Reproductive Health Care Billing Manual
Reproductive Health Care and Related Services
- Family Planning and Family Planning-Related Services
- Abortion Services
- Women’s Health Care
- CMS 1500 Reference Table
- Hospital Inpatient Billing
- Billing Information
- Timely Filing
- Reproductive Health Care Billing Manual Revisions Log
Return to Billing Manuals Web Page
Family Planning and Family Planning-Related Services
Covered Services
Family planning services mean those services provided to members of child-bearing age, including sexually active minors, with the intent to delay, prevent, or plan for a pregnancy.
Family planning services may include: physical examinations, diagnoses, treatments, counseling, supplies (including all FDA-approved contraceptives, except spermicides and female condoms), Prescriptions, follow-up visits to evaluate or manage outcomes associated with contraceptive methods, pregnancy tests, sterilization services, and counseling services focused on preventing, delaying, or planning a pregnancy.
Non-Covered Family Planning Services
Services to identify and/or treat a member’s infertility concerns are not included as a Family Planning-related service, nor is infertility a covered Health First Colorado Service.
Voluntary Sterilization
Sterilization for family planning is a covered benefit. Sterilization (i.e., tubal ligations, tubal occlusion, and vasectomies) is intended to be a permanent, irreversible procedure to prevent consenting individuals from becoming pregnant or fathering a child. Submission of family planning sterilization claims should always include the family planning modifier (FP) and be submitted in accordance with the following procedure codes:
| CPT/HCPCS or Dx Code | Modifier 1 | Modifier 2 |
|---|---|---|
| Z30.2 | ||
| 55250 | FP | |
| 55450 | FP | |
| 55870 | FP | |
| 58340 | FP | |
| 58345 | FP | |
| 58600 | FP | |
| 58605 | FP | |
| 58611 | FP | |
| 58661 | FP | |
| 58670 | FP | |
| 58700 | FP | |
| 58720 | FP | |
| 58940 | FP | |
| 64435 | FP | |
| 74742 | FP | |
| 76831 | FP | |
| 76856 | FP |
Requirements for Sterilization Procedures
Claims for sterilization procedures should be submitted electronically. A copy of the Health First Colorado Consent for Sterilization- MED 178 Form, located on the Provider Forms Web Page under the Sterilization Consent Forms drop-down menu. If more than one provider bills for a sterilization procedure, each provider must include a copy of the consent form with their own claim. This includes the hospital, surgeon, the anesthesiologist, and the assistant surgeon. Even though it is one procedure and one consent form, the form must be sent with every related claim or that claim may be denied.
Informed Sterilization Consent Requirements
The person obtaining informed consent must be a professional staff member who is qualified to address all the consenting individual's questions concerning medical, surgical, and anesthesia issues.
Informed consent is considered to have been given when the person who obtained consent for the sterilization procedure meets all of the following criteria:
- Has offered to answer any questions that the individual who is to be sterilized may have concerning the procedure
- Has provided a copy of the consent form to the individual
- Has verbally provided all of the following information or advice to the individual who is to be sterilized:
- Advice that the individual is free to withhold or withdraw consent at any time before the sterilization is done without affecting the right to any future care or treatment and without loss or withdrawal of any federally funded program benefits to which the individual might be otherwise entitled
- A description of available alternative methods of family planning and birth control
- Advice that the sterilization procedure is considered to be irreversible
- A thorough explanation of the specific sterilization procedure to be performed
- A full description of the discomforts and risks that may accompany or follow the performance of the procedure, including an explanation of the type and possible effects of any anesthetic to be used
- A full description of the benefits or advantages that may be expected as a result of the sterilization
- Advise that the sterilization will not be performed for at least 30 days, except in the case of premature delivery or emergency abdominal surgery
- Suitable arrangements have been made to ensure that the preceding information was effectively communicated to an individual who is blind, deaf, or otherwise handicapped
- The individual to be sterilized was permitted to have a witness of his or her choice present when consent was obtained
- The consent form requirements (noted below) were met
- Any additional requirement of the state or local law for obtaining consent was followed
- Informed consent may not be obtained while the individual to be sterilized is:
- In labor or childbirth
- Seeking to obtain or is obtaining an abortion
- Under the influence of alcohol or other substances that may affect the individual's sense of awareness
MED-178 Consent Form Requirements
Evidence of informed consent must be provided on the Consent to Sterilization - MED 178 Form located on the Provider Forms web page under the Sterilization Consent Forms drop-down menu. The fiscal agent is required to ensure that the provisions of the law have been followed before Health First Colorado payment can be made for sterilization procedures. Information entered on the consent form must correspond directly to the information on the submitted Health First Colorado claim form.
