May 2022
Project Category: Strengthen Case Management Redesign
The transformation of Colorado’s case management system is underway, requiring a complete reorganization of a decades-old system. As the case management system adapts and transforms, the Department is focusing on ways it can support case management agencies for the upcoming changes and growing pains that may come along with them. To assist with expected organizational and system changes, the Department is assisting agencies in a number of ways with ARPA funding such as capacity-building funds, change management expertise, and evolving systems of support for agencies, members, and their families.
What is Case Management Redesign?
Case Management Redesign refers to several initiatives that will help make accessing long-term services and supports (LTSS) easier by changing case management agencies to serve all Home and Community-Based Service (HCBS) waivers so people have one place to go. The redesign process will also ensure that there are the right number of case management agencies in Colorado to meet demand and will focus on increasing the quality of case management services.
Why is Case Management Redesign happening?
Single Entry Points (SEPs), Community Centered Boards (CCBs), and private Case Management Agencies currently provide case management for individuals with disabilities who participate in the Colorado Department of Health Care Policy & Financing’s (the Department) 10 HCBS waiver programs. Each agency type serves different waiver programs, creating silos.
In addition to case management services, many Case Management Agencies (CMAs) also provide direct services to program recipients, creating a conflict of interest that is no longer allowable by the Centers for Medicare and Medicaid Services (CMS). This federal requirement to separate case management and direct services is called Conflict-Free Case Management.
Individuals who are seeking or receiving LTSS often qualify for multiple programs and end up navigating between systems that are divided by program, making the system difficult for members.
Case Management Redesign is intended to simplify access and remove silos so members can more easily navigate and find the right programs and services that work for them. It will require one case management agency to provide case management services for all waiver programs in each region (or “catchment area”). This change will also create consistency in the quality, accountability and stability of the case management services people receive across the state. It will allow the Department to provide oversight and support to ensure a high-performing case management system statewide.
These changes will also meet the federal Conflict-Free Case Management requirement and allow the Department to ensure quality case management services for members across the state.
Why is Case Management Redesign happening NOW?
In 2014, CMS, the Department’s federal partner, released the “HCBS Settings Final Rule.” It included many requirements for providers to make changes to their processes to increase person-centeredness.
This rule also included a requirement for case management agencies to be “conflict free,” which means that they cannot provide services to the same person they are providing case management services to. Colorado risks losing 50% of the budget for HCBS (federal funding) if we do not come into compliance with Conflict-Free Case Management by July 1, 2024. This would mean less people in Colorado being able to access these vital services in the future.
Additionally, Colorado’s population is changing. The state has the second fastest aging population in the country and with individuals living longer, many have multiple chronic conditions that make their needs more complex. To meet the needs of the changing demands of members, it is critical that the system be modernized.
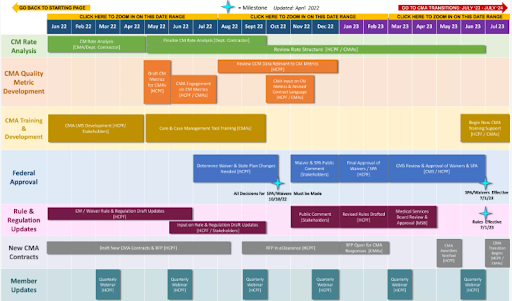
What is the timeline for Case Management Redesign?
Case Management Redesign work is already underway. We hope that you can join us in this effort! The work is projected to continue until July 2024 when the newly designed system will be in place. You can view a fully interactive timeline of the project, including all the various components, on the Case Management Redesign website.
Will members still have a choice of case management agency?
Members will receive case management services from the agency that holds the contract in their catchment area except for in cases where both the individual and agency agree to other terms.
If a person wants to be served by another agency in an adjacent catchment area, if both the individual and the agency agree, this will be allowable.
How is the Department specifically helping CMAs to prepare for this large system change?
Through ARPA funding, the Department is supporting CMAs in a number of ways to ensure that they are prepared for the change that lies ahead.
Capacity Building:
Beginning in April 2022, training and educational sessions were launched, focusing on key topic areas relevant to the project of Case Management Redesign.
The first session in April focused on Change Management. The next session in May focused on grant writing.
In conjunction with the educational sessions, a Culture Change Series started in May. This three-part series is designed to listen and learn from the people whose lives are most affected by case management services.
Part 1 of this three-part series, centered on listening and learning directly from people with disabilities and their advocates, who provided their insights and talked about what CMAs will need to know about working with people with disabilities. The presentation and recording for Part 1 are posted on the CMRD webpage.
Part 2 will take place on June 7 and focus on learning from Older Adults. Information about the meeting is on the CMRD webpage.
Finally, Part 3 of the series, titled Balancing Equity and Unique Needs, will take place on July 26. It will feature national experts in person-centered thinking and equitable approaches to working with different populations. Information about the meeting is on the CMRD webpage.
Rates:
The Department has prioritized evaluating and identifying best practices in case management and developing a proposed rate structure for case management activities and services including tiered rates for supporting members with complex care needs.
Since the project began in October 2021, case management agencies have been completing a comprehensive case management activity time analysis until June 2, 2022. This valuable work will further the evaluation of Colorado’s case management rates.
Best Practices:
Focusing on people who have long-term disabilities and those with comorbidities, this project is conducting a system mapping to further define roles and responsibilities across systems to support individuals through holistic care management and identifying training/support needs for implementation.
Case Management Agency Training Program:
In order to ensure CMAs are prepared for the future system, The Department is developing and implementing comprehensive training for case management agencies to improve quality and consistency statewide. The training program will be for CMAs, Regional Accountable Entities (RAEs), and Managed Care Organizations (MCOs) for all waiver programs and services, as well as behavioral health services, State Plan benefits, benefits counseling, and Community First Choice (CFC). All the training will be incorporated into a Learning Management System (LMS) allowing the Department to assign and monitor training completion.
The Department is currently undergoing an internal analysis of existing case management training materials to build a new training structure that will be available for case managers through the new LMS. Key foundational training materials are being developed at this time.
Long-term Care Eligibility Process Improvements
This project will work with stakeholders to identify solutions to barriers to long-term care eligibility, both from a physical eligibility and a financial eligibility perspective. Any changes will result in the need for system enhancements as well as training for counties, Medical Assistance sites, and case managers on eligibility requirements for waiver programs and other long-term care programs. Recruiting for the Department staff associated with this project is in process.