Early Intervention Billing Manual
- Early Intervention Services (EI)
- Allowable Early Intervention Services
- Allowable Early Intervention Providers
- Targeted Case Management (TCM)
- Frequently Asked Questions (FAQs)
- Billable Activities
- Non-Reimbursable Targeted Case Management Services
- Other Health First Colorado Covered Services
- Natural Environments
- Early Intervention Procedure Code Table
- Procedure Code Table
- Early Intervention Paper Claim Reference Table
- Timely Filing
- Early Intervention Revisions Log
Return to Billing Manuals Web Page
Early Intervention Services (EI)
Early Intervention Services provides developmental supports and services to children birth to three (3) years of age* who have either a significant developmental delay or a diagnosed condition that has a high probability of resulting in a developmental delay and are determined to be eligible for the program.
*Some children remain in early intervention until Preschool Special Education services begin
Targeted Case Management (TCM) Services are provided through the Early Intervention Service Broker for children actively enrolled in Early Intervention Services program and Health First Colorado (Colorado's Medicaid program).
Allowable Early Intervention Services
General Definition
Allowable Early Intervention Services are those services that are:
- Designed to meet the developmental needs of an infant or toddler with a significant developmental delay or the needs of the family related to enhancing the infant's or toddler's development
- Selected in collaboration with the infant's or toddler's family
- Provided in conformity with an Individualized Family Service Plan (IFSP)
- Based on appropriate evidence-based practices and related to functional outcomes
- Provided under public supervision to assure, through monitoring, that services are provided in accordance with these requirements
- Provided by qualified personnel as defined in Colorado's Part C State Plan
- Provided in the natural environments of the infant or toddler and the family including the family's home and/or community settings in which infants and toddlers without disabilities participate, unless otherwise justified on the IFSP
- Provided in a culturally relevant manner, including the use of an interpreter if needed
Role of Service Providers
All Early Intervention service providers are responsible for:
- Consulting with parents, service coordinators, other service providers and representatives of other community agencies where the infant or toddler participates to ensure the effective provision and coordination of Early Intervention Services
- Billing Health First Colorado appropriately for services rendered when the service is a benefit of Health First Colorado
- Completing all required Prior Authorization requests for Health First Colorado covered services in a timely manner
- Collaborating with service coordinators when recommending referrals for other professional services
Allowable Early Intervention Providers
Early Intervention Service Brokers can become billing agents, if they choose, for EI service providers. The Department of Health Care Policy & Financing (the Department) does not regulate who can act in the capacity of billing agent. To bill a fee-for-service code, the provider must be approved to provide that service.
Once the provider has provided a service, the billing agent can bill using the rendering provider's Health First Colorado National Provider Identifier (NPI) number in both the billing and rendering fields. The Early Intervention Service Brokers cannot pay additional money to the providers for the service that they are billing Health First Colorado for (e.g., if the reimbursement for a code is $60 from Health First Colorado and the Early Intervention Service Broker generally pays $75 to non-Health First Colorado providers, they can't pay the $15 difference to the provider). When a provider signs up to become a Health First Colorado provider, he/she signs a contract agreeing to accept the Health First Colorado payment for the services he/she bills. However, if the Early Intervention Service Broker wants to pay for additional services not covered by Health First Colorado, such as transportation to and/or from the member’s house that is up to each Early Intervention Service Broker and provider to decide between them.
Health First Colorado does not regulate who can fill out the provider application. Early Intervention Service Broker staff can choose to fill out the Health First Colorado application for providers. The provider is still responsible for reading the application and signing it.
Targeted Case Management (TCM)
TCM is an optional Health First Colorado benefit for members who have been determined by an Early Intervention Service Broker to have a developmental disability and are actively enrolled in Early Intervention Services. The purpose of case management is:
- Facilitate Enrollment
- Service Plan Development
- Service Monitoring
- Coordination of Services/Benefits which include but is not limited to: Educational, Mental Health, Emotional, Social, Medical
- Ensure Non-Duplication of Services
These activities include, but are not limited to:
- Locating, coordinating, and monitoring needed developmental disabilities services
- Coordinating with other non-developmental disabilities funded services to ensure non-duplication of services
- Monitoring the effective and efficient provision of services across multiple funding sources
Activities will not:
- Restrict members to a limited provider set. Members may choose any willing Health First Colorado provider for Health First Colorado services
- Limit case management services provided in a manner consistent with the member's best interest
- Be used to restrict a member's access to other services
- Compel members to receive case management services
- Be used as a reason for case managers to deny other State Plan services
Frequently Asked Questions (FAQs)
Is a physician’s prescription required in order to bill the T1026 code for EI evaluations conducted for children enrolled in Medicaid?
- No, a physician’s prescription is not required in order to bill T1026 for EI evaluations conducted for children.
Do providers need to bill primary insurers before they bill Medicaid?
