Doula Billing Manual
The doula benefit program is administered by the Colorado Department of Health Care Policy & Financing (the Department). This billing manual describes information regarding the benefit's programmatic components and billing requirements. The information in this manual is subject to change as the Department periodically modifies the doula benefit program’s benefits and services. The manual will be updated as new policies are implemented.
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for general information about Health First Colorado (Colorado's Medicaid program). The manual provides information about billing Health First Colorado, reimbursement policies, provider participation, eligibility requirements, and other useful information.
Table of Contents
- Program Overview
- Billing Information
- CMS 1500 Paper Claim Reference Table
- Timely Filing
- Doula Billing Manual Revision Log
Program Overview
On July 1, 2024, the Colorado Department of Health Care Policy and Financing (the Department) implemented a doula benefit for Health First Colorado members.
Rules and Regulations
The doula benefit is administered by the Department. Rules governing the program are outlined in the Code of Colorado Regulations 10 C.C.R. 2505-10 8.734. Providers are required to comply with all the rules and guidance provided by the Department and are encouraged to contact the Department's policy specialist with any questions. Contact HCPF_MaternalChildHealth@state.co.us. Updates to policy and guidance will be published in this manual. Providers will be given notice of updates through the Department’s monthly Provider Bulletin, and providers are responsible for subscribing and reviewing Provider Bulletins for changing policy.
The doula benefit is available to pregnant and postpartum people who are enrolled in Health First Colorado. The program gives eligible members access to doula care, including prenatal, labor and delivery, and postpartum support.
To be eligible for the program, a person must meet the following criteria:
- Be eligible for Health First Colorado
- Be pregnant or have given birth within the last 365 days
This benefit includes three (3) categories of services and is available to all eligible Health First Colorado members.
- Prenatal support
- Continuous labor and delivery support
- Postpartum support
The intent of this benefit is to leverage the community-based doula model that improves outcomes for pregnant people through continuous labor support with wraparound pre and postnatal care. This benefit is not a substitute for clinical obstetric care or behavioral health care with licensed providers. Additionally, while many doulas have other qualifications that may support pregnant and postpartum people, this does not include other support services for pregnant, laboring and postpartum people that would fall outside a doula’s scope—including but not limited to childbirth education, clinical or medical tasks, lactation services, massage therapy or infant sleep support.
Visit the Reproductive and Maternal Health Programs and Resources web page for more information on the doula benefit.
Contact HCPF_MaternalChildHealth@state.co.us with questions.
Provider Enrollment and Participation
Providers must be enrolled as a Health First Colorado (Colorado's Medicaid program) provider to:
- Provide care to a Health First Colorado member, and to
- Submit claims for payment to Health First Colorado
Visit the Provider Enrollment web page if interested in becoming a Health First Colorado provider. Training on doula program enrollment can be found at the Department’s Doula web page under doula enrollment training.
Eligible Rendering Providers
Doula support services may only be provided by individuals who meet the qualifications of either the:
- Certification Pathway, or the
- Experience Pathway
The following enrolled provider types (PT) may provide doula support services:
- Doula - PT 79
- IBCLC – PT 70
- CLC or CLE – PT 71
Doula benefit program providers must be enrolled in Health First Colorado under the doula provider type (PT 79) or enrolled as a lactation support service provider type (PT 70 or PT 71).
Guidance for Doula Providers adding Lactation Services
Enrolled Doula providers who meet IBCLC, CLC or CLE qualifications per 10 C.C.R. 2505-10 8.732.9 may provide lactation support without separate PT 70 or 71 enrollment.
