Appeals
Appeals (if you disagree with a health coverage decision)
You have a right to file an appeal. You can appeal if you disagree about a decision about whether you qualify for Health First Colorado (Colorado’s Medicaid program). You can also appeal any decision about services that you receive.
Appeal means you disagree with a decision, and you ask in writing for a formal hearing (state fair hearing) with a judge.
You must appeal within 60 days of the date on the letter that has the decision you disagree with. This letter is also called a Notice of Action.
What can I appeal?
Things you can appeal include:
- You no longer qualify for Health First Colorado (Colorado’s Medicaid program).
- Your application for Medicaid was denied.
- You didn’t receive a response to your application.
- A service you get is set to be reduced or stopped.
- You did not get notice that
- your health coverage was ending, or
- covered services or benefits are set to be reduced or stopped.
Benefits and services appeals
If you disagree with a decision about your benefits or services, you may need to start the appeal process with the health care organization that manages those benefits.
Follow the directions in your letter, and pay attention to the deadlines. If you miss a deadline you may lose or have a gap in your coverage.
If you file a benefits or services appeal with your health plan and you disagree with their decision, you may ask for a formal hearing.
Eligibility appeals (whether you qualify for Medicaid)
If you disagree with a decision about whether you qualify for Health First Colorado (eligibility), you can
- Ask for an informal meeting with your eligibility site or county.
- File an appeal for a formal hearing (state fair hearing).
- Ask for both an informal meeting and file an appeal at the same time.
Informal meeting
If you disagree with an eligibility decision, you can ask for an informal meeting with your county or eligibility site.
Ask for an informal meeting within 60 days of the date on your Notice of Action.
Asking for an informal meeting does not guarantee you can keep your coverage after the termination date listed on the letter.
To continue your health coverage, you must ask for a formal hearing (state fair hearing).
Formal hearing (state fair hearing)
You can ask for a formal hearing with the Office of Administrative Courts if
- You disagree with a decision about your eligibility or benefits.
- You already followed the appeals process with your health plan and disagreed with their decision.
Formal hearings are also known as “appeals” or “state fair hearings.”
Appeals are decided by an administrative law judge with the Office of Administrative Courts. They will listen to both sides before making a decision.
Good to know:
- Asking for a formal hearing is the only way to keep your health coverage during the appeals process.
- Pay attention to the date: If you try to appeal after 60 days, the Office of Administrative Courts may not accept your appeal.
Expedited (faster) appeals
If waiting for an appeal will endanger your health, you can ask the Office of Administrative Courts for an expedited (or faster) appeal.
How to ask for an expedited (faster) hearing
Child Health Plan Plus (CHP+) appeals
If you do not qualify for CHP+ when you renew, or if you disagree with a decision about your services, follow the appeals process on your letter. CHP+ eligibility appeals go to the Colorado Medical Assistance Program (CMAP).
For questions about the CHP+ appeals process, contact CHP+ Customer Service at 800-359-1991 (State Relay: 711)
Rules: 10 CCR 2505-3 600
Keeping your health coverage during an appeal
- Asking for a formal appeal is the only way to continue your health coverage.
- Pay attention to the date: If you try to appeal after 60 days, the Office of Administrative Courts may not accept your appeal.
Learn more about keeping your health coverage during an appeal.
How to ask for an informal meeting
You can ask for an informal meeting by phone or in writing. Send your request to the address listed in the informal meeting section of your Notice of Action. The eligibility office will send you a letter with the date and time of your informal meeting. You can ask to have the meeting in person or by phone. The eligibility office will mail you their final decision within 3 days after the meeting.
Good to know:
- You can ask for an informal meeting and a formal hearing at the same time.
- You must ask for an informal meeting and/or a formal hearing 60 calendar days from the date listed on the Notice of Action letter.
- You must ask for a formal hearing to continue your health coverage. Asking only for an informal meeting does not guarantee you can keep your coverage after the termination date listed on the letter.
Key points
- Follow the instructions in your letter about what to do and who to contact if you disagree with the decision.
- Pay attention to the deadlines listed in your letter.
- Need help?