A copy of the Consent to Sterilization - MED 178 Form must be attached to every claim submitted for reimbursement of sterilization charges. If more than one provider bills for a sterilization procedure, each provider must include a copy of the consent form with their own claim. This includes the hospital, surgeon, the anesthesiologist, and the assistant surgeon. Even though it is one procedure and one consent form, the form must be sent with every related claim or that claim may be denied. The surgeon is responsible for assuring that the MED-178 consent form is properly completed and providing copies of the form to the other providers for billing purposes.
Spanish forms are acceptable and are located on the Provider Forms web page under the Sterilization Consent Forms drop-down menu.
A sterilization consent form initiated in another state is acceptable when the text is complete and consistent with the Colorado form.
Claims that are denied because of errors, omissions, or inconsistencies on the MED-178 may be resubmitted if corrections to the consent form can be made in a legally acceptable manner. Any corrections to the member's portion of the sterilization consent must be approved and initialed by the member.
Exceptions
At least 30 days, but not more than 180 days, must pass between the date of informed consent and the date of sterilization, with the following exceptions:
- Emergency Abdominal Surgery
An individual may consent to sterilization at the time of emergency abdominal surgery if at least 72 hours have passed since they gave informed consent for the sterilization. - Premature Delivery
A member may consent to sterilization at the time of the premature delivery if at least 72 hours have passed since they gave informed consent for the sterilization, and the consent was obtained at least 30 days before the expected date of delivery.
The person may not be an "institutionalized individual."
Institutionalized includes:- Involuntary confinement or detention, under a civil or criminal statute, in a correctional or rehabilitative facility, including a mental hospital or other facility for the care and treatment of mental illness.
- Confinement under a voluntary commitment in a mental hospital or other facility for the care and treatment of mental illness.
Unpaid or denied claims resulting from providers' failure to follow the required procedures in obtaining informed consent or failure to submit required documentation with the claim may not be billed to the member (§§ 25.5-4-300.4 — 25.5-4-310).
The following procedure codes are examples used for sterilization:
- 58600
- 58605
- 58565
- 58670
- 55450
- 55250
- 58611
The diagnosis code(s) associated:
Z30.2: Encounter for sterilization
Z98.51 or Z98.52: Use for sterilization follow-up evaluations
Male and Female surgical sterilization procedure codes and surgical methodologies (bilateral examples) are listed below in the Billing Guidance section. For additional surgical codes, refer to the ICD-10-PCS manual. If surgical procedures are unilateral (not bilateral) and surgery does not result in sterilization, utilize the appropriate right (RT) or left (LT) modifier with the procedure code on claims. When the unilateral procedure does not lead to complete sterilization, the MED-178 Sterilization Consent Form is not required.
Basic Fertility Services
- Counseling services focused on understanding the basic reproductive health system and fertility cycle, as related to methods to prevent, delay or plan for a pregnancy
- Basic fertility evaluations may include a pelvic exam, ultrasounds, or sperm analysis to support a member’s understanding of their ability to achieve a healthy pregnancy.
Family Planning-Related Services
Family planning-related services are essential, medically necessary services provided in a family planning setting as part of or as follow-up to a family planning visit. Such services are provided because they were identified or diagnosed during a family planning visit.