Enrolled doula providers are required to submit a copy of their current certification through the Provider Web Portal as one of the following:
- Certified International Board-Certified Lactation Consultant (IBCLC) with current certification by the International Board of Lactation Consultant Examiners (IBLCE)
- Certified Lactation Counselor (CLC) with current certification by the Academy of Lactation Policy and Practice, Inc. (ALPP)
- Certified Lactation Educator (CLE) with current certification by the Childbirth and Postpartum Professional Association (CAPPA)
Doula providers are required to submit a copy of their current lactation certification and must receive verification that the submission was approved prior to rendering or billing for lactation support services. This verification process ensures compliance with program standards and protects continued access to reimbursement. Providers who do not complete this step will be subject to enforcement actions in accordance with Section 25.5-4-301, C.R.S., and 10 C.C.R. 2505-10, Section 8.076.
Supervision Requirements
Doulas providing lactation services must follow guidance outlined in the Lactation Billing Manual.
Certified Lactation Counselors (CLCs) with current certification by the Academy of Lactation Policy and Practice, Inc. (ALPP) and Certified Lactation Educators (CLEs) with current certification by the Childbirth and Postpartum Professional Association (CAPPA) may only provide lactation support services under the general supervision of enrolled:
Physicians (MDs) – PT 05/65
Osteopaths (DOs) – PT 26
Physician Assistants (PAs) – PT 39
Advanced Practice Nurses (APNs) - PT 41
Certified Nurse Midwives (CNMs) – PT 22
International-Board Certified Lactation Consultants (IBCLCs) – PT 70
Eligible Billing Providers
The only group provider types that may bill for doula services are Clinic (PT 16), Non-physician Practitioner Group (PT 25), and Lactation/Doula Professional Group (PT 72).
When claims are submitted using this billing provider type, the rendering provider on the claim must be that of the provider who themselves rendered the service. The rendering provider must be formally affiliated with the group in order for the claim to be processed.
Lactation/Doula Professional Group (PT 72) is a group practice consisting of any of the following professionals who are enrolled with the Department as approved providers:
- International Board-Certified Lactation Consultant
- Certified Lactation Counselor
- Certified Lactation Educator
- Doula
This billing provider type 72 must have at least one (1) IBCLC or doula affiliated with the group. It is used as a billing provider type for a group practice of lactation support service providers and/or doulas.
Recommendation for Doula Services
Doula support services are provided as preventive services and require an electronic or written recommendation by a physician or other licensed practitioner of the healing arts acting within their scope of practice in accordance with 42 CFR 440.130(c).
Providers must maintain the record of a licensed provider’s recommendation for each member before initiating doula support services, storing the record in a manner consistent with HIPAA requirements. All claims for doula support services must have the NPI number of the enrolled provider who ordered/recommended the doula support service to be indicated on the claim. This field is labeled "Referring Provider" in the Provider Web Portal. The enrolled provider types who may recommend these services are:
- Physicians (PT 05, 65)
- Osteopaths (PT 26)
- Physician Assistants (PT 39)
- Advanced Practice Nurses (PT 41)
- Nurse Midwife (PT 22)
- Certified Professional Midwives/Direct Entry Midwife (PT 69)
- Certified Midwife (PT 80)
- Licensed Psychologist (PT 37)
- Licensed Behavioral Health Clinician (PT 38)
- Non-Physician Practitioner-Individual (PT 24)
The recommending provider indicated on the claim must be actively enrolled with Health First Colorado (42 CFR 455.410(b)). If the indicated provider is not actively enrolled the claim will be denied. Reference the Ordering, Prescribing, and Referring Claim Project Identifier for further details.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for general billing information.
Third-Party Liability (TPL)
The term Third-Party Liability (TPL) describes circumstances when a Health First Colorado member has health insurance or other potential resources - in addition to the Health First Colorado program - that may pay for medical services.
An estimated 10% of Health First Colorado members have other health insurance resources available to pay for medical expenses.
While most benefits require a process by which Medicaid would be the payer of last resort because Federal regulations require that all available health insurance benefits be used before Health First Colorado considers payment, Third Party Liability (TPL) edits will be automatically bypassed for both commercial insurance and Medicare when claims are submitted by the following provider types:
- PT 70 - Lactation Consultant
- PT 72 - Lactation/Doula Professional Group
- PT 79 - Doula
For more information on TPL, please visit the general provider billing manual section that discusses these rules in greater depth.
