Children's Habilitation Residential Program (CHRP) Waiver Program Billing Manual
- Overview
- Prior Authorization Requests (PARs)
- PAR Submission
- Claim Submission
- Children's Habilitation Residential Program (CHRP)
- Denver Regional Pricing
- Children's Habilitation Residential Program (CHRP) Standard Procedure Code Table – Outside Denver
- Paper Claim Reference Table
- CMS 1500 CHRP Claim Example
- Timely Filing
- HCBS CHRP Manual Revisions Log
Return to Billing Manuals Web Page
Overview
Home and Community-Based Services (HCBS) are certain Health First Colorado (Colorado's Medicaid program) benefits available to Members in their homes and communities as an alternative to institutional care. HCBS programs for persons with developmental disabilities include the Children's Habilitation Residential Program (HCBS-CHRP).
Waiver programs provide additional Health First Colorado benefits to specific populations who meet special eligibility criteria.
Level of care determinations are made annually by the Case Management Agencies serving each of the 20 Designated Service Areas statewide. Members must meet financial, medical, and program criteria to access services under a waiver. The applicant must be at risk of placement in a nursing facility, hospital, or ICF/IID (intermediate care facility for Individuals with Intellectual Disabilities). To use waiver benefits, Members must be willing to receive services in their homes or communities. A Member who receives services through a waiver is also eligible for all basic Health First Colorado covered services except nursing facility and long-term hospital care.
Applicants may apply for more than one (1) waiver but may only receive services through one (1) waiver at a time.
Prior Authorization Requests (PARs)
All HCBS services require prior authorization before they can be reimbursed by Health First Colorado. Case Managers at one (1) of the 20 CMAs complete the Prior Authorization Requests for their specific programs according to instructions published in the regulations for the Department of Health Care Policy & Financing (the Department).
The CMA's responsibilities include, but are not limited to:
- Informing Members and/or legal guardian of the eligibility process
- Submitting evidence of Member eligibility for the waiver to the county Department of Human/Social Services for a Health First Colorado Member identification number
- Developing the appropriate Prior Authorization Request of services and projected costs for approval
- As the authorizing agent, submitting the prior authorization information to the fiscal agent. Refer to Appendix D located on the Billing Manuals web page under the Appendices drop-down for a list of authorizing agents.
- Assessing the Member's health and social needs.
- Arranging for face-to-face contact with the Member within 30 calendar days of receipt of the referral
- Monitoring and evaluating services
- Reassessing each Member
- Demonstrating continued cost-effectiveness whenever services increase or decrease
Approval of prior authorization does not guarantee payment and does not serve as a timely filing waiver. Prior authorization only assures that the approved service is a medical necessity and is considered a benefit of Health First Colorado. All claims, including those for prior authorized services, must meet eligibility and claim submission requirements (e.g., timely filing, Provider Agency information completed appropriately, required attachments included, etc.) before payment can be made.
Prior approvals must be completed thoroughly and accurately. If an error is noted on an approved request, it should be brought to the attention of the Member's Case Manager for corrections. Procedure codes, quantities, etc., may be changed or entered by the Member's Case Manager.
The authorizing CMA is responsible for timely submission and distribution of copies of approvals to Provider Agencies.
PAR Submission
The HCBS-CHRP Pars are electronically submitted by Case Managers via the Bridge, which directly interfaces with the Colorado interChange. Case Managers can access the Bridge via the Medicaid Enterprise User Provisioning System (MEUPS). Provider Agencies are not afforded access to the Bridge, but may obtain PAR information from Case Managers, the Provider Services Call Center, or through the Provider Web Portal.
Claim Submission
Submission of claims for services rendered must not be duplicative. Duplicate claims are any claims paid across more than one (1) claim number for the same beneficiary, date, procedure code and service state by the same Provider Agency. Duplicate claims can include different procedure codes but with overlapping service definitions. Duplicate claims also include a single Provider Agency offering more than one (1) service simultaneously. All overlapping services rendered and subsequent billing claims must have supporting documentation that clearly identifies the necessity and non-duplication of overlapping services to verify these services were provided separately and independently of one another.