- Call the member services number in your letter,
- Contact your eligibility site, or
- Contact the Health First Colorado Managed Care Ombudsman:
- 877-435-7123 or TTY 888-876-8864
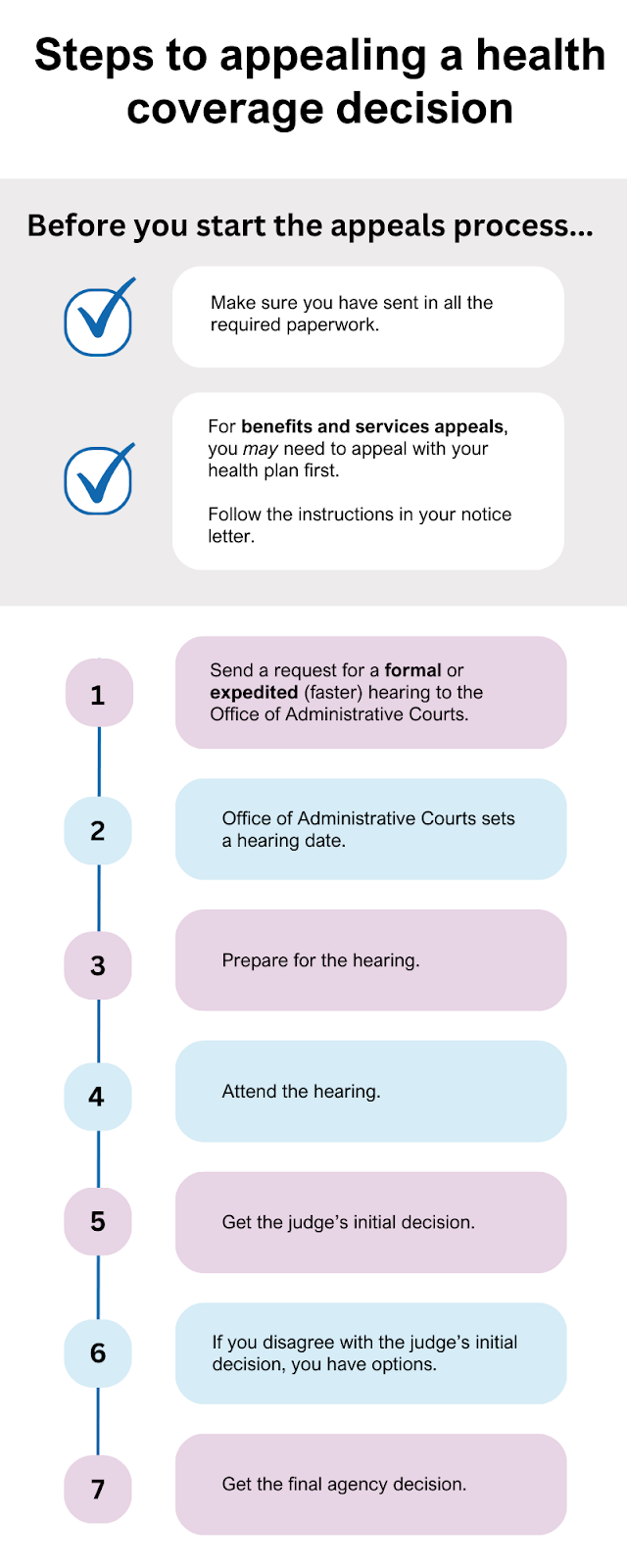
How to ask for a formal hearing
Before you begin the appeal process, check if you turned in all your required paperwork.
If you get a letter saying you’re losing or being denied coverage, read the letter and find out if you’ve turned in all the required information and paperwork.
You may be able to solve the issue quickly by submitting all the necessary documents and information.
Step 1: Send a written request for a formal hearing or an expedited hearing to the Office of Administrative Courts.
If you disagree with a decision about your eligibility,
Or,
If you already filed a benefits appeal or quick appeal with the health plan that manages your benefits and disagreed with their decision,
You can ask for a formal hearing with the Office of Administrative Courts. A formal hearing is also known as an “appeal” or a “state fair hearing.”
You can ask for a formal hearing in any of these ways:
A. Fill out the “Request for State Level Hearing” form. Find this form on the Office of Administrative Courts forms page under General Services Forms.
B Write a letter to the Office of Administrative Courts.
Your letter must include:
- Your name,
- Your signature (if mailing or faxing),
- Your mailing address, and
- Your phone number.
Helpful to include, but not required:
- A case number or Member ID.
- Reason you disagree with the decision.
- A copy of the decision letter.
- A request for an interpreter or other accommodations (if needed).
Mail, fax, email or bring your Appeal Request Form or letter to:
Office of Administrative Courts
1525 Sherman St., 4th floor
Denver, CO 80203
Fax: 303-866-5909 (10 pages or fewer; otherwise, mail your request)
Email: oac-gs@state.co.us
You can also request an appeal online using the Office of Administrative Courts e-filing system (registration required).
How to ask for an expedited (faster) hearing
If waiting for an appeal will endanger your health, you can ask the Office of Administrative Courts for an expedited (or faster) appeal.
