Fee-for-Service Behavioral Health Benefit
- General Policies
- General Billing Information
- Covered Services and Limitations
- CMS 1500 Paper Claim Reference Table
- Timely Filing
- Fee-For-Service Behavioral Health Benefit Revisions Log
Return to Billing Manuals Web Page
General Policies
The Fee-For-Service (FFS) Behavioral Health Benefit is a group of services designed to provide medically necessary behavioral health services to certain Health First Colorado (Colorado's Medicaid program) members. This Benefit includes both Mental Health services and Substance Use Disorder (SUD) services. Members are not required to obtain a referral from their Primary Care Physician (PCP) or Primary Care Medical Provider (PCMP) to receive these services.
Regional Accountable Entities (RAEs) are responsible for covering behavioral health services for nearly all Health First Colorado members. To verify if a Health First Colorado member's behavioral health services are covered, providers must perform a member eligibility query in the Provider Web Portal. The member eligibility query will display both a member’s Health First Colorado eligibility as well as which RAE a member is attributed to, which is responsible for covering the member's behavioral health services.
Members who are eligible for the FFS Behavioral Health Benefit are limited to:
- Members who do not have active enrollment in a RAE. See Program Rule 8.212 for the policy which exempts Health First Colorado members from RAE coverage. Only a small percentage of members meeting very specific criteria will be exempt. Member exemption is determined by the Department.
- Members being treated for a condition not eligible for reimbursement under the RAE (such as Autism Spectrum Disorder or Gender Identity Disorder).
Providers must reference APPENDIX I in the State Behavioral Health Services (SBHS) Billing Manual for a list of RAE-covered services, and the Diagnoses Section to confirm RAE-covered diagnoses. A number of services, such as office administered drugs (e.g. Suboxone) are covered Health First Colorado benefits but are not covered by the RAE. These services must always be billed FFS to the Health First Colorado fiscal agent, Gainwell Technologies.
A primary care provider can bill FFS up to six (6) short-term behavioral health visits per fiscal year. Visit the Accountable Care Collaborative Phase II web page for details on the Short-Term Behavioral Health Services policy.
General Billing Information
Refer to the General Provider Information Manual for general billing information.
Medical Necessity
Health First Colorado can only reimburse for services that are considered Medically Necessary. According to 10 CCR 2505-10 section 8.076.1.8, a service is considered medically necessary when it:
- Will, or is reasonably expected to prevent, diagnose, cure, correct, reduce, or ameliorate the pain and suffering, or the physical, mental, cognitive, or developmental effects of an illness, condition, injury, or disability. This may include a course of treatment that includes mere observation or no treatment at all. For members under age 21, per section 8.280.4E, this includes a reasonable expectation that the service will assist the member to achieve or maintain maximum functional capacity in performing one (1) or more Activities of Daily Living.
- Is provided in accordance with generally accepted professional standards for health care in the United States;
- Is clinically appropriate in terms of type, frequency, extent, site, and duration;
- Is not primarily for the economic benefit of the provider or primarily for the convenience of the member, caretaker, or provider;
- Is delivered in the most appropriate setting(s) required by the member's condition;
- Is not experimental or investigational; and
- Is not more costly than other equally effective treatment options.
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
Federal Medicaid law, 42 U.S.C.§ 1396d(r), requires state Medicaid programs to provide EPSDT benefits for members under 21 years of age. This means Health First Colorado is required to cover any service for members age 20 or younger that is medically necessary “to correct or ameliorate a defect, physical or mental illness, or a condition identified by screening,” whether or not the service is covered under the Colorado State Medicaid Plan. “Ameliorate” means to “make more tolerable” or, in other words, to improve or maintain the member’s health in the best condition possible, compensate for a health problem, prevent it from worsening, or prevent the development of additional health problems. Even if the service will not cure the member’s condition, it must be covered if it is medically necessary to improve or maintain the member’s overall health.
EPSDT does not require the state Health First Colorado agency to provide any service, product, or procedure that is:
- Unsafe, ineffective, or experimental/investigational.
- Not medical in nature or not generally recognized as an accepted method of medical practice or treatment.
