Pediatric Behavioral Therapies Billing Manual
- Pediatric Behavioral Therapies Benefit Overview
- General Benefit Policies
- Payment for Covered Services
- Allowed Place for Service Codes
- General Billing Information
- Eligible Providers
- Prior Authorization Requests (PARs)
- CMS 1500 Paper Claim Reference Table
- Pediatric Behavioral Therapies Revisions Log
Return to Billing Manuals Web Page
The purpose of this billing manual is to provide policy and billing guidance to providers to obtain reimbursement for behavioral therapy services. This manual is updated periodically to reflect changes in policy and regulations. It applies only to the Health First Colorado (Colorado's Medicaid program) Pediatric Behavioral Therapies (PBT) Benefit and does not address services available through other Health First Colorado benefits or any services available through Home and Community-Based Services (HCBS) waiver programs.
Pediatric Behavioral Therapies Benefit Overview
Behavioral therapy services are a treatment that helps change maladaptive behaviors. These services must be found to be medically necessary to be covered.
The Pediatric Behavioral Therapies benefit is available to Health First Colorado members who:
- Are 20 years old and younger
- Meet the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) medically necessary criteria for behavioral therapy services. Visit the Early and Periodic Screening, Diagnostic and Treatment web page for more information on medical necessity
All PBT services must be pre-approved in a Prior Authorization Request (PAR) process. Visit the Provider Contact web page for the Colorado PAR information.
If a member requires support of a medically skilled caregiver to complete a task, such as bathing or hygiene, the associated task shall be considered skilled in nature and covered under other Health First Colorado state plan benefits. Visit the Home Health Program web page for more information.
If a member requires assistance with personal care tasks, those services are covered under other Health First Colorado state plan benefits. Visit the Pediatric Personal Care Benefit web page for more information.
Co-Treatment Matrix
The following chart represents co-treatment policy for PBT providers.
| Home Health Therapist | Pediatric Behavioral Therapist | Outpatient Therapist (Occupational, Physical, and Speech therapists) | Home Health CNA | Personal Care Provider | |
| Pediatric Behavioral Therapist | Allowable only with joint goals in PAR and with approval. | Allowable with clear reason for safety or medical necessity in PAR and with approval only. | Providers will only bill for the time interacting with the member, and not the total time in the room. Must have clear, joint goals in PAR and with approval. | Must provide and document the need for a multi-modality visit, and services must be documented in the care plan - services must be auditable. PBT goals and interventions must be documented in the plan of care with a description of how they are performed with CNA tasks. | Must provide and document the need for the multi-modality visit, and services documented in the care plan - services must be auditable. PBT goals and interventions must be documented in the plan of care with a description of how they are performed with PC tasks. |
Telemedicine and Pediatric Behavioral Therapy:
Pediatric Behavioral Therapists are covered under the telemedicine policy.
General Benefit Policies
- All Outpatient therapy services must have a written order/prescription/referral by any of the following:
- Physician (M.D. or D.O.)
- Physician Assistant
- Nurse Practitioner
- Licensed Psychologist
- An approved Individualized Family Service Plan (IFSP) for Early Intervention Speech Therapy. (Senate bill 07-004 states the IFSP "shall qualify as meeting the standard for medically necessary services." Therefore, no physician is required to sign a work order for the IFSP.)
- Pursuant to the Affordable Care Act's requirements that State Medicaid Agencies ensure correct ordering, prescribing, and referring (OPR) National Provider Identification (NPI) numbers be on the claim form (42 CFR § 455.440).
- Therapies provided as part of a member's individualized education program (IEP) by a therapist in the school setting and billing the School Health Services Program are not separately reimbursable. These services are paid for by the school district and providers may not submit claims for services performed in the school setting. Visit the School Health Services Program web page for details.
Payment for Covered Services
- Members may be billed for non-covered services in accordance with C.R.S. 25.5-4- 301(1)(a)(I).
- (1) (a) (I) Except as provided in section 25.5-4-302 and subparagraph (III) of this paragraph (a), no recipient or estate of the recipient shall be liable for the cost or the cost remaining after payment by Medicaid, Medicare, or a private insurer of medical benefits authorized by Title XIX of the social security act, by this title, or by rules promulgated by the state board, which benefits are rendered to the recipient by a provider of medical services authorized to render such service in the state of Colorado, except those contributions required pursuant to section 25.5-4- 209 (1). However, a recipient may enter into a documented agreement with a provider under which the recipient agrees to pay for items or services that are non-reimbursable under the medical assistance program. Under these circumstances, a recipient is liable for the cost of such services and items.
