Pediatric Personal Care Benefit Billing Manual
- Personal Care Benefit Overview
- Billing Information
- Eligible Providers
- Prior Authorization Requests (PARs)
- Claim Submission
- CMS 1500 Paper Claim Reference Table
- Timely Filing
- Pediatric Personal Care Specialty Manual Revisions Log
Return to Billing Manuals Web Page
The purpose of this billing manual is to provide policy and billing guidance to providers to obtain reimbursement for personal care services. This manual is updated periodically to reflect changes in policy and regulations. It applies only to the Health First Colorado (Colorado's Medicaid program) Pediatric Personal Care benefit and does not address services available through other Health First Colorado benefits or any services available through Home and Community-Based Services (HCBS) waiver programs.
Personal Care Benefit Overview
The Pediatric Personal Care benefit is available to Health First Colorado members 20 years old and younger who require Personal Care (PC) services.
PC services are medically necessary services that do not require a provider to have a medical certification or a professional license to safely provide services. Under this benefit, a PC provider assists the Health First Colorado member with PC tasks in order to meet his or her physical, maintenance, and supportive needs. This assistance may take the form of hands-on assistance (actually performing a task for the person), supervision (ensuring a task is performed safely, including active intervention), or prompting or cueing the member to complete the task.
If a member requires support of a medically skilled caregiver to complete a task, such as bathing or hygiene, the associated task shall be considered skilled in nature and covered under other Health First Colorado state plan benefits and/or Colorado HCBS waiver programs.
Waiver Case Managers must collaborate with Pediatric PC providers to ensure that Prior Authorization Requests (PARs) are submitted correctly and on time to prevent overlap or omission of authorized PC units between the Medical PAR and Waiver PAR.
PC providers must work with the member's case manager to ensure that any current PARS for these services are cancelled or modified prior to starting services under the Health First Colorado fee for service program.
Refer to the Personal Care Benefit Coverage Standard for additional information about this benefit, including eligibility rules for providers, details about what tasks are covered and interaction with other Health First Colorado programs.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information.
Ordering, Prescribing and Referring (OPR) Providers
Effective July 1, 2022, the Department of Health Care Policy & Financing (the Department) began enforcing the federal requirement 42 CFR § 455.440, which requires that all claims for Home Health services include the National Provider Identifier (NPI) of the provider who ordered the service and 42 CFR 455.440, that requires the NPI is associated with an actively enrolled Health First Colorado provider.
Providers are required to enter the NPI of the ordering provider into the following locations for claim submission. This field may be labeled "Referring Provider" in the Provider Web Portal.
Professional claims
- Paper claims use field 17.b.
- Electronic submissions use loop 2420 with qualifier DK (Ordering) DN (Referring) or DQ (Supervising).
Pediatric Personal Care services can be ordered by either a physician or an allowed practitioner. Allowed practitioners are defined in accordance with State law as Physician Assistant (PA), Nurse Practitioner (NP) or Clinical Nurse Specialist (CNS). The ordering provider must also be actively enrolled with Health First Colorado. The claim will be denied if these conditions are not met.
Providers should refer to the Ordering, Prescribing and Referring Claim Identifier Project web page or Program Rule 10 CCR 2505-10 8.125.8.A for further information.
Eligible Providers
Prescribing/Ordering Providers
- Physician, either a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO)
- Advanced Practice Nurse (APN)
Note: Under the Centers for Medicare & Medicaid Services (CMS) Conditions of Participation, all 485 Plans of Care – or other form with identical content – must be signed by an MD, DO or APN.
Rendering and Billing Provider Numbers
Personal Care services must be billed using the 837 Professional (837P) transaction or CMS 1500 form, which requires using rendering provider identification numbers.
Class B agencies billing for PC services through Online Portal must enter their billing NPI number in the Rendering Provider ID field on the Detail Line Items tab or in line 24J of the CMS 1500 Professional claim form.
Each agency’s specific billing number will be used to reimburse the claim.
Prior Authorization Requests (PARs)
The ColoradoPAR Program is Health First Colorado’s Utilization Management (UM) Program. A third-party vendor reviews Prior Authorization Requests (PARs) to ensure services requested meet medical necessity guidelines and are within Health First Colorado’s policies.
The ColoradoPAR Program’s third-party vendor processes electronic PARs through an online PAR portal. The online PAR portal is a web-based HIPAA-compliant PAR system that offers providers 24/7 access to the information and functions providers need. Clinical documentation will be accepted in the following formats: doc, docx, xls, xlsx, ppt, pdf, jpg, gif, bmp, tiff, tif, and jpeg.
