Screening, Brief Intervention and Referral to Treatment (SBIRT) Program
- Program Overview
- General Billing Information
- Key Clinical Definitions
- Member Eligibility
- Eligible Providers
- SBIRT Billing Information
- Procedure Code Overview
- National Correct Coding Initiative (NCCI) Edits for SBIRT
- Screening and Brief Intervention Procedure Codes
- Negative Screening Result Procedure Code
- Diagnosis Codes
- Allowable Place of Service Codes
- Emergency Department
- Federally Qualified Health Centers (FQHCs) / Rural Health Clinics (RHC)
- Additional Policies
- Member Benefit Limitations
- CMS 1500 SBIRT Paper Claim Reference Table
- Resources
- Timely Filing
- SBIRT Revisions Log
Return to Billing Manuals Web Page
Program Overview
Health First Colorado only reimburses providers for medically necessary services furnished to eligible members.
The purpose of this billing manual is to provide policy and billing guidance to providers to obtain reimbursement for SBIRT services. This manual is updated periodically to reflect changes in policy and regulations.
Screening, Brief Intervention and Referral to Treatment is designed to prevent members from developing a substance use disorder, for early detection of a suspected substance use disorder, or to refer members for treatment. These services are not intended to treat members already diagnosed with a substance use disorder or those members already receiving substance use disorder treatment services. Members who are pregnant may be eligible for additional substance use screening and intervention services through Special Connections, Outpatient Substance Use Disorder treatment and the Prenatal Plus program.
Treatment referrals must be made to the member's Regional Accountable Entity (RAE). Visit the Health First Colorado Regional Organizations web page for contact information and further details.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Key Clinical Definitions
Pre-Screen (aka Brief Screen)
A pre-screen is defined by the Substance Abuse and Mental Health Services Administration (SAMHSA) as "a rapid, proactive procedure to identify individuals who may have a condition or be at risk for a condition before obvious manifestations occur." It involves short questions relating to alcohol and drug use and should be administered prior to beginning a full screening. Pre-screens are considered part of routine medical management and are not a separately reimbursable service.
The current approved pre-screening tools are:
- The Parents, Peers, Partner and Pregnancy (The 4P’s) Screening Tool
- The Parents, Peers, Partner, Pregnancy and Past (The 5P’s) Screening Tools
Full Screen
Full screens entail asking members a validated series of questions to assess the level of a member's substance use. Full screens are covered for members with signs, symptoms, and medical conditions that suggest risky or problem alcohol or drug use.
Full screenings should be used as a primary method for educating members about the health effects of using alcohol and other drugs. Health First Colorado (Colorado's Medicaid Program) covers screening services in a wide variety of settings to increase the chance of identifying individuals at risk for future substance abuse.
Providers are required to use an evidence-based screening tool to identify members at risk for substance use problems. The screening tool should be simple enough to be administered by a wide range of health care professionals. The tool must demonstrate sufficient evidence of validity and reliability to accurately identify members at potential risk for substance use disorder. Enough information must be generated from utilizing the tool to customize an appropriate intervention based on the identified level of substance use. Providers may use more than one (1) screening tool during the screening process if appropriate, however, no additional reimbursement will be made.
Health First Colorado has approved several evidence-based screening tools and will update the list as new methods become available.
The current approved evidence-based screening tools are:
- The Alcohol Use Disorders Identification Test (AUDIT)
- The Drug Abuse Screening Test (DAST)
- The Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST)
- The Car, Relax, Alone, Forget, Friends, Trouble Screening Test (CRAFFT), which has been validated for adolescents
- The Problem-Oriented Screening Instrument for Teenagers (POSIT)
- The Cannabis Use Disorders Test-revised (CUDIT-R), for adults and adolescents
- The Screening to Brief Intervention (S2BI), for adolescents
Brief Intervention
Brief interventions are interactions with members that are intended to induce a change in a health-related behavior. Often one (1) to three (3) follow-up contacts are provided to assess and promote progress and to evaluate the need for additional services. Brief interventions are typically used as a management strategy for members with risky or problem alcohol or drug use who are not dependent. This includes members who may or may not qualify for a Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) diagnosis of alcohol or drug abuse.
