Enhance Quality Outcomes
The Need
A primary responsibility of the Department is ensuring the health, wellness, and safety of our members. As such, we must implement quality standards and maintain strict oversight of provider agencies. The Department proposes a series of projects to develop quality frameworks and oversight requirements, resulting in anticipated cost savings, provider accountability, and improved quality outcomes.
Initiative 8.02 - Provider Oversight
Read a more in-depth summary of this project's outcomes
Initiative 8.04 - Pay-for-Performance for PACE
Read a more in-depth summary of this project's outcomes
Initiative 8.05 - Pay-for-Performance for Home Health & HCBS
Read a more in-depth summary of this project's outcomes
Initiative 8.06 - PACE Licensure
Read a more in-depth summary of this project's outcomes
Initiative 8.07 - eConsult To Improve Quality
Read a more in-depth summary of this project's outcomes
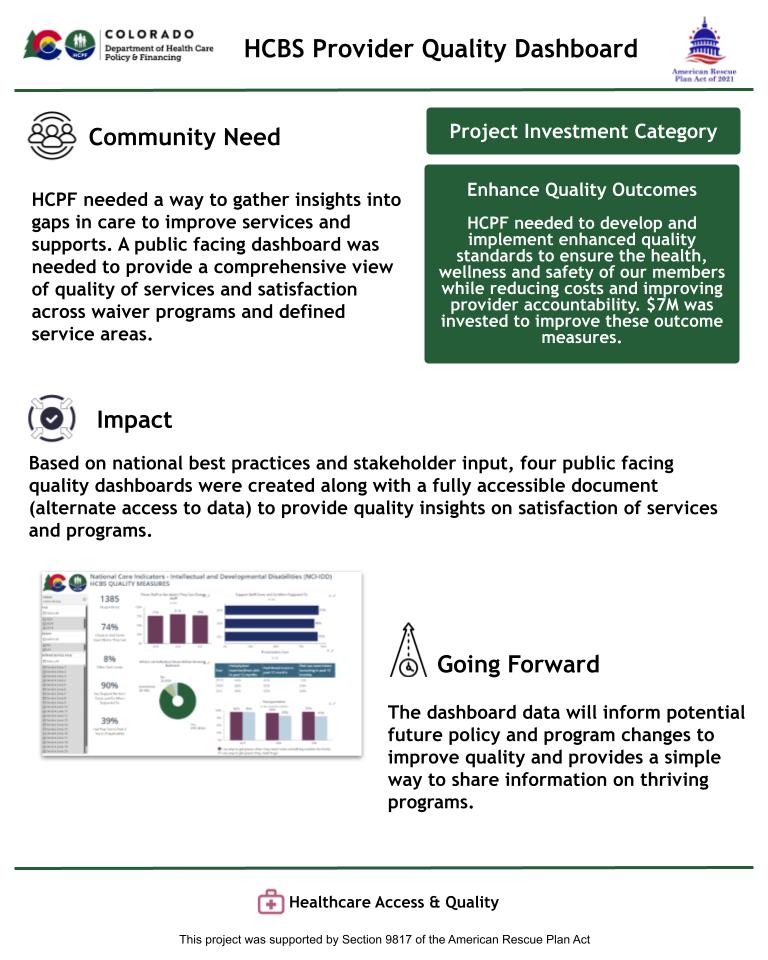
Initiative 8.08 - HCBS Provider Quality Dashboards
Read a more in-depth summary of this project's outcomes
Initiative 8.09 - Waiver Quality Expansion
Read a more in-depth summary of this project's outcomes
Initiative 8.10 - Criminal Justice Partnership
Read a more in-depth summary of this project's outcomes
Initiative 8.11 - Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Benefits Training
Read a more in-depth summary of this project's outcomes