Submitting a Professional Claim
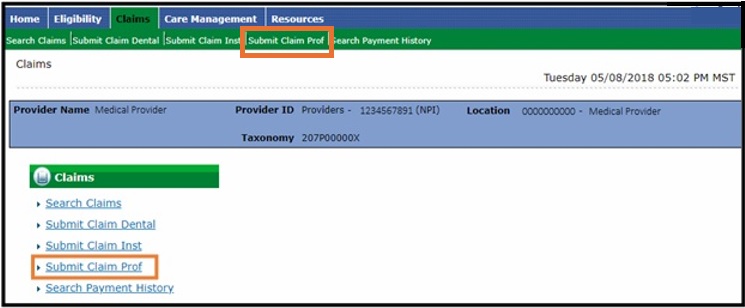
- Log in to the Provider Web Portal.
- Select Claims in the header.

- Select Submit Claim Prof.
Submit Professional Claim: Step 1 (Provider and Member Information)
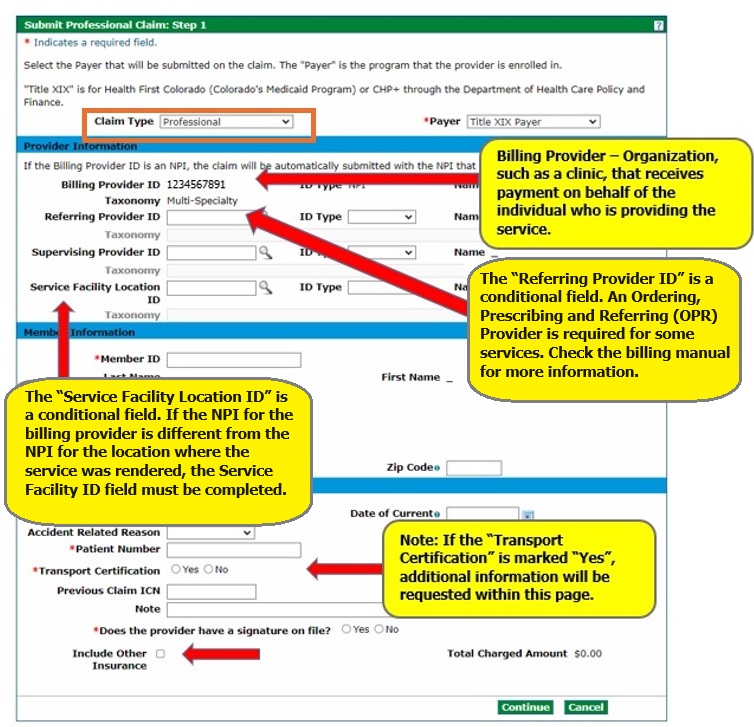
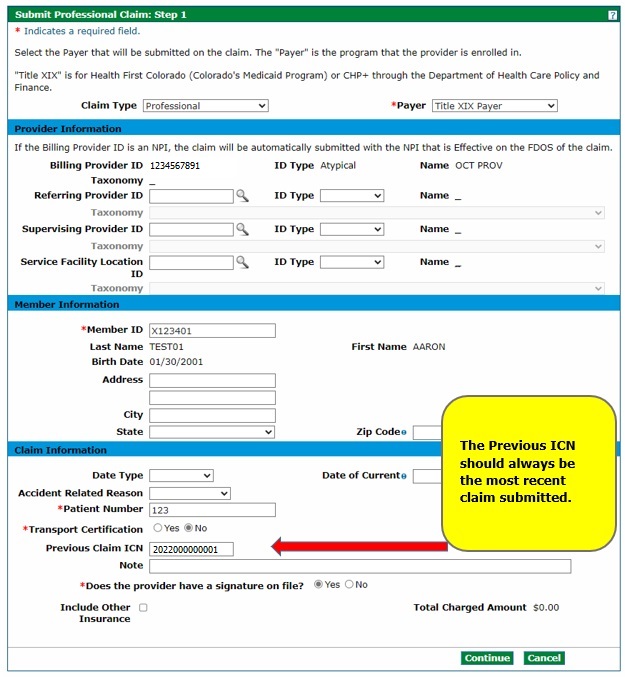
Select the "Claim Type" (Professional or Professional Crossover) and then enter the information needed for the claim on the Submit Professional Claim: Step 1 page.
Only select a claim type of Professional Crossover if there is Medicare information to enter on the claim. Professional Crossover Medicare information will be entered on the Submit Professional Claim: Step 3 panel.