Service limitations on scope, amount, duration, frequency, and/or other specific criteria described in the above screening policies may be exceeded or may not apply as long as the provider documentation shows how the service, product, or procedure will correct, improve or maintain the recipient's health, compensate for a health problem, prevent it from worsening, or prevent the development of additional health problems.
Providers may be subject to post-payment review to assure the use of a validated, standardized screening tool and medical justification for screens in excess of the stated benefit limits.
Covered Services and Limitations
Updated July 2024
CPT codes, descriptions and other data only are copyright 1995 - 2023 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association (AMA).
| Procedure Code | Short Code Description |
|---|---|
| 90785 | Interactive complexity (List separately in addition to the code for primary procedure) |
| 90791 | Psychiatric diagnostic evaluation |
| 90792 | Psychiatric diagnostic evaluation with medical services |
| 90832 | Psychotherapy, 30 minutes with member and/or family member |
| 90833 | Psychotherapy, 30 mins, with member or family member, when performed with an E&M service listed separately |
| 90834 | Psychotherapy, 45 minutes with member and/or family member |
| 90836 | Psychotherapy, 45 mins, with member or family member, when performed with an E&M service listed separately |
| 90837 | Psychotherapy, 60 minutes with member and/or family member |
| 90838 | Psychotherapy, 60 mins, with member or family member, when performed with an E&M service listed separately |
| 90839 | Psychotherapy for crisis, first 60 minutes |
| 90840 | Psychotherapy for crisis, each additional 30 minutes (list separately in addition to code for primary service) |
| 90846 | Family psychotherapy (w/o pt.) |
| 90847 | Family psychotherapy (conjoint) |
| 90849 | Multiple-family group psychotherapy |
| 90853 | Group psychotherapy (not multi-family) |
| 90863 | Pharmacologic management, including prescription and review of medication, when performed with psychotherapy services (list separately in addition to the code for primary procedure) |
| 96105 | Assessment of aphasia, per hour |
| 96110 | Developmental test limited, per instrument used |
| 96111 | Developmental test extended, with interpretation and report |
| 96116 | Neurobehavioral status exam, per hour |
| 96121 | Neurobehavioral status exam by physician or other qualified healthcare professional, both face-to-face time with the patient and time interpreting test results and preparing the report; each additional hour list separately in addition to code for primary procedure. |
| 96125 | Cognitive test by healthcare professional, per hour |
| 96127 | Brief emotional or behavioral assessment, per standardized instrument |
| 96130 | Evaluation of psychological test, first hour |
| 96131 | Evaluation of psychological test, each additional hour |
| 96132 | Evaluation of neuropsychological test, first hour |
| 96133 | Evaluation of neuropsychological test, each additional hour |
| 96136 | Administration of psychological or neuropsychological test, first 30 minutes |
| 96137 | Administration of psychological or neuropsychological test, each additional 30 minutes |
| 96138 | Administration of psychological or neuropsychological test by technician, first 30 minutes |
| 96139 | Administration of psychological or neuropsychological test by technician, each additional 30 minutes |
| 96146 | Psychological or neuropsychological test administration, with single automated, standardized instrument via electronic platform, with automated result only |
| 99367 | Medical Team Conference w/ Interdisciplinary Team w/out Pt and/or Family and Participation by Physician, 30 mins or more |
| A0999+ET | Behavioral Health Secure Transport |
| A0425+ET | Ground Mileage, per statute mile |
| H0001+HF | Alcohol/drug assessment, 1 unit per day, untimed |
| H0004+HF | Individual/family counseling and therapy, 8 units per day, 15 min. unit |
| H0005+HF | Group counseling and therapy, 1 unit per day, 1 hour unit |
| H0006+HF | SUD Targeted case management, 4 units per day, 15 min. unit |
| H0010+HF | Clinically Managed Residential Withdrawal Management: ASAM Level 3.2WM, per-diem |
| H0011 | Clinically managed residential withdrawal management: ASAM level 3.7WM, per diem |