Family planning-related services could include:
- Drugs for the treatment of Sexually Transmitted Diseases (STD) or Sexually Transmitted Infections (STI) when the STD/STI is identified, or diagnosed, during a routine or periodic family planning visit. A follow-up encounter for STD/STI treatment and drugs may be covered. In addition, subsequent follow-up visits to rescreen for STIs/STDs based on the Centers for Disease Control and Prevention guidelines may be covered.
- A comprehensive patient history, physical, laboratory tests, contraceptive counseling, cervical cancer screening, and other prevention services, regardless of gender.
- Drugs for the treatment of lower genital tract and genital skin infections/disorders, and urinary tract infections, when the infection or disorder is identified or diagnosed, during a routine or periodic family planning visit. A follow-up encounter for treatment or drugs may be covered.
- Reproductive health-related evaluations or preventive services (related to reproductive health and identified on the U.S. Preventive Service Task Force, A & B Recommendations) such as cervical cancer screening, syphilis, chlamydia and gonorrhea screening, HIV screening, tobacco cessation services, or depression screening.
Licensed practitioners must be enrolled with Health First Colorado. They must only render family planning-related services within the scope of their practice. Claims should have the appropriate CPT/HCPCS codes that are designated as family planning services with the FP+32 modifiers (excluding any abortion services) at the detail level on the claim.
Billing Guidance
Providers Billing on the CMS 1500 Claim Form
Use the appropriate procedure/diagnosis code from the recommended list above, and the family planning modifier (FP).
Providers Billing on the UB-04 Claim Form
The ICD-10 Sterilization Diagnosis Code: Z30.2 (Encounter for sterilization) and appropriate procedure code (with the FP modifier) OR one ICD-10 PCS code (a 7-digit alpha-numeric code)
Sterilization ICD-10 Surgical Procedural Codes (PCSs) should be selected from the following methodologies:
ICD-10 PCS Female Sterilization
Legend:
Section: 0=Medical and Surgical
Body System: U= Female Reproductive System
Body Part:
- 2 = Ovaries, Bilateral
- 7 = Fallopian Tubes, Bilateral
Approach:
- 0 = Open
- 3 = Percutaneous
- 4 = Percutaneous Endoscopic
- 7 = Via Natural or Artificial Opening
- 8 = Via Natural or Artificial Opening Endoscopic
- F = External
Device:
- C, D, Z (most sterilization is Z= no device)
Qualifier:
- Z = no qualifier
- X = Diagnostic (for excision/biopsy)
Destruction (Root Operation =5)
| Code | Body Part | Approach |
|---|---|---|
| 0U520ZZ | Ovaries, Bilateral (2) | Open (0) |
| 0U523ZZ | Ovaries, Bilateral (2) | Percutaneous (3) |
| 0U524ZZ | Ovaries, Bilateral (2) | Percutaneous Endoscopic (4) |
| 0U528ZZ | Ovaries, Bilateral (2) | Via Natural or Artificial Opening Endoscopic (8) |
| 0U570ZZ | Fallopian Tubes, Bilateral (7) | Open (0) |
