Entering National Drug Code (NDC) Information on Claims
The information below provides guidance for entering National Drug Code (NDC) information on a claim. A professional claim (CMS 1500) is used to illustrate this example including screen shots.
Attention:
Refer to Appendix X - HCPCS / NDC Crosswalk for Billing Physician-Administered Drugs located on the Billing Manuals web page under the Appendices drop-down for the most current list of HCPCS codes and corresponding NDC numbers for use in billing physician-administered drugs.
A code must be present in the crosswalk before it can be used in a claim on the Web Portal. If the NDC is not found in the crosswalk, claims should be submitted via batch or paper.
The NDC is a unique product identifier used in the United States for drugs intended for human use. The Drug Listing Act of 1972 requires registered drug establishments to provide the Food and Drug Administration (FDA) with a current list of all drugs manufactured, prepared, propagated, compounded, or processed by it for commercial distribution. Drug products are identified and reported using the NDC.
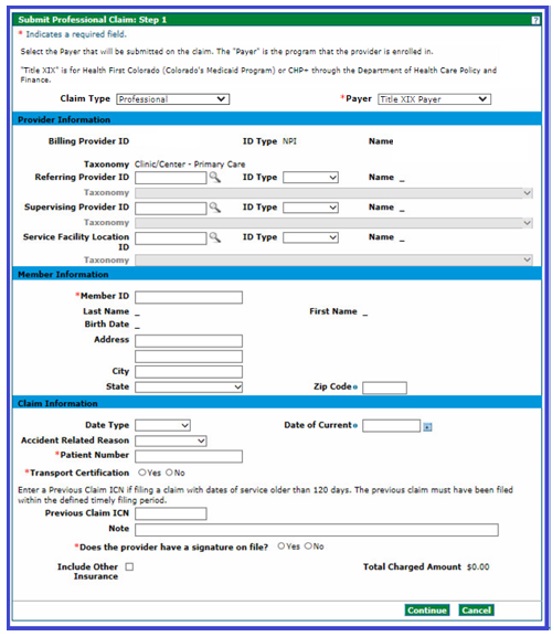
- Enter the information needed for the claim on the Submit Professional Claim: Step 1 page and select Continue. Note: Selecting a payer is a required field. The Payer is the program that the provider is enrolled in. Title XIX is for Health First Colorado (Colorado’s Medicaid program) or Child Health Plan Plus (CHP+) through the Department of Health Care Policy & Financing (the Department).
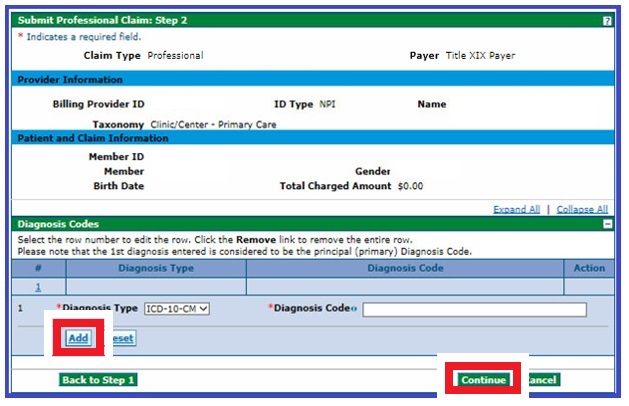
- Enter the diagnosis type and diagnosis code on the Submit Professional Claim: Step 2 panel in the Diagnosis Codes section and click Add.
- Click Continue.
- Click the [+] to expand the NDC section on the Submit Professional Claim: Step 3 panel.
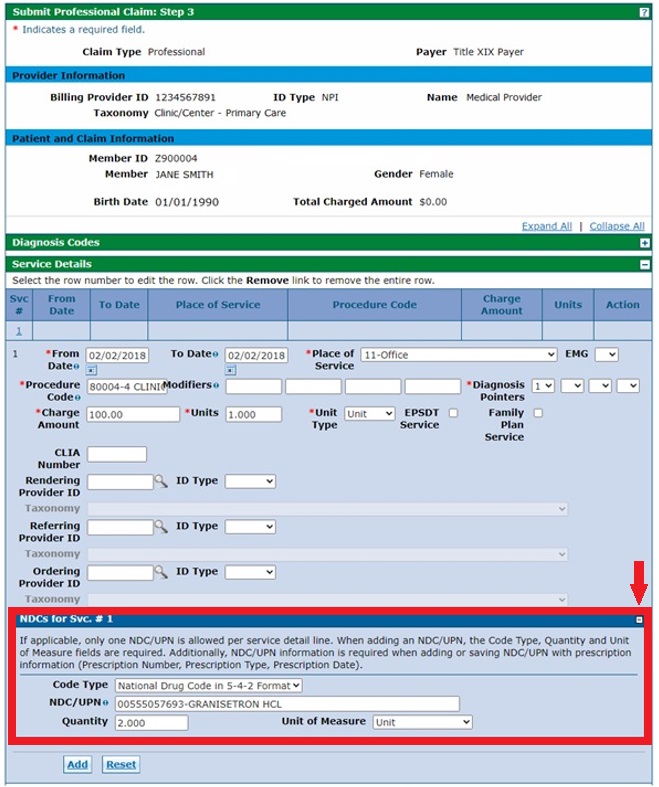
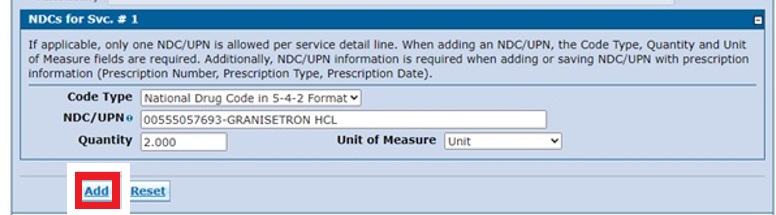
- Enter the information in the Service Details and NDCs for Svc # 1 sections. Note: NDCs are entered per service detail as applicable. Click Add when finished.
Need More Help?
Visit the Quick Guides web page to find all the Provider Web Portal Quick Guides.