia, aphasia, a laryngectomy and any other conditions that severely inhibit expressive communication) to express thoughts or ideas through an alternative means.
SGDs are classified as either Digitized or Synthesized (CCR 2505-10, § 8.590.1.S):
- Digitized - Use words or phrases that have been pre-recorded by someone other than the member for playback, when commanded by the member.
- Synthesized - Utilize technology that allows input from the member in order to generate speech. These devices are not limited to pre-recorded messages and allow the member to create unique messages.
Tablet Computers are a benefit when they are primarily utilized as a Synthesized SGD.
Tablet Computer - A portable, integrated SGD, contained in a single panel, which utilizes touch screen technology. It is a device that has been manufactured by an entity that does not specialize in the production of SGDs or has not been re-branded specifically as an SGD.
Accessories for SGDs, such as speech generating software, mounting systems, safety and protection accessories (cases, screen protectors, etc.), and alternate access or input methods (buttons, switches, eye gaze, etc.), may be covered.
All PARs for SGDs and/or their accessories must include a communication assessment from the member's Speech Language Pathologist (SLP). (CCR 2505-10, § § 8.590.3.E and 8.590.7.O).
The assessment must include documentation of:
- The member's communication limitations and skills.
- A history of communication-related therapies.
- A description of the trials completed, including how each trial met or failed to meet the member's functional communication needs.
- Evidence that alternative, natural communication methods have been ineffective.
- The member's ability to operate the device or accessory, both cognitively and physically.
- Expected improvement in the member's independence or personal safety, ability to communicate medical and basic needs, provide feedback on treatment or therapy programs, and prevent secondary impairments.
Prior Authorization Request (PAR) Process
As stated above, three (3) trials of three (3) separate SGDs must be done prior to requesting a device. These trials should also include at least two (2) different manufacturers’ software.
Repairs to an SGD or accessory do not require a communication assessment. If the frequency or cumulative cost of repairs is excessive (as determined by Health First Colorado's designated review entity), replacement will be considered. If the cumulative cost of repairs exceeds 60% of the cost of replacing the SGD and/or accessory (including labor), a quote for replacement must be included with the PAR.
Replacement (10 CCR 2505-10, § 8.590.2.K)
The minimum replacement timeline for an SGD is five (5) years, with the following exceptions:
- There has been a significant change in the member's condition (as determined by Health First Colorado's designated review entity).
- Stolen devices may be replaced within the five (5)-year timeline; however, the member is limited to one (1)-time replacement due to theft, and a police report must be provided for verification of the incident.
Replacement accessories do not require an SLP assessment, provided that the replacement is an exact duplicate of the original.
- In the event the original accessory has been discontinued or is otherwise no longer available, a manufacturer recommended alternative would not require an SLP assessment.
Equipment, accessories and supplies that do not have a primary medical use will not be covered, which includes any items that are unnecessary for operation of the SGD or are unrelated to the SGD (10 CCR 2505-10, § 8.590.7.O.3.b.)
Cochlear Implant Processor/Bone-Anchored Hearing Aids (BAHA) Replacements
For lost/stolen processors:
- If stolen, a police report must be filed, and confirmation of the report should be submitted with the PAR.
- Documentation of the product’s warranty must be submitted with the new Prior Authorization Request to verify that a replacement is not covered by the manufacturer. PARs may be pended to verify the purchase date and warranty expiration.
- Documentation related to how the member/caretaker will prevent the situation from occurring again.
- Replacements are covered once per device, per side.
- If the missing device is less than five (5) years old, upgrades will not be authorized as part of the replacement. If the device is greater than five (5) years old and an upgrade is being requested as the replacement, refer to the upgrade policy below.
For upgrades:
- Upgrades can be considered medically necessary for processors that are more than five (5) years old and in the following situations:
- There is documentation that the current device is no longer functional to produce adequate sound, or
- The member has had a documented medical or lifestyle change that has resulted in the current device no longer being appropriate, or
- The device requires repairs that are no longer possible because it is obsolete. PARs may be pended to gather additional details regarding how the device is obsolete.
- All requests must meet the definition of medical necessity as stated in CCR 2505-10 8.076.8
- In all cases, an upgrade must be expected to have at least one (1) of the following:
- Significantly enhance auditory performance
- Decrease possible safety concerns
- Improve member’s quality of life
Oxygen Contents and Oxygen Delivery Systems
Oxygen contents and delivery systems must be billed by the Supply provider.
Continuous and Bilevel Positive Airway Pressure Devices (CPAP/BiPAP)
CPAPs and BiPAPs require a trial (rental) period of 30-90 days, in which the member must demonstrate compliance, before a purchase request will be approved. Home sleep studies are accepted, and Questionnaire #8 is required for adults 21 years of age and over. Compliance is defined as usage that is four (4) hours per night on 70% of nights during a consecutive thirty (30) day period anytime during the approved trial/rental period.
- If the member does not reach compliance by the end of the trial period, a second trial period may be covered within a one (1)-year time frame at the discretion of the treating physician, a new prescription is required but not a new sleep study.
- An extension of a trial period may be requested in the event of unforeseen circumstances (i.e. hospitalization, illness, etc.) and will be considered on a case-by-case basis.
- Members 20 years of age and under may rent for up to six (6) months and provided that they demonstrate increasing compliance a purchase may be approved prior to reaching compliance.
Note: All related supplies are inclusive of the device's rental reimbursement and cannot be billed separately.
CPAP/BiPAP Replacement and Supplies
- If a device is replaced within five (5) years because of loss, theft, or irreparable damage there is no requirement for a new sleep test or trial period.
- If a device is replaced after five (5) years, there must be a face-to-face evaluation by the members treating physician (within six (6) months of the request) that documents that the beneficiary continues to use and benefit from the device. There is no requirement for a new sleep test or trial period.
- When supplies are needed for a member-owned device, the PAR must include either a download from the device that demonstrates compliance or a face-to-face evaluation by the members treating physician (within six [6] months of the request) that documents that the beneficiary continues to use and benefit from the device.
- If a member received a device prior to enrollment with Health First Colorado and is in need of a new device or supplies, then documentation that the beneficiary had a sleep test must be provided with the initial PAR. There is no requirement for a new sleep test unless the documentation from the prior test cannot be provided.
- Requests for replacement devices solely due to the device being older than five (5) years are not medically necessary and will not be covered.
Mobility Equipment (Manual Wheelchairs, Power Wheelchairs and Scooters)
Refer to the Wheelchair Benefit Coverage Policy for wheelchair-specific coverage policy.
All mobility equipment purchases require a PAR and must be accompanied by a signed letter of medical necessity from a physician, physician assistant, nurse practitioner, occupational therapist, or a physical therapist. Customized items must be identified separately and included in the letter of medical necessity.
Members who meet medical criteria guidelines may receive one (1) primary device and, when deemed necessary, one (1) secondary device within a five (5)-year time period. Replacement of stolen equipment requires a police report that conforms to criteria outlined in the Colorado Revised Statutes. Primary and secondary equipment cannot be duplicates.
- Providers must retain record of the serial number for each approved item. All claims for wheelchairs must be submitted with the serial number of the equipment that was approved on the PAR.
- Primary, secondary, and back-up equipment are identified by their modifier(s) and serial number and should be indicated on all wheelchair claims to avoid duplicate claim denials.
- Beginning July 1, 2017, all PARs and claims for:
- New primary and new secondary mobility equipment and all associated components must include the NU modifier.
- New equipment that is replacing existing equipment, the RA modifier should be included.
- Parts (or systems) that are being replaced as part of a modification should include the NU and RA modifier.
- Parts that are being replaced as part of a repair should include the RB modifier and should not include the NU modifier.
Note: Any time used equipment or parts are provided rather than new equipment or parts, the UE modifier should be used or used in place of the NU modifier. Refer to the Used and Refurbished DME and P&O section in this manual for additional information.
Primary and Secondary mobility equipment repairs are a Health First Colorado benefit when the member owns the equipment and the repair cost does not exceed the equipment's replacement cost. Repairs to back-up equipment or the short-term rental of back-up equipment may be covered. PARs for wheelchair repair no longer require a prescription or signature from the physician.
Prior Authorization for Repairs and Modifications
PARs submitted with multiple pieces of equipment on the same request will be denied, each wheelchair or scooter that requires PAR must be submitted on separate requests. The following information must be included in the request, requests lacking any of the following information will result in a denial or will be returned to the provider for the missing information:
- Equipment type indication: manual, power, or scooter and
- Manufacturer, make, and model, and
- Serial number: PARs for repair and modification must identify the serial number of the base equipment in field 16 (paper) or field 12 (electronic) on the PAR form, and
- If available, the original wheelchair purchase date or PAR number, and
- Beginning July 1, 2017, the PAR must contain the RA or RB modifier depending on the request.
PARs for wheelchair repair no longer require a prescription or signature from the physician. The DME supplier must have either supplied the member with the initial equipment and have all corresponding medical documentation on file or must obtain a written order prior to delivery (WOPD) that has the make, model, and serial number of the equipment requiring repair. A new WOPD is not required for each repair as long as the above listed criteria is met.
Note: Repairs for members residing in a nursing facility may be covered if the wheelchair was owned by the member prior to entering the facility. In this instance, the PAR must indicate that the member is residing in the nursing facility by checking "yes" in the appropriate field on the PA request. The PAR will not be processed without this disclosure.
Complex Rehabilitation Technology (CRT)
Complex Rehabilitation Technology (CRT) includes individually configured manual wheelchair systems, power wheelchair systems, adaptive seating systems, alternative positioning systems, standing frames, gait trainers, and specifically designed options and accessories classified as DME. Only qualified CRT suppliers may bill CRT procedure codes. Refer to the CRT HCPCS Code Table section in this manual for the CRT procedure codes.
The following are considered Adaptive Seating Systems and are therefore considered CRT as stated above.
- Special bathing, toileting, showering, and or combination systems.
- Adaptive Car Seats
- Activity Chairs
Adaptive Car Seat and Buckle Clip Policy
Medical Necessity: see 10 CCR 2505-10 8.076.1.8 for the definition of Medical Necessity.
The following non-exhaustive factors establish medical necessity of car seats as a covered benefit for all Health First Colorado members per 10 CCR 2505-10 8.590.2.G.17:
- Has unstable head and/or trunk control or;
- Is unable to independently maintain a seated position or;
- Is in a spica cast and cannot fit in a commercial infant/child car seat/booster seat or;
- Has a condition that results in uncontrolled movement (e.g., seizure)
If a member aged 0-20 has needs functionally comparable to those listed above, or other medically documented positioning needs that fall outside of these four indications, they must be clearly documented for consideration.
Prior Authorization: Use procedure code T5001 for billing purposes. A Prior Authorization Request, a Complex Rehabilitation Technology (CRT) Specialized Assessment, and a Face-to-Face (F2F) evaluation are needed.
Replacement Policy
- Replacement car seats are covered under Code of Colorado Regulations 10 CCR 2505-10 8.590.2.J.
- Members aged 20 and younger, while continuing to grow and develop physically, are eligible for car seat replacement every three (3) years. However, early replacement will be considered with documentation that demonstrates a medical or functional need and why repairs or modifications to the current car seat are not sufficient.
- Members aged 21 and older are eligible for car seat replacement every five (5) years. However, early replacement will be considered with documentation that demonstrates a medical or functional need and why repairs or modifications to the current car seat are not sufficient.
Limitations
- The selected device must be the least costly model that meets the child’s documented medical positioning requirements.
- If a less costly option is available to meet the child’s documented medical needs (e.g., accessories such as buckle clip guards), that option must be used first. Additional information can be found in the Buckle Clip Policy section.
- Documentation must demonstrate the medical need for the car seat, including the condition(s) applicable to the need for the car seat.
- Requests based solely on typical child behavior (e.g., curiosity without an underlying medical or behavioral diagnosis) do not meet the criteria for medical necessity and are not covered.
- Requests based solely on routine passenger-safety concerns, without an underlying medical or behavioral diagnosis, do not meet the criteria for medical necessity and are not covered.
- Conventional car seats are not covered.
- The child’s weight and height do not meet the manufacturer’s product weight/height requirements.
- Accessories that are integral to therapeutic positioning are covered if the clinician documents their medical necessity. Accessories that do not assist with positioning or are not related to modifying the car seat for growth purposes are not covered.
- Car seats that are intended for use beyond the intended function as a car seat (e.g., as an in-home positioning chair) are not covered.
- If a car seat must be modified or paired with adaptive accessories to meet a medical need, those modifications must be documented.
Buckle Clip Policy
Clip guards (also called chest clip guards, harness clip guards, or buckle guards) are small plastic or fabric devices attached to a car seat harness. The purpose of these clips is to prevent a child with a developmental or cognitive disorder from unbuckling or manipulating the harness system while the vehicle is in use.
Prior Authorization: Use E1399 for billing purposes. Providers must provide education to the member’s parent or legal guardian on the use of the buckle clip and any associated risks. Providers will also be required to provide documentation of the education that was completed.
Replacement Policy: Replacement buckle clips are covered under Code of Colorado Regulations 10 CCR 2505-10 8.590.2.J.
Limitations
- Documentation must show the member has a developmental or cognitive disorder or impairment that can lead to frequent unbuckling or eloping and would make travel with a car seat unsafe.
- If the use of a buckle clip fails to address the developmental or cognitive disorder or impairment adequately, this must be documented, and an alternative solution may be covered.
