Provider Web Portal Quick Guide - Reading the Remittance Advice (RA) Dated Before 1/9/2019
Introduction
This Quick Guide is to be used for RAs received before 1/9/2019. For RAs received on or after 1/9/2019, refer to the most recent Reading the Remittance Advice (RA) Dated on or After 1/9/2019 Quick Guide on the Quick Guides web page
RA Sections and Page Numbering
The downloadable PDF RA file will not include every page that is included in the printable RA.
Address Cover Page (Page 1): The Address Cover Page will never appear in the PDF file, as it is used if mailing an RA.
Banner Message Section (Page 2): Any important messages from the Department of Health Care Policy & Financing (the Department) will appear on page 2.
Payment Notice Section: The Payment Notice section will never appear in the PDF file, as it is used for printing a physical check or EFT notice when mailing an RA.
Interpreting Claim Numbers
Each claim and adjustment is assigned a unique claim number, known as the internal control number (ICN). The following diagram and table provide detailed information about interpreting the claim number.
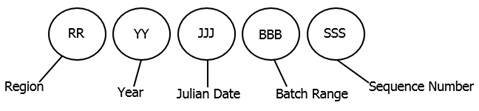
| Type of Number and Description | Applicable Number and Description |
|---|---|
| Region - The first two digits indicate how Health First Colorado received the claim or adjustment request. | 10 - Paper Claims with No Attachments 11 - Paper Claim with Attachments 20, 21 - Batch Claim 22 - Web Portal Claim with No Attachments 23 - Web Portal Claim with Attachments 25 - PBM Pharmacy Claims 30, 31, 40 - Claims Converted from Old MMIS 50 - Provider Initiated Adjustment (via paper) 51, 52, 53, 55, 57, 58 - System Initiated Adjustments 54 - Mass Void 56 - Mass Void Request or Single Claim Void 59 - Provider Initiated Electronic Adjustment 80 - Claim Resubmission by Gainwell Technologies, formerly DXC 94 - Web Portal Reconsideration Claims with Attachments (Note: If OZ is used for attachment, this region code indicating reconsideration will be automatically assigned, even if a reconsideration is not indicated by the provider.) 95 - Provider Initiated Web Portal Reconsideration Adjustment with Attachments |
| Year - Two digits indicate the year the claim was received. | For example, the year 2017 would appear as 17. |
| Julian Date - Three digits indicate the day of the year, by Julian date, that the claim was received. | For example, February 3 would appear as 034. |
| Batch Range - Three digits indicate the batch range assigned to the claim. | The batch range is used internally by Health First Colorado and is not applicable to providers. |
| Sequence Number - Three digits indicate the sequence number assigned within the batch range. | The sequence number is used internally by Health First Colorado and is not applicable to providers. |
Adjustments and Recoupments
Providers will see a Claim Adjustments section in the Remittance Advice (RA) if any of their claims were adjusted during the current financial cycle.
- Adjustments can be provider-initiated or system-generated (refer to region codes above).
- Recoupments are generally done on the same RA as the adjusted claim. See Scenario 1, Figures 1-3.
- Exception: Provider does not have enough paid claims to satisfy the recoupments. If the recoupment amount exceeds the paid claim amount, the recoupment will continue to the next weeks' RA until the total amount is recouped. See Scenario 2, Figures 4-8 for more information.
- Claim information will appear in the adjustment section for each claim type.
- Additional payment or overpayment to be withheld will be listed for each adjustment.
See the Claim Adjustment section in the figure below for Scenario 1.
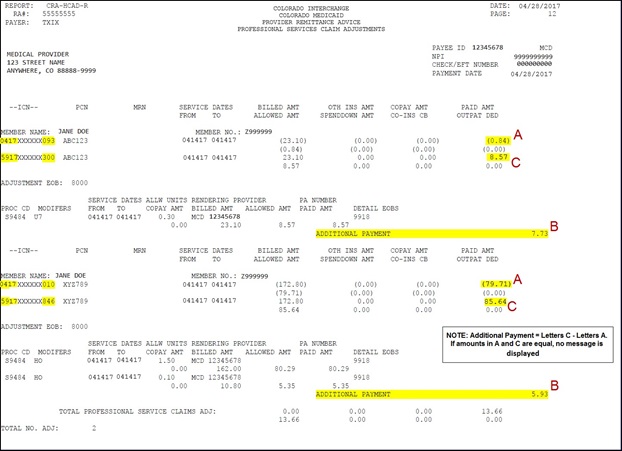
Figure 1 . RA Claim Adjustment - Additional Payment
Financial Transactions Page
The Financial Transactions page details the provider's weekly financial activity. Financial transactions reported on the RA include payouts, refunds, accounts receivable and payments for claims.
Under the Accounts Receivable section, the following information is provided:
- A/R Number
- Setup Date
- Balance
- Adjustment ICN
See the Financial Transaction page in the figure below for Scenario 1.