Write “expedited appeal” on your request and write why you’re asking for a faster appeal.
Step 2: The Office of Administrative Courts sets a formal hearing date.
Formal hearing
After the Office of Administrative Courts gets your appeal request, they will mail you a letter with the time and date of your formal hearing. This is called a Notice of Hearing.
Expedited hearing
If you asked for an expedited hearing, the Office of Administrative Courts will send your request to the Office of Appeals at the Colorado Department of Health Care Policy and Financing, which administers Health First Colorado (Colorado’s Medicaid program).
The Office of Appeals will decide in 1 business day if they accept or deny your expedited appeal request.
- If the Office of Appeals says “yes,” to an expedited appeal request, they will call you to schedule a hearing. The hearing will be over the phone or video conference and will take place within a few days.
- If the Office of Appeals says “no” to your request for an expedited appeal, you will still get a formal hearing through the Office of Administrative Courts. The Office of Administrative Courts will mail you a letter with the time and date of your formal hearing.
Step 3: Prepare for the hearing.
Gather supporting information
Prepare for your hearing by gathering any supporting information about your case and send it to the organization that sent the denial or reduction (Appellee), and the Office of Administrative Courts no later than 10 days before the hearing. These papers should show the judge why you disagree with the decision.
You don’t need a lawyer for a formal or expedited hearing. You can represent yourself or ask someone to represent you. That person can be a provider, an advocate, a lawyer, a family member or any other person you trust.
If you want someone who is not a lawyer to represent you, fill out the Non-Attorney Authorization form. Both of you must sign the form. Return the form to the Office of Administrative Courts.
Step 4: Attend the hearing.
This is where you get to share your story and explain why you believe you qualify for Health First Colorado, or why you should receive the services your provider requested.
The following video by the Colorado Department of Personnel and Administration’s Office of Administrative courts explains what you can expect to happen at your hearing.
Step 5: Get the judge’s initial decision.
In most cases, the judge will make a written decision in 20 days. The Office of Appeals will send you a copy of the judge's decision, called a Notice of Initial Decision.
This is not a final decision!
- If you agree with the initial decision, you do not need to take any action. Wait for the Office of Appeals to issue the Final Agency Decision.
- If you disagree with the judge’s initial decision, you still have options.
- If the judge decides in your favor, the organization that sent the denial or reduction letter (Appellee) can still file exceptions. If that happens, you have a chance to respond before a Final Agency Decision is issued by the Office of Appeals.
Step 6: What to do if you disagree with the judge’s initial decision
If you disagree with the judge’s initial decision, you can file a written exception to the Office of Appeals within 18 days of getting the Notice of Initial Decision.
Exceptions are your written arguments stating why you believe the initial decision is incorrect.
This is the last step in the appeal process before the Office of Appeals issues a Final Agency Decision.
Key facts about written exceptions:
- The Office of Appeals must receive your written exception by the due date on the Notice of Initial Decision letter.
- If you need more time to review the judge’s initial decision or to order a free transcript, you can ask the HCPF Office of Appeals for an extension.
- The Office of Appeals must receive your request for an extension by the due date on the Notice of Initial Decision letter.
- You do not need a lawyer to request an extension or file a written exception.
Step 7: Get the final agency decision.
After you send your written exception to the Office of Appeals, the other side (Appellee) will have a chance to review and respond to your written exception.
The Office of Appeals will then review your written exception and any response from the other side and issue a Final Agency Decision.
- If you agree with the Final Agency Decision, you do not need to take any action. If the Final Agency Decision was in your favor, your benefits and services will be restored if they were reduced or denied.
- If you disagree with the Final Agency Decision, you may file a motion for reconsideration with the Office of Appeals. Or, you may file a judicial review in state district court. Follow the instructions in your Final Agency Decision letter.
What to do if you no longer qualify for Health First Colorado?
If the final agency decision is not in your favor, and you no longer qualify for Health First Colorado, you can
- Reapply for coverage on Colorado PEAK, or
- Find health insurance at Connect for Health Colorado, Colorado’s official health insurance marketplace.
- Connect for Health Colorado lets you apply for financial help to lower the cost of health insurance.
FAQ: What if I no longer qualify for Health First Colorado or CHP+?
Key facts about appeals
Keeping your health coverage during the appeal process
Asking for a formal hearing (state fair hearing) is the only way to keep your health coverage during the appeals process.
Eligibility Appeals
If you get a Notice of Action saying you no longer qualify for Health First Colorado, you can ask for a formal hearing (a state fair hearing).