- Requests based solely on routine passenger-safety concerns, without an underlying medical or behavioral diagnosis, do not meet the criteria for medical necessity and are not covered.
- Requests based solely on typical child behavior (e.g., curiosity without an underlying medical or behavioral diagnosis) do not meet the criteria for medical necessity and are not covered.
Prescribing Providers
Complex Rehabilitation Technology must be prescribed by a physician, physician assistant, nurse practitioner, occupational therapist, or physical therapist. The prescription must be within the scope of the prescribing provider's license.
Billing Providers
Only providers enrolled as a CRT supplier may bill for CRT codes. In order to qualify as a CRT supplier, providers must:
- Be accredited by a recognized accrediting organization as a supplier of CRT.
- Meet the supplier and quality standards established for DME suppliers under the Medicare or Health First Colorado program.
- Employ at least one (1) qualified CRT professional (ATP) for each location.
- Have CRT professionals present during member evaluation to:
- Assist in selecting the appropriate CRT items for such needs and capacities.
- Provide the member technology- related training in the proper use and maintenance of the selected CRT items.
- Directly involve with the assessment, and determination of the appropriate individually configured complex rehabilitation technology for the member, with such involvement to include seeing the member visually either in person or by any other real-time means within a reasonable time frame during the determination process.
- Maintain a reasonable supply of parts, adequate physical facilities, and qualified services or repair technicians to provide members with prompt service and repair of all CRT it sells or supplies.
- Provide the member written information at the time of sale as to how to access service and repair.
Existing Health First Colorado DME providers that want to enroll as a CRT Supplier, need to request a letter of intent to enroll as a CRT supplier. Suppliers with multiple Health First Colorado provider ID numbers need to submit a letter of intent for each provider ID number that will bill CRT for Health First Colorado.
Providers must retain record of the serial number for each approved repair item. The serial number must also be included on the CMS 1500 claim form in field 30 for all paper claims.
Pursuant to HB22-1290 Changes to Medicaid for Wheelchair Repairs, the department will no longer require prior authorization requests (PARs) for repairs of Complex Rehabilitative Technology (CRT) equipment. Effective July 1, 2022, claims related to the repair of CRT will not require a PAR when billed with modifier RB.
Enclosed/Safety Bed Coverage
Between May 1, 2022 and May 31, 2025, Questionnaire #19 is not required to be submitted with Prior Authorization Requests (PARs) for these items. Effective June 1, 2025, Questionnaire #19 will again be required for these items. HCPCS code E1399 is used to request and bill for these items.
Requests for these items will now consist of a single attestation within Keystone Peer Review Organization (Acentra’s) electronic system, Atrezzo. Providers will be asked to confirm that caregivers have been educated on safe and proper use of the bed.
Bed Rails
Bed rails are a covered benefit for hospital beds only and must be from the same manufacturer as the bed they will be installed on.
Vocational Items
Durable Medical Equipment is reviewed for medical necessity on an individual basis. Requests determined to be primarily for vocational purposes are not considered a medical benefit and will not be covered.
Hip Kits
Hip kits may be covered using procedure code E1399 and are therefore manually priced. When requesting a hip kit, pricing information should be submitted for a pre-packaged kit. Submitting invoices for individual items and referring to them as a kit will not be approved. If pricing is submitted for individual items, each item must be listed on the PAR with a separate HCPCS code for each. In these cases, medical necessity will also be determined for each item separately. When requesting a pre-packaged hip kit as one (1) item, medical necessity will be determined for the kit, only when it contains any combination of the following items:
- Reacher
- Leg lifter
- Sock aid
- Shoehorn
- Dressing stick
- Long scrub sponge
If a hip kit is requested and includes items not listed, they may be pended for additional justification.
Prosthetics and Orthotics (P&O)
The benefit includes, but is not limited to, items such as breast prostheses, braces, artificial limbs, implants, and orthopedic shoes for diabetic members. Some services require prior authorization.
Supplies
Disposable Supplies
Disposable supplies are a benefit of Health First Colorado for use by the member in his/her home. With the exception of gloves, the Home Health agency is responsible for providing all supplies necessary to meet the universal precaution requirement during a visit.
Beginning August 1, 2015, nasal atomizers (A4210) are a benefit when used in conjunction with the rescue medications Naloxone or Midazolam. Refer to Appendix P located on the Billing Manuals web page under the Appendices drop-down for coverage information on Naloxone and Midazolam.
Between April 1, 2022 and March 31, 2025, the following table should be used when billing for these products. Prior authorization is required for these HCPCS codes. Please be aware that different manufacturers may provide a different number of catheters with the system included in A4459. Providers should keep this in mind when determining how many units of A4453 are needed.
Beginning April 1, 2025, the information below should be used when billing for these products. A4459 no longer includes catheters. Prior authorization is required for these HCPCS codes.
- HCPCS A4459: Manual trans-anal irrigation system, includes water reservoir, pump, tubing, and accessories, without catheter, any type.
- HCPCS A4453: Rectal catheter with or without balloon, for use with any type transanal irrigation system, each.
Irrigation Supplies
As part of the 2022 new HCPCS procedure codes, A4397 has been discontinued and replaced by A4436 (reusable irrigation sleeve) and A4437 (disposable irrigation sleeve). A4437 has specific coverage criteria that providers will be asked to verify during the PAR process. At least one (1) of the following must be true for A4437 to be medically necessary:
- 1. Difficult pouching situations requiring better fit of disposable irrigation sleeve;
- Challenging abdominal contours, or
- Concerns with leakage / infection
- Type of pouching system individual uses when not irrigating is not compatible with reusable sleeves .
- Thick and pasty stool consistency is a clinical reason to use a disposable irrigation sleeve.
Enteral nutrition (EN) refers to medical formula/solutions when ordered by a physician, physician assistant, or nurse practitioner and provided according to standards of practice. The allowance for all items includes delivery to a member's residence. Equipment, supplies, and nutrients for enteral feeding or food supplements are a benefit when prior authorized.
Durable Medical Equipment providers should request that members participate in the Women, Infants and Children (WIC) program as a primary resource for medically necessary enteral nutrition products. Enteral nutrition products are a covered benefit when a member has been prescribed over the WIC limit and or WIC is unable to fulfill the prescription due to supply. Providers have the option of requesting a three (3) month PAR for members in the process of applying for WIC. After WIC determination is completed, provider may then submit a new PAR for one (1) year less one (1) day.
Questionnaire #10 for Oral and Enteral Nutrition Formula is not a required form as of 2018. However, it is still accepted as a form of documentation when signed by a physician. For accessibility, the questionnaire is located on the Provider Forms web page under the DMEPOS Forms drop-down. However, this form is optional and is still only acceptable when signed by a physician.
Human Milk Fortifier products are a covered benefit using HCPCS B4155. Effective June 1, 2025, these products can be provided with Health First Colorado as the primary payer instead of WIC. Providers are encouraged to referenced the Colorado specific guidelines for these products.
PARs and claims must identify the calculated number of units as specified in the HCPCS Code Table section of this billing manual. Nutritional supplements are not for replacement of conventional foods or for use as a convenience item.
Breast Pump Coverage
Effective for dates of service June 8, 2022, or later, DMEPOS providers may bill Health First Colorado as the primary payer for manual and or single user electric breastfeeding pumps.
Effective for dates of service on/after July 1, 2025, providers may supply a bundle of breast pump equipment that includes: one manual pump, one single-user electric pump and one set of replacement shields/flanges. This bundle is billed using HCPCS E0603 + modifier U1. All components of this bundle must be supplied for it to be correctly billed.
The Women, Infant and Children (WIC) program was previously the primary payer of breast pumps for Health First Colorado members. Health First Colorado only covered pumps under specific circumstances related to infant hospitalization of at least 54 days.
This limited coverage policy ended on June 7, 2022.
The WIC program has not changed. Members may acquire a breast pump from Health First Colorado or WIC.
- Prior authorization requests (PARs) are not required.
- Members may receive a breast pump as early as the 28th week of pregnancy. Per EPSDT policy, deliveries prior to 28 weeks qualify for a breast pump immediately following the birth.
- Postpartum members may receive a pump at any time.
- Breast pumps may be prescribed by a physician, physician assistant, nurse practitioner, or certified nurse midwife.
- As is required for all DMEPOS, a prescription from a physician, physician assistant, or nurse practitioner is needed.
- Claims will not be denied based on the diagnosis code used. However, diagnosis code Z39.1 is appropriate.
- The Colorado interChange has been updated to allow for these changes.
- Procedure code E0604 with modifier RR should be used when billing for multi-user breast pumps.
- Effective January 1, 2023, the reimbursement rate for E0604RR is $219.67. The interChange has been updated for the rate and code combination.
- This is a continuous rental item that will not be converted to purchase.
- Prior authorization requests are required.
- Prescriptions should include information on why a single user pump is not sufficient for the member.
- Multi-user pumps may be rented for up to two (2) years, but a PAR will need to be submitted for continuation of services after one (1) year.
- Providers are required to provide members with any necessary material and training on appropriate cleaning, storage, and use.
- A single user collection kit specifically made for the corresponding pump must also be provided to each user and is not to be billed separately.
- Additional accessories and supplies needed during the usage period, including replacement parts, are inclusive of the monthly rate and should not be billed separately.
- All rented pumps must be FDA approved as a multi-user breast pump.
- Single user breast pumps (electric and manual) remain a covered benefit, prior authorization requests not required.
- Members may receive a breast pump as early as the 28th week of pregnancy. Per EPSDT policy, deliveries prior to 28 weeks qualify for a breast pump immediately following the birth.
Lactation Support Services (HCPCS S9443) can be billed by Supplier, however a rendering provider ID is required on the claim. See the Lactation Support Services billing manual for details.
Donor Human Milk Coverage
Donor breast milk must be medically necessary and prescribed by an authorized prescriptive authority for use by an eligible member.
Eligible Providers
Only providers who are accredited by the Human Milk Banking Association of North America (HMBANA) may supply donated human breast milk. Accreditation from HMBANA must be included in the provider’s enrollment application and must be kept current. Providers may not supply or bill for donor milk if their accreditation is not current.
Billing
Use T2101 with modifier BO when billing for donor breast milk. A prior authorization request is required.
Only suppliers who have an active accreditation from HMBANA may bill T2101.
Home Intravenous (IV) Equipment
Home Intravenous (IV) equipment is a benefit for administration of Total Parenteral Nutrition (TPN), administration of antibiotics, maintenance of electrolyte balances, hydration, or other medications. The home IV therapy solutions and medications in this manual that are indicated as a home mix are a pharmacy benefit. The following HCPCS codes must be provided by a pharmacy per pharmacy billing requirements using a rebatable National Drug Code (NDC) number: B4164, B4168, B4172, B4176, B4178, B4180, B4189, B4193, B4197, B4199, B4216, B5000, B5100, and B5200. These codes are only reimbursed as a supply benefit for crossover claims when provided as an inpatient therapy for full benefit Medicare-Health First Colorado members.
Diabetic Supplies
Most diabetic supplies, such as glucose testing meters, test strips and other related supplies are a benefit with a prescription from a physician, physician assistant or nurse practitioner. Diabetic supplies are available for insulin, and non-insulin dependent members. Diabetic supplies must be billed as DMEPOS. Pharmacies billing supplies must follow Supply billing procedures and will not be reimbursed if billed as a pharmacy claim using NDC codes.
Continuous Glucose Monitor (CGM) Benefit Coverage
In addition to physicians, physician assistants, nurse practitioners and clinical pharmacists may order/prescribe CGMs.
For prior authorization requests on or after November 1, 2025, HCPF will align to Medicare’s Glucose Monitor policy. Medicare’s Glucose Monitor policy can be found CMS Medicare Coverage Database web page. For prior authorizations prior to November 1, 2025, see the Retired DMEPOS Policies section of this manual.
Per Senate Bill 24-168, members who have been diagnosed with Gestational Diabetes and are not being treated with insulin will also qualify for CGM coverage. Eligibility is only covered during the duration of the pregnancy.
CGM Prior Authorization Requests (PARs) must be submitted to the Department’s third-party utilization management vendor. PARs, including requests for CGM supplies, will be limited to a 6-month period.
When requesting a CGM in the online PAR portal, providers will be asked whether the member has received or if there is documented plan to receive diabetes education specifically related to CGMs.
Replacement and Upgrades
CGM replacement policy per 8.590.2.J. Repairs and replacement parts are covered under the following conditions:
The item was purchased by Medicaid; or
The item is owned by the member, member’s family or guardian; and
The item is used exclusively by the member; and
The item’s need for repair was not caused by member misuse or abuse; and
The item is no longer under the manufacturer warranty.
An upgrade to a new model or different brand of CGM may be deemed medically necessary in the following situations:
There is documentation that the current device is no longer functional either partially or entirely, and therefore is no longer clinically effective, or
The requested upgrade is different in its capability and would be expected to provide better clinical outcomes than the current device, and
The member has been using their current device for at least three (3) years.
If the current CGM requires repair or replacement that is no longer possible because it is obsolete, requests may be approved in cases where use is less than three (3) years. PARs may be pended to gather additional details regarding the device being obsolete.
All requests must meet the definition of medical necessity as stated in CCR 2505-10 8.076.8.
For requests to upgrade a CGM where the new device has the same manufacturer and procedure code as the current device, the upgrade request may be approved regardless of the devices condition, functionality and length of use. Cases will continue to be reviewed for medical necessity and may include ensuring compatibility of the new device with the member’s insulin pump.