Refer to the service definitions on the Colorado Code of Regulations website to identify if claims are duplicative. Refer to the provider specialty code enrollment requirements on the HCBS Provider Specialty Code List web page to identify services that must be provided by an individual Provider Agency.
In any instance in which duplicate billings result in Medicaid reimbursement, a recovery shall be made by the Department against the Provider Agency.
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Children's Habilitation Residential Program (CHRP)
- HCBS-CHRP is a residential service and support program for children and youth from birth through age 20. HCBS-CHRP provides services for children and youth who have an intellectual or developmental disability and extraordinary needs that put them in at risk of, or in need of, out-of-home placement in a nursing facility, hospital, or ICF/IID.
The waiver provides support for eligible children who:
- May require added support as they transition back to the family home from a foster care or residential setting.
- May require services to support their families in remaining in the family home.
- Have an intellectual or developmental disability or developmental delay if under age five (5) and have intensive behavioral and/or medical support needs that put them at risk or in need of out-of-home placement.
- Are willing to receive services in their homes or communities.
The waiver is designed to assist children/youth to acquire, retain, and/or improve self-help, socialization, and adaptive skills necessary to live in the community with a plan to include services. Enrollment into the HCBS-CHRP waiver occurs through area Case Management Agencies.
The following services are provided through CHRP when deemed appropriate and adequate by the child/youth's physician and they are to be provided in the community, as available:
- Community Connector
- Habilitation (Residential 24-hour support)
- Respite
- Hippotherapy
- Massage Therapy
- Movement Therapy
- Child and Youth Mentorship
- Wraparound Services
Denver Regional Pricing
Certain HCBS delivered to members while they are within the City and County of Denver are eligible for higher rates. Information relative to these services, and guidance on the applicability of these rates to certain services, can be found in the Denver Minimum Wage Pricing Appendix, on the Department’s billing manual page under “HCBS”.
Children's Habilitation Residential Program (CHRP) Standard Procedure Code Table – Outside Denver
Providers may bill the following procedure codes for CHRP services:
| Description | Procedure Code | Modifiers | Unit Designation |
|---|---|---|---|
| Specialty 883: Community Connector | |||
| Community Connector | H2021 | U9 | 15 Minutes |
| Community Connector Parental Provision (service will begin transitioning off the waiver on 7/1/2025) | H2021 | U9, HA | 15 Minutes |
| Specialty 884: Foster Home | |||
| Foster Home Level 1 | H0041 | U9 | Day |
| Foster Home Level 2 | H0041 | U9, 22 | Day |
| Foster Home Level 3 | H0041 | U9, TF | Day |
| Foster Home Level 4 | H0041 | U9, TF, 22 | Day |
| Foster Home Level 5 | H0041 | U9, TG | Day |
| Foster Home Level 6 | H0041 | U9, TG, 22 | Day |
| Foster Home Level 7 | H0041 | U9, HA, TG, HK | Day |
| Specialty 884: Habilitation - Group Home | |||
| Group Home Level 1 | T2016 | U9 | Day |
| Group Home Level 2 | T2016 | U9, 22 | Day |
| Group Home Level 3 | T2016 | U9, TF | Day |
| Group Home Level 4 | T2016 | U9, TF, 22 | Day |
| Group Home Level 5 | T2016 | U9, TG | Day |
| Group Home Level 6 | T2016 | U9, TG, 22 | Day |
| Group Home Level 7 | T2016 | U9, HA, TT, TG | Day |
| Specialty 884: Residential Child Care Facility | |||
