Qualified Residential Treatment Program Billing Manual
- General Policies
- Program Overview
- Billing Information
- Program Benefits
- Critical Incident Reporting
- CMS 1500 Paper Claim Reference Table
- Timely Filing
- QRTP Revision Log
Return to Billing Manuals Web Page
General Policies
- Health First Colorado (Colorado's Medicaid program) members have their behavioral health services paid for by Regional Accountable Entities (RAEs). Regional Accountable entities are managed care entities responsible for covering behavioral health benefits for nearly all Health First Colorado members.
- See Program Rule 8.212 for details about the RAE program, including policy which exempts Health First Colorado members from RAE coverage. Only a small percentage of members meeting very specific criteria will be exempt. Member exemption is determined by the Department.
- Residential services for children or youth in the custody of the Colorado Department of Human Services -Division of Child Welfare or Division of Youth Services are among the members exempted from RAE coverage by Program Rule 8.212.
- Visit the Health First Colorado Regional Organizations web page for details about RAE coverage.
- To verify if a Health First Colorado member's behavioral health services are covered by an RAE, providers must perform a member eligibility query in the Provider Web Portal. Each RAE may have its own similar tool for providers to query member eligibility. Both tools are valid for checking member eligibility.
The member eligibility query will display whether the RAE is responsible for covering the member's services. If the member is covered by the RAE, all claims for covered behavioral health services must be sent to the RAE for payment. - All behavioral health providers must be enrolled with Health First Colorado and contracted with the RAE. Providers must contact the RAE which serves their region to begin the enrollment process. Visit the Health First Colorado Regional Organizations web page for details.
- Providers who are denied RAE enrollment may not bill Gainwell Fee-For-Service (FFS) as an alternative reimbursement route. Providers denied RAE enrollment may not treat Health First Colorado members for services covered by the RAE.
- Providers who are denied RAE enrollment may still render and be reimbursed for services not covered by the RAE.
- Providers must reference the State Behavioral Health Services Billing Manual for a list of RAE-covered services and conditions.
- Billing information included below is only applicable to services rendered to children or youth in the custody of the Colorado Department of Human Services -Division of Child Welfare or Division of Youth Services, who are not covered by the RAE.
Program Overview
Qualified Residential Treatment Programs (QRTP) means a facility that provides residential trauma-informed treatment that is designed to address the needs, including clinical needs, of children with serious emotional or behavioral disorders or disturbances. As appropriate, QRTP treatment facilitates the participation of family members in the child’s treatment program, including siblings, and documents outreach to family members, including siblings. Providers must be enrolled as a Health First Colorado provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to the Health First Colorado
Health First Colorado reimburses providers for medically necessary services furnished to eligible members.
Providers should refer to the Code of Colorado Regulations Program Rules (10 CCR 2505-10) for specific information when providing medical/surgical services.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
The Residential Provider Billing and Policy slides are available online.
Program Benefits
Health First Colorado benefits are provided through Qualified Residential Treatment Programs (QRTPs) to enrolled members who reside in the facility on a per-diem basis. Health First Colorado benefits are provided through Qualified Residential Treatment Programs (QRTPs) to enrolled members who reside in the facility on a per-diem basis. The per diem rate includes medically necessary services included in the member’s stabilization plan created by the QRTP in accordance Colorado Department of Human Services (CDHS) regulations, as well as services included in the member’s individual child and family plan created by the QRTP in accordance with CDHS regulations. These services include but are not limited to: medication administration and oversight, and individual, group, and family therapy. Services included in the per diem rate may not be billed by outside providers.
The following services are not covered for members in a QRTP: room and board, educational, vocational, and job training services, recreational or social activities, and services provided to inmates of public institutions or residents of Institutions of Mental Disease (IMD). 10 CCR 2505-10 8.765.
Physical and dental health services, as well as behavioral health services not included in the per diem rate, such as substance use disorder treatment, may be billed by an outside provider to the appropriate payor (RAE or the Department). 10 CCR 2505-10 8.765 and 10 CCR 2505-10 8.280.