Covered CGM Devices and National Drug Code (NDC) Crosswalk
| HCPCS | MODIFIER | NDC | Product Name | Product Category |
|---|---|---|---|---|
| Dexcom, Inc. | ||||
| A4239 | Blank* | 08627005303 | Dexcom G6 Sensor | Blood Glucose Sensor |
| A9277 | U1 | 08627001601 | Dexcom G6 Transmitter | Blood Glucose Transmitter |
| E2103 | U3 | 08627009111 | Dexcom G6 Receiver | Blood Glucose Receiver |
| A4239 | U3 | 08627007701 | Dexcom G7 Sensor | Blood Glucose Sensor |
| E2103 | U2 | 08627007801 | Dexcom G7 Receiver | Blood Glucose Receiver |
| Ascensia Diabetes Care | ||||
| A9276 | U1 | 17491002296 | Eversense E3 Sensor - HLDR | Glucose Sensor, Implant/Dexamet |
| A9277 | Blank* | 17491002292 | Eversense E3 Smart Transmitter | Blood Glucose Transmitter |
| Abbott Diabetes Care Sales Corp. | ||||
| A4239 | U2 | 57599000101 | FreeStyle Libre 14 Day Sensor | Flash Glucose Sensor |
| A4239 | U1 | 57599083500 | FreeStyle Libre 2 Plus Sensor | Blood Glucose Sensor |
| A4239 | U2 | 57599080000 | FreeStyle Libre 2 Sensor | Flash Glucose Sensor |
| E2103 | Blank* | 57599080300 | FreeStyle Libre 2 Reader | Blood Glucose Reader |
| A4239 | U2 | 57599081800 | FreeStyle Libre 3 Sensor | Blood Glucose Sensor |
| E2103 | Blank* | 57599082000 | FreeStyle Libre 3 Reader | Blood Glucose Reader |
| A4239 | U1 | 57599084400 | FreeStyle Libre 3 Sensor Plus | Blood Glucose Sensor |
| Medtronic Inc. | ||||
| A4238 | Blank* | 63000041338 | Guardian 4 Glucose Sensor | Blood Glucose Sensor |
| A4238 | Blank* | 63000051968 | Guardian 4 Glucose Sensor | Blood Glucose Sensor |
| A9277 | U2 | 63000044515 | Guardian 4 Transmitter Kit | Blood Glucose Transmitter |
| A9277 | U2 | 63000044516 | Guardian 4 Transmitter Kit | Blood Glucose Transmitter |
| A9277 | U2 | 43169095568 | Guardian Link 3 Transmitter | Blood Glucose Transmitter |
| A9277 | U2 | 63000031699 | Guardian Link 3 Transmitter | Blood Glucose Transmitter |
| A4238 | Blank* | 43169070405 | Guardian Sensor 3 | Blood Glucose Sensor |
| A4238 | Blank* | 63000017962 | Guardian Sensor 3 | Blood Glucose Sensor |
| A4238 | Blank* | 63000033698 | Guardian Sensor 3 | Blood Glucose Sensor |
| A4238 | Blank* | 63000035844 | Guardian Sensor 3 | Blood Glucose Sensor |
| A4238 | U1 | 63000095638 | Simplera Sync Sensor | Blood Glucose Sensor |
| A4238 | U1 | 63000095640 | Simplera Sync Sensor | Blood Glucose Sensor |
| A9276 | Blank* | 63000056502 | Simplera Sensor, 5 pack | Blood Glucose Sensor |
| A9276 | Blank* | 63000056504 | Simplera Sensor, 5 pack | Blood Glucose Sensor |
| A9276 | Blank* | 63000082957 | Simplera Sensor, 5 pack | Blood Glucose Sensor |
| A9276 | Blank* | 63000082965 | Simplera Sensor, 5 pack | Blood Glucose Sensor |
| A9276 | U2 | 57599088000 | Minimed Instinct Sensor | Blood Glucose Sensor |
*In the modifier column, the term “Blank” indicates that no modifier should be submitted with the procedure code and NDC combination. Claims will deny if the proper HCPCS, Modifier, and NDC combination is not submitted as listed above.
The Preferred Diabetic Supply List (PDSL) can be found on the Pharmacy Resource web page.
CGM Products with No NDC
CGM products that do not have an NDC or Wholesale Acquisition Cost (WAC) must be submitted as a professional claim and will require Questionnaire 20 to be submitted with the prior authorization request (PAR) and to the claim. Questionnaire 20 can be found on the Provider Forms web page. Claims must be submitted with an invoice or manufacturer’s suggested retail price (MSRP) attached.
Medtronic CGM products that do not have an NDC may use E2102 or E2103 for prior authorization requests and billing purposes.
Procedure code A9274 with modifier U1 is a covered service and requires prior authorization for Omnipod® 5 and DASH® products. This code and modifier combination is manually priced. Claims must be submitted via the Provider Web Portal with an invoice or manufacturer’s suggested retail price (MSRP) attached and the appropriate modifier for pricing.
Incontinence Products or Briefs
The prescribing practitioner's prescription must include incontinence as a condition of a primary or secondary diagnosis in order for the member to qualify for reimbursement by Health First Colorado. Diapers or briefs for children under four (4) years old are an expected childhood expense and are not a Health First Colorado benefit.
COMBINATION LIMIT: Products are limited to 360 per calendar month in any combination of diapers, liners, and undergarments. Medically necessary usage above that amount requires prior authorization.
Medically necessary wipes are a benefit under EPSDT, wipes for incontinence only are not medically necessary. Wipes for use by a Home Health provider are not a benefit. Prior Authorization Requests are not required. Effective July 1, 2021, providers must use HCPCS A9286 for this benefit.
A4520 Incontinence garment, any type, (e.g. brief, diaper) each
The code A4520 is not an open code. If the PDAC has assigned an incontinence product the code A4520, the claim (and PAR if required) should use the most appropriate T-code listed in the HCPCS Code Table section within this manual.
Nerivio Coverage
The Nerivio product (HCPCS A4540)is used for treating migraines and is covered under the following medical necessity criteria.
Nerivio may be approved if member has:
- Trialed and failed adequate trials in terms of duration and dose of all preferred treatments for acute and preventative migraine treatment per current Preferred Drug List (PDL)
- Trial failure is defined as lack of efficacy, allergy, intolerable side effects, contraindication to therapy or significant drug-drug interaction
- Submission must include documentation of the specifics (medication, dosage, duration, effects, and/or contraindication) of these trials
AND
- Behavioral and lifestyle recommendations from the American Headache Society have been unsuccessful
- Submission must include documentation of the specific interventions, similar to the above as applicable.
AND
- Other headache types/contributions have been addressed (with, at minimum, a documented discussion of the plan/interventions implemented to ameliorate the issues).
For reference, here is a list of some acute and preventive categories of pharmaceutical migraine treatments:
- Angiotensin II receptor blockers/angiotensin converting enzyme inhibitors
- Antiemetics
- Anticonvulsants
- Anti-depressants/non-opioid analgesia
- Beta blockers
- Botulism Toxin
- Calcium channel blockers
- Calcitonin gene related peptide inhibitors
- Cyproheptadine (pediatric)
- Ditans
- Ergots
- Methylxanthines
- Non-steroidal anti-inflammatories
- Nutraceuticals
- Triptans
Heparin Flushes
All Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) providers are reminded that Healthcare Common Procedure Coding System (HCPCS) J1642 is billed per 10 United States Pharmacopeia (USP) units of heparin and is billed by potency, not volume. Below is an example of how HCPCS J1642 should be calculated.
Product example:
Description: Heparin Lock 500 UN- 5 milliliters (mL) syringe (NDC 64253-0333-35) Concentration: 100 units/mL (500 units divided by 5 mL)
Total units per syringe: 500 USP
Billing calculation:
Total units per syringe: 500 USP
Billing units: 500 (total units/syringe) divided by 10 = 50 units billed
Special Considerations
Rental
There may be a financial cap on rental items. If the total cost for rental of an item reaches the cost of purchase, the item will be converted to a purchase unless otherwise specified. Rental amounts in excess of purchase amounts are subject to recovery.
Modifier RR (rental) or KR (partial month rental) should be on all PARs (if required) and claims. One (1) unit of a code with the RR modifier is the equivalent of a one (1)-month rental. One (1) unit of a code with the KR modifier is the equivalent of a one (1)-day rental.
- In some cases, as indicated in the HCPCS Code Table section, RR billed with multiple units and a date span is used to represent a daily rental. The number of days in the date span should equal the number of units for that line item.
Accessories, supplies, maintenance, and repairs are inclusive in the reimbursement of rented equipment, unless otherwise specified.
For ventilator equipment that is considered a continuous rental, accessories and supplies may be billed separately. Continuous rental items (i.e., ventilators) do not require the KH (1st month rental) modifier. Additionally, if a member qualifies to have a back-up ventilator, two (2) units may be billed per month, otherwise, only one (1) unit is allowable.
Continuous rental items require a Face-to-Face visit for both initial requests and renewals. Refer to the Face-To-Face (F2F) Requirements section in this manual.
Related Medical Supplies
Supplies accompanying DME that has been prescribed and is owned by and currently being used by the member are covered.
Used and Refurbished DME and P&O
Supply providers have the option to request used and/or refurbished DME and P&O. Equipment may be donated, passed down from a sibling, or purchased from a DMEPOS provider post refurbishment. Used equipment also includes equipment that has not been previously rented or sold (e.g., equipment used for trial periods or as a demonstrator). All used and refurbished equipment requires a PAR.
The DMEPOS provider must guarantee that the equipment provided to the member is in "like new" condition, and that any modifications are made prior to the delivery of the equipment. The cost of repairs or modifications must not exceed the cost of replacement equipment. The provider will maintain a one (1) year limited warranty that covers all necessary parts or repairs. Comparison pricing for new equipment must be included in the PAR documentation. PAR documentation must include the make, model, and serial number of equipment. The Used Equipment (UE) modifier must be included on all used and refurbished equipment PARs and claims.
Examples of allowable used or refurbished equipment include but are not limited to:
- Manual Wheelchairs
- Power Operated Vehicles (Scooters)
- Power Wheelchairs
- Hospital Beds (Frame only, new mattress must be purchased)
- Lifts
- Speech Generating Devices
If new equipment is rented to and subsequently purchased by the same member, it would not be considered used. Supplies (disposable items) may not be provided as used.
Unless a part of the Upper Payment Limit (UPL), the maximum allowable for used/refurbished equipment is 60% of the equipment's maximum allowable for purchase. Refer to the Federal Upper Payment Limit (UPL) Requirement section in this manual.
Dates of Service after the Death of a Health First Colorado Member
Health First Colorado will reimburse supply providers for durable medical rental equipment, oxygen, and bulk supplies that are drop-shipped to the member's home for services rendered during the month of the member's death, only if the claim’s date of service is before the member’s date of death. Health First Colorado will make recoveries for all DMEPOS services following the date of the member's death.
The interChange operationalizes this policy in the following ways:
- If the claim's 'date of service' occurs before the member's 'date of death' within the same month, the claim will be paid and not recouped.
- If the claim's 'date of service' occurs on/after the member's 'date of death' within the same month, and for all following months, the claim will be denied or eventually recouped.
Span Billing for Certain Supplies
The following items may have a date span of up to 30 calendar days on claims submitted to the Department:
- Diabetic testing supplies (i.e., test strips, lancets)
- Continuous passive motion devices (CPM)
- Parenteral and enteral nutrition
- Parenteral and enteral administration kits
- External infusion pump supplies
- Over the Counter, at-home COVID-19 tests
- Trans-anal irrigation products (HCPCS A4453)
- Other supplies that have an NCCI MUE limit (refer to the January 2024 Provider Bulletin (2400503) located on the Bulletins web page)
Suppliers must span the dates of service using "From" and "To" dates on any claim for the items listed above. The "From" date is when the items were provided to the member. The "To" date is the last date the supplies are expected to be used. For example, if you are providing a 30-day supply of diabetic testing strips to a member, the "From" date on the claim would be "01/01/2021" and the "To" date would be "01/30/2021”.
Shipped Supplies
Suppliers may not automatically dispense a quantity of supplies on a predetermined regular basis. Members must be contacted prior to shipping to ensure that member information is correct, there have been no changes to the prescription, and supplies/additional supplies are needed. Member contact consists of either a request from the member/caregiver that supplies are needed or a member/caregiver's response to an inquiry by the DMEPOS Provider that supplies are needed. Members may not be charged for costs associated with shipping and handling.
Providers must use the date the supply was delivered to the member as the From Date on claim submissions for shipped supplies.
Face-To-Face (F2F) Requirements
A face-to-face (F2F) encounter is a federally required visit in which members must meet with a physician, or other allowed practitioner, within six (6) months prior to the date the member receives the equipment.
The F2F encounter documentation must demonstrate that the prescriber met F2F with the member specifically related to the member's primary clinical need for the prescribed DME item.
The F2F must be conducted and documented by the following allowed practitioners:
- Physician
- Physician Assistant
- Nurse Practitioner
- Occupational Therapist (effective 8/06/2025)
- Physical Therapist (effective, 8/06/2024)
- Pharmacist (effective 5/28/2025) or
- Clinical Nurse Specialist
Non-physicians (listed above) that perform a F2F, must communicate their clinical findings of that F2F encounter to the physician responsible for prescribing the related DME. These, and all F2F clinical findings, must be incorporated into a written or electronic document included and maintained in the member's medical record.
The F2F requirement does not apply to all DME but is required for those codes that Medicare has published as requiring a F2F encounter.