Covered Doula Services
Doula services are billed using two (2) Healthcare Common Procedure Coding System (HCPCS) procedure codes, two (2) International Classification of Diseases (ICD)-10 diagnosis codes, and a combination of modifier codes if services are delivered via telemedicine. The modifier codes shown below should only be used in circumstances involving telemedicine.
Covered services are limited to 180 minutes of prenatal care and 180 minutes of postpartum care per member, and one instance of labor and delivery per member pregnancy during a 12-month period regardless of the number of doula providers who treat that member.
A member or doula cannot distribute that amount differently, and those services are maxed out to the member. For example, if one (1) doula is reimbursed for one (1) 60-minute visit and one (1) 90-minute visit during the prenatal period, a second doula can only be reimbursed for the remaining 30 minutes (two (2) units of service) for that same member.
Should a doula identify a need beyond these additional approved services they may reach out to the member’s Regional Accountable Entity for care coordination.
Prenatal Doula Services: A doula can be reimbursed for up to 180 minutes of prenatal care per member for HCPCS Procedure Code T1032. There is a limit of 12 units of service per member during a 12-month period (period starts at the time of the first doula claim).
Postpartum Doula Services: A doula can be reimbursed for up to 180 minutes of postpartum care for HCPCS Procedure Code T1032. There is a limit of 12 units of service per member during a 12-month period (period starts at the time of the first doula claim).
Labor and Delivery: A doula may be reimbursed for labor and delivery support services once per member within a 12-month period. Reimbursement is billed under HCPCS Procedure Code T1033, regardless of the length of the labor and delivery. The doula and member should discuss expectations and processes should the labor and delivery exceed the time that the doula is able to assist.
Per the HCPF General Provider Billing Manual guidance, providers are advised to bill their usual and customary charges. Refer to the current Health First Colorado Fee Schedule for rates.
Coding Table for Doula Services
| Procedure Code | Description (short) | Required ICD-10 Diagnosis Codes | Limitations per 12-month period |
| T1032 | Doula birth worker services, billed per 15 minutes. Used for prenatal and postpartum services.
This is a ‘timed’ code. 1 unit of service = 15 minutes of direct member contact services provided. Instructions for rounding increments are found below.
Telemedicine service delivery is allowed. | Prenatal Services: Z33.1
Postpartum Services: Z39.2 | 12 units of service (180 minutes) covered per member pregnancy for Prenatal services,
and
12 units of service (180 minutes) covered per member pregnancy for Postpartum services |
| T1033 | Doula birth worker services, per delivery. Used for labor and delivery services.
This is an ‘untimed’ code. 1 unit of service = all doula services provided during a member’s labor & delivery. This code is only to be reported once per member, per delivery.
Telemedicine service delivery is not allowed. | Z33.1 | 1 unit of service covered per member pregnancy |
| Modifier Codes for Telemedicine Service Delivery for T1032 Only | Description |
| FQ | The service was furnished using audio-only communication technology. |
| FR | The supervising practitioner was present through two-way, audio/video communication technology.
|
| 93 | Synchronous Telemedicine Service Rendered Via Telephone or Other Real-Time Interactive -Audio-Only Telecommunications System
|
| 95 | Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunications System
|
Reporting Units of Service
A. Timed and Untimed Codes
When reporting service units for CPT/HCPCS codes where the procedure is not defined by a specific timeframe ("untimed" CPT/HCPCS), the provider enters "1" in the field labeled "units." For untimed codes, units are reported based on the number of times the procedure is performed, as described in the CPT/HCPCS code definition.
Example 1: A member received doula birth worker services related to a delivery, represented by HCPCS "untimed" code T1033. Regardless of the number of minutes spent providing this service, only one (1) unit of service is appropriately billed.