- Yes. Please note that Health First Colorado is the payor of last resort. If a member has primary health coverage through a third party, such as a commercial or individual policy, the member must utilize that primary third-party coverage prior to utilizing Medicaid services (10 CCR § 2505-10:8.061.4). If a member fails to comply with the primary health coverage requirements, the member will be liable to the provider for the health services and Medicaid will not be liable (§ 8.061.5, C.R.S. § 25.5-4-301(1)(a)(III)(A)).
- If a provider who is not enrolled into the member's primary health coverage knowingly provides health services to a Medicaid member, neither the member nor Medicaid will be liable for the costs of services unless the member and the provider entered into a written agreement in which the member agrees to pay for items provided or services rendered that are outside of the network or plan protocols (C.R.S. § 25.5-4-301(1)(a)(III)(B)).
What are the allowed Place of Service (POS) codes for EI evaluations?
- The current allowed POS codes for EI evaluations are: 02, 10, 11, 12, 20.
Will use of EI codes require Electronic Visit Verification (EVV)?
- Refer to the EVV Program Manual which lists all benefits which require EVV.
When billing for an EI Evaluation using the code T1026, what fields must be completed when billing?
- The Order, Prescribing, and Rendering (OPR) provider must be present, along with two (2) separate NPI numbers.
Billable Activities
Comprehensive Assessment and Periodic Reassessment
- Determine need for: Medical, Educational, Social, or other EI Services
Service Plan Development based on information collected through assessment
- Specifies goals for meeting all service needs
- Activities to ensure member participation
- Work with individual and others to develop goals
Service and Support Coordination
- Coordination of the services being provided in the Service Plan to ensure continuity of service provision
- Help individuals obtain needed services and activities and link them to the appropriate provider
Activity TCM activity that is being performed
- Multiple related activities or activities performed within a single day should be entered into a single log note
- Must be a billable activity
- Type of contact can be Direct or Indirect, however, length of activity must be at least 7.5 minutes in order to bill one (1) unit. Voice mails left or received, or emails sent and received are not an acceptable way to bill for one (1) unit.
In order to meet federal regulations related to billing of TCM services, providers who bill TCM services shall have the "EI Fundamentals & Education/Experience" box in the Early Intervention Data System. Providers who bill without this box checked will be referred to HCPF Program Integrity.
Non-Reimbursable Targeted Case Management Services
Activities that may be a service coordination responsibility but are not reimbursed as TCM services are those activities either paid through the "Early Intervention Contract", personnel costs, indirect costs, or a service to be paid by third party or activities that are built into the rate structure for TCM services. The list below is not exhaustive:
- Intake and initial eligibility determination for the EI Colorado Program
- Preparation for and participation in the dispute resolution processes in accordance with Federal Part C Regulations of the IDEA (34 C.F.R. Part 303) procedural safeguards
- Assessment costs for determining the individual's need for a physical or psychological examination or evaluation
- Payment for the costs of the administration of other services or programs to which a recipient is referred (e.g., educational services), general administrative programs of the Health First Colorado program
- The provision of any medical treatment or service
- Service coordination staff meetings not related to individual child and family reviews
- Completing time sheets or billing documents, billing Health First Colorado for services which are included in the cost of doing normal business.
- Discharge planning from an institution or hospital
- Administrative activities such as eligibility determination, screening, intake outreach and utilization review
- Care coordination or case management activities covered by Health First Colorado in the ACC and Healthy Communities programs
- Formal policy advocacy and developing new provider resources
- Service coordination training and personnel development
- Prior authorization of services
- Services which are provided by a staff person who has not completed the appropriate training to meet the requirements for the EI Fundamentals &Education/Experience box to be checked in the Early Intervention Data System
- Recreational events provided by the Broker when no service coordination activity is provided
- Fund raising activities for the Broker
- Voice mail messages (should be combined together with other approved activities to form one [1] note)
- Multiple case managers or supervisors in a single meeting, only one (1) person can bill for the meeting
- Supervisors cannot bill for TCM time, only a service coordinator can bill for TCM services
Other Health First Colorado Covered Services
Other services which can be billed to Health First Colorado include, but are not limited to:
- Occupational Therapies
- Physical Therapies
- Speech Therapies
- Assistive Technology
- Audiology or hearing services
- Developmental Screenings, including but not limited to: the M-CHAT and Ages and Stages
Natural Environments
Part C of IDEA requires "to the maximum extent appropriate to the needs of the child, early intervention services must be provided in natural environments, including the home and community settings in which children without disabilities participate." (34 CFR § 303.12(b))
By definition, natural environments mean "settings that are natural or normal for the child's age peers who have no disabilities." (34 CFR § 303.18)
The exception to the rule reads "the provision of early intervention services for any infant or toddler with a disability occurs in a setting other than a natural environment that is most appropriate, as determined by the parent and the individualized family service plan team, only when early intervention cannot be achieved satisfactorily for the infant or toddler in a natural environment."
The provision of early intervention services taking place in natural environments is not just a guiding principle or suggestion, it is a legal requirement.