| 0U573ZZ | Fallopian Tubes, Bilateral (7) | Percutaneous (3) |
| 0U574ZZ | Fallopian Tubes, Bilateral (7) | Percutaneous Endoscopic (4) |
| 0U578ZZ | Fallopian Tubes, Bilateral (7) | Via Natural or Artificial Opening Endoscopic (8) |
All destruction codes: device = Z, qualifier = Z
Division (Root Operation = 8)
Pattern: 0 U 8 2 (Approach 0, 3, 4) ZZ
(Only ovaries, Bilateral)
| Code | Body Part | Approach |
|---|---|---|
| 0U820ZZ | Ovaries, Bilateral (2) | Open (0) |
| 0U823ZZ | Ovaries, Bilateral (2) | Percutaneous (3) |
| 0U824ZZ | Ovaries, Bilateral (2) | Percutaneous Endoscopic (4) |
Device= Z, Qualifier = Z
Excision (Root Operation = B)
Pattern: 0 U B [Body Part 2 or 7] [Approach 0,3,4,7,8] Z [Qualifier X or Z]
Excision – Ovaries, Bilateral (Body Part = 2)
| Code | Approach | Qualifier |
|---|---|---|
| 0UB20ZX | Open (0) | X – Diagnostic |
| 0UB20ZZ | Open (0) | Z – No qualifier |
| 0UB23ZX | Percutaneous (3) | X – Diagnostic |
| 0UB23ZZ | Percutaneous (3) | Z – No qualifier |
| 0UB24ZX | Percutaneous Endoscopic (4) | X – Diagnostic |
| 0UB24ZZ | Percutaneous Endoscopic (4) | Z – No qualifier |
| 0UB27ZX | Via Natural or Artificial Opening (7) | X – Diagnostic |
| 0UB27ZZ | Via Natural or Artificial Opening (7) | Z – No qualifier |
| 0UB28ZX | Via Natural or Artificial Opening Endoscopic (8) | X – Diagnostic |
| 0UB28ZZ | Via Natural or Artificial Opening Endoscopic (8) | Z – No qualifier |
Excision – Fallopian Tubes, Bilateral (Body Part = 7)
| Code | Approach | Qualifier |
|---|---|---|
| 0UB70ZX | Open (0) | X – Diagnostic |
| 0UB70ZZ | Open (0) | Z – No qualifier |
| 0UB73ZX | Percutaneous (3) | X – Diagnostic |
| 0UB73ZZ | Percutaneous (3) | Z – No qualifier |
| 0UB74ZX | Percutaneous Endoscopic (4) | X – Diagnostic |
| 0UB74ZZ | Percutaneous Endoscopic (4) | Z – No qualifier |
| 0UB77ZX | Via Natural or Artificial Opening (7) | X – Diagnostic |
| 0UB77ZZ | Via Natural or Artificial Opening (7) | Z – No qualifier |
| 0UB78ZX | Via Natural or Artificial Opening Endoscopic (8) | X – Diagnostic |
| 0UB78ZZ | Via Natural or Artificial Opening Endoscopic (8) | Z – No qualifier |
Device= Z for all excision codes
Occlusion (Root Operation = L)
4A. Occlusion – Fallopian Tubes, Bilateral, Approaches 0/3/4
Pattern: 0 U L 7 [Approach 0,3,4] [Device C,D,Z] Z
| Code | Approach | Device (char only) |
|---|---|---|
| 0UL70CZ | Open (0) | C |
| 0UL70DZ | Open (0) | D |
| 0UL70ZZ | Open (0) | Z |
| 0UL73CZ | Percutaneous (3) | C |
| 0UL73DZ | Percutaneous (3) | D |
| 0UL73ZZ | Percutaneous (3) | Z |
| 0UL74CZ | Percutaneous Endoscopic (4) | C |
| 0UL74DZ | Percutaneous Endoscopic (4) | D |
| 0UL74ZZ | Percutaneous Endoscopic (4) | Z |
Occlusion- Fallopian Tubes, Bilateral, Approaches 7/8
Pattern: 0 U L 7 [Approach 7,8] [Device D,Z] Z
| Code | Approach | Device |
|---|---|---|
| 0UL77DZ | Via Natural or Artificial Opening (7) | D |
| 0UL77ZZ | Via Natural or Artificial Opening (7) | Z |
| 0UL78DZ | Via Natural or Artificial Opening Endoscopic (8) | D |