To keep your coverage during the eligibility appeals process
- You must be a current Health First Colorado member.
and
- The Office of Administrative Courts must get your written request for appeal (state fair hearing) within 60 days of the Notice of Action.
Your coverage will continue until a final decision is made on your appeal.
Note: If you are applying for Health First Colorado for the first time and you do not qualify, you can appeal. However, there is no continuation of benefits.
Benefits Appeals
If you get a notice denying or reducing your benefits or services, you can ask for a formal hearing (a state fair hearing).
To keep getting the benefit or service you are receiving,
- The Office of Administrative Courts must get your written request for appeal (state fair hearing) within 60 days of the notice of denial or reduction of benefits.
Your benefits or services will continue until a final decision is made on your appeal.
Note: If you ask for a new benefit or service, and you get denied, there is no continuation of benefits or services.
Health Plan Appeals
If you get a letter (Notice of Adverse Benefit Determination) from your health plan telling you they are ending or changing your services, and you disagree with this decision, you can appeal to your health plan.
If you file an appeal with your health plan within 60 days of the date on the notice, you can continue your benefits during your appeal.
If you lose the appeal to your health plan, you can ask for a formal hearing (state fair hearing).
The Office of Administrative Courts must get your written request for appeal (state fair hearing) within 120 days of the health plan’s final decision.
How to ask for a formal hearing.
For eligibility appeals, you can ask for both an informal meeting and a formal hearing at the same time.
You can ask for an informal meeting with your eligibility site and a formal hearing with the Office of Administrative Courts at the same time.
The informal meeting usually happens first. If your problem is resolved during the informal meeting, your eligibility site will help you cancel the formal hearing.
Instructions for asking for an informal meeting and a formal hearing are included in your denial letter.
You can ask for a faster appeal if your health is at risk.
This is called an expedited appeal (eligibility).
To file an expedited appeal, follow the instructions for How to ask for a formal hearing and write “expedited appeal” on your request and write why you’re asking for a faster appeal.
To file a quick appeal with the health care organization that manages your benefits, follow the instructions in your letter.
You can represent yourself at the appeal or ask someone to represent you.
That person can be a provider, an advocate, a lawyer, a family member or any other person you trust.
If you ask someone to represent you, you need to fill out the Non-Attorney Authorization form.
Both you and your representative must sign the form. After you both sign the form, return it to the Office of Administrative Courts.
You can find this form on HCPF’s Health Insurance Portability and Accountability Act Privacy Forms webpage. You can also find the Health First Colorado Non-Attorney Authorization form in the General Services section of the OAC forms page.
You can ask for the information used to make the decision before the hearing.
You can ask the organization who issued the Notice of Action (Appellee) to see the case file and other information they used to make their decision. The Appellee’s contact information will be in the notice letter.
You have the right to ask for help understanding your Notice of Action letter or writing your appeal.
Contact the health care organization that manages your benefits for help. The contact information will be listed in your Notice of Action letter.
You can also ask the Health First Colorado Managed Care Ombudsman for help. Call 877-435-7123 or TTY 888-876-8864 or State Relay: 711 for callers with speech or hearing disabilities.
If you're appealing a benefits decision made by the Colorado Department of Health Care Policy and Financing, then an Appeals Navigator will contact you.
You have the right to ask for accommodations or an interpreter during your hearing.
Auxiliary aids and services for individuals with disabilities and language services for individuals whose first language is not English may be provided upon request. Requests should be made as soon as possible. Contact information for each hearing type is listed below.
For accommodations for formal hearings, contact:
Office of Administrative Courts
1525 Sherman St., 4th floor
Denver, CO 80203
Phone: (303) 866-5626
State Relay (TTY): 711
Tell them:
- Your name
- Your case number
- The date of your formal hearing
- The specific accommodations or language interpretation that you need for your formal hearing
For accommodations for approved expedited hearings, contact:
Colorado Department of Health Care Policy and Financing Office of Appeals
303 E. 17th Avenue
Denver, CO 80203
Phone: (303) 866-5654
Fax: (303) 866-4411
Email: hcpf_officeofappeals@state.co.us
Tell them:
- Your name
- Your contact information
- Your case number
- The date of your expedited hearing
- The specific accommodations or language interpretation that you need for your expedited hearing
Getting help with an appeal
You can contact these government offices with questions:
Health First Colorado Member Contact Center
The Health First Colorado Member Contact Center is who you should contact if you have questions about Medicaid.