Early Intervention Procedure Code Table
Providers may bill procedure codes for Early Intervention Services as follows:
It is important to remember that State General Funds and Federal Part C Funds can be used for the reimbursement of provider travel time when billing Health First Colorado. Generally, providers' travel time is included in their negotiated hourly rate, however, in situations where providers are being asked to travel significant distances the Community Centered Board may decide to reimburse this cost to providers. This would be considered a related cost aligned with the service.
Early Intervention (Special Code 87)
| Description | Procedure Code | Modifier(s) | Notes |
|---|---|---|---|
| Any Health First Colorado service provided to a child enrolled in Early Intervention | all | TL | All services should be billed with the addition of the TL modifier. This is for identification purposes only. IFSP should be submitted along with any PAR request filed for services. |
Procedure Code Table
Targeted Case Management - Early Intervention (Special Code 87)
| Description | Procedure Code | Modifier(s) | Unit Designation |
|---|---|---|---|
| Targeted Case Management - Early Intervention Services | T1017 | TL | 15 Minutes - the use of the modifier here is required and is not solely for identification purposes. |
| Intensive, extended multidisciplinary services provided to children with complex medical, physical, medical and psychosocial impairments, per hour. Can be used for EI assessments only. Place of Service 12 is allowable for EI only. | T1026 | TL | Per hour - the use of the modifier here is required and is not solely for identification purposes. |
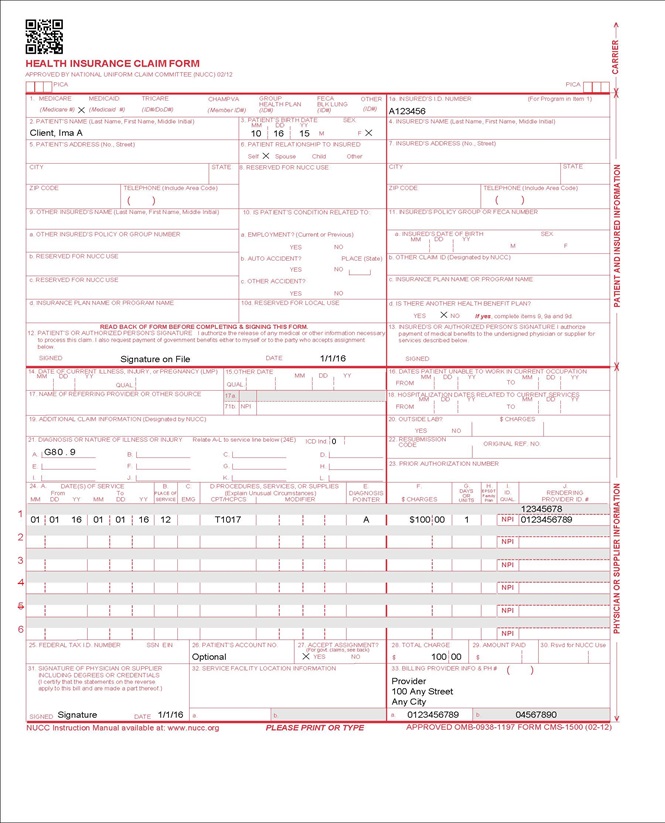
Early Intervention Paper Claim Reference Table
The reference table describes required fields for the Centers for Medicare & Medicaid Services (CMS) 1500 paper claim form for Early Intervention claims:
| CMS Field Number and Label | Field is | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven (7)-digit Medicaid ID number as it appears on the Medicaid Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010125 for January 1, 2025. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | |||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Not Required | |||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||||||||||||||||||||||||||
| 15. Other Date | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | Enter the six (6)-character prior authorization number from the approved Prior Authorization Request (PAR). Do not combine services from more than one (1) approved PAR on a single claim form. Do not attach a copy of the approved PAR unless advised to do so by the authorizing agent or the fiscal agent. Complete when the service requires prior authorization. | ||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010125 for January 1, 2025.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not Required | |||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form.
| ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado-covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area)
Family Planning (unshaded area) | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Not Required | |||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010125 for January 1, 2025. | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type (PT) is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the PT is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
Early Intervention Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Early Intervention Revisions Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 10/3/2016 | Manual revised for interChange implementation. For manual revisions prior to 10/3/2016 Please refer to Archive. | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 6/15/2018 | Updated timely filing information and removed references to LBOD, removed general billing information already available in the General Provider Information manual | DXC |
| 12/20/2018 | Clarification to signature requirements | HCPF |
| 2/26/2020 | Converted to web page | HCPF |
| 3/1/2020 | Clarification to the use of EI Colorado database for Training, Education and Experience box | HCPF |
| 9/10/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 10/23/2020 | Replaced "database" with "Early Intervention Data System" | HCPF |
| 5/30/2022 | Added change to age restriction, added new billing code | HCPF |
| 7/6/2022 | Removed words "Targeted Case Management" from procedure code table | HCPF |
| 11/18/2022 | Added *some children remain in early intervention until Preschool Special Education services begin to page 1 | HCPF |
| 12/22/2022 | Added FAQs section | HCPF |
| 2/11/2025 | Updated name of Early Intervention service provider | HCPF |