Children and Youth Mental Health Treatment Act (CYMHTA) clients, who are also Health First Colorado members, are assessed with the CYMHTA assessment in place of the Enhanced Standardized Assessment (ESA). QRTP treatment for qualifying CYMHTA clients is eligible for per diem reimbursement. Providers may submit claims as described below.
Prior Authorization and Utilization Management (UM) Requirements
QRTP services are subject to UM approval. UM and Enhanced Standardized Assessment (ESA) requirements are located in Operational Memo (OM) 25-032 located on the 2025 Memo Series web page under 2025 Operational Memos
QRTP Benefits
QRTPs are responsible for providing behavioral mental health services to members residing in their facilities.
The following procedure codes can be billed for services provided in a QRTP:
| Code | Description | Modifier |
|---|---|---|
| H0019 | Behavioral health; long-term residential, without room and board, per diem (1 unit per day) | U1 |
QRTP Non-Included Services:
- Behavioral health-related prescription drugs. Claims for prescription drugs are submitted to the Health First Colorado fiscal agent under the FFS Reimbursement Program or to the MCO for MCO-enrolled members.
- Services in a Psychiatric Residential Treatments Facility (PRTF).
- Room and board
The following days are not billable:
- The day of discharge.
- Days when the client is in detention.
- Days when the client receives none of the services included in the per diem rate due to elopement.
Days the client spends away from the facility, due to an M1 hold or a temporary pass, but still receiving covered services, are billable for up to 4 days.
Critical Incident Reporting
QRTPs are required to submit all critical incident reports that involve Health First Colorado (Colorado’s Medicaid program) members to the Department of Health Care Policy and Financing (the Department). This requirement does not replace or supersede any existing reporting requirements for other state agencies or departments.
All critical incidents, as defined in the Colorado Department of Human Services (CDHS) rule at 12 C.C.R. 2509-8: 7.701.2, must be reported to the Department for Health First Colorado members only, with non-member information being anonymized.
CDHS rule at 12 C.C.R. 2509-8: 7.701.2 states that critical incidents include death, abuse and neglect, injury, illness, and emergency response. See the rule text for further details and explanation.
Providers must follow all critical incident reporting and timing requirements as described in CDHS rule at 12 C.C.R. 2509-8: 7.701.52 when reporting to the Department. CDHS rule at 12 C.C.R. 2509-8: 7.701.52 states that critical incidents must be reported within 24 hours, excluding weekends and holidays, of the occurrence of a critical incident at the facility or within 24 hours of a child’s return to the facility.
Critical Incidents must be submitted to the Department via the Residential Childcare Provider Critical Incident Information Form.
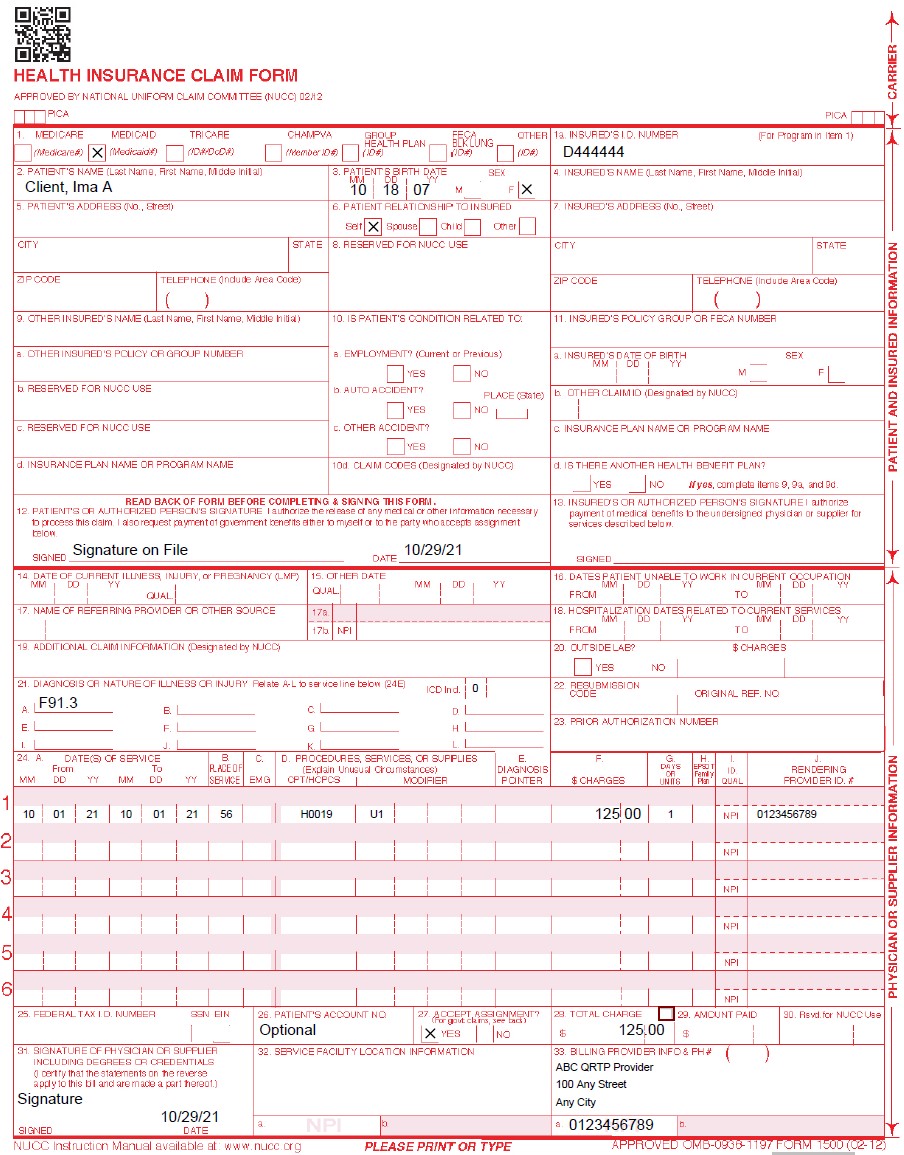