The Billing Provider ID will be used for claims payment. The Provider Web Portal automatically selects the National Provider Identifier (NPI) that is effective on the "From Date" in the Service Details section and inserts that NPI into the "Billing Provider ID" field during Submit Professional Claim: Step 3 if the Billing Provider ID is an NPI.
Note: The rendering provider will be entered on the detail line.
Note that fields with red asterisks (*) may be required. Providers must include the Member ID and a patient number, which can be any number the provider assigns for internal records, on the Submit Professional Claim: Step 1 panel. A response on Transport Certification and whether the provider has a signature on file is also required. "Yes" must be selected for provider signature on file in order to continue with the claim.
Check the "Include Other Insurance" box to indicate commercial (non-Medicare) Third-Party Liability (TPL) coverage. Refer to the Entering Other Insurance or Medicare Crossover Information Quick Guide on the Quick Guides web page for more information on submitting Professional Claims with TPL and Medicare (Crossover).
Click Continue.
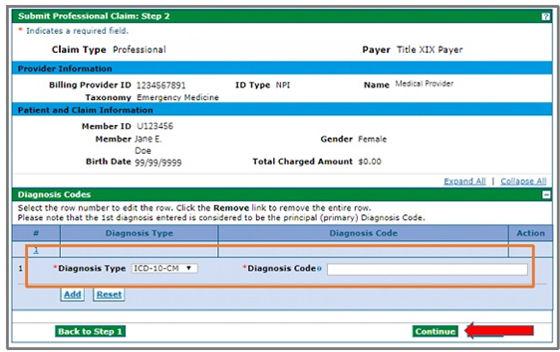
Submit Professional Claim: Step 2 (Diagnoses Details)
Enter the "Diagnosis Type" and "Diagnosis Code" information on the Submit Professional Claim: Step 2 panel under "Diagnosis Codes," and then click "Add."
Repeat to enter as many diagnosis codes as necessary.
When finished entering diagnoses, click Continue.
Submit Professional Claim: Step 3 (Service Details)
Enter service detail information under “Service Details,” and then click "Add." Note that fields with red asterisks (*) are required, including date of service, place of service, procedure code, diagnosis pointer(s), charge amount, units and unit type.
Note: A diagnosis pointer connects the service entered with the diagnoses it is intended to treat. For example, if the service entered is in relation to the first and second diagnoses listed on the Submit Professional Claim: Step 2 screen, providers would enter “1” and “2” as the diagnosis pointers. Providers may need to expand the Diagnosis Codes panel for a list of all diagnoses entered in Step 2.
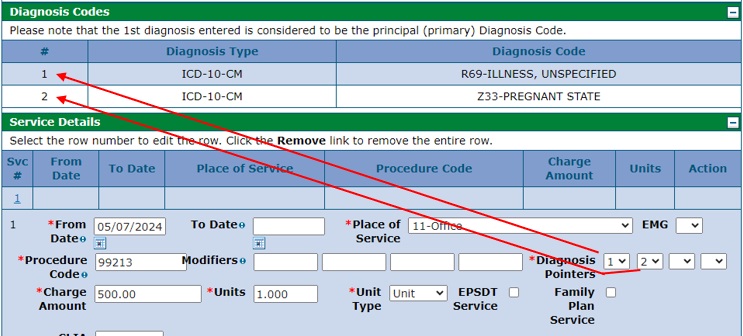
Note: Select “Y” in the EMG field if the service was rendered due to an emergency.
The Rendering Provider ID is also required. The rendering provider is the individual who performed the billed service.
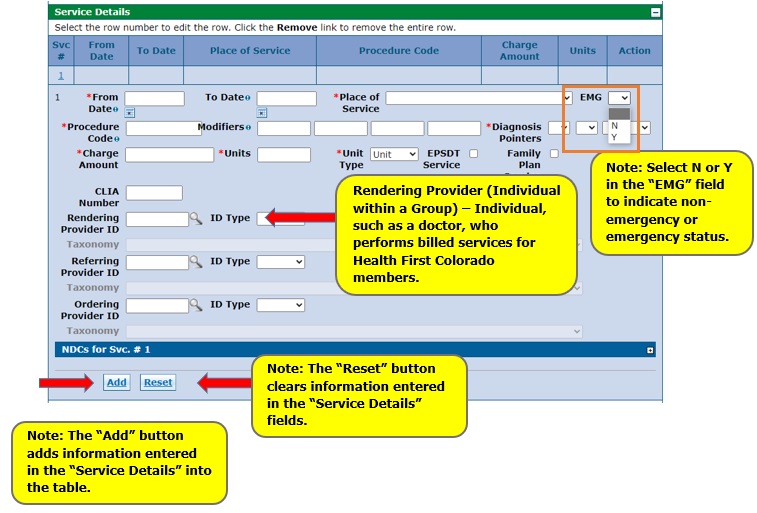
Repeat these steps to enter as many service line items as necessary.