| 0UL78ZZ | Via Natural or Artificial Opening Endoscopic (8) | Z |
Resection (Root Operation = T)
Pattern: 0 U T [Body Part 2 or 7] [Approach 0,4,7,8,F] Z Z
Resection – Ovaries, Bilateral (Body Part = 2)
| Code | Approach |
|---|---|
| 0UT20ZZ | Open (0) |
| 0UT24ZZ | Percutaneous Endoscopic (4) |
| 0UT27ZZ | Via Natural or Artificial Opening (7) |
| 0UT28ZZ | Via Natural or Artificial Opening Endoscopic (8) |
| 0UT2FZZ | External (F) |
Resection- Fallopian Tubes, Bilateral (Body Part = 7)
| Code | Approach |
|---|---|
| 0UT70ZZ | Open (0) |
| 0UT74ZZ | Percutaneous Endoscopic (4) |
| 0UT77ZZ | Via Natural or Artificial Opening (7) |
| 0UT78ZZ | Via Natural or Artificial Opening Endoscopic (8) |
| 0UT7FZZ | External (F) |
Device= Z, Qualifier= Z for all resection codes
ICD-10 PCS Male Sterilization (Bilateral)
Legend:
Section: 0 = Medical and Surgical
- Body System: V = Male Reproductive System
- Body Part: Q = Vas Deferens, Bilateral
- Root Operations:
- 5 = Destruction
- B = Excision
- L = Occlusion
- T = Resection
- Approaches: 0 (Open), 3 (Percutaneous), 4 (Percutaneous Endoscopic), 8 (Via natural or artificial opening endoscopic)
- Device: C, D, Z (depending on operation)
- Qualifier: Z (or X for excision-diagnostic)
Destruction of Vas Deferens, Bilateral (Root Operation = 5)
Pattern: 0 V 5 Q [Approach 0,3,4,8] Z Z
Meaning: Destroying both vas deferens (e.g., burning, cutting with destruction intent).
| ICD-10-PCS Code |
|---|
| 0V5Q0ZZ |
| 0V5Q3ZZ |
| 0V5Q4ZZ |
| 0V5Q8ZZ |
Excision of the Vas Deferens, Bilateral
Root Operation = B
Pattern: 0 V B Q [Approach: 0,3,4,8] Z [Qualifier X or Z]
Excision – Therapeutic/Non-Diagnostic (Qualifier = Z)
| ICD-10-PCS Code |
|---|
| 0VBQ0ZZ |
| 0VBQ3ZZ |
| 0VBQ4ZZ |
| 0VBQ8ZZ |
Excision- Diagnostic (Qualifier = X)
| ICD-10-PCS Code |
|---|
| 0VBQ0ZX |
| 0VBQ3ZX |
| 0VBQ4ZX |
| 0VBQ8ZX |
Occlusion of the Vas Deferens, Bilateral
Root Operation = L
Pattern: 0 V L Q [Approach: 0,3,4,8] [Device: C, D, Z] Z
Open Approach (0)
| ICD-10-PCS Code |
|---|
| 0VLQ0CZ |
| 0VLQ0DZ |
| 0VLQ0ZZ |
Percutaneous Approach (3)
| ICD-10-PCS Code |
|---|
| 0VLQ3CZ |
| 0VLQ3DZ |
| 0VLQ3ZZ |
Percutaneous Endoscopic Approach (4)
| ICD-10-PCS Code |
|---|
| 0VLQ4CZ |
| 0VLQ4DZ |
| 0VLQ4ZZ |
Via Natural or Artificial Opening Endoscopic (8)
| ICD-10-PCS Code |
|---|
| 0VLQ8CZ |
| 0VLQ8DZ |
| 0VLQ8ZZ |
Resection of Vas Deferens, Bilateral
Root Operation = T
Pattern: 0 V T Q [Approach: 0,4] Z Z
| ICD-10-PCS Code |
|---|
| 0VTQ0ZZ |
| 0VTQ4ZZ |
Abortion Services
Abortions
Effective January 1, 2026, coverage of abortion services was expanded in compliance with SB25-183 for the following eligibility categories:
Eligibility Categories
- Medicaid (TXIX), including Cover all Coloradoans
- Emergency Medicaid Services, also referred to as “Emergency Medical (EMS) and Reproductive Health Care Program (RHCS)”. Please see Health First Colorado’s Emergency Services Program web page for more information on the emergency services covered under the EMS benefit plan.