- If Prior Authorization Requests (PAR) for services are required, the following policy applies:
- Technical/lack of information (LOI) denial does not mean those services are not covered. Members may not be billed for services denied for LOI.
- Services partially approved are still considered covered services. Members may not be billed for the denied portion of the request.
- Services totally denied for not meeting medical necessity criteria are considered non-covered services.
Allowed Place of Service Codes
The following place of service codes are allowed:
| Place of Service (POS) | Code Description |
| 02 | Telemedicine (Refer to the Telemedicine Billing Manual) |
| 03 | School |
| 11 | Office |
| 12 | Home (Refer to the Electronic Visit Verification (EVV) Billing Manual) |
| 99 | Other - Community Based (Refer to the EVV Billing Manual) |
- Telemedicine place of service (POS) code 02 is available for specific procedure codes. Visit the Telemedicine - Provider Information web page for a list of allowed procedure codes.
- Effective May 3, 2024, place of service 03 is an allowed place of service for all fee-for-service benefits. In order for community providers to bill fee-for-service to children in a school setting, the provider must follow school district policy. Please reference the Community Providers in a School Setting Policy memo.
- Services provided at an Outpatient Hospital are reported on the institutional claim type and are reimbursed as part of the hospital's EAPG payment. Institutional claim types do not have the POS code field.
- Rule allows for services to be rendered at a location of "Community". Since there is no exact POS code which aligns with this description, POS code 99 should be reported.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Eligible Providers
Organizations with a Tax ID must enroll as Provider Type 83 - Behavioral Therapy Clinic.
Eligible individuals to affiliate with Provider Type 83 are:
- Psychologist with a doctorate degree - Provider Type 37
- Licensed Behavioral Health Clinician - Provider Type 38
- Behavioral Therapist - Provider Type 84
Provider Types 37, 38 and 84 must be affiliated with Provider Type 83.
Providers who enrolled prior to 2019 and are currently Provider Type 25 must re-enroll as Provider Type 83 during the revalidation process. Providers may need to re-enroll as Provider Type 83 sooner if a Behavioral Therapist (Provider Type 84) is affiliating with the group.
Rendering and Billing Provider Numbers
PBT services must be billed using the 837 Professional (837P) transaction or CMS 1500 form, which requires using rendering and billing National Provider IDs (NPIs).
Each agency's specific billing number will be used to reimburse the provider.
Pediatric Behavioral Therapy Benefit Procedure Code Table
Allowable Procedure Coding
- 97153
- 97154
- 97155
- 97158
- 97151
- 97151 TJ
Prior Authorization Requests (PARs)
Independent therapists and therapy clinics must submit, and have approved, PARs for medically necessary services prior to rendering the services.
Prior Authorization Requests are approved for up to a six (6)-month period (depending on medical necessity determined by the authorizing agency).
- Incomplete, incorrect or insufficient member information on a PAR request form will not be accepted.
Submit PARs for the number of units for each specific procedure code requested, not for the number of services. Modifiers must be included on both the PAR and claim submission.
PAR Requests Must Include:
- Legibly written and signed ordering practitioner prescription or approved Plan of Care, to include:
- Diagnosis (preferably with ICD-10 code)
- Reason for therapy
- The number of requested therapy sessions per week
- Total duration of therapy
- The member's treatment history, including current assessment and treatment. Include duration of previous treatment and treating diagnosis if completed by the requesting provider.
- Current treatment diagnosis
- Course of treatment, measurable goals and reasonable expectation of completed treatment
- Documentation supporting medical necessity for the course and duration of treatment being requested
- Assessment or progress notes submitted for documentation, must not be more than 60 days prior to submission of PAR request.
- The billing provider name and address needs to be present in field #25 on the PAR.
- The authorizing agency reviews all completed PARs and approves or denies, by individual line item, each requested service or supply listed on the PAR. PAR status inquiries can be made through the Provider Web Portal and results are included in PAR letters. Read the results carefully as some line items may be approved and others denied. Do not render or bill for services until the PAR has been processed
- The claim must contain the PAR number for payment.