| Residential Child Care Facility Level 1 (Per Diem) | T2016 | U9, HA | Day |
| Residential Child Care Facility Level 2 (Per Diem) | T2016 | U9, HA, TJ | Day |
| Residential Child Care Facility Level 3 (Per Diem) | T2016 | U9, HA, TF | Day |
| Residential Child Care Facility Level 4 (Per Diem) | T2016 | U9, HA, TG | Day |
| Residential Child Care Facility Level 5 (Per Diem) | T2016 | U9, HA, TT | Day |
| Residential Child Care Facility Level 6 (Per Diem) | T2016 | U9, HA, 22 | Day |
Specialty 741: Hippotherapy Services removed from the CHRP waiver effective July 1, 2024. Refer to the Physical and Occupational Therapy Billing Manual or Speech Therapy Billing Manual for State Plan Hippotherapy. | |||
| Specialty 743: Movement Therapy | |||
| Movement Therapy-Bachelors | G0176 | U9 | 15 Minutes |
| Movement Therapy-Masters | G0176 | U9,22 | 15 Minutes |
| Specialty 742: Massage Therapy | |||
| Massage Therapy | 97124 | U9 | 15 Minutes |
| Specialty 885: Respite | |||
| Respite - in the Family Home | S5150 | U9, HA | 15 Minutes |
| Respite - in the Family Home/Per Diem | S5151 | U9, HA | 15 Minutes |
| Specialty 885: Respite - Residential Settings | |||
| Respite - in the Family Home | S5150 | U9, HI | 15 Minutes |
| Respite - in the Family Home | S5151 | U9, HI | Day |
| Specialties 885 and 676: Unskilled Respite | |||
| Unskilled Group Respite, Unit | S5150 | U9, HQ | 15 Minutes |
| Unskilled Group Respite, Day | S5151 | U9, TJ | Day |
| Specialty 615: Skilled Respite | |||
| Skilled CNA (4 hours or less) | T1005 | U9 | 15 Minutes |
| Skilled RN, LPN (4 hours or less) | T1005 | U9, TD | 15 Minutes |
| Skilled CNA (4 hours or more) | S9125 | U9 | Day |
| Skilled RN, LPN (4 hours or more) | S9125 | U9, TD | Day |
| Specialty 882: CHRP Youth Mentorship-CES/CHRP Therapeutic Respite | |||
| Skilled Therapeutic (4 hours or less) | T1005 | U9, HA | 15 Minutes |
| Skilled Therapeutic (4 hours or more) | S9125 | U9, HA | Day |
| Child and Youth Mentorship (formerly “In Home Services”) | H2021 | U9, HA, HM | 15 Minutes |
| Specialty 886: Wraparound | |||
| Same code may be billed for either Transition or Intensive Support Services | |||
| Wraparound Plan | H2021 | U9, HA, TL | 15 Minutes |
| Prevention and Monitoring | H2021 | U9, HA, HN | 15 Minutes |
| Specialty 683: Wellness Education Benefit | |||
| Wellness Education Benefit | 98960 | U9 | 1 unit per month |
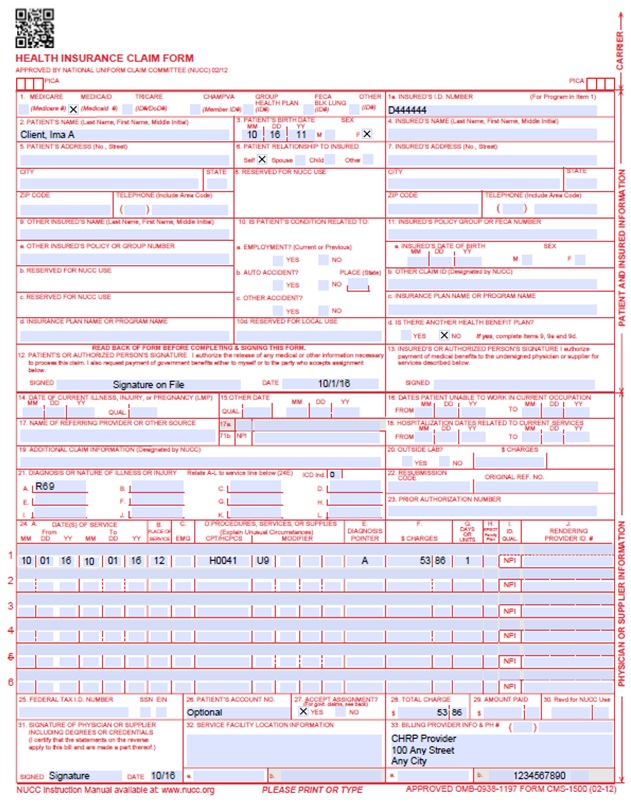
Paper Claim Reference Table
The following paper form reference table gives required and/or conditional fields for the paper CMS 1500 claim form for CHRP claims:
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven (7)-digit ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Not required | |||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Not Required | |||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Not Required | |||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | |||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Not Required | |||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||||||||||||||||||||||||||
| 15. Other Date | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. HCBS CHRP may use R69 | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | HCBS Leave Blank | ||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010116 for January 1, 2016.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