- Child Health Plan Plus (CHP+)
Covered Services
Services related to abortions will be fully covered via state funds for members enrolled in the above programs, regardless of circumstance. Members will no longer be subject to member deductibles, co-payments, or co-insurance for these services and may not be billed for them ( CO Rev. Stat. §25.5-4-301).
CHP+ providers must submit their claims to their CHP+ Managed Care Organization (MCO) for manual reconciliation reimbursement.
Family Planning Expanded Income Population (FAMPL) and Abortion Access
The FAMPL population receives federal match, under Senate Bill 21-025, an “eligible member” for FAMPL is defined as one who:
- Is not pregnant and whose income does not exceed the state’s current effective income level for pregnant people under the Children’s Health Plan Plus (CHP+).
- Refer to the Family Planning Expansion Billing Manual for more information on the expansion eligibility groups.
Considering federal matching may not be used for abortion procedures, FAMPL members cannot receive abortion coverage while remaining in the federally matched eligibility category.
The following guidance outlines how FAMPL members can access abortion care.
- The member must report the pregnancy
- The member will then be automatically moved into CHP+, which covers abortion services billed with Z33.2 using state-only funds.
- The member will receive 12 months of continuous CHP+ coverage, during which abortion services are payable.
Providers should assist members, when appropriate, in understanding the need to report pregnancy to ensure correct benefit enrollment for the services they are seeking.
Treatment for Non-Viable Pregnancy
The Department will continue to seek federal match regarding treatment related to non-viable pregnancies. No documentation is required for reimbursement of non-viable pregnancy treatment. When a member receives treatment for a non-viable pregnancy condition, an appropriate diagnosis code (listed below) must be listed:
- O00.0-O00.9 Ectopic Pregnancy
- O01.0-O01.9 Hydatidiform mole
- O02.0-O02.9 Other abnormal products of conception
- O02.1 Missed Abortion (incomplete miscarriage)
- O03.0-O03.9 Spontaneous Abortion
- O08.0-O08.9 Complications following ectopic and molar pregnancy
Claim Submission Requirements
Separation of State-Funded and Federally Matched Services (Professional Claims Only)
All abortion and abortion related-services must be billed together on a single claim funded by state-only dollars. Other services provided on the same date of service that qualify for a federal match must be billed on a separate claim:
Example:
- A member receives an abortion and an Intrauterine Device (IUD) insertion on the same date of service:
- Claim 1 (state-funded):
- Abortion procedure and all abortion-related services
- No FP or FP+32 modifiers
- Claim 2 (federally matched):
- IUD device and insertion
- FP or FP+32 modifiers, as appropriate
- Claim 1 (state-funded):
This ensures accurate federal vs. state fund allocation and prevents claim denials, reprocessing, or potential recoupment.
Modifier and Telemedicine Guidance
Family Planning Modifiers: FP and FP+32
Although abortion is classified as a family planning service under state law, abortion claims must not include the FP or FP+32 modifiers. FP modifiers indicate federally matched services, and abortion services are reimbursed with state-only funds. Using the FP modifiers on abortion claims will cause claims reprocessing or denials.
The Department requests that providers not append FP to FP+32 modifiers to abortion procedures, abortion-related E/M services, telemedicine components of abortion care, and S0199 abortion service bundles.
Telemedicine and S0199
Effective January 1, 2026, providers are no longer required to append Modifier 52 to S0199 when telemedicine is used for any portion of the service. Telemedicine may be used for components such as counseling, follow-up consultation, or confirmation of pregnancy.
Procedure Codes
Elective abortions are identified via diagnosis code Z33.2; no documentation is required for reimbursement of elective abortion-related services. Current system restrictions limiting abortion coverage to cases of incest, rape, or life endangerment will be removed, effective January 1, 2026.