| H0015 | Alcohol and/or drug services; intensive outpatient program (IOP) |
| H0016 | Alcohol and/or drug service; partial hospitalization program (PHP) |
| H0020+HF | Alcohol and/or drug services; Methadone administration and/or service, 1 unit per day, untimed |
| H2036+U1 | ASAM level 3.1 - Clinically managed low-intensity residential services, per diem |
| H2036+U3 | ASAM level 3.3 - Clinically managed population-specific high-intensity residential services, per diem |
| H2036+U5 | ASAM level 3.5 - Clinically managed high-intensity residential services, per diem |
| H2036+U7 | ASAM level 3.7 - Medically monitored intensive inpatient services, per diem |
| S9445+HF | Alcohol/drug screening counseling, 1 unit per day, untimed |
| J0571 | Buprenorphine, oral; 5 units per day; 1 mg unit |
| J0572 | Buprenorphine/naloxone, oral, less than or equal to three (3) mg, 5 units per day, < or = three (3) mg unit |
| J0573 | Buprenorphine/naloxone, oral, greater than three (3) mg, but less than or equal to six (6) mg; 5 units per day; Three (3) mg-six (6) mg unit |
| J0574 | Buprenorphine/naloxone, oral, greater than six (6) mg, but less than or equal to 10 mg; 4 units per day; 7-10mg unit |
| J0575 | Buprenorphine/naloxone, oral, greater than 10 mg; 3 units per day; > or =10mg unit |
| J2315 | Office administered injection: Naltrexone, depot form, one (1) mg; 380 mg / day, limit one (1) injection per month; 1 mg unit |
The codes used for submitting claims for services provided to Health First Colorado members represent services that are approved by the Centers for Medicare & Medicaid Services (CMS) and services that may be provided by an enrolled Health First Colorado provider.
HIPAA requires providers to comply with the coding guidelines of the AMA CPT Procedure Codes and the International Classification of Disease, Clinical Modification Diagnosis Codes. If there is no time designated in the official descriptor, the code represents one (1) unit or session. Providers should regularly consult monthly bulletins on the Provider Bulletins web page. To receive electronic provider bulletin notifications, an email address can be entered into the Provider web portal in the (MMIS) Provider Data Maintenance area or by signing up on the Communications Mailing List. Bulletins include updates on approved procedure codes as well as the maximum allowable units billed per procedure.
Services Not Covered by the FFS Behavioral Health Benefit
- Services and covered diagnoses included under the responsibility of a RAE are not covered under the FFS Behavioral Health Benefit for members attributed to a RAE.
- Court-Ordered services. Services that are ordered by a court are not automatically covered or excluded by Health First Colorado. Services must meet Medical Necessity criteria to be reimbursed by Health First Colorado.
- Services provided by email, text message, facsimile transmission, and online research.
- Room and board services.
- Educational, vocational and job training services.
- Habilitation services.
- Services to inmates in public institutions (i.e. correctional facilities) as defined in 42 CFR § 435.1009.
- Mental health services to individuals residing in institutions for mental diseases as defined in 42 CFR § 435.1009 are not covered outside of the RAE.
- Recreational and social activities.
- Day treatment program services.
- Peer advocate services.
Opioid Treatment Providers
Opioid Treatment Providers (OTPs) must enroll as medical clinics, Provider Type 16, with Gainwell. Visit the Find Your Provider Type web page for details. Individual rendering providers must have their own NPI number and enrollment.
An OTP may dispense Suboxone for take home dosing, however this dispensing is not considered a BH benefit. Rather, it is considered a pharmacy benefit, and the OTP is responsible to seek reimbursement for the drug under the pharmacy benefit.
Other ancillary medical services, as required by Methadone treatment guidelines outlined by SAMSHA, provided by OTPs (physical health assessments, blood draws, etc.) are considered physical health services. Therefore, these physical health services are never billed to the RAE. They are always billed to Gainwell.
Laboratory services, also required as part of treatment monitoring by OTPs managing Methadone treatment, require CLIA certification or a waiver.