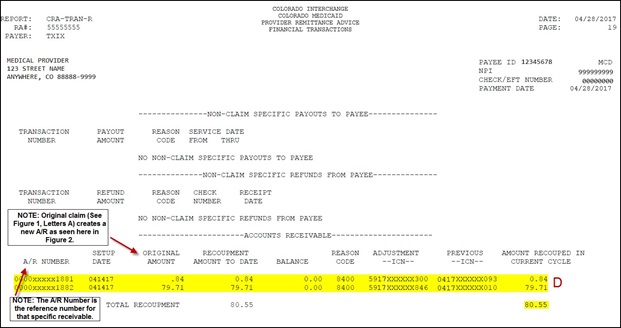
Figure 2 . RA Financial Transactions - Initial AR Setup
See the Summary page in the figure below for Scenario 1.
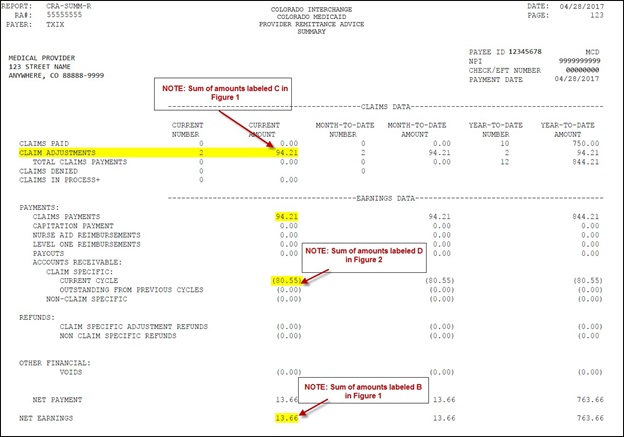
Figure 3. RA Summary 2
See a full set of RAs for Scenario 2 in the figures below.
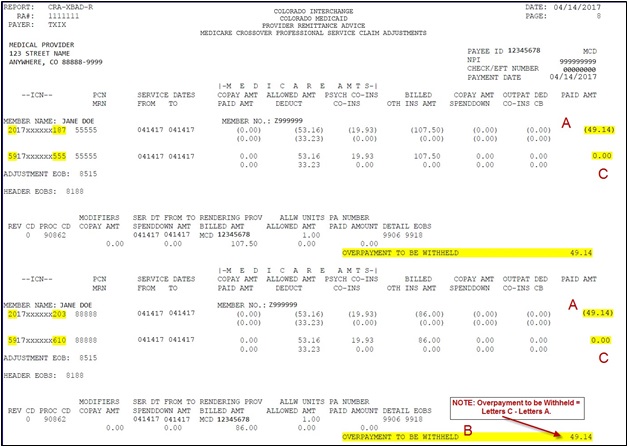
Figure 4 . RA Claim Adjustment - Overpayment to be Withheld
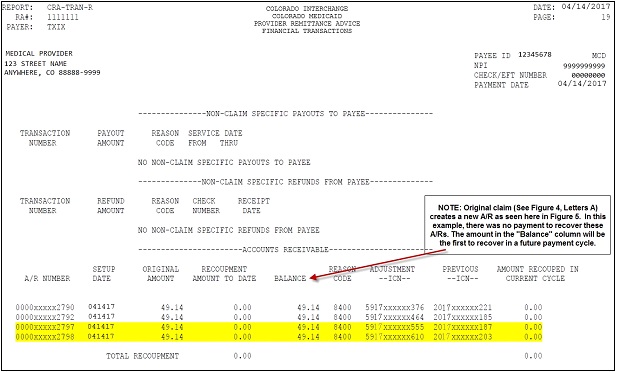
Figure 5 . RA Financial Transaction - Initial AR Setup
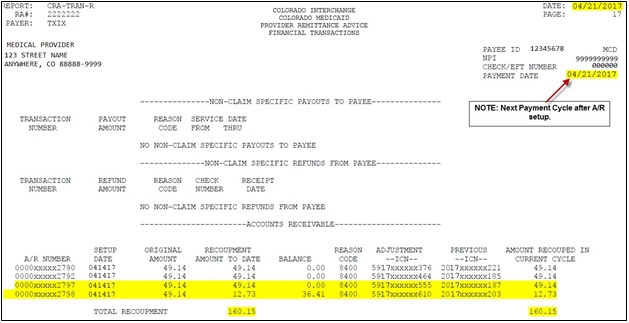
Figure 6 . RA Financial Transaction - First AR Withholdings
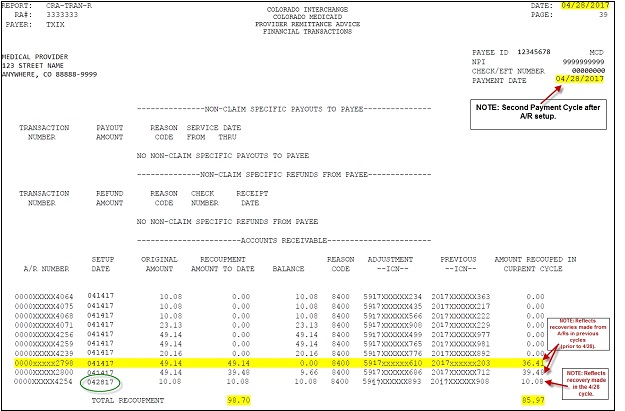
Figure 7 . RA Financial Transaction - Final AR Withholdings