CMS 1500 Paper Claim Reference Table
The paper claim reference table lists required and conditional fields for the CMS 1500 paper claim form for QRTF claims. Refer to the General Provider Information manual located on the Department's Billing Manuals web page. for complete CMS 1500 paper claim instructions.
The appropriate POS code for QRTP paper and electronic claim submissions services is 56 (Psychiatric Residential Treatment Center) and is identified by using the specific modifiers along with the procedure codes (see above table).
Instructions for completing and submitting electronic claims are available through the X12N Technical Report 3 (TR3) for the 837P (wpc-edi.com), 837P Companion Guide (located on the Electronic Data Interchange (EDI) Support web page of the Department's website), and in the Provider Web Portal User Guide (via within the Web Portal).
The “Rendering Provider” NPI should refer to the enrolled, Licensed Behavioral Health Professional responsible for overseeing the care of the member associated with the claim.
| CMS Field Number & Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | |||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Not Required | |||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than twelve diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010116 for January 1, 2016.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. The Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not Required | |||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form.
| ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area)
Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. Refer to the guidance above. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Required | Federal Tax Number must match the one associated with the provider’s enrolled NPI number. | ||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Not Required | |||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Conditional | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. If the Service Facility location is the same address as that reported in the Billing Provider Name, the Service Facility Location must not be sent. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
Qualified Residential Treatment Program Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
QRTF Revision Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 10/1/2021 | Created new benefit | HCPF |
| 10/29/2021 | Place of Service and Payment Limits update | HCPF |
| 12/8/2021 | Updated Billing Guidance and Reference Table | HCPF |
| 07/22/2022 | DYS and ARD Billing Guidance added | HCPF |
| 12/16/2022 | Per diem clarification | HCPF |
| 12/22/2022 | Per diem medication clarification | HCPF |
| 1/6/2023 | CYMHTA edits | HCPF |
| 3/27/2023 | Updated AWS URL Links | HCPF |
| 4/7/2023 | Added link to Provider webinar and slides | HCPF |
| 12/7/2023 | Update claim instructions | HCPF |
| 3/31/2025 | Critical Incident Reporting | HCPF |
| 10/24/2025 | Utilization Management and Enhanced Standardized Assessment information added | HCPF |