Brief substance use intervention services are covered for members who, through the use of an evidence-based screening tool, are identified as at-risk for a substance use disorder(s). Brief intervention may be single or multiple sessions to increase insight and awareness regarding substance use and motivation for changes in behavior. Alternatively, a brief intervention may also be used to increase motivation and acceptance of a referral for substance use treatment. Intervention services may occur on the same date of service as the screening or on a later date. Brief intervention is not covered prior to screening.
Providers are required to use effective strategies for counseling and intervention. Examples of demonstrated effective strategies include the following:
Follow-Up
Follow-up services include interactions that occur after initial intervention, treatment, or referral services, and are intended to reassess a member's status, assess a member's progress, promote or sustain a reduction in alcohol or drug use, and/or assess a member's need for additional services.
Referral
Members who appear to be alcohol- or drug-dependent are typically referred to alcohol and drug treatment programs. Treatment referrals must be made to the member's Regional Accountable Entity (RAE). Visit the RAE web page for contact information and further details.
Member Eligibility
The SBIRT benefit is available to members ages 12 and older who are enrolled in Health First Colorado. Members enrolled in a Health First Colorado HMO or managed care organization (MCO) must receive SBIRT services through the HMO or MCO.
Eligible Providers
The following licensed providers are eligible to provide SBIRT or supervise staff who provide SBIRT:
- Physician/psychiatrist
- Psychologist, PsyD / Ph.D.
- Masters level clinicians:
- Licensed clinical social worker (LSCW)
- Licensed marriage and family therapist (LMFT)
- Licensed professional counselor (LPC)
- Nurse Practitioner
- Physician Assistant
Non-licensed providers may deliver SBIRT under the supervision of a licensed provider if such supervision is within the legal scope of practice for that licensed provider.
Providers must be enrolled in Health First Colorado in order to:
- Treat a Health First Colorado member
- Submit claims for payment to Health First Colorado
Training Requirements for Licensed and Unlicensed Health Care Professionals
In order to directly deliver screening and intervention services, providers are required to participate in training that provides information about the implementation of evidence-based protocols for screening, brief interventions, and referrals to treatment. Face-to-face trainings and consultations are available through various entities such as SBIRT Colorado, Colorado Community Managed Care Network, and the Emergency Nurses Association.
Unlicensed providers may deliver SBIRT services under the supervision of licensed providers if such supervision is within the legal scope of practice for that licensed provider. The licensed provider assumes professional responsibility for the services provided by the unlicensed provider. All unlicensed providers who deliver SBIRT services under the supervision of licensed providers must meet the following requirements:
- Unlicensed health care professionals must complete a minimum of 60 hours of professional training (e.g., education, coursework, internship, practicum) within their respective field. This experience must include a minimum of four (4) hours of training that is directly related to SBIRT services. At least 30 of the 60 hours must meet the requirements state below.
- Unlicensed health care professionals must complete a minimum of 30 hours of face-to-face patient contact within their field. This may include internships, on-the-job training, or professional experience.
All providers are required to retain documentation confirming that staff providing SBIRT meet the training, education, and supervision requirements.
SBIRT Billing Information
The procedure codes used to report SBIRT services for reimbursement are consistent among all provider types. This section will provide a comprehensive overview of the elements necessary to report SBIRT services in various billing scenarios. A provider may not submit a claim containing both Current Procedural Terminology (CPT) and Healthcare Common Procedural Coding System (HCPCS) codes. The provider must use either the CPT or the HCPCS codes designated for SBIRT services.
Currently, Colorado SBIRT has codes only for the screening and brief intervention services for 15 - 30 minutes (procedure code 99408) or greater than 30 minutes (procedure code 99409). If billing an E/M service and either 99408 or 99409 on a claim, providers should use modifier –25 to indicate that the E/M service is separately identifiable. Ensure the E/M service is documented and coded appropriately.
Procedure code H0049 can be billed when a full screening is conducted and the result is negative. H0049 may be billed in addition to the E/M code for the visit.
Procedure Code Overview
Health First Colorado accepts procedure codes that are approved by the Centers for Medicare & Medicaid Services (CMS). The procedure codes are used to submit claims for services provided to Health First Colorado members and represent services that may be provided by enrolled certified Health First Colorado providers.