Visit the ColoradoPAR web page for information and instructions on how to submit PARs electronically through the online PAR portal. For additional assistance or support, contact the ColoradoPAR provider helpline at 888-801-9355. PAR status may be verified in the online PAR portal or by contacting the ColoradoPAR provider helpline. The approved PAR identification number must be submitted with the claim to receive payment.
Claims for prior authorized services must be submitted within 365days of the date of service. Services rendered prior to the authorized date will be denied reimbursement.
Approval of the PAR does not guarantee payment by Health First Colorado. The member and the PC provider shall meet all applicable eligibility requirements at the time services are rendered and services shall be delivered in accordance with all applicable service limitations. Health First Colorado is the payer of last resort and the presence of an approved or partially approved PAR does not release the agency from the requirement to bill Medicare or other third-party insurance prior to billing Health First Colorado.
PAR Requirements
- Any provider submitting a PAR must be enrolled in the Health First Colorado Program. Providers must also verify eligibility at the time service is rendered and include the necessary information with the PAR.
- All PC services require prior authorization by Health First Colorado's third-party vendor using the approved prior authorization request online portal.
- The PAR is comprised of a completed Personal Care Assessment Tool (PCAT), the physician's orders, and the Plan of Care:
- The PCAT can be completed by a Class A or B agency
- PC services must be ordered in writing by the member's prescribing provider as part of a written Plan of Care
- The prescribing provider's order and signed Plan of Care must be submitted with the PCAT as part of the PAR
- It is the agency's responsibility to provide sufficient documentation to support the medical necessity for the requested services.
- PC services PARs may be submitted for up to a full year of anticipated services unless:
- The member is not expected to need a full year of services
- The member's eligibility is not expected to span the entire year or,
- As otherwise specified by Health First Colorado.
- PARs must be submitted to Health First Colorado's third-party vendor in accordance with 10 CCR 2505-10 § 8.058.
- A PAR will be pended by Health First Colorado's third-party vendor if all of the required information is not provided in the PAR, or additional information is required by the third-party vendor to complete the review. If the third-party vendor does not receive the required documentation within four (4) business days, the PAR will be denied for lack of information.
- When a PAR includes a request for reimbursement for two (2) staff members at the same time (excluding supervisory visits) to perform two-person transfers or another PC task, documentation supporting the need for two (2) people and the reason adaptive equipment cannot be used must be included.
- All other information determined necessary by Health First Colorado's third-party vendor to make a decision on the medical necessity and appropriateness of the proposed treatment plan must be included.
- The agency is required to submit a PAR revision, which must include revisions to all documentation, including the Plan of Care, if/when the member experiences a change in condition necessitating a change in the amount, duration, or frequency of a member's PC services.
- When a member receiving PC services through Health First Colorado receives additional PC services through a Home and Community-Based Services (HCBS) waiver, the HCBS waiver program is considered the payer of last resort.
- The PAR will be reviewed by medical experts in children's health who work for the Health First Colorado program's third-party vendor. Nurses and doctors will decide if the request for personal care meets the rules for medical necessity and for the Personal Care Benefit.
- An approved PAR is valid for up to one (1) year. After one (1) year, a Personal Care provider must submit a new PAR for another year of PC services.
Peer-to-Peer and Reconsideration Process
Prior to denying or partially denying a PAR, the MD, DO or APN that requested the PAR will be contacted to discuss the PAR over the phone in a process called a Peer-To-Peer review. If the Peer-To-Peer review still results in a denied or partially denied PAR, the Personal Care provider may work with the MD, DO or APN on these two (2) options:
- PAR Reconsideration: A PAR Reconsideration is similar to a second opinion and must be requested by the Personal Care provider. A MD, DO or APN who is different from the one who made the initial PAR denial will re-review the PAR along with the new information and make a final PAR decision. Additional documents not submitted with the original request may be submitted during the Reconsideration process.
- PAR Resubmission: Submit a new PAR that includes additional medical information needed for the PAR review.
The provider will be notified of the final PAR determination via the online PAR portal. The provider and member will receive the final PAR determination letter from the Department’s fiscal agent. If the PAR is denied, the provider will also receive a detailed explanation of why the PAR was denied. A member who receives a denial notification letter has the option to submit a written request for an appeal to the Office of Administrative Courts.