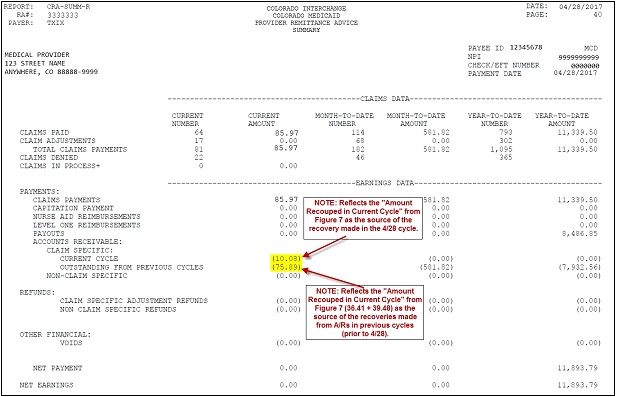
Figure8 . RA Summary
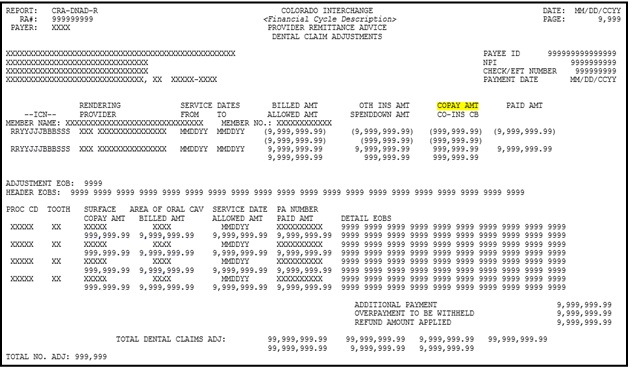
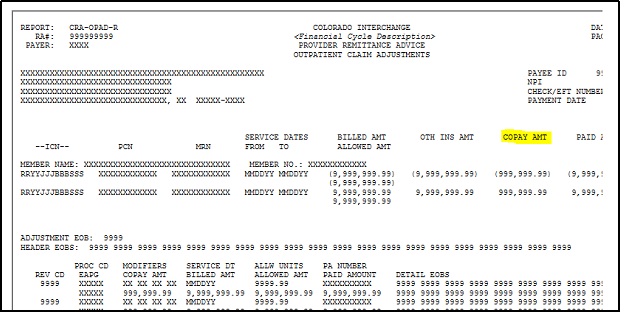
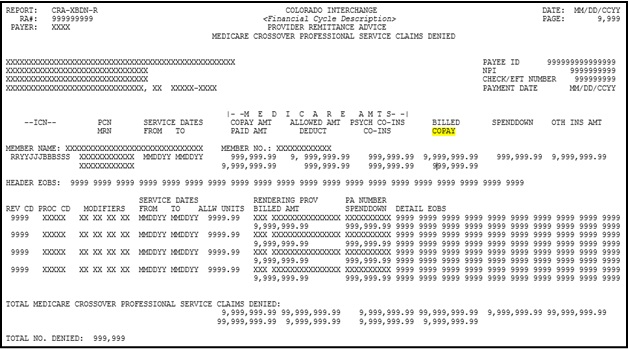
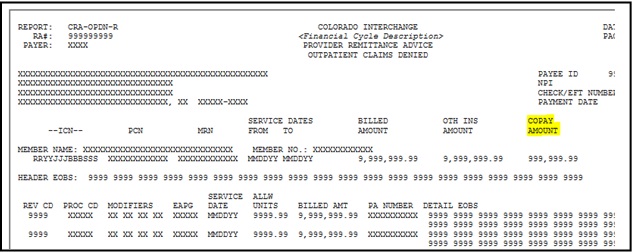
Recognizing Co-pay
Co-pay represents the amount of member responsibility on a claim detail that is to be collected by the provider at the time the service is rendered.
Co-pay appears on the RA as "COPAY AMT" for the following RA types:
- Dental Claim Adjustments
- Dental Claims Paid
- Professional Service Claim Adjustments
- Professional Service Claims Paid
- Compound Drug Claim Adjustments
- Compound Drug Claims Paid
- Drug Claim