The Healthcare Common Procedural Coding System (HCPCS) are divided into two (2) principal subsystems, referred to as level I and level II of the HCPCS. Level I of the HCPCS is comprised of CPT, a numeric coding system maintained by the American Medical Association (AMA).
The CPT is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other health care professionals. Level II of the HCPCS is a standardized coding system that is used primarily to identify products, supplies, and services not included in the CPT codes, such as ambulance services and durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) when used outside a physician's office. Level II codes are also referred to as alpha-numeric codes because they consist of a single alphabetical letter followed by four (4) numeric digits, while CPT codes are identified using five (5) numeric digits.
The Health Insurance Portability & Accountability Act requires providers to comply with the coding guidelines of the AMA CPT Procedure Codes and the International Classification of Disease, Clinical Modification Diagnosis Codes. If there is no time designated in the official descriptor, the code represents one (1) unit or session.
Visit the Bulletins web page for monthly bulletins, which include updates on approved procedures codes and the maximum allowable units billed per procedure. Visit the Provider News web page to sign up for provider bulletin communications.
National Correct Coding Initiative (NCCI) Edits for SBIRT
Policy guidance for NCCI provided in this manual does not supersede Federal NCCI policy. It is published to assist providers in understanding how the Health First Colorado SBIRT benefit is affected by NCCI edits. Health First Colorado's policy is to allow SBIRT codes to be billed on the same day as other Evaluation & Management (E&M) services (10 CCR 2505-10 8.747.6.C)
NCCI Procedure-to-procedure (PTP) billing edits affect SBIRT codes. Pursuant to the National Correct Coding Initiative Policy Manual (revision 1/1/2016 - Chapter XI - Page 9), if a provider reports the SBIRT codes 99408 and 99409 with an E&M, psychiatric diagnostic, or psychotherapy code utilizing an NCCI PTP-associated modifier, the provider is certifying that the SBIRT code service is:
- A distinct and separate service performed during a separate time period (not necessarily a separate member encounter) than the E&M, psychiatric diagnostic, or psychotherapy service and,
- Is a service that is not included in the E&M, psychiatric diagnostic, or psychotherapy service based on the clinical reason for the E&M, psychiatric diagnostic, or psychotherapy service.
If the E&M, psychiatric diagnostic, or psychotherapy service would normally include assessment and/or intervention of alcohol or substance abuse based on the member's clinical presentation, SBIRT codes may not be additionally reported.
Providers may attach bypass modifiers (typically '25' or '59') to 99408- and 99409-line items which allow those line items to be reimbursed in addition to the E&M code. Visit the Centers for Medicare & Medicaid Services (CMS) NCCI web page for further instruction on NCCI edits and bypass modifier use.
Screening and Brief Intervention Procedure Codes
| Procedure Code | Description | Modifier | Ancillary Diagnosis | Unit of Service | Prior Authorization Required |
|---|---|---|---|---|---|
| 99408 | Alcohol and/or substance (other than tobacco) abuse structured screening (eg, AUDIT, DAST), and brief intervention (SBI) services; 15 to 30 minutes. | Modifier 25 or 59 may be applied to bypass NCCI edits. | Z71.41 Z71.51 | Limit one (1) per day, four (4) per state fiscal year. Each session is limited to two (2) units per session, at 15 minutes per unit. | No PA |
| 99409 | Alcohol and/or substance (other than tobacco) abuse structured screening (eg, AUDIT, DAST), and brief intervention (SBI) services; greater than 30 minutes. | Modifier 59 may be applied to bypass NCCI edits. | Z71.41 Z71.51 | Limit one (1) per day, two (2) per state fiscal year. | No PA |
Clinical guidance for procedure codes 99408 and 99409:
Screening and brief intervention describes a different type of member-physician interaction than the provision of general advice. It requires a significant amount of time and additional acquired skills to deliver. Screening and brief intervention techniques are discrete, clearly distinguishable clinical procedures that are effective in identifying problematic alcohol or substance use. Components include but are not limited to:
- Using a standardized screening tool
- Providing feedback to the member on the screening results
- Discussing negative consequences that have occurred and the overall severity of the problem
- Motivating the member toward behavioral change
- A joint decision-making process regarding alcohol and/or drug use
- Discussing and agreeing on plans for follow-up with member
Ancillary staff, including health educators, may perform SBIRT services under the supervision of a credentialed provider. The services should relate to a plan of care and will require billing under the supervising physician. SBIRT screening and brief intervention that does not meet the minimum 15-minute threshold is not separately reimbursable. These are time-based codes; therefore, documentation must denote start/stop time or total face-to-face time with the member. Due to procedure code 99409 being inclusive of the time spent before 30 minutes is accumulated, the two (2) procedure codes may not be billed together on the same date of service. Both procedure codes account for screening and brief intervention, therefore state fiscal yearly limits for screening and brief intervention apply to each.