To date, Medicare has chosen to not enforce their F2F requirements. As a result, the F2F code list has not been updated since 2016.
The F2F encounter must happen within six (6) months prior to the start of services and must be performed by the prescribing physician or other allowed practitioner.
As defined in 10 CCR 2505-10, § 8.590.1 the start of services means the date that the ordering practitioner signs the written order for durable medical equipment following the face-to-face encounter with the member.
A F2F is only required for the initiation of the DME. The provision of the prescribed DME item does not require multiple F2F encounters for each related item, only documentation that the F2F occurred and is related to the main reason the DME item is needed.
For items that are continuous rental, F2F within six (6) months is a requirement on both initial requests as well as renewals.
Repair and replacement do not require the F2F.
The F2F encounter must be documented to include the following:
- the primary reason the member requires the prescribed DME, and
- the F2F encounter was related to the primary reason the member requires the prescribed DME, and
- the signature allowed practitioner who performed the F2F encounter,
- the date of the F2F encounter,
- that the F2F encounter occurred within six (6) months.
The member's medical need for the DME item should be clearly communicated in the F2F documentation. This will aid manufacturers in supplying the DME item without sending the member back multiple times for unnecessary F2F encounters.
Note: The prescriber's responsibility, concerning a F2F encounter, is to meet with the member and document the member's medical need for an item of DME, not to detail every DME item the member might need.
F2F encounters may be performed via telehealth if available.
Pricing
There are three (3) ways to determine the maximum allowable for DMEPOS: the fee schedule, the Manufacturer's Suggested Retail Price (MSRP), and By Invoice.
Percentages noted below can be found in 10 CCR 2505-10, Section 8.590.7 of the Health First Colorado rules.
Usual and Customary Charge (U&C): What a provider would charge the general public for the product/service.
The Submitted Charge on a claim, regardless of how the maximum allowable is determined, should always be a provider's U&C.
Fee Schedule
For fee schedule items, reimbursement is the lower of the U&C or the fee schedule rate. No additional handling, shipping or tax charges may be billed.
Refer to the fee schedule located on the Provider Rates and Fee Schedule web page for the majority of the DMEPOS codes.
Federal Upper Payment Limit (UPL) Requirement
As of January 1, 2018, Health First Colorado is required to comply with the Consolidated Appropriations Act of 2016 (Section 503) which means Health First Colorado cannot pay more than what Medicare would have paid in the aggregate for certain DME services. The original effective date was January 1, 2019, but the Cures Act (Section 5002) changed the effective date to January 1, 2018.
- Compliance is measured by Health First Colorado's aggregate expenditure on a per calendar year basis.
- If the code was NOT billed/paid by both Medicare and Health First Colorado during the prior calendar year, it is NOT included.
- Only DME codes beginning with A, E and K are included.
- Orthotics, prosthetics, and disposable supply codes are not included.
- Medicare's competitive bid codes that are in line with points two (2) and three (3) are included.
- Oxygen and oxygen systems are included.
Codes that fall within the scope of the UPL are indicated in the HCPCS Code Table in the Comments column with the following notation:
*Code is subject to the 2019 DME UPL
Refer to the fee schedule located on the Rates and Fee Schedules web page under the Durable Medical Equipment, Upper Payment Limit section for the DME UPL codes.
Manufacturer Suggested Retail Price (MSRP)
For dates of service between July 1, 2024 and June 30, 2025, if the fee schedule states, "Code is Manually Priced", reimbursement is the lower of (MSRP less 13.78%) or the provider's U&C.
For dates of service between July 1, 2025 and September 30, 2025, if the fee schedule states, "Code is Manually Priced", reimbursement is the lower of (MSRP less 13.56%) or the provider's U&C.
For dates of service beginning on October 1, 2025, if the fee schedule states, “Code is Manually Priced”, reimbursement is the lower of (MSRP less 13.78%) or the provider’s U&C.
- The provider must keep a copy of the item's invoice and documented MSRP.
- The documented MSRP must include the name of the provider's employee that received and documented the MSRP, and the date the MSRP was received.
- Providers may not submit for reimbursement for either state sales tax collection or shipping costs.
- Providers must add the 'SC' modifier when using the MSRP for pricing.
- Providers must attach a copy of the MSRP on all PARs and claims.
- Providers may manually indicate on the MSRP documentation the actual quantity supplied to the member if it differs from claim total.
- Providers may not use MSRP pricing for procedure code A9901.
By Invoice
For dates of service between July 1, 2024 and June 20, 2025, if the fee schedule states, "Code is Manually Priced" and the product has no MSRP, reimbursement is the lower of the Actual Acquisition Cost plus 24.06% or the provider's U&C.
For dates of service between July 1, 2025 and September 30, 2025, if the fee schedule states, "Code is Manually Priced" and the product has no MSRP, reimbursement is the lower of the Actual Acquisition Cost plus 24.45% or the provider's U&C.
For dates of service beginning on October 1, 2025, if the fee schedule states, “Code is Manually Priced” and the product has no MSRP, reimbursement is the lower of the Actual Acquisition Cost plus 24.06% or the provider’s U&C.
Actual Acquisition Costs are defined as the manufacturer's list price for the item less any standard trade discount applied to lower the actual cost to the provider but excluding any time sensitive or otherwise conditional discounts available to the provider. The provider must keep a copy of the item's invoice.
Misrepresentation of Actual Acquisition Costs could result in State or Federal, civil or criminal sanctions.
In order to receive the maximum allowable reimbursement for By Invoice items, one (1) unit of procedure code with the 'UB' modifier must be included on the claim. The Submitted Charge should reflect the provider's U&C minus the Actual Acquisition Cost.
Effective July 1, 2018, A9901 will no longer be used for Manual Pricing by invoice. The percentage above the invoice cost will be calculated in line with the base code, similar to how MSRP works.
Providers must attach a copy of the invoice on all PARs and claims.
Line items that are reimbursed by invoice must:
- Include the 'UB' modifier, and
- The Submitted Charge must match the amount on the invoice (excluding A9901).
Effective July 1, 2024, maximum allowable is:
- E1399 UB: $1229.00 (actual invoice cost + 24.06%)
The Submitted Charge should reflect the provider's U&C.
The math for calculating the maximum allowable must be shown. It may be added to the invoice or a separate attachment. Using the above example:
- $1000 x 1.2406 = $1240.60, or
- $1000 x .2406 = $240.60 + $1000 = $1240.60
- If the full quantity on the invoice was not provided to the member (i.e. a bulk order) a breakdown of the cost per unit multiplied by the quantity provided must be shown. In the instance where a manufacturer puts the cost per unit on their invoice, the per unit price calculation does not need to be shown. However, the unit price does need to be multiplied by the quantity provided.
After verifying the calculation, claims processors will price the claim at the lower of U&C or the actual invoice cost plus the percentage.
Maximum Allowable for Rental
Fee schedule: With the exception of oxygen and items noted as continuous rental, rental reimbursement caps at the item's purchase price.
MSRP or By Invoice Pricing: Fee schedule items that require manual pricing for rental, excluding oxygen, are reimbursed using the MSRP or Invoice methodology, divided by 10, for one (1) month of rental. If for a partial month rental, divide again by 30 for the daily maximum allowable. Total rental reimbursement cannot exceed the maximum allowable purchase price.
Rebates
If a rebate is available, the provider must reflect U&C minus the rebate received or anticipated from the manufacturer.
Prior Authorization Requests (PARs)
Some supply items and most DME items require prior authorization. A member may be required to receive an occupational therapy evaluation to determine appropriateness of prescribed equipment such as motorized chairs. This manual contains a detailed list of prior authorization requirements as well as the correct form and mailing address for each PAR.
Prior Authorization Requests must be submitted and approved before services are rendered. The service must be rendered by the identified supplier on the approved PAR. Services rendered must match the approved services exactly.
Approval of a PAR does not guarantee Health First Colorado payment and does not serve as a timely filing waiver. Prior authorization only assures that the approved service is a medical necessity and is considered a benefit of Health First Colorado. In reviewing for medical necessity, the Utilization Management Vendor may deny an item that has been deemed unsafe for the member. All claims, including those for prior authorized services, must meet eligibility and claim submission requirements (e.g., timely filing, detailed provider information, detailed description of medical necessity, all required attachments included, etc.) before payment can be made.
PAR Submission
All PARs must be submitted by the supply provider that intends to submit the claim for the service and have an attached prescription from the prescribing authority and any other required documentation. Each PAR must include the name and phone number of the member's Primary Care Physician (if applicable). PAR requests for members with a non-Health First Colorado primary care physician must include the primary care provider's National Provider Identifier (NPI), contact information and note in the "comment" section stating that the referring provider is not a Health First Colorado provider and prescriptive authority has been verified. Providers shall not charge a member for items covered as a Health First Colorado benefit. This includes but is not limited to blood pressure monitors, blood glucose monitors, walkers, canes, nutritional supplements, and incontinence products.
Prior Authorization Request dates typically have a date span for one (1) year less one (1) day. Exceptions for decreased span dates less than one (1) year are allowed in certain circumstances such as short-term rental or WIC application period. Dates must not exceed one (1) year and must match the dates on individual line items, or the PAR will be denied.
All PARs and revisions processed by the ColoradoPAR Program must be submitted through the PAR portal. Prior Authorization Requests submitted via fax or mail will not be processed by the ColoradoPAR Program and subsequently not reviewed for medical necessity. These PARs will be returned to providers via mail.
This requirement only impacts PARs submitted to the ColoradoPAR Program.
The electronic PAR format will be required unless an exception is granted by the ColoradoPAR Program. Exceptions may be granted for providers who submit five (5) or less PARs per month. To request an exception, more information on electronic submission, or any other questions regarding PARs submitted to the ColoradoPAR Program, contact the ColoradoPAR Program at 888-801-9355 or visit the Department's ColoradoPAR Program web page.
PAR Review and Notification
The actual number of units approved for any item may be reduced or increased by the reviewer evaluating the PAR.
Once review is complete, the status of a PAR (approved, partially approved or denied) is available through the Health First Colorado Secure Web Portal (Provider Web Portal). In addition, both the provider and the member receive a letter indicating whether or not the services were authorized. The letter will include a PAR number that must be included on the claim.
DME Safety Equipment Policy
As part of the Prior Authorization Request (PAR) process, Health First Colorado’s PAR vendor reviews requests for safety of the member. It is the member’s responsibility to ensure safe installation of any safety equipment that modifies the home and or their environment. This would refer to items such as rails that attach to a wall, toilet, or other part of the home. The department refers to these items as permanently affixed safety equipment. Due to substantial risk of safety for the member, the department will not approve of safety items that are not permanently affixed. This includes but is not limited to items attached by means of a suction cup or tension mechanism.
However, PARs are still reviewed for safety on an individual basis and this policy should not be used to assume that all permanently affixed items are safe for every member.
- DME most commonly impacted by this policy:
- E0241 Bathtub wall rail, each
- E0242 Bathtub rail, floor base, each
- E0243 Toilet rail, each
- E0246 Transfer tub rail attachment, each
Submitting Claims after PAR Approval
Providers must receive an approval for all items/services that require a prior authorization before submitting a claim.
Once prior authorization is received, claims should only include the approved PAR number and, if applicable, the serial number of the approved equipment. In most cases, it is not necessary to submit a copy of the approved PAR. Providers will be notified if a copy of the approved PAR is needed.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
8.280.4.E Other EPSDT Benefits
Other health care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Section 1905(a) of the Social Security Act are a covered benefit under EPSDT when medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, regardless of whether such goods and services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a good or service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one (1) or more Activities of Daily Living; and meets the criteria set forth at Section 8.076.1.8.b - g.
- The service provides a safe environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly.
Questionnaires
Visit the Provider Forms web page under the DMEPOS Forms drop-down for all questionnaires.
Complex Rehabilitation Technology (CRT)
Complex Rehabilitation Technology Suppliers must comply with additional regulations for repair orders created on or after October 1, 2023. Pursuant to 10 C.C.R. 2505-10 8.590.5.E. the following required metrics are to be reported by suppliers on all CRT repairs, including members also enrolled in Medicare coverage. Members with additional coverage other than Medicare, such as private insurance, are excluded from these reports.
- Quality of CRT repairs shall be reported to the Department using the data points 2: a-i detailed below.
- At the time the repair is fulfilled, regardless of the location, members will be asked to confirm that the equipment has been repaired to their satisfaction.
- Members, their legal guardian or other authorized representative may be asked to confirm verbally or in writing, provided that the answers can be verified by a signature and date.
- This information may be obtained on a delivery ticket or as a separate form. This metric will be used to measure the number of repairs that were reported as satisfactory, not satisfactory or where an answer was not obtained.
- Metrics must be reported using the following:
- Medicaid Identification Number
- Type of equipment being repaired: Manual wheelchair, power wheelchair, non-wheelchair mobility device or other equipment
- Does the member also have Medicare? Yes or no
- Order creation date
- Date of first available evaluation appointment (optional)
- Date evaluation occurred
- Does the member have secondary/back up equipment? Yes or no
- Quality of repair answer: Satisfactory, not satisfactory or answer not obtained
- Repair fulfillment date
CRT Suppliers must send their reports to HCPF_DME@state.co.us twice per calendar year following this deadline table:
| Date of Repair Fulfillment | Report Submission Deadline |
|---|---|
| December 1 – May 31 | June 30 |
| June 1 – November 30 | December 31 |
There are two (2) levels of documentation requirements associated with PARs for CRT:
- Basic Documentation
- This level of documentation does not require a specialty evaluation. Basic documentation requirements apply to all CRT wheelchairs and wheelchair-related items that require a PAR. The basic documentation should include at a minimum the following information:
- Member's name, date of birth, residence address, height and weight, and all relevant medical diagnoses.
