Residential Child Care Facility (RCCF) Program (Mental Health Program)
- Program Overview
- Billing Information
- Program Benefits
- CMS 1500 Paper Claim Reference Table
- Timely Filing
- Residential Child Care Facility Revision Log
Return to Billing Manuals Web Page
Program Overview
Health First Colorado (Colorado's Medicaid program) will no longer reimburse Residential Child Care Facilities (RCCFs) who are enrolled as Provider Type (PT) 52. Effective for dates of service July 1, 2022, only services rendered under Early and Periodic Screening, Diagnosis and Treatment (EPSDT) in accordance with Section 8.280 are a covered Residential Child Care Facility (RCCF) benefit.
Health First Colorado will only reimburse residential treatment for members when provided in a Qualified Residential Treatment Program (QRTP) or a Psychiatric Residential Treatment Facility (PRTF).
There are 2 exceptions to this policy: The Children's Habilitation Residential Program (CHRP) Waiver providers, who are enrolled as PT 52 and PT 36, may continue to submit claims for clinical services through their RCCF provider enrollment. Crisis Stabilization Units (CSUs) are the second exception.
Providers must be enrolled as a Health First Colorado provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to the Health First Colorado
The Health First Colorado reimburses providers for medically necessary medical and surgical services furnished to eligible members.
Providers should refer to the Code of Colorado Regulations, Program Rules (10 CCR 2505-10), for specific information when providing medical/surgical services.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Program Benefits
Health First Colorado mental health benefits are provided through Residential Child Care Facilities (RCCFs) to enrolled members who reside in the facility on a fee-for-service basis.
Enrollment and Participation
Almost all Health First Colorado members are enrolled in the Mental Health Programs. However, members residing in Residential Child Care Facilities can receive mental health services from physicians, licensed mental health professionals, nurse practitioners, and physician assistants. RCCFs enroll and act as billing agents by submitting claims for these provider types either employed or contracted with the RCCF.
RCCF Benefits
RCCFs are responsible for providing mental health services to members residing in their facilities.
The following procedure codes can be billed for services provided in a RCCF by a physician, osteopath, licensed psychologist, licensed clinical social worker, licensed marriage, and family therapist or licensed professional counselor:
| Code |
|---|
| 90791 or 90792 |
| +90785 |
| 90832 |
| 90834 |
| 90837 |
| 90846 |
| 90847 |
| 90853 |
| 96101 |
| 96102 |
The following procedure codes can be billed for services provided in a RCCF by a physician or osteopath:
| Code |
|---|
| +90833 |
| +90836 |
| 90839 |
| +90840 |
The following procedure code can be billed for services provided in a RCCF by a physician, osteopath, nurse practitioner or physician assistant:
| Code |
|---|
| +90863 |
RCCF Non-Included Services:
- Mental health-related prescription drugs. Claims for prescription drugs are submitted to the Health First Colorado fiscal agent under the FFS Reimbursement Program or to the MCO for MCO-enrolled members.
- Services in a Psychiatric Residential Treatment Facility (PRTF). PRTF claims are submitted to the fiscal agent for a per diem reimbursement.
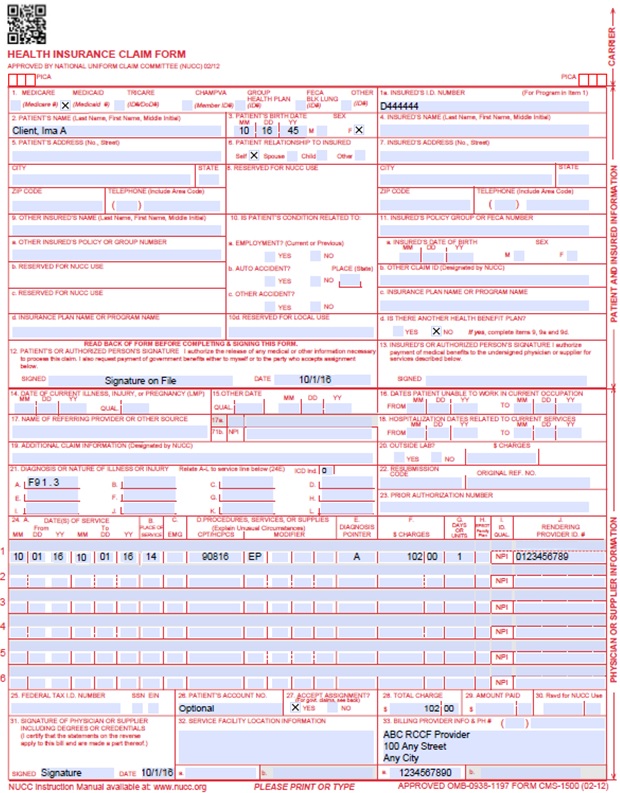
CMS 1500 Paper Claim Reference Table
The paper claim reference table lists required and conditional fields for the CMS 1500 paper claim form for RCCF claims. For complete CMS 1500 paper claim instructions, refer to the General Provider Information manual located on the Department's Billing Manuals web page.
The appropriate POS codes for RCCF paper and electronic claim submissions services are 11 (Office) or 14 (Group Home) and are identified by using the specific modifiers along with the procedure codes (see above table).
Instructions for completing and submitting electronic claims are available through the X12N Technical Report 3 (TR3) for the 837P (wpc-edi.com), 837P Companion Guide (located on the Electronic Data Interchange (EDI) Support web page of the Department's website), and in the Provider Web Portal User Guide (via within the Provider Web Portal).
| CMS Field Number & Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | |||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Not Required | |||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010116 for January 1, 2016.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. The Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not Required | |||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form.
| ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1)procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area)
Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Not Required | |||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
Residential Child Care Facility Claim Example
Timely Filing
For more information on timely filing policy, including the resubmission rules for denied claims, refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu.
RCCF Revisions Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 12/1/2016 | Updated for new Fiscal Agent | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 2/9/2018 | Removed NDC supplemental qualifier - not relevant for RCCF providers | DXC |
| 6/25/2018 | Updated billing and timely filing to point to general manual | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 2/12/2020 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 7/6/2022 | Update RCCF coverage to reflect regulation | HCPF |