Note: Use POS Code 12 (Home) for Foster Home, Group Home and Respite. Use ether POS 11 (Office) or POS 11 (Home) where applicable for all other services. | ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not Required | |||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. Refer to the CHRP Rate Schedules located on the Rates and Fee Schedule web page. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Required | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. Refer to the CHRP Rate Schedules located on the Rates and Fee Schedule web page. | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | General Instructions | A unit represents the number of times the described procedure or service was rendered. Except as instructed in this manual or in Health First Colorado bulletins, the billed unit must correspond to procedure code descriptions. The following examples show the relationship between the procedure description and the entry of units. Home and Community-Based Services Combine units of services for a single procedure code for the billed time period on one (1) detail line. Dates of service do not have to be reported separately. Example: If 40 units of personal care services were provided on various days throughout the month of January, bill the personal care procedure code with a From Date of 01/03/XX and a To Date of 01/31/XX and 40 units. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Not Required | |||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Not Required | |||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Conditional | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
CMS 1500 CHRP Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
HCBS CHRP Manual Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates are based on Colorado iC Stage II Provider Billing Manuals Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 6/26/2018 | Updated billing and timely | HCPF |
| 6/28/2018 | Removed HCPCS (duplicated from general) | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/19/2019 | Clarification to signature requirements | HCPF |
| 7/15/2019 | Updated new services, removed Special Program Code references, clarified CCB responsibility, removed outdated services. | HCPF |
| 3/3/2020 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the Paper Claim Reference Table | HCPF |
| 10/2/2020 | Updated language describing CHRP services and eligibility, Changed Supported Community Connections to Community Connector, corrected errors in the Respite modifiers, Place of Service instructions. | HCPF |
| 11/18/2020 | Added in the new RCCF benefit effective 01/01/21 | HCPF |
| 11/4/2022 | Added specialties | HCPF |
| 4/3/2023 | Updated AWS URL Links | HCPF |
| 6/26/2023 | Added Specialty Numbers, adjusted where “Intensive Support Services” is listed in the manual. | HCPF |
| 7/1/2023 | Added Level 7 Foster Home/Group Home, adjusted the position of certain services within the billing manual. | HCPF |
| 12/20/2023 | Added Community Connector Parental Provision | HCPF |
| 2/12/2024 | Added Respite Additional Services and updated Wraparound Services | HCPF |
| 4/25/2024 | Added new Denver County codes and completed corrections | HCPF |
| 5/9/2024 | Corrected H1 to HA on Wraparound Services | HCPF |
| 7/19/2024 | Added duplicative claims language to Claims submission, removed Hippotherapy codes and added link to PT/OT billing manual | HCPF |
| 12/8/2024 | Updated manual to reflect updated policy and added/modified procedure codes as a result of the implementation of the Denver Regional Pricing procedure code/modifiers; added references to new Denver Regional Pricing Billing Appendix. Deleted antiquated references to Community Centered Boards/updated language to reflect contracts with Case Management Agencies relative to Case Management Redesign. | HCPF |
| 04/02/2025 | Added Wellness Education Benefit. | HCPF |
| 10/22/2025 | Added note to Community Connector Parental Provision service code. | HCPF |
| 12/05/2025 | Added Unskilled Group Respite services. | HCPF |