Claim Submission
Pediatric Personal Care Benefit Procedure Code Table
Providers may bill the following procedure codes for Pediatric Personal Care services:
| Pediatric Personal Care Benefit Procedure Code Table | ||
| Description | Procedure Code | Units |
| Personal Care services, per 15 minutes, not for an inpatient or resident of a hospital nursing facility, icf/mr or imd, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant). | T1019 | 1 unit = 15 minutes |
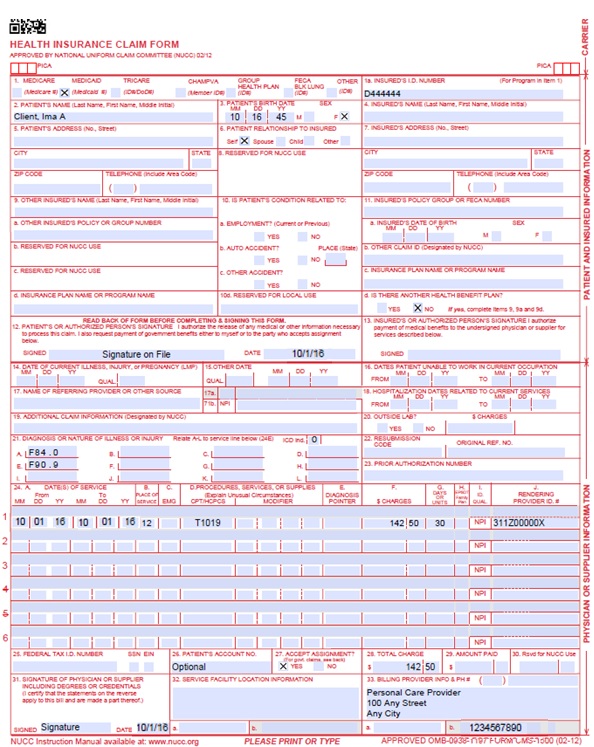
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number & Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an “X” in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured’s ID Number | Required | Enter the member's seven-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two digits for the month, two digits for the date, and two digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked “YES”, enter the insured’s last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Not Required | When appropriate, place an "X" in the correct box to indicate whether one or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | |||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Required | OPR NPI Number is required in accordance with Program Rule 10 CCR 2505-10 8.125.8.A. | ||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Conditional | Complete for services provided in an inpatient hospital setting. Enter the date of hospital admission and the date of discharge using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070115 for July 1, 2015. If the member is still hospitalized, the discharge date may be omitted. This information is not edited. | ||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one but no more than twelve diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six lines of information on the paper claim. If more than six lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two dates: a “From” date of services and a “To” date of service. Enter the date of service using two digits for the month, two digits for the date and two digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
EPSDT | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Conditional | Enter a “Y” for YES or leave blank for NO in the bottom, unshaded area of the field to indicate the service is rendered for a life-threatening condition or one that requires immediate medical intervention. If a “Y” for YES is entered, the service on this detail line is exempt from co-payment requirements. | ||||||||||||||||||||||||||||||||||||
| 24D. | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of 4 characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. Anesthesia Services Anesthesia services must be reported as minutes. Units may only be reported for anesthesia services when the code description includes a time period. Anesthesia time begins when the anesthetist begins member preparation for induction in the operating room or an equivalent area and ends when the anesthetist is no longer in constant attendance. No additional benefit or additional units are added for emergency conditions or the member’s physical status. The fiscal agent converts reported anesthesia time into fifteen-minute units. Any fractional unit of service is rounded up to the next fifteen-minute increment. Codes that define units as inclusive numbers Some services such as allergy testing define units by the number of services as an inclusive number, not as additional services. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early & Periodic Screening, Diagnosis, and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available - Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) Not Required | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent.
| ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
Pediatric Personal Care Claim Example
Timely Filing
Refer to the General Provider Information Manual available on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
Pediatric Personal Care Specialty Manual Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE |
| 6/27/2018 | Updated billing information and timely filing, removed redundant information found in the General Provider Information manual | HCPF |
| 7/2/2018 | Minor style and consistency edits | DXC |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 1/22/2020 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 12/11/20 | Updated claims for PAR submission to 365 days from 120 | HCPF |
| 9/11/2023 | Added Ordering, Prescribing, Referring (OPR) Policy. Updated field #17 on claim reference table, corrected punctuation and spacing errors. | HCPF |