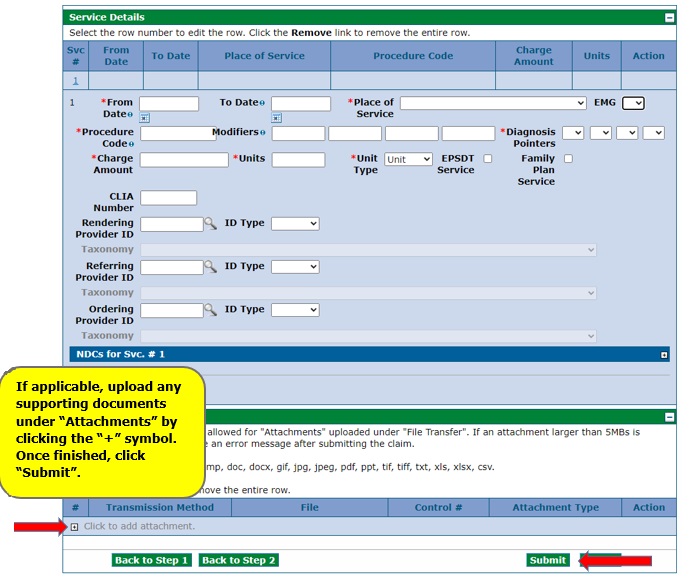
Upload any supporting documents, if applicable, under "Attachments" by clicking the "+" symbol. Note that there are very few instances when attachments are needed. Attachments are not required for Third-Party Liability Explanation of Benefits (EOBs), medical or session notes and explanations to have denied claims reconsidered.
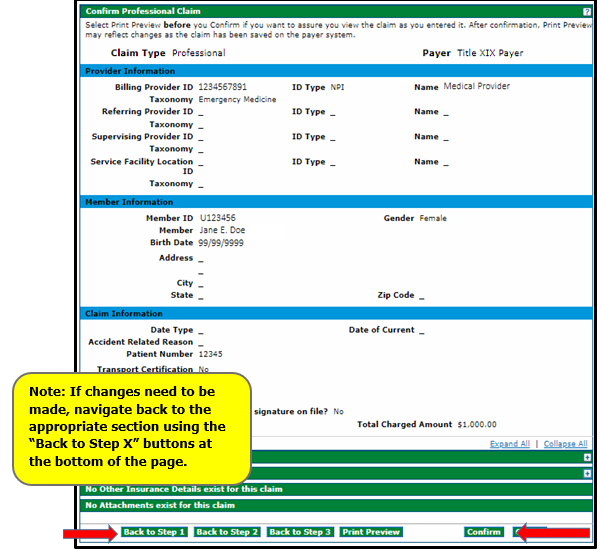
Confirm Professional Claim
Review the information entered on the Confirm Professional Claim panel, and then click Confirm.
Navigate back to the appropriate step using the "Back to Step X" buttons at the bottom of the panel if changes need to be made. Do not use the web browser's "back" button as it can cause errors on the claim.
The claim status and Claim ID (also known as the Internal Control Number or ICN) will be displayed on the Submit Professional Claim: Confirmation page. This will also appear on the Remittance Advice (RA).
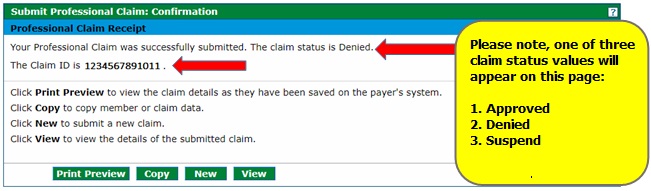
Note: A "Suspended" claim status in the Provider Web Portal means that the claim requires manual review by the fiscal agent's claims staff before a final disposition (status) can be assigned.
Suspended claims only show up once on the Remittance Advice (RA) (and not at all on the 835). The claim will not appear again on the RA until the claim either denies or pays. Once the claim is finalized, it will be reported on the RA and the 835.
Resubmitting a Claim Outside of Timely Filing
(Conditional) Enter the previous Claim ID (or Internal Control Number [ICN]) in the field “Previous Claim ICN” if resubmitting a claim after the date of service is past 365 days. Claims must be resubmitted within 60 days of the last action in order to adhere to timely filing guidelines.
Need More Help?
Visit the Quick Guides web page to find all the Provider Web Portal Quick Guides.