Procedure code 99408 / procedure code 99409 may only be billed when all these conditions are met:
- When a full screen is positive
- When they account for the time of full screening, brief intervention and/or referral to treatment
Note: The state fiscal year is July 1 through June 30.
Negative Screening Result Procedure Code
Procedure code H0049 - Alcohol and/or drug screening, (untimed)
| Procedure Code | Description | Modifier | Ancillary Diagnosis | Unit of Service | Prior Authorization Required |
|---|---|---|---|---|---|
| H0049 | Alcohol and/or drug screening (e.g., AUDIT, DAST, CRAFFT, etc.) | Modifier 59 may be applied to bypass NCCI edits. | Z13.9 | Limit one (1) per day, two (2) per state fiscal year. | No PA |
A full screen will frequently be negative, and the member will not require brief intervention or referral to treatment. These instances are still reimbursable using the HCPCS procedure code H0049. When using procedure code H0049, a unit of service is equivalent to the total amount of time required to administer the screening. Therefore, when billing the screening the units of service should always equal one (1) regardless of time spent completing the screening.
Procedure code H0049 may only be billed when all these conditions are met:
- It followed a positive pre-screen
- The full screen was negative
- A brief intervention or referral to treatment was not necessary
Procedure code H0049 may not be billed in conjunction with procedure code 99408 or procedure code 99409 because those two (2) codes are also inclusive of a full screening.
Diagnosis Codes
Diagnosis codes play a critical role in supporting the medical necessity of the CPT or HCPCS codes that are billed. Below are tables of common ancillary (non-principal) diagnosis codes for reporting SBIRT services, and allowable codes for reporting the place of service for providing SBIRT services.
Ancillary ICD-10 Codes for SBIRT
| ICD-10 Code | Description |
| Z13.9 | Encounter for screening, unspecified |
| Z71.41 | Alcohol abuse counseling & surveillance of alcoholic |
| Z71.51 | Drug abuse counseling and surveillance of drug abuser |
Allowable Place of Service Codes
| Code | Description |
|---|---|
| 03 | School |
| 11 | Office |
| 12 | Home |
| 21 | Inpatient Hospital |
| 22 | Outpatient Hospital |
| 23 | Emergency Room Hospital |
Emergency Department
SBIRT that is provided in the hospital emergency department may be billed directly to Health First Colorado by the rendering physician or may be included in the hospital claim, but never both.
Federally Qualified Health Centers (FQHCs) / Rural Health Clinics (RHC)
Reimbursement for SBIRT is included in the encounter rate payment. No separate reimbursement for SBIRT is allowable in these settings. Providers must still attach procedure codes H0049, 99408, or 99409 and the appropriate ancillary diagnosis codes to the encounter claim.
Additional Policies
- Screening Brief Intervention Treatment is not designed to address smoking and tobacco cessation services unless it is a co-occurring diagnosis with another substance such as drugs or alcohol. Tobacco-only services are not a SBIRT billable benefit.
- Screening Brief Intervention Treatment must be provided face-to-face with the member or via telemedicine (simultaneous audio and video transmission or by telephone audio-only) with the member.
- A physician order, referral, or prescription is not required for any component of SBIRT.
- A prior authorization request is not required.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
8.280.4.E Other EPSDT Benefits
Other health care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Section 1905(a) of the Social Security Act are a covered benefit under EPSDT when medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, regardless of whether such goods and services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a good or service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one (1) or more Activities of Daily Living; and meets the criteria set forth at Section 8.076.1.8.b - g.
- The service provides a safe environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly.
Member Benefit Limitations
- Up to two (2) full screens per state fiscal year.
- Up to four (4) sessions of brief intervention/referral per state fiscal year.