Abortion and Pregnancy-Related Procedure Codes
The following CPT codes are appropriate for abortion and pregnancy-related services:
- 01964
- 01965
- 01966
- 58120
- 59100
- 59812-59830
- 59840
- 59841
- 59850
- 59851
- 59852
- 59855
- 59856
- 59857
- S0190
- S0191
- S0199
Surgical Procedure Codes
- 10A00ZZ
- 10A07Z6
- 10A07ZW
- 10A07ZX
- 10A07ZZ
- 10A08ZZ
Women’s Health Care
Women’s Health Services
Women’s Health Services include annual primary care, gynecological care, and other targeted reproductive tissue-related health care services such as:
- Sexually Transmitted Infection (STI) testing and treatment
- Hysterectomies
- Mastectomies, when medically necessary
- Breast reconstruction (Following and within 5 years of a mastectomy)
- Other reproductive tissue removal, when medically necessary
Women’s Health Services also include related preventive services as identified by the U.S. Preventive Services Task Force (USPSTF) and Health Resources and Services Administration (HRSA) recommendations.
Preventive services may include:
- Cervical Cancer Screening
- Mammograms
- BRCA genetic screening, when medically necessary, with genetic counseling and testing
- HPV vaccinations
- Any other relevant preventive services, as identified by the USPSTF
Hysterectomies
Hysterectomy is a benefit of Health First Colorado when performed solely for medical reasons.
Hysterectomies require an appropriately signed Departmental Acknowledgement/ Certification Statement form as a claim attachment for reimbursement for services rendered.
Hysterectomies are not considered a family planning benefit nor a Health First Colorado benefit if:
- The hysterectomy is performed solely for sterilization, or
- If there was more than one purpose for the procedure, and it would not have been performed but for sterilization.
The following conditions must be met for hysterectomy claims reimbursement:
- The claims must be submitted electronically
- Prior to the surgery, the person who secures consent to perform the hysterectomy must inform the member (and the person's representative, if in attendance) verbally and in writing that the hysterectomy will render the member permanently incapable of bearing children (sterile).
- The member and the person's representative, if any, must sign a Departmental Acknowledgement/Certification Statement Form for Hysterectomy as a written acknowledgment that the member has been informed that the hysterectomy will render the member permanently incapable of reproducing. The written Departmental Acknowledgment Form must be signed and dated by the member, completed by the provider, and submitted with the claim.
A written acknowledgment form from the member is not required if:
- The member is already sterile at the time of the hysterectomy, or
- The hysterectomy is performed because of a life-threatening emergency in which the practitioner determines that prior acknowledgment is not possible.
If the member’s acknowledgment is not required because of one of the above-noted exceptions, the practitioner who performs the hysterectomy must certify in writing on the Departmental Acknowledgement/Certification Statement Form, one of the following:
- That the member was already sterile at the time of hysterectomy, and stating the cause of the sterility; or
- The member required the hysterectomy under a life-threatening emergency in which the practitioner determined that prior acknowledgment by the member was not possible. The statement form must describe the nature of the emergency.
A copy of the member’s signed and dated Acknowledgment/Certification Statement Form or the practitioner’s signed and dated Certification Statement Form, as described above, must be attached to all claims submitted for hysterectomy services. The Acknowledgment/Certification Statement Form for a Hysterectomy, on which to report the required information, is located on the Provider Forms web page under Claim Forms and Attachments -> Women’s Health. Providers may copy this form, as needed, for attachment to claim(s). The submitted form must be signed and dated by the practitioner performing the hysterectomy.
The surgeon is responsible for providing copies of the appropriate acknowledgment or certification to the hospital, anesthesiologist, and assistant surgeon for billing purposes. A copy of the written acknowledgment or practitioner’s statement must be attached.