- A summary of the member's current medical condition, prognosis, previous and current treatments that are pertinent to the requested item.
- Length of anticipated need for the requested item.
- A brief description of the member's impairment in functional mobility that establishes that they have a mobility limitation and the item is needed for a medical purpose.
- If the recommended item is not the least costly option available to meet the member's medical need, documentation must contain a brief description of the impairments in body functions or structures that rule out use of the less costly item to justify the need for the recommended item.
- A description of how the member will operate the device (e.g., self-propel, tiller, joystick, etc.). Include a statement summarizing the member's mental and physical abilities/limitations as they pertain to member's ability to operate the recommended equipment appropriately for the duration of recommended use and in the environments in which it will routinely be used.
- If applicable, a brief description of the member's seating and positioning needs, and how these will be adequately met by the recommended device.
- If applicable, a brief description of where the equipment is to be used (example home, school, place of work, neighborhood, rural, city, train, etc.), including the accessibility of member's residence or non-institutional setting. Include if the equipment will be transported in a vehicle and how, as well as the capability of the member or caregiver to properly operate the equipment in these environments.
- A brief description of any anticipated changes in the member's physical size, medical or functional status which may require modifications to the equipment, and how the equipment will accommodate the member's needs over time. The recommended equipment should be capable of modification to meet the needs for anticipated improvement or deterioration of functional mobility when possible.
- Detailed description of all manually priced items that are requested including manufacturer's retail pricing or invoice information with itemized pricing, including the description of the specific base, any attached seating system components, and any attached accessories.
- All basic documentation paperwork (except for repair and replacement) requires the signature of the ordering provider, indicating that he or she agrees with the recommendation, and has evaluated the member within the past 12 months of signing and dating the required paperwork.
Specialty Evaluation Documentation
*This section represents an overview of the specialty evaluation requirement and is not intended to limit or restrict access to Specialty Evals.
This level of documentation provides further details in order to establish medical necessity. A specialty evaluation is an assessment performed by a licensed/certified medical professional (such as a Physical Therapist, Occupational Therapist, or physician) who has no financial relationship with the DME supplier and who has specific training and experience in complex rehab technology wheelchair evaluations. The evaluation includes the physical and functional evaluation, treatment plan, goal setting, preliminary device feature determination, trials/simulations, fittings, function related training, determination of outcomes, and related follow-up. This evaluation is performed in conjunction with an equipment supplier who is a Rehabilitation Engineering and Assistive Technology Society of North America (RESNA)-certified Assistive Technology Professional (ATP), and who assists with the home environment accessibility survey, system configuration, fitting, adjustments, programming, and product related follow up.
Specialty evaluation is required for:
- A new CRT wheelchair or a replacement CRT wheelchair after the 5th year mark for adults and 3rd year mark for children.
- A new custom contoured seating system or modification.
- Modification to a seating system
- An addition of power seating or alternative drive control to a wheelchair.
- Date(s) of specialty evaluation
- The name and signature of licensed/certified medical professional completing the evaluation and assessment
- A statement attesting that the person performing the assessment has no financial relationship with the DME provider should be included.
- A brief description of the specialty evaluation process that was completed, which includes a summary of the pertinent assessment findings/outcomes in the following assessment areas that apply:
- Functional mobility, including transfers
- Sitting balance/postural alignment
- Existence and severity of postural asymmetries
- Sensory function, if impaired
- Neuromusculoskeletal function (movement, muscle tone, coordination)
- Mat exam (joint range of motion, deformities, orthopedic impairment), addressing the existence and severity of orthopedic deformities
- Equipment trials/simulations
- A description of the member's current mobility and/or seating equipment, how long the member has been using the current equipment and why it no longer meets the member's needs.
- Information on any recent changes in the member's physical or functional status, and any expected or potential surgeries that will improve or further limit mobility.
- If applicable, information regarding the member's seating and positioning needs and the specific seating equipment and accessories required to meet those needs.
- A summary of the type of mobility equipment that will best meet the member's medical and functional needs and an explanation of the basic and/or instrumental ADLs that will be possible with this equipment that would not be possible with a lower level or lower cost item.
- If applicable, documentation that supports why a tilt seat function is necessary to meet the member's medical and/or functional needs.
- If a member has a progressive disability, the documentation must indicate how the item will accommodate the member's needs over time. If a member is expected to grow, the wheelchair must have a growth potential.
- All specialty evaluation paperwork requires the signature of the ordering physician, indicating that he or she agrees with the recommendation and has evaluated the member within the past 12 months of signing and dating the required paperwork.
- Items that require a specialty evaluation must include both the basic and specialty evaluation documentation. Documentation for specialty evaluation should include the following information in addition to the basic documentation requirements previously listed:
Note: Specialty evaluation is not required for CRT repair and replacement.
Return of Incorrect Equipment
Per 10 CCR 2505-10 8.590.4.H, providers must pick up incorrect or inappropriate items that have been supplied to the member within five (5) business days of notification. Providers may not bill for those items and must submit a credit adjustment with 20 business days if the claim was previously submitted.
Record Keeping
Supply providers must maintain the records described below for all items provided to member. Supply providers must keep the information for seven (7) years, and provide a copy of any documentation to the Department and member or his/her representative upon request.
- Prescribing practitioner's prescription(s),
- Approved prior authorization requests,
- Additional documentation received from physicians or other licensed practitioners,
- Documentation that the member or caregiver has been provided with the following:
- Manufacturer's instructions,
- Warranty information,
- Registration documents,
- Service manual, and
- Operating guides.
- Documentation on all reimbursed equipment, which shall include:
- Manufacturer's name and address,
- Date acquired,
- Acquisition cost,
- Model number,
- Serial number, and
- Accessories, attachments or special features included in the item.
- Verification that equipment requiring repairs belongs to the presenting member.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Using Modifiers
Modifiers are used with HCPCS codes to describe circumstances that may change or alter payment or provide additional information. Refer to the approved modifiers for use with DME procedure codes in field locator 19c in the Paper Claim Reference Table section.
The following modifiers are approved for use with DME procedure codes and must be used when applicable:
| AV | Item furnished in conjunction with a prosthetic device, prosthetic or orthotic |
| BO | Orally administered nutrition, not by feeding tube |
| KH | DMEPOS item, initial claim, purchase or first month rental |
| KI | DMEPOS item, second or third month rental. |
| KR | Rental item, billing for partial month |
| MS | Six (6) month maintenance and servicing fee for reasonable and necessary parts and labor which are not covered under any manufacturer or supplier warranty |
| RR | Rental (use the RR modifier when DME is to be rented) |
| SC | Medically Necessary Service or Supply - To be used with MSRP priced codes only |
| TT | Individualized service provided to more than one (1) member in same setting |
| TW | Secondary or back-up equipment |
| UB | Invoice cost - To be used with "By Invoice" priced codes only |
| NU | New Equipment |
| UE | Used Equipment |
| Effective July 1, 2017 | |
| RA | Replacement of a DME, orthotic or prosthetic item |
| RB | Replacement of part of a DME, orthotic or prosthetic item furnished as part of a repair |
| Effective June 1, 2018: | |
| KF | Item designated by the FDA as a Class III device |
Procedure/HCPCS Codes Overview
The Department develops procedure codes that are approved by the Centers for Medicare & Medicaid Services (CMS). The codes are used for submitting claims for services provided to Health First Colorado members and represent services that may be provided by enrolled certified Health First Colorado providers.
The Healthcare Common Procedural Coding System (HCPCS) is divided into two (2) principal subsystems, referred to as level I and level II of the HCPCS. Level I of the HCPCS is comprised of CPT (Current Procedural Terminology), a numeric coding system maintained by the American Medical Association (AMA).
The CPT is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other health care professionals. Level II of the HCPCS is a standardized coding system that is used primarily to identify products, supplies, and services not included in the CPT codes, such as ambulance services, durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) when used outside a physician's office. Level II codes are also referred to as alphanumeric codes because they consist of a single alphabetical letter followed by four (4) numeric digits, while CPT codes are identified using five (5) numeric digits.
National Correct Coding Initiative
Note that Medically Unlikely Edits (MUEs) may apply for some codes. Visit the National Correct Coding Initiative (NCCI) web page.
Paper PAR Instructional Reference
| Field Label | Completion Format | Instructions |
|---|---|---|
| The upper margin of the PAR form must be left blank. This area is for authorizing agency use only. | ||
| Invoice/Pat Account Number | Text | Optional Enter up to 12 characters (numbers, letters, hyphens) that help the provider identify the claim or member. |
| 1. Member Name | Text | Required Enter the member's last name, first name, and middle initial exactly as it appears on the eligibility verification. Example: Adams, Mary A. |
| 2. Member Identification Number | 7 characters | Required This number consists of a letter prefix followed by six (6) numbers. Example: A123456 |
| 3. Sex | Check box MF | Required Enter an "X" in the appropriate box. |
| 4. Date of Birth | 6 digits | Required Enter the member's birth date using a MMDDYY format. Example: January 1, 2025 = 010125 |
| 5. Member Address | Characters: numbers and letters | Required Enter the member's full address: Street, city, state, and zip code. |
| 6. Member Telephone Number | Text | Optional Enter the member's telephone number. |
| 7. Prior Authorization Number | None | Leave Blank This field is automatically system assigned |
| 8. Dates Covered by This Request | 6 digits for From date and 6 digits for Through date | Optional Enter the date(s) within which service(s) will be provided. If left blank, dates are entered by the authorizing agent. Authorized services must be provided within these dates. Use the MMDDYY format. Example: January 1, 2025 - January 31, 2025 = From 010125 Through 013125 |
| 9. Does Member Reside in a Nursing Facility? | Check Box Yes/No | Required Check the appropriate box. |
| 10.Group Home Name if Member Resides in a Group Home | Text | Conditional Complete if member resides in a group home. Enter the name of the group home or residence. |
| 11.Diagnosis | Text | Required Enter the diagnosis code and sufficient relevant diagnostic information to justify the request. Include the prognosis. Provide relevant clinical information, other drugs or alternative therapies tried in treating the condition, results of tests, etc., to justify a Health First Colorado determination of medical necessity. Approval of the PAR is based on documented medical necessity. Attach documents as required. |
| 12.Requesting Authorization for Repairs | Text | Conditional Complete if requesting repairs for equipment owned by the member. Enter the serial number of the equipment. |
| 13.Indicate Length of Necessity | Text | Conditional Complete if renting equipment. Provide best estimate of how long equipment will be needed. |
| 14.Estimated Cost of Equipment | Digits | Conditional Complete if purchasing, replacing, or repairing equipment. Provide best estimate of cost for labor and replacement part(s) for repair or cost for purchases. |
| 15.Services To Be Authorized | None | Preprinted Do not alter preprinted lines. No more than five (5) items can be requested on one (1) form. |
| 16.Describe Procedure, Supply, or Drug to be Provided | Text | Required Enter the description of the service/procedure to be provided. Include model number for DME purchase or serial number for repair. |
| 17.Procedure, Supply or Drug Code | 5 digits | Required Enter the appropriate HCPCS code for each item that will be billed on the claim form. The authorizing agent may change any code. The approved code(s) on the PAR form must be used on the claim form. |
| 18.Number of Services | Digits | Required Enter the number of units for supplies, services or equipment requested. If this field is blank, the authorizing agent will complete with one (1) unit. |
| 19.Authorized No. of Services | None | Leave Blank The authorizing agent indicates the number of services authorized which may or may not equal the number requested in Field 18 (Number Of Services). |
| 20.A=Approved D=Denied | None | Leave Blank Providers should check the PAR on-line or refer to the PAR letter. |
| 21.Primary Care Physician (PCP) Name | Text | Conditional Complete if member has a PCP. Enter the PCP's name as it appears on the current eligibility verification. |
| Telephone Number | Text | Optional Enter the PCP's telephone number. |
| 22.Primary Care Physician Address | Text | Conditional Complete if member has a PCP. Enter the PCP's complete address. |
| 23.PCP Provider Number | 8 Digits | Conditional Complete if member has a PCP. Enter the PCP's eight (8)-digit Colorado Medical Assistance provider number. This number must be obtained by contacting the PCP for the necessary authorization. |
| 24.Name and Address of Provider Requesting Prior Authorization | Text | Required Enter the complete name and address of the physician requesting prior authorization (the physician ordering/writing the prescription). |
| 25.Name of Provider Who will Render Service | Text | Required Enter the name and telephone number of the supplier who will render the service. |
| 26.Signature | Text | Required The prescribing authority must sign the PAR or the prescription must be attached. If prescription is attached notate "see attached." Do not send the original prescription, send a photocopy on an 8¬Ω x 11 sheet. The written diagnosis must be entered in Field 11 (Diagnosis), even if a prescription form is attached. A rubber stamp facsimile signature is not acceptable on the PAR. |
| Telephone Number | Text | Required Enter the telephone number of the requesting provider. |
| 27. Date Signed | 6 Digits | Required Enter the date the PAR form is signed by the requesting provider. |
| 28. Requesting Provider Number | 8 Digits | Required Enter the eight (8)-digit Health First Colorado provider number of the requesting provider. |
| Telephone Number | Text | Required Enter the telephone number of the requesting provider. |
| 29. Billing Provider Number | 8 Digits | Required Enter the eight (8)-digit Health First Colorado provider number of the billing provider. The billing provider must be enrolled in Health First Colorado. |
| 30. Comments or Reasons For Denial of Benefits | None | Leave Blank Refer to the PAR response for comments submitted by the authorizing agency. |
| 31. PA Number Being Revised | Text | Leave Blank This field is completed by the authorizing agency. |
Paper Claim Reference Table
Supply and DME claims are submitted on the CMS 1500 claim form or as an 837P transaction. The following paper claim form reference table shows required fields and detailed field completion instructions.