Reimbursement
Reimbursement for SBIRT services will be made at the lesser of the provider's usual and customary charge or the Health First Colorado maximum allowable fee for the service. Health First Colorado will pay for separate and additional services on the same day as SBIRT, including medically necessary E&M services. The SBIRT codes will not be separately reimbursed when billing under the Mental Health and Substance Use Disorder Screening benefit using procedure codes H0002 and H0004, or with any other HCPCS or CPT code that represents the same or similar services. Claims cannot be submitted using combined CPT and HCPCS codes designated for SBIRT services (e.g., procedure code 99408 and procedure code H0049).
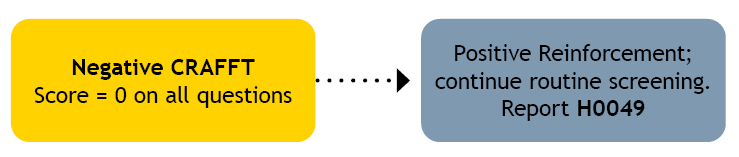
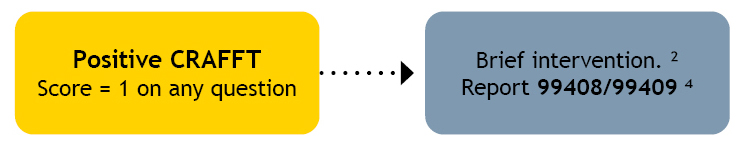
Adolescent SBIRT Using the CRAFFT - Billing Algorithm
This algorithm pertains to patients who answered positively to one (1) or more of the three (3) pre-screening questions.
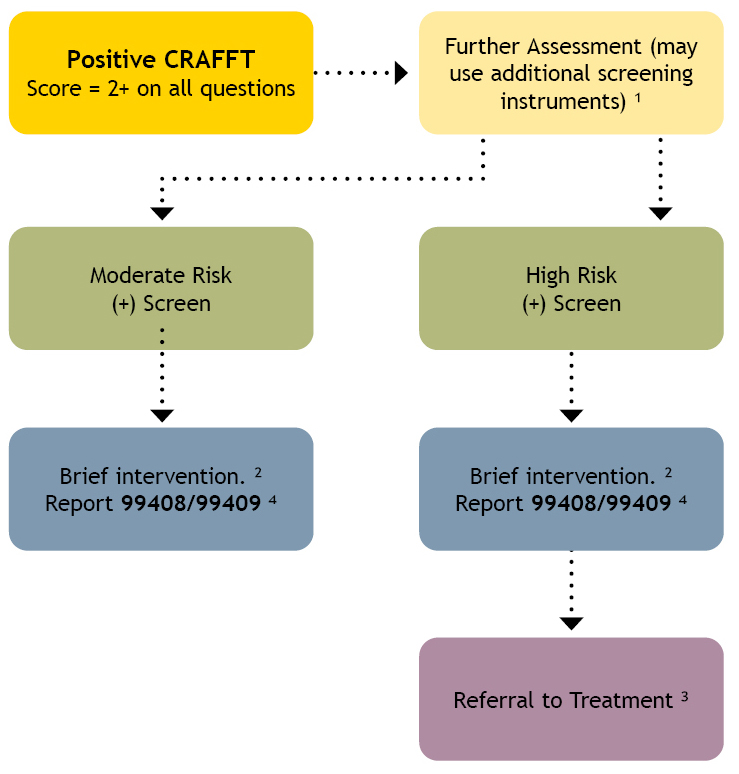
1 – Further screening instruments that could be used: AUDIT, CUDIT-R, DAST-10© and others. Determine level of risk based on scores and other factors such as types of drinking or drug use, psychosocial factors, potential for pregnancy and recent changes in behavior or academics related to substances.
2 – Motivational Conversations/Brief Intervention (BI): Provide feedback, explore, substance use, set goal(s) for change. BI may be completed in one (1) or two (2) visits. Medicaid reimburses for up to four (4) BI per year.
3 – Referral to Treatment: Identify and assess co-occurring conditions, identify appropriate level of services and treatment based on need, arrange services, arrange coordination and follow-up. Referrals may be internal or external. Treatment may include medications, counseling, mutual support and addressing social needs.
4 – Brief Intervention codes 99408 (15-30 minutes) and 99409 (≥30 minutes) can only be used when the time requirement is met.