HCPCS code T1032 specifies that the direct (one-on-one) time spent in patient contact is 15 minutes. Providers report these "timed" procedure codes for services delivered on any single calendar day using HCPCS codes and the appropriate number of 15-minute units of service.
Example 2: A member received a total of 60 minutes of prenatal doula birth worker services codes using HCPCS "timed" code T1032 which is defined in 15-minute units, on a given date of service. The provider would then report four (4) units of code T1032.
B. Counting Minutes for Times Codes in 15-Minute Units
When only one (1) service is provided in a day, providers should not bill for services performed for less than eight (8) minutes. For any single timed HCPCS code in the same day measured in 15-minute units, providers bill a single 15-minute unit for treatment greater than or equal to eight (8) minutes through and including 22 minutes. If the duration of a single modality or procedure in a day is greater than or equal to 23 minutes, through and including 37 minutes, then two (2) units should be billed. Time intervals for one (1) through eight (8) units are as follows:
| Billed Units Increment | Time Spent in Direct Patient Contact |
| 1 unit of service | 8 minutes through 22 minutes |
| 2 units of service | 23 minutes through 37 minutes |
| 3 units of service | 38 minutes through 52 minutes |
| 4 units of service | 53 minutes through 67 minutes |
| 5 units of service | 68 minutes through 82 minutes |
| 6 units of service | 83 minutes through 97 minutes |
| 7 units of service | 98 minutes through 112 minutes |
| 8 units of service | 113 minutes through 127 minutes |
The pattern remains the same for treatment times in excess of two (2) hours.
Example 3: A member received a total of 105 minutes of prenatal doula birth worker services codes using HCPCS "timed" code T1032 which is defined in 15-minute units, on a given date of service. The provider would then report seven (7) units of code T1032.
The provider must maintain documentation in accordance with 10 CCR 2505-10 8.130.2. that complies with state and federal regulations. The doula should be able to quickly identify and share information about each visit, including timestamps for the duration of each visit providing direct service to an eligible member. This is used to validate the number of units of service billed for reimbursement.
Physical Health Managed Care
Doula services are not included in Health First Colorado physical health managed care plans, however doula services are still covered benefits for members enrolled in those plans. All claims for doula services should be billed to the Department’s Fiscal Agent, Gainwell Technologies, even if the member is attributed to a Health First Colorado physical health managed care plan.
Place of Service
Doulas can provide prenatal and postpartum care in variety of settings, including the member’s home, clinics and provider offices, community-based settings or via telehealth. A full list of allowable places of service for doula services are indicated below.
Labor and delivery services (T1033) cannot be provided via telemedicine with Place of Service codes 02 or 10. While doulas must provide in-person labor and delivery support, location can vary.
Official descriptors of the Place of Service can be found on the CMS website.
| Allowed Place of Service Code | Description (short) |
| 02 | Telehealth Provided Other than in Patient’s Home |
| 03 | School |
| 04 | Homeless Shelter |
| 05 | Indian Health Service Free-standing facility |
| 06 | Indian Health Service Provider based facility |
| 08 | Tribal 638 Provider-based Facility |
| 09 | Prison/ Correctional Facility |
| 10 | Telehealth Provided in Patient’s Home |
| 11 | Office |
| 12 | Home |
| 19 | Off Campus-Outpatient Hospital |
| 20 | Urgent Care Facility |
| 21 | Inpatient Hospital |
| 22 | On Campus-Outpatient Hospital |
| 23 | Emergency Room |
| 25 | Birthing Center |
| 50 | Federally Qualified Health Center |
| 53 | Community Mental Health Center |
| 55 | Residential Substance Abuse Treatment Facility |
| 57 | Non-residential Substance Abuse Treatment Facility |
| 71 | Public Health Clinic |
| 72 | Rural Health Clinic |
Contact Information
Contact the Provider Services Call Center with billing inquiries.
Contact the Department's Doula Benefit policy specialist at hcpf_maternalchildhealth@state.co.us for all other inquiries.