Instructions for completing and submitting electronic claims are available through the X12N Technical Report 3 (TR3) for the 837P (wpc-edi.com), 837P Companion Guide (on the Electronic Data Interchange (EDI) Support web page of the Department's website), and in the Web Portal User Guide (via within the Provider Web Portal).
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 010125 for January 1, 2025. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "yes", enter the insured's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "yes", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11d is marked "yes", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010125 for January 1, 2025. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked YES, complete 9, 9a and 9d | ||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. Enter the applicable qualifier to identify which date is being reported 431 Onset of Current Symptoms or Illness 484 Last Menstrual Period | ||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Required | Providers are required to include the NPI of the referring provider in this field. In the Provider Web Portal, this field may be labeled as “referring provider”. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010125 for January 1, 2025. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | Durable Medical Equipment Complete for DME purchases, repairs, and labor. Enter the make, model and serial number of the equipment. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | Complete for medical equipment and supplies that require prior authorization. If the procedure code requires prior authorization, enter the prior authorization from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agency or the fiscal agent. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010125 for January 1, 2025.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form.
| ||||||||||||||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area)
Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010125 for January 1, 2025. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||||||||||||||
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
Column Instructions for HCPCS Code Table
Code Column
HCPCS codes consist of a letter followed by four (4) numbers. Read the entire entry to determine the benefit status of the item. Providers are instructed to submit the HCPCS code most closely describing the item being requested on the PAR form. Health First Colorado reserves the right to amend the coding for any approved item.
Description Column
A description of the item as provided by Centers for Medicare & Medicaid Services (CMS) is listed. When possible and appropriate, the description of the item includes a notation of the billing unit. For disposable supplies, one (1) billing unit represents one (1) item unless otherwise noted.
PAR Column
This column is used to identify if prior authorization is required for the item identified and to identify which reviewing agency to send the PAR to for review.
| Yes | PARs for these items are reviewed by the ColoradoPAR Program. |
| No | The identified item does not require prior authorization when provided to an eligible member. If there is a unit limit and the member needs to exceed that limit, a PAR may be submitted. |
| Con | (Conditional) The item requires prior authorization under certain circumstances. Refer to the comments section next to the item or the subheading description for an explanation of the circumstances. |
Unit Limit Column
Unit limits are displayed with the maximum unit allowable and the minimum time between requests. Some items may have special provisions for unit limits with more detail in the Comment Column.
- Y = Year
- M = Month
- W = Week
- D = Day
**This column is being updated on a continual basis, further updates will be made to complete this column. No changes are being made to unit limits, they are only being identified in an easily accessible column. Unit limits may be identified in the comment column until changes are made.**
Comment Column
The comment section outlines specific or special instructions as well as more detailed information on unit limits where applicable.
Comments expand on the description and identify any required special PAR or billing instructions. The notation "DELETED" means that the code is invalid effective the day following the date shown in the "COMMENTS" column. Newly added codes become effective on the date shown. For example, procedure codes deleted effective 12/31/17 can be used only for non-prior authorized services provided prior to 1/1/18 or on PARs approved prior to 1/1/18.
Questionnaires: Some codes require a questionnaire to be filled out to be sent in with the PAR. The questionnaires are located on the Provider Forms web page under the Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) Forms drop-down menu. In the code table, a questionnaire is indicated by 'Q' and the number associated with the questionnaire (i.e., Q1, Q2, Q15, etc.).
F2F: (Face-to-face) Codes that fall under the face-to-face regulation are indicated by the notation 'F2F'. Please refer to the Face-To-Face section of this manual for details of the regulation.
HCPCS Code Table
This opens a new web page, and there are links back to this section of this manual.
CRT HCPCS Code Table
The following codes are pure CRT codes. Only qualified CRT suppliers may bill for these codes.
For the purpose of the table below only, note the following definitions.
Pursuant to HB22-1290 Changes to Medicaid for Wheelchair Repairs, the department will no longer require prior authorization requests (PARs) for repairs of Complex Rehabilitative Technology (CRT) equipment. Effective July 1, 2022, claims related to the repair of CRT will not require a PAR when billed with modifiers RB. Refer to the definition of repair below to clarify what is included in this policy.
Note: The PAR column in the table below is for purchase only and not repair.
New
- Purchase of equipment not previously owned.
- Replacement equipment after the 5th year mark for adults and 3rd year mark for children.
Mod (Modification)
A change or alteration to a member-owned piece of equipment. I.E. A different seating system to be placed on an existing base.
Con (Conditional)
Specialty eval is only required when the member is switching from or adding to a standard drive control (Joystick, any type) and/or attendant control.
Repair
Repair is fixing any part of the equipment so that it performs in a way that is safe and functional for the member. Repair can include replacement where the replacement part was original to the equipment base. Adding equipment that was not part of the original base is a modification.
CRT HCPCS Code Table
*The Specialty Eval column represents when the eval is required and is not intended to limit or restrict access to Specialty Evals.
Clarification Note (added April 2025): even if a HCPCS code in this table shows “No” in the Specialty Eval column, a Specialty Evaluation is still required if the item will be customized.
| Code | Description | PAR | Unit Limits | Comments | Specialty Eval | |
|---|---|---|---|---|---|---|
| New | Mod | |||||
| E0637 | Combination sit to stand/table system, any size including pediatric, with seat lift feature, with or without wheels | Yes | Required: F2F | Yes | Yes | |
| E0638 | Standing frame/table system, one (1) position (e.g. upright, supine or prone stander), any size including pediatric, with or without wheels | Yes | Required: F2F | Yes | Yes | |
| E0641 | Standing frame/table system, multi-position (e.g. three (3)-way stander), any size including pediatric, with or without wheels | Yes | Required: F2F | Yes | Yes | |
| E0642 | Standing frame/table system, mobile (dynamic stander), any size including pediatric | Yes | Required: F2F | Yes | Yes | |
| E0986 | Manual wheelchair accessory, push activated power assist, each | Yes | Required: F2F | No | No | |
| E1002 | Wheelchair accessory, power seating system, tilt only | Yes | Required: Q15 | Yes | Yes | |
| E1003 | Wheelchair accessory, power seating system, recline only, without shear reduction | Yes | Required: Q15 | Yes | Yes | |
| E1004 | Wheelchair accessory, power seating system, recline only, with mechanical shear reduction | Yes | Required: Q15 | Yes | Yes | |
| E1005 | Wheelchair accessory, power seating system, recline only, with power shear reduction | Yes | Required: Q15 | Yes | Yes | |
| E1006 | Wheelchair accessory, power seating system, combination tilt and recline, without shear reduction | Yes | Required: Q15 | Yes | Yes | |
| E1007 | Wheelchair accessory, power seating system, combination tilt and recline, with mechanical shear reduction | Yes | Required: Q15 | Yes | Yes | |
| E1008 | Wheelchair accessory, power seating system, combination tilt and recline, with power shear reduction | Yes | Required: Q15 | Yes | Yes | |
| E1009 | Wheelchair accessory, addition to power seating system, mechanically linked leg elevation system, including pushrod and leg rest, each | Yes | Yes | Yes | ||
| E1010 | Wheelchair accessory, addition to power seating system, power leg elevation system, including pushrod and leg rest, each | Yes | Yes | Yes | ||
| E1011 | Modification to pediatric size wheelchair width adjustment package (not to be dispensed with initial chair) | Yes | For modification of existing wheelchair only | No | No | |
| E1012 | Wheelchair accessory, addition to power seating system, center mount power elevating leg rest/platform, complete system, any type, each | Yes | Yes | Yes | ||
| E1014 | Reclining back, addition to pediatric size wheelchair | Yes | Required: F2F, Q15 | No | No | |
| E1032 | Wheelchair accessory, manual swingaway, retractable or removable mounting hardware used with joystick or other drive control interface | Yes | Required: F2F. Code opened 4-1-2025 | No | No | |
| E1033 | Wheelchair accessory, manual swingaway, retractable or removable mounting hardware for headrest, cushioned, any type | Yes | Required: F2F. Code opened 4-1-2025 | No | No | |
| E1034 | Wheelchair accessory, manual swingaway, retractable or removable mounting hardware for lateral trunk or hip support, any type | Yes | 4/Y | Required: F2F. Code opened 4-1-2025 | No | No |
| E1037 | Transport chair, pediatric size | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1161 | Manual adult size wheelchair, includes tilt- in-space | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1220 | Wheelchair, specially sized or constructed (indicate brand name, model number, if any, and justification) | Yes | Yes | No | ||
| E1228 | Special back height for wheelchair | Yes | Required: F2F | No | No | |
| E1229 | Wheelchair, pediatric size, not otherwise specified | Yes | Yes | No | ||
| E1231 | Wheelchair, pediatric size, tilt-in-space, rigid, adjustable, with seating system | Yes | No | No | ||
| E1232 | Wheelchair, pediatric size, tilt-in-space, folding, adjustable, with seating system | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1233 | Wheelchair, pediatric size, tilt-in-space, rigid, adjustable, without seating system | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1234 | Wheelchair, pediatric size, tilt-in-space, folding, adjustable, without seating system | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1235 | Wheelchair, pediatric size, rigid, adjustable, with seating system | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1236 | Wheelchair, pediatric size, folding, adjustable, with seating system | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1237 | Wheelchair, pediatric size, rigid, adjustable, without seating system | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1238 | Wheelchair, pediatric size, folding, adjustable, without seating system | Yes | Required: F2F *Code is subject to the 2019 DME UPL | No | No | |
| E1239 | Power wheelchair, pediatric size, not otherwise specified | Yes | Yes | No | ||
| E2209 | Accessory, arm trough, with or without hand support, each | Yes | 1 unit = 1 arm trough | No | No | |
| E2291 | Back, planar, for pediatric size wheelchair including fixed attaching hardware | Yes | No | No | ||
| E2292 | Seat, planar, for pediatric size wheelchair including fixed attached hardware | Yes | No | No | ||
| E2293 | Back, contoured, for pediatric size wheelchair including fixed attaching hardware | Yes | No | No | ||
| E2294 | Seat, contoured, for pediatric size wheelchair including fixed attaching hardware | Yes | No | No | ||
| E2295 | Manual wheelchair accessory, for pediatric size wheelchair, dynamic seating frame, allows coordinated movement of multiple positioning features | Yes | Yes | No | ||
| E2298 | Complex rehabilitative power wheelchair accessory, power seat elevation system, any type | Yes | Required: Q17 Code Opened 04-01-2024. | Yes | Yes | |
| E2300 | Wheelchair accessory, power seat elevation, system, any type | Yes | Required: Q17 Code closed 03-31-2024 | Yes | Yes | |
| E2301 | Wheelchair accessory, power standing system, any type | Yes | Yes | Yes | ||
| E2310 | Power wheelchair accessory, electronic connection between wheelchair controller and two (2) or more power seating system motor, including all related electronics, indicator feature, mechanical function selection switch, and fixed mounting hardware | Yes | Yes | No | ||
| E2311 | Power wheelchair accessory, electronic connection between wheelchair controller and one (1) power seating system motor, including all related electronics, indicator feature, mechanical function selection switch, and fixed mounting hardware | Yes | Yes | No | ||
| E2312 | Power wheelchair accessory, hand or chin control interface, mini-proportional remote joystick, proportional, including fixed mounting hardware | Yes | Yes | No | ||
| E2313 | Power wheelchair accessory, harness for upgrade to expandable controller, including all fasteners, connectors and mounting hardware, each | Yes | Yes | No | ||