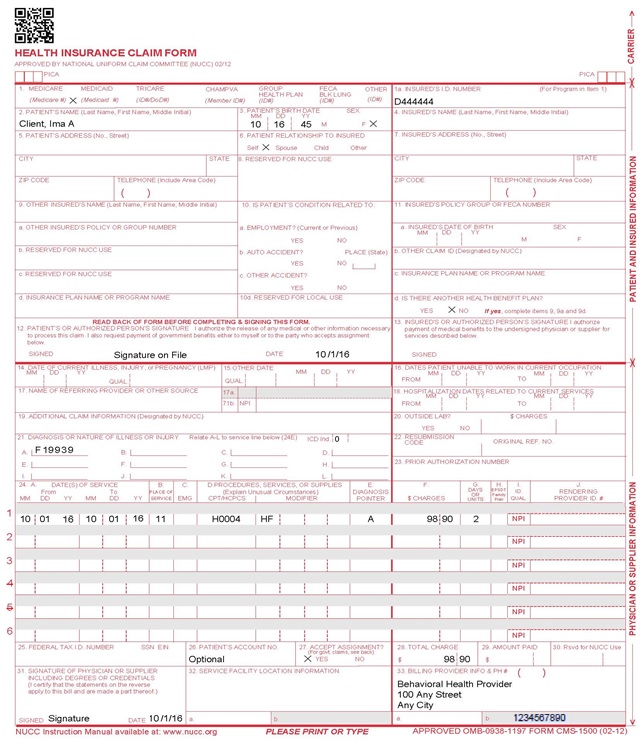
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Not Required | |||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Not Required | |||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | |||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Not Required | |||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Conditional | Leave blank | ||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
Single Date of Service: Enter the six (6)-digit date of service in the "From" field. Completion of the "To" field is not required. Do not spread the date entry across the two (2) fields. | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not Required | |||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the procedure code that specifically describes the service for which payment is requested. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Conditional | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | General Instructions | A unit represents the number of times the described procedure or service was rendered. Except as instructed in this manual or in Health First Colorado bulletins, the billed unit must correspond to procedure code descriptions. The following examples show the relationship between the procedure description and the entry of units. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Not Required | EPSDT (shaded area) Not Required Family Planning (unshaded area) Not Required | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Not Required | |||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
CMS 1500 Behavioral Health Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
Fee-For-Service Behavioral Health Benefit Revisions Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manuals Comment Log v0_2.xlsx | HPE (now DXC) |
| /10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 5/9/2018 | Revision of policies to reflect changes made to 8.746. Revision of SUD eligible providers and SUD benefit limitations. Clarification of Methadone Clinic enrollment details. | HCPF |
| 6/25/2018 | Updated billing section to point at general manual, replaced multiple instances of BHO with RAE | HCPF |
| 7/26/2018 | Included information on the 6 short term behavioral health visits in the primary care setting related to ACC 2 | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 7/11/2019 | Updated Appendices' links and verbiage | DXC |
| 12/30/2019 | Converted to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |
| 11/16/2020 | Removed section on Social Ambulatory Detox, replaced with direction to SUD Residential and Inpatient Services. Removed HCPCS S3005, T1007, T1019, T1023 from coding table effective 12-31-20. These services are now part of the residential/inpatient provider manual. Removed residential treatment from non-covered services section (effective 1-1-21) and revised IMD language. | HCPF |
| 7/6/2021 | Updating with the standard EPSDT policy language. | HCPF |
| 7/29/2021 | Updated the Substance Use Disorder Procedure Code Table to include procedure code H0010 for Clinically Managed Residential Withdrawal Management. | HCPF |
| 9/23/2021 | DORA has changed the prefix on the LAC license to ACD. Updated the abbreviation for Licensed Addiction Counselor from LAC to ACD. | HCPF |
| 3/1/2022 | Updated mental health procedure code table. | HCPF |
| 5/13/2022 | Updated mental health services procedure code table and substance use disorder procedure code table. | HCPF |
| 3/27/2023 | Updated AWS URL Links | HCPF |
| 5/22/2023 | Replaced instances of DXC with Gainwell Technologies | HCPF |
| 7/1/2024 | Moved retired codes from charts above to this section. Codes 96101, 96102, 96103, 96111, 96118, 96119 were retired on 12/31/2018; Added SUD Residential Codes, Made major revisions to overall layout and content: Removed narrative descriptions of general covered MH and SUD services leaving the combined BH covered Procedure codes with descriptions only; Removed eligible providers lists since these are clinically driven; edited policy language to provide clarity, correction, and alignment with HCPF’s Capitated BH Benefit where appropriate. | HCPF |
| 8/15/2025 | Updated ACC link for Phase 3, added code 99367, clarified H0005 with modifier HF | HCPF |