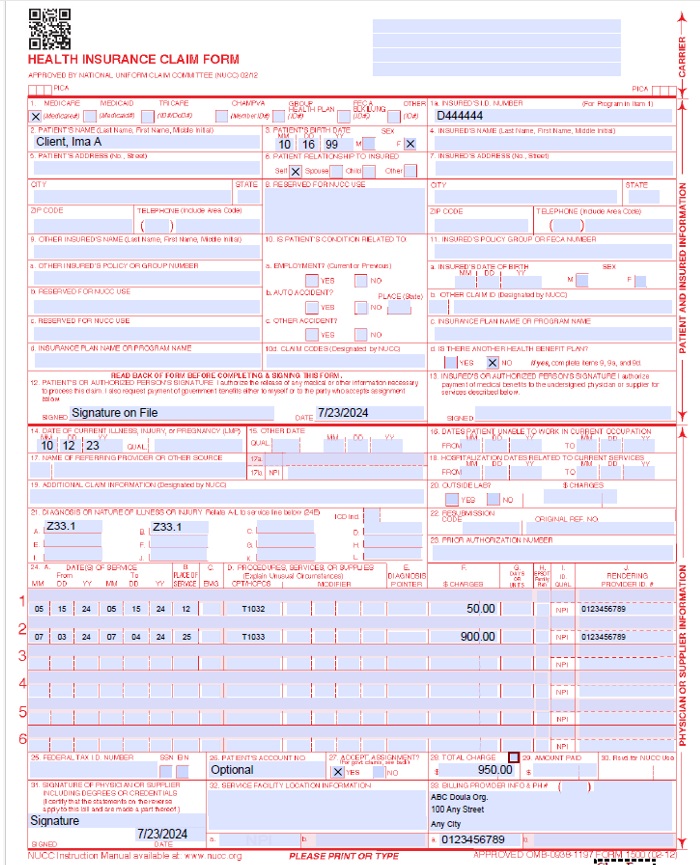
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number & Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven (7)-digit Health First Colorado ID number as it appears on the Medicaid Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||
| 17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 code: Z33.1 or Z39.2 depending on the procedure code billed. | ||||||||||||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left-hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | Prior Authorization Enter the six (6)-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. | ||||||||||||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019.
| ||||||||||||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. | ||||||||||||||||||||||||||||||||||||||||||||||
24D.Procedures, Services, or Supplies
| Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. Either T1032 or T1033. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four modifiers may be entered when using the paper claim form.
95 - Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunications System | ||||||||||||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado-covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early & Periodic Screening, Diagnosis, and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available- Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) If the service is Family Planning, such as for contraception or sterilization, enter "Y" for YES or "N" for NO in the bottom, unshaded area of the field. | ||||||||||||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado doula provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two digits for the year. Example: 070116 for July 1, 2016. Unacceptable signature alternatives: Claim preparation personnel may not sign the enrolled provider's name. Initials are not acceptable as a signature. Typed or computer printed names are not acceptable as a signature. "Signature on file" notation is not acceptable in place of an authorized signature. | ||||||||||||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||||||||||||
CMS 1500 Doula Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Doula Billing Manual Revision Log
Revision Date | Addition/Changes | Made by |
|---|---|---|
| 8/9/2024 | Creation of Manual | HCPF |
| 12/17/2024 | Added OPR policy information; added information for Doula services provided by a dually- qualified IBCLC, CLC, CLE; added information about group billing including PT 72. | HCPF |
| 8/21/2025 | Added Third Party Liability (TPL) edits update for PT 72 and PT 79. Added Rendering Providers | HCPF |
| 10/22/2025 | Added Guidance for doula providers about lactation services and link to fee schedule. | HCPF |
| 11/17/2025 | Added Guidance for Lactation Supervision Requirements | HCPF |
| 2/9/2026 | Updated list of OPR providers | HCPF |