Phone: 800-221-3943 State Relay (TTY): 711
Office of Administrative Court’s Clerk’s Office
The Office of Administrative Court’s Clerk's Office may be able to help you with questions about how to file an appeal, questions about your hearing, and any questions about how to get information to your judge.
Phone: 303-866-5626
Help with benefits appeals:
Contact the health care organization that manages your benefits for help. The contact information will be listed in your letter.
Health First Colorado Managed Care Ombudsman
Phone: 877-435-7123 or TTY 888-876-8864 or State Relay: 711.
Email: help123@maxmus.com
If you're appealing a benefits decision made by the Colorado Department of Health Care Policy and Financing, then an Appeals Navigator will contact you.
Legal help
These organizations may be able to help you with legal questions:
Colorado Legal Services (CLS)
CLS may be able to help. They provide legal help for low-income Coloradans with civil legal needs, and they are free.
Call CLS at 303-837-1313, or fill out their online intake form at: coloradolegalservices.org
Colorado Cross-Disability Coalition (CCDC)
CCDC has non-lawyer advocates who may be able to help with appeals if you have a disability.
Call the main office at 303-839-1775. Learn more at ccdconline.org/contact.
Colorado Center on Law and Policy (CCLP)
CCLP has lawyer advocates who may be able to help with appeals or answer questions about the process.
Call CCLP at 303-573-5669 or get more information at copolicy.org.
Remember: You don’t have to have a lawyer. You can ask for an appeal by yourself, or with someone who is not a lawyer. If you have a case manager, you can ask them for help.
Glossary (definitions) of appeals terms
appeal: A written request sent to a state office saying you disagree with an eligibility or benefits decision, and you want a formal hearing with an administrative law judge.
appeals navigator: The person who helps you with benefits appeals decisions made by the Colorado Department of Health Care Policy and Financing or Acentra.
appellant: The organization that sends the Denial or Reduction Notice of Action, application denial or termination notice.
appellee: The organization that sends the denial or reduction notice of action letter.
approved expedited hearing: A request for a faster appeal that’s been approved by the Colorado Department of Health Care Policy and Financing Office of Appeals.
benefits: Health care services, medicine and supplies that are covered by Health First Colorado.
date of action: means the intended date on which a termination, suspension, reduction, transfer or discharge becomes effective.
eligibility: Whether or not someone qualifies for a program like Health First Colorado.
exceptions: Written arguments stating why you believe the administrative law judge’s initial decision is incorrect.
expedited hearing: A faster formal (eligibility) appeal, requested if waiting for an appeal will endanger the Appellant’s health.
extensions: Requests for more time to do something, like review the judge’s initial decision or order a transcript.
Final Agency Decision: A letter issued by the Colorado Department of Health Care Policy and Financing Office of Appeals after they review the judge’s initial decision, any written exceptions, and any responses from the other side.
formal hearing: A meeting with an administrative law judge from the Office of Administrative Courts. Also known as “state fair hearing” or “appeal.”
HCPF: Acronym for the Colorado Department of Health Care Policy and Financing, the agency that administers Health First Colorado (Colorado’s Medicaid program) and Child Health Plan Plus (CHP+).
health plan: The organization or company that Health First Colorado works with to manage your benefits, like Elevate Medicaid Choice (formerly known as Denver Health) and Rocky Mountain Health Plan Prime.
informal meeting: A discussion with your eligibility site about their decision on your coverage (eligibility).
Notice of Action: A letter sent to people who apply for Health First Colorado, or are already enrolled, regarding a denial, approval, termination and/or changes to their eligibility or benefits.
Notice of Initial Decision: The administrative law judge’s first decision on your appeal. This is not a final decision.
Office of Administrative Courts (OAC): Colorado's centralized administrative court system. This administrative court system lets agencies and citizens resolve certain disputes while avoiding the time and expense of going to district court.
Office of Appeals: The team of legal experts at the Colorado Department of Health Care Policy and Financing who review all sides of an appeal case and issue a Final Agency Decision.
Ombudsman: People who help settle grievances, appeals and other issues related to your health care.
quick appeal: A faster benefits appeal, requested with the managed care organization (Denver (Elevate) Health Medicaid Choice or Rocky Mountain Health Plan Prime) if waiting for a benefits appeal will endanger the Appellant’s health.
regular appeal: A meeting with an administrative law judge from the Office of Administrative Courts. Also known as “formal hearing” or “state fair hearing.”
State Fair Hearing: A meeting with an administrative law judge from the Office of Administrative Courts. Also known as “formal hearing” or “appeal.”
written exception: Exceptions are your written arguments stating why you believe the Initial Decision is incorrect, based on either incorrect factual findings or improper conclusions of law.