| E2321 | Power wheelchair accessory, hand control interface, remote joysticks, non- proportional, including all related electronics, mechanical stop switch, and fixed mounting hardware | Yes | Yes | No | ||
| E2322 | Power wheelchair accessory, hand control interface, multiple mechanical switches, non-proportional, including all related electronics, mechanical stop switch, and fixed mounting hardware | Yes | Yes | No | ||
| E2323 | Power wheelchair accessory, specialty joystick handle for hand control interface, prefabricated | Yes | Yes | No | ||
| E2324 | Power wheelchair accessory, chin cup for chin control interface | Yes | No | No | ||
| E2325 | Power wheelchair accessory, sip and puff interface, non-proportional, including all related electronics, mechanical stop switch, and manual swing away mounting hardware | Yes | Yes | Yes | ||
| E2326 | Power wheelchair accessory, breath tube kit for sip and puff interface | Yes | No | No | ||
| E2327 | Power wheelchair accessory, head control interface, mechanical, proportional, including all related electronics, mechanical direction change switch, and | Yes | Yes | Con | ||
| E2328 | Power wheelchair accessory, head control or extremity control interface, electronic, proportional, including all related electronics and fixed mounting hardware | Yes | Yes | Con | ||
| E2329 | Power wheelchair accessory, head control interface, contact switch mechanism, non- proportional, including all related electronics, mechanical stop switch, mechanical direction change switch, head array, and fixed mounting hardware | Yes | Yes | Con | ||
| E2330 | Power wheelchair accessory, head control interface, proximity switch mechanism, non-proportional, including all related electronics, mechanical stop switch, mechanical direction change switch, head array, and fixed mounting hardware | Yes | Yes | Con | ||
| E2331 | Power wheelchair accessory, attendant control, proportional, including all related electronics and fixed mounting hardware | Yes | Yes | Yes | ||
| E2351 | Power wheelchair accessory, electronic interface to operate speech generating device using power wheelchair control interface | Yes | No | No | ||
| E2373 | Power wheelchair accessory, hand or chin control interface, compact remote joystick, proportional, including fixed mounting hardware | Yes | Yes | No | ||
| E2374 | Power wheelchair accessory, hand or chin control interface, standard remote joystick (not including controller), proportional, including all related electronics and fixed mounting hardware, replacement only | Con | one (1) per three (3) Y | PAR required for more than one (1) per three (3) Y | No | No |
| E2376 | Power wheelchair accessory, expandable controller, including all related electronics and mounting hardware, replacement only | Con | one (1) per Y | Over one (1) unit requires PAR | No | No |
| E2377 | Power wheelchair accessory, expandable controller, including all related electronics and mounting hardware, upgrade provided at initial issue | Yes | No | No | ||
| E2609 | Custom fabricated wheelchair seat cushion, any size | Yes | Identify specific brand/name of cushion requested on prior authorization request | Yes | Yes | |
| E2610 | Wheelchair seat cushion, powered | Yes | Identify specific brand/name of cushion requested on prior authorization request | Yes | Yes | |
| E2617 | Custom fabricated wheelchair back cushion, any size, including any type mounting hardware | Yes | Identify specific brand/name of cushion requested on prior authorization request | Yes | Yes | |
| E8000 | Gait trainer, pediatric size, posterior support, includes all accessories and components | Yes | Use for adults also.Required: F2F | Yes | Yes | |
| E8001 | Gait trainer, pediatric size, upright support, includes all accessories and components | Yes | Use for adults also. Required: F2F | Yes | Yes | |
| E8002 | Gait trainer, pediatric size, anterior support, includes all accessories and components | Yes | Use for adults also. Required: F2F | Yes | Yes | |
| K0005 | Ultra-lightweight wheelchair | Yes | Required: F2F *Code is subject to the 2019 DME UPL | Yes | No | |
| K0008 | Custom manual wheelchair base | Yes | Yes | No | ||
| K0009 | Other manual wheelchair/base | Yes | Do not use for titanium manual wheelchairs, see K0005 or K0008. *Code is subject to the 2019 DME UPL | Yes | No | |
| K0669 | Wheelchair accessory wheelchair seat or back cushion does not meet specific code criteria or no written coding verification from DME PDAC | Yes | Yes | Yes | ||
| K0835 | Power wheelchair, group 2 standard, single power option, single power option, sling/solid seat/back, patient weight capacity up to and including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0836 | Power wheelchair, group 2 standard, single power option, captain's chair. Member weight capacity up to and including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0837 | Power wheelchair, group 2 heavy duty, single power option, sling/solid seat/back, patient weight capacity 301 to 450 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0838 | Power wheelchair, group 2 heavy duty, single power option, captain's chair, patient weight capacity 301 to 450 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0839 | Power wheelchair, group 2 very heavy duty, single power option, sling/solid seat/back, patient weight capacity 451 to 600 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0840 | Power wheelchair, group 2 very heavy duty, single power option, sling/solid seat/back, patient weight capacity 601 pounds or more | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0841 | Power wheelchair, group 2 standard, multiple power option, sling/solid seat/back, patient weight capacity up to including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0842 | Power wheelchair, group 2 standard, multiple power option, captain's chair, patient weight capacity up to and including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0843 | Power wheelchair, group 2 heavy duty, multiple power option, sling/solid seat/back, patient weight capacity 301 to 450 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0848 | Power wheelchair, group 3 standard, sling/solid seat/back, patient weight capacity up to and including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0849 | Power wheelchair, group 3 standard, captain's chair, patient weight capacity up to and including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0850 | Power wheelchair, group 3 heavy duty, sling/solid seat/back, patient weight capacity 301 to 450 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0851 | Power wheelchair, group 3 heavy duty, captain's chair, patient weight capacity 301 to 450 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0852 | Power wheelchair, group 3 very heavy duty, sling/solid seat/back, patient weight capacity 451 to 600 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0853 | Power wheelchair, group 3 very heavy duty, captain's chair, patient weight capacity, 451 to 600 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0854 | Power wheelchair, group 3 extra heavy duty, sling/solid seat/back, patient weight capacity 601 pounds or more | Yes | Yes | No | ||
| K0855 | Power wheelchair, group 3 extra heavy duty, captain's chair, patient weight capacity 601 pounds or more | Yes | Yes | No | ||
| K0856 | Power wheelchair, group 3 standard, single power option, sling/solid seat/back, patient weight capacity up to and including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0857 | Power wheelchair, group 3 standard, single power option, captain's chair, patient weight capacity up to and including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0858 | Power wheelchair, group 3 heavy duty, single power option, sling/solid seat/back, patient weight capacity 301 to 450 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0859 | Power wheelchair, group 3 heavy duty, single power option, captain's chair, patient weight capacity 301 to 450 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0860 | Power wheelchair, group 3 very heavy duty, single power option, sling/solid seat/back. Member weight capacity 451 to 600 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0861 | Power wheelchair, group 3 standard, multiple power option, sling/solid seat/back, patient weight capacity up to including 300 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0862 | Power wheelchair, group 3 heavy duty, multiple power option, sling/solid seat/back, patient weight capacity 301 to 450 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0863 | Power wheelchair, group 3 very heavy duty, multiple power option, sling/solid seat/back, patient weight capacity 451 to 600 pounds | Yes | *Code is subject to the 2019 DME UPL | Yes | No | |
| K0864 | Power wheelchair, group 3 extra heavy duty, multiple power option, sling/solid seat/back, patient weight capacity 601 pounds or more | Yes | Yes | No | ||
| K0868 | Power wheelchair, group 4 standard, sling/solid seat/back, patient weight capacity up to and including 300 pounds | Yes | Yes | No | ||
| K0869 | Power wheelchair, group 4 standard, captain's chair, patient weight capacity up to and including 300 pounds | Yes | Yes | No | ||
| K0870 | Power wheelchair, group 4 heavy duty, sling/solid seat/back, patient weight capacity 301 to 450 pounds | Yes | Yes | No | ||
| K0871 | Power wheelchair, group 4 very heavy duty, sling/solid seat/back, patient weight capacity 451 to 600 pounds | Yes | Yes | No | ||
| K0877 | Power wheelchair, group 4 standard, single power option, sling/solid seat/back, patient weight capacity up to including 300 pounds | Yes | Yes | No | ||
| K0878 | Power wheelchair, group 4 standard, single power option, captain's chair, patient weight capacity up to and including 300 pounds | Yes | Yes | No | ||
| K0879 | Power wheelchair, group 4 heavy duty, single power option, sling/solid seat/back, patient weight capacity 301 to 450 pounds | Yes | Yes | No | ||
| K0880 | Power wheelchair, group 4 very heavy duty, single power option, sling/solid seat/back, patient weight 451 to 600 pounds | Yes | Yes | No | ||
| K0884 | Power wheelchair, group 4 standard, multiple power option, sling/solid seat/back, patient weight capacity up to and including 300 pounds | Yes | Yes | No | ||
| K0885 | Power wheelchair, group 4 standard, multiple power option, captain's chair weight capacity up to and including 300 pounds | Yes | Yes | No | ||
| K0886 | Power wheelchair, group 4 heavy duty, multiple power option, sling/solid seat/back, patient weight capacity 301 to 450 pounds | Yes | Yes | No | ||
| K0890 | Power wheelchair, group 5 pediatric, single power option, sling/solid seat/back, patient weight capacity up to and including 125 pounds | Yes | Yes | No | ||
| K0891 | Power wheelchair, group 5 pediatric, multiple power option, sling/solid seat/back, patient weight capacity up to and including 125 pounds | Yes | Yes | No | ||
| K0898 | Power wheelchair, not otherwise classified | Yes | Yes | No | ||
Supply (Wound Care) CMS 1500 Claim Example
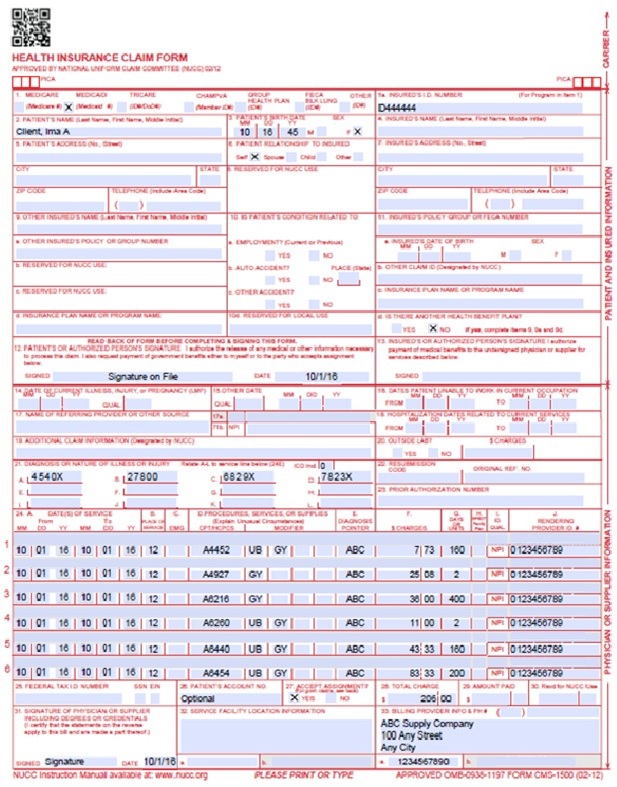
DME (Wheelchair) CMS 1500 Claim Example
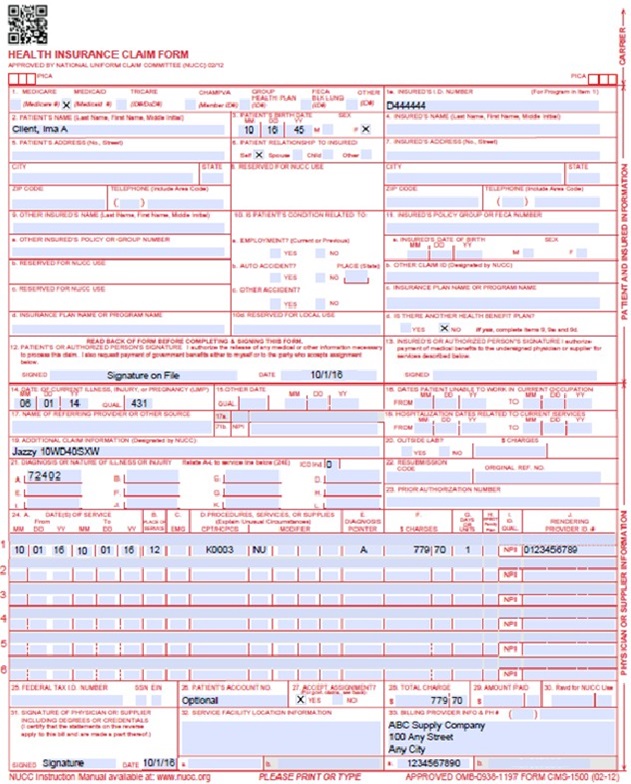
Retired DMEPOS Policies
Over-The-Counter, At-Home COVID-19 Tests
Effective January 15, 2022, OTC at-home COVID-19 rapid tests are a covered benefit for Health First Colorado Members. Providers should use HCPCS procedure code E1399+U1 to bill for these tests. These tests are covered for dates of service through September 30, 2024. Effective October 1, 2024, OTC COVID-19 tests are not a covered benefit.
Coverage Criteria:
- Member co-pays are not required.
- Prior Authorization is not required.
- Test coverage is limited to 15 units of service per month per member.
- Span-billing is permitted for monthly allowance.
- One (1) unit of service is equal to one (1) individual test. If a package includes two (2) tests, the provider should bill for two (2) units of service.
- Providers must bill Health First Colorado the same amount as the retail price on a per-test basis. For example, if the provider sells a two (2)-test pack for $14, they would bill two (2) units of service at $7 each to Health First Colorado.
- A prescription is necessary to receive reimbursement, as is required for all DMEPOS. However, the Public Readiness and Emergency Preparedness Act allows for pharmacists to order these tests.
- Providers must use the NPI of the ordering provider, such as the pharmacist, on all claims.
- All claims for tests should also be billed to Gainwell Technologies (GWT) Fee-For-Service (FFS), including for members enrolled in the Denver Health and Rocky Mountain Health Plan managed care networks.
- Tests are a benefit for members regardless of diagnosis. However, diagnosis code Z20.822 for potential COVID exposure is also appropriate.
Continuous Glucose Monitors (CGM) Coverage Policy Prior to November 1, 2025
For prior authorization requests prior to November 1, 2025, the following criteria must be followed:
CGMs and related supplies are covered by Health First Colorado when all of the following coverage criteria (1-5) are met:
- The beneficiary has diabetes mellitus; and
- The beneficiary is insulin-treated with multiple (three [3] or more) daily administrations of insulin or a continuous subcutaneous insulin infusion (CSII) pump; and,
- The beneficiary’s insulin treatment regimen requires frequent adjustment by the beneficiary on the basis of BGM or CGM testing results; and,
- Within six (6) months prior to ordering the CGM, the treating practitioner has an in-person visit with the beneficiary to evaluate their diabetes control and determines that criteria (1-3) above are met; and,
- Every six (6) months following the initial prescription of the CGM, the treating practitioner has an in-person visit with the beneficiary to assess adherence to their CGM regimen and diabetes treatment plan.