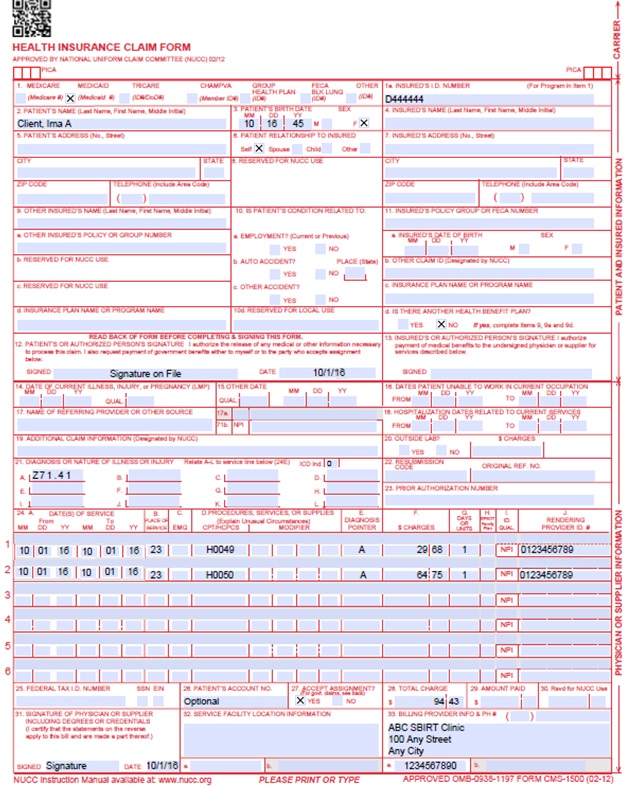
SBIRT Paper Claim Reference Table
The following paper form reference table describes required fields for the paper CMS 1500 claim form for SBIRT claims:
| CMS Field Number & Label | Field is: | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070118 for July 1, 2018. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Other Date | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070118 for July 1, 2018. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left-hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010116 for January 1, 2016.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area)
Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
CMS 1500 SBIRT Claim Example
Resources
- SBIRT Colorado Face-to-face training, consultation and other education opportunities
- SBIRT Training online
- Alcohol Screening/Guidelines
- Colorado Office of Behavioral Health referral resources for substance use and mental health prevention, treatment and recovery
- Substance Abuse and Mental Health Services Administration Behavioral Health Treatment Services Locator
- Online training modules to practice screening and brief intervention skills with virtual members
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
SBIRT Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 8/9/2017 | Added CUDIT-R and SB2I tools | HCPF |
| 4/4/2018 | Revised pre-screen policy. It is no longer a pre-requisite for a full screen. | HCPF |
| 5/9/2018 | Added the Adolescent SBIRT Billing Algorithm which is a joint project with the Office of Behavioral Health and Department of Public Health and Environment | HCPF |
| 6/25/2018 | Updated billing to point to general manual Replaced BHO with RAE | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 1/22/2019 | Update links to resources | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 2/27/2020 | Converted to web page | HCPF |
| 3/27/2020 | Fixed broken hyperlinks throughout. | HCPF |
| 7/28/2020 | Added section to training requirements | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 3/9/2021 | Clarified that SBIRT may be provided via telephone-only using telemedicine | HCPF |
| 7/7/2021 | Updating with the standard EPSDT policy language. | HCPF |
| 10/8/2021 | Updated “Alcohol Use Disorders Inventory Test” to “Alcohol Use Identification Test” under the Full Screen section. | HCPF |
| 3/27/2023 | Updated AWS URL Links | HCPF |
| 8/21/2024 | Updated the flowchart for Adolescent SBIRT Using the CRAFFT - Billing Algorithm for accessibility. Updated the number of limitations for brief intervention and added a supplemental resource for billing guidance on encounters that do not reach the 15-minute limit. | HCPF |
| 9/11/2024 | Updated graphic, added footnotes | HCPF |
| 10/9/2024 | Updated allowable units of service for 99408 and member benefit limitations. Also added an updated flowchart for Adolescent SBIRT Using the CRAFFT - Billing Algorithm for accessibility. | HCPF |
| 5/20/2025 | Added the 4 P’s and 5 P’s Screening tools | HCPF |