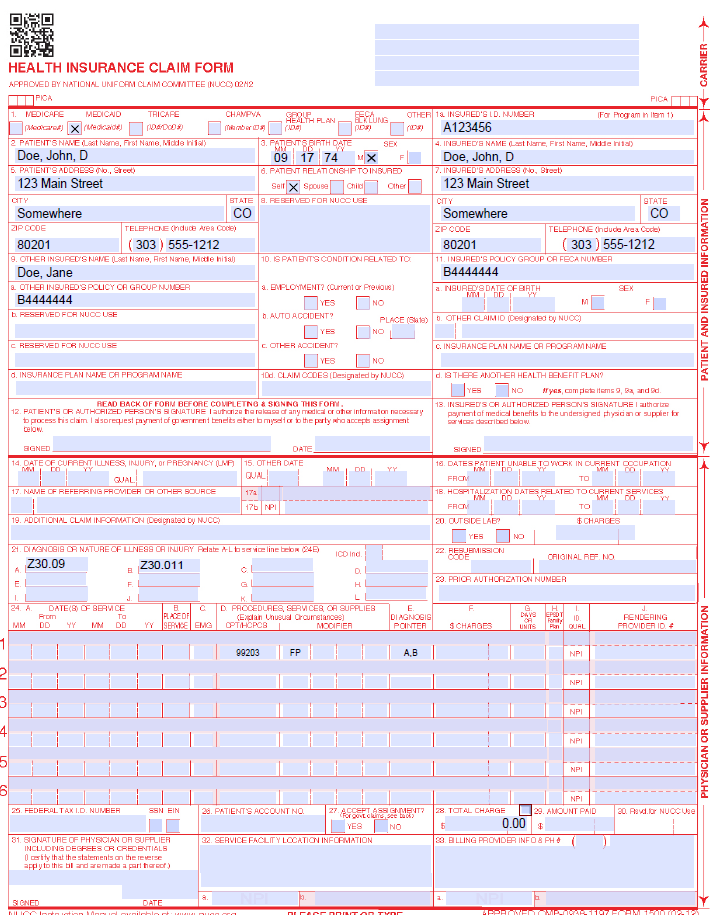
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 013125 for January 31, 2025. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 013125 for January 31, 2025. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 013125 for January 31, 2025. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | Transportation When applicable, enter the word "TRANSPORT CERT" to certify that you have a transportation certificate or trip sheet on file for this service. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left-hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | CLIA When applicable, enter the word "CLIA" followed by the number. Prior Authorization Enter the six (6)-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
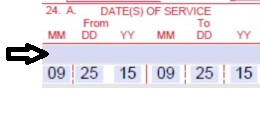
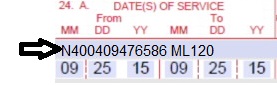
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 013125 for January 31, 2025.
or
Span dates of service
Practitioner claims must be consecutive days.
Example: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a "Y" for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. If a "Y" for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. G7 – Termination of pregnancy resulting from rape, incest, or certified by physician as life-threatening. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado-covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Anesthesia Services Anesthesia time begins when the anesthetist begins member preparation for induction in the operating room or an equivalent area and ends when the anesthetist is no longer in constant attendance. No additional benefits or additional units are added for emergency conditions or the member's physical status. Codes that define units as inclusive numbers | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the National Provider Identifier (NPI) of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 013125 for January 31, 2025. Unacceptable signature alternatives: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type (PT) is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the PT is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Reproductive Health Care Claim Example
Hospital Inpatient Billing
For hospital inpatient billing, the FP and FP+32 modifiers cannot be added to the detail level of the claim. For inpatient services, such as sterilization or Immediate Postpartum Long-Acting Reversible Contraception (IPP-LARC) device insertion, providers must use the ICD-10 diagnosis and surgical procedural (PSC) codes below to identify the family planning service.
Refer to the IPP-LARC section of the Inpatient/Outpatient Billing Manual for further IPP-LARC billing instructions.
Refer to the Immediate Post-Partum Long-Acting Reversible Contraceptives (IPP-LARCs) information under the Separate Procedures section of the Obstetrical Care Billing Manual.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Reproductive Health Billing Manual Revision Log
| Revision Date | Addition/Changes | Made by: |
|---|---|---|
| 8/25/2025 | Initial Reproductive Health Billing Manual created. | HCPF |
| 12/10/2025 | Addition of new abortion coverage billing guidance | HCPF |
| 1/5/2026 | Conversion to web format | HCPF |