Initial Coverage Criteria
- The beneficiary has diabetes mellitus; and
- The beneficiary is insulin-treated with multiple (three [3] or more) daily administrations of insulin or a continuous subcutaneous insulin infusion (CSII) pump; and
- The beneficiary’s insulin treatment regimen requires frequent adjustment by the beneficiary on the basis of BGM or CGM testing results; and
- Within six (6) months prior to ordering the CGM, the treating practitioner has an in-person or telehealth visit with the beneficiary to evaluate their diabetes control and determines that criteria (1-3) above are met; and
- Every six (6) months following the initial prescription of the CGM, the treating practitioner has an in-person or telehealth visit with the beneficiary to assess adherence to their CGM regimen and diabetes treatment plan; and
- Receipt of, or documented plan to receive, diabetes education specific to the use of CGMs; and,
- Be able to hear and view the CGM alerts and respond accordingly, or have a caregiver who is able to do so, and
- Providers should verify that the patient meets the manufacturer’s recommendations for appropriate age range, testing and calibration requirements, etc. before prescribing the CGM device.
- Or has an otherwise qualifying circumstance or is otherwise deemed medically necessary.
Back to Top
Reauthorization Criteria + Supplies
- Individual meets all the initial criteria (except for the SMBG requirement), and
- In-person or telehealth visit with treating practitioner within at least six (6) months of CGM renewal prescription, and
- Provider determines that the individual is regularly utilizing the device.
- Individual receives ongoing instruction and evaluation of technique, results, and their ability to use data from CGM to adjust therapy, or
- Has an otherwise qualifying circumstance or is otherwise deemed medically necessary.
- For members who initially qualified for a CGM with three (3) or more daily insulin administrations, reauthorization may be approved even if use of a CGM has since decreased their daily insulin needs.
DMEPOS Revisions Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 2/22/2018 | Minor style/formatting edits | HCPF |
| 3/26/2018 | TENS/NMES: removed duplicated rows from HCPCS Table and moved the policy guidance to the Covered Benefits section. C/BiPAP: Updated rental minimum from 60 to 30 days Added clarification on the usage of the RA, RB, NU, and UE modifiers under Billing for Wheelchairs. Added RA modifier to last bullet under (wheelchair) repairs and mods. Re-titled AACDs to SGDs, removed language regarding incorporation by reference in the CCR, and added language from the 2013 AACD BCS that was not put into Rule. Pricing: Updated Rule reference from 8.590.7.I to 8.590.7, updated section to reflect 1.402% rate increase from Long Bill (SB17-254), added clarity/re-worded By Invoice section. Added information regarding upcoming process change (no A9901). A4649/T5999 E2378: corrected units from 1 to 3 per year (1 per feature) | HCPF |
| 6/25/2018 | Updated general billing and timely to point to general manual | HCPF |
| 2/11/2019 | Updated Manufacturer Suggested Retail Price (MSRP) section with new percentage calculation examples. | DXC |
| 3/9/2019 | Updated the codes subject to the Upper Payment Limit as identified by the PDAC codes both Medicare and Medicaid paid for in 2019. Added Prosthetic and Orthotic codes with current prior authorization requirements and associated unit limits. Removed NCCI MUE unit limits and redirected providers to see the NCCI MUE list to reflect most current limits published by CMS. Manufacturers Suggested Retail Price (MSRP) reimbursement updated to reflect July 1, 2018 rates. | HCPF |
| 7/10/2019 | Updated Appendices' links and verbiage | DXC |
| 7/18/2019 | Added new rates for lesser-of | HCPF |
| 2/26/2020 | Converted to web page | HCPF |
| 9/10/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 10/21/2020 |
| HCPF |
| 3/2/2021 |
| HCPF |
| 5/6/2021 |
| HCPF |
| 8/26/2021 |
| HCPF |
| 10/5/2021 | Updated CGM product table | HCPF |
| 1/15/2022 | • Updated manual pricing percentages.
| HCPF |
| 3/1/2022 | • Specific coverage criteria for A4437 added. • DME safety policy added. • Cochlear Implant Processor replacement criteria added. • Diagnosis code information added to COVID-19 test coverage. • Enclosed/safety bed criteria added. • SGD coverage updated (additions made were previously enforced). • E2300 in CRT code table updated to include Q17 as a requirement (was previously removed by accident). • Peristeen coding has been updated. • F2F requirement removed from codes E0973, E0981, and E0982 to be aligned with F2F policy for replacement/repair. | HCPF |
| 7/1/2022 | • CGM attestation for education requirement added. • DME enclosed/safety bed policy updated. • Added clarification that BAHAs are included in Cochlear implant replacement policy. • Manual pricing percentages were updated. • Questionnaire #10 added as optional form. • New Omnipod billing instructions added. • Clarified CRT policy. • PAR policy on CRT repairs from HB22-1290 added to CRT section and CRT code table. • New Omnipod billing instructions added. • Added F2F requirements for continuous rental items, policy was previously enforced. • Corrected weight from 200lbs to 250lbs for K0006 on HCPCS table. • New breast pump coverage added. | HCPF |
| 10/01/2022 | • Included bed rail policy from October 2022 provider bulletin. • Changed ‘electric’ breast pumps to ‘single user’ for clarification. • Minor Formatting updates | HCPF |
| 12/01/2022 | • Added FreeStyle Libre 3 to CGM devices. • Corrected start of services definition to be aligned with CCR, F2F requirement did not change. • Updated eligible prescribers. • Midwives added as prescriber in Breast Pump policy. • Removed manufacturer specific TAI product language. • Edited Enteral Nutrition Products to include WIC supply issues. • Vocational DME added. | HCPF |
| 01/01/2023 | • Multi-user breast pump policy published • Single user policy updated to include early delivery per EPSDT. • Clarified CPAP replacement policy does not cover replacements due to age. • Details added to field 17 in paper claims reference table. | HCPF |
| 04/01/2023 | • Added Dexcom G7 to CGM covered Devices. • CGM Upgrade policy published. • Defined repair for CRT PAR policy. • Removed AACD policy standard link and embedded it into the manual. • Defined Hip Kits. • Clarification made to wipes policy. • Updated unit limits for procedure codes A4927, A4452, T4521-T4535, T4543, T4544, A4207, A4353, B4087, B4088, A4216 effective April 1, 2023. See provider bulletin for details. | HCPF |
| 05/01/2023 | • Added procedure codes A4238 and E2102 effective 5-1-2023 • Added procedure codes from 4-1-2023 CMS update • Corrected A4250 coding description to 100 strips per unit • Deleted A4649 from HCPCS page, as code was replaced by T5999 see October 2017 provider bulletin for details. • Wheelchair benefit coverage standard converted to web format and linked within manual. | HCPF |
| 07/01/2023 | • Updated MSRP and Invoice pricing percentages effective July 1, 2023 • Corrected manually priced rentals should be divided by 10 months, not 13 to be aligned with how rental rates are established. | HCPF |
| 01/01/2024 | • Span billing policy updated to allow for NCCI MUE limits. • Osteogenic stimulator criteria added. • Guardian sensor 4 added to CGM covered devices. | HCPF |
| 04/01/2024 | • CGM Upgrade policy edited and FreeStyle Libre 2 Plus added to covered devices. • CRT provider metrics instructions added. • 2024 HCPCS added. | HCPF |
| 07/01/2024 | • April HCPCS added. • July 1, 2024, manual pricing percentages updated. • OTC At-Home COVID-19 Test coverage end date added. • A9272 PAR status corrected • Continuous passive motion devices criteria added. • Advanced lymphedema pumps criteria added. | HCPF |
| 12/17/2024 | Corrected MSRP and Invoicing rates. | HCPF |
| 03/18/2025 | • October 2024 HCPCS added. • January 2025 HCPCS added. • April 2025 HCPCS added. • Clarified this clarifying language to CGM coverage section: “For members who initially qualified for a CGM with three (3) or more daily insulin administrations, reauthorization may be approved even if use of a CGM has since decreased their daily insulin needs.” | HCPF |
| 04/25/2025 | • HCPCS table • Added policy around human milk fortifier; Effective 6-1-2025, these products can be provided with Medicaid as the primary payer instead of WIC. • Updated unit limit for HCPCS E0603, effective 5-1-2025 limited to 2 per state fiscal year • Removed PAR requirement for HCPCS A4282-A4286 effective 5-1-2025 • Added new codes covered effective 4-1-2025 (A6515, A6516, A6517, A6518, A6519, A6611, A9154, E0201, E1022, E1023, E1032, E1033, E1034, E1832, L0720, L1933, L1952, L5827, L6028, L6029, L6030, L6031, L6032, L6033, L6037, L6700, L7406 • Updated enclosed safety bed coverage to specify that Questionnaire #19 will again be required effective June 1, 2025. • Added in CRT code table: Clarification Note (added April 2025): even if a HCPCS code in this table shows “No” in the Specialty Eval column, a Specialty Evaluation is still required if the item will be customized. • Clarified the need for Face-to-Face requirements for HCPCS: T5001, E0637, E0638, E0641, E0642, E8000, E8001, E8002. • For E1399 in the coding manual under Walkers category, added “For walkers and gait trainers assigned code E1399 by the PDAC, a F2F and Specialty Eval are required. Updated the descriptions for A4453 and A4459 effective 4-1-25. | HCPF |
| 5/28/2025 | • Updated manually priced percentages effective July 1, 2025 • Under span billing for certain supplies, added transanal irrigation products (HCPCS A4453) • Updated policy for transanal irrigation system to match April 2025 updates to HCPCS. • Added Nerivio coverage criteria • Added clarification that clinical pharmacists can order/prescribe CGMs • Added clarification to HCPCS manual for code A4284 that it has a MUE limit of 1 per day, and that 1 Unit of Service = 1 pair/set of replacement breast shields/flanges. • Added A9999 to the Breast Pump Supplies HCPCS manual section specifying its use for membrane and value replacement parts | HCPF |
| 6/23/2025 | • Updated breast pump policy to include E0603 with modifier U1 as a bundled option that must include a manual pump, an electric pump and replacement shields/flanges being billed on the same date of service. • Added Return of Incorrect Equipment information. • Updated Continuous Glucose Monitor (CGM) with the Wholesale Acquisition Cost (WAC) and NDC crosswalk table. • Updated policy for A9901 as a non-covered service and delivery, set-up and supplies are included in the payment rates for DME, Supply, Orthotic or Prosthetic items. | HCPF |
| 7/21/2025 | • Update to include occupational therapists as prescribing providers effective August 6, 2025. • Update to the wheelchair policy coverage to provide specificity that wheelchair mounted robotic arm devices are not covered as of August 1, 2025. | HCPF |
| 8/13/2025 | • Update to include E0766 on the DMEPOS HCPCS table. • Updates to Continuous Glucose Monitor (CGM), Wholesale Acquisition Cost (WAC), and NDC crosswalk table to include HCPCS and modifier updates • Added Heparin (HCPCS J1642) billing example and J1642 to DMEPOS HCPCS table • Updated Allowed Practitioners under the Face-to-Face Requirements | HCPF |
| 9/2/2025 | • Added Adaptive Car Seat and Buckle Clip Policy • Made edits to the CGM/NDC crosswalk • Added Medicare Glucose Policy link, effective Nov 1, 2025 • Moved Over-The-Counter COVID-19 tests to retired policies section • Made edits to the MSRP and By Invoice sections effective Oct 1, 2025 | HCPF |
| 9/25/2025 | • Fixed missing Medicare CGM policy link • Fixed misspelling of “June” in safety bed section • Added new HCPCS (A4288, L1007, L6034, L6035, L6038, L6039, E0150, E0658, E0659) effective October 1, 2025 • Updated descriptions to HCPCS L6028, L5673, L5679, L5783, and L7406 effective October 1, 2025 | HCPF |
| 10/20/2025 | • Added additional guidance for CGMs that do not have an NDC number specifying that Questionnaire 20 will need to be used and will need to be billed as a professional claim • Added gestational diabetes CGM policy, per SB24-168 • Added link to the Pharmacy Resource page for PDSL • Corrected CGM NDC/HCPCS table for Dexcom G6 and G7 receivers • Added HCPCS E1032, E1033, and E1034 to the CRT HCPCS table which were previously left off when added in April 2025 • Adjusted language throughout to reflect occupational therapists being allowed to prescribe/order equipment • Made units allowed for E1028, E1034, and A4287 on DMEPOS HCPCS Table | HCPF |
| 11/13/2025 | • Added Donor Breast Milk Coverage Policy section • Adjusted units allowed for E1034 on DMEPOS HCPCS Table | HCPF |
| 02/09/2026 | • Added physical therapist/occupational therapist as an ordering provider throughout. • Moved previous (prior to Nov 1, 2025) CGM criteria to the “Retired Policy” section • Added billing instructions for CGMs that do not have an NDC • Adjusted A4288 limit from 6/Y to 12/Y • Added HCPCS A4295, A4296, and A4297 and adjusted HCPCS A4351, A4352, and A4353 descriptions for the 2026 HCPCS | HCPF |