Approval of a PAR does not guarantee Health First Colorado payment and does not serve as a timely filing waiver. Prior authorization only assures that the service is considered a benefit of Health First Colorado. All claims, including those for prior authorized services, must meet eligibility and claim submission requirements (e.g., timely filing, third party resources payment pursued, required attachments included, etc.) before payment can be made.
Providers should direct inquiries to the authorizing agency, located on the Provider Contact web page, if the PAR is denied.
The Health First Colorado PAR forms are available on the Provider Forms web page or by contacting the ColoradoPAR Program.
Documentation of clinical Applied Behavior Analysis (ABA) services must meet Council of Autism Service Providers (CASP) minimum requirements. Templates can be found at: https://www.casproviders.org/access-the-templates
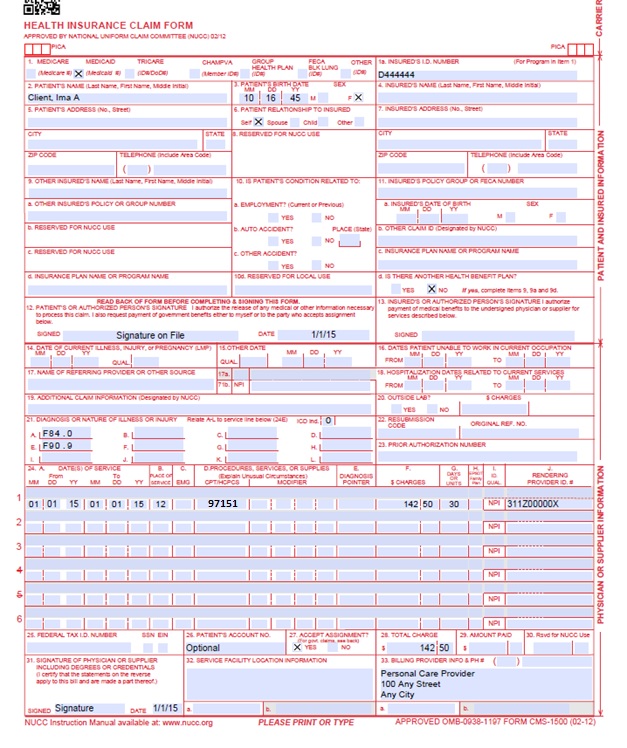
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456 | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014 Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Not Required | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | |||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Not Required | |||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070115 for July 1, 2015. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
EPSDT | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one (1) that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||
| 24D. | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. Anesthesia Services Anesthesia services must be reported as minutes. Units may only be reported for anesthesia services when the code description includes a time period. Anesthesia time begins when the anesthetist begins member preparation for induction in the operating room or an equivalent area and ends when the anesthetist is no longer in constant attendance. No additional benefit or additional units are added for emergency conditions or the member's physical status. The fiscal agent converts reported anesthesia time into fifteen minute units. Any fractional unit of service is rounded up to the next fifteen minute increment. Codes that define units as inclusive numbers Some services such as allergy testing define units by the number of services as an inclusive number, not as additional services. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early and Periodic Screening, Diagnosis, and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available- Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) Not Required | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016 Unacceptable signature alternatives: | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
Pediatric Behavioral Therapy Claim Example
Pediatric Behavioral Therapies Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 8/29/2016 | Added new code to code table | HCPF |
| 8/17/2017 | Added updated codes to table | HCPF |
| 10/16/2017 | Language Modification | HCPF |
| 6/25/2018 | Updated billing to point to general manual, removed PAR information (found on general manual) | HCPF |
| 6/28/2018 | Removed claim submission info that is found in general manual | HCPF |
| 8/3/2018 | Updated to new format, added co-treatment chart and language modification | HCPF |
| 1/4/2019 | Updated HCPC codes | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 01/21/2020 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 7/1/2021 | Removed outdated HCPF codes and removed rates from the manual | HCPF |
| 1/1/2023 | Updated General Benefit Policies, Covered Services and Prior Authorization Requests | HCPF |
| 8/1/2024 | Added POS 03 and deleted concurrent PAR language | HCPF |
| 8/12/2024 | Added Licensed Psychologist to referring provider type to better align with criteria and OPR requirements and language update for enrollment | HCPF |
| 12/02/2024 | Clarified school-based language, added EVV language and a link to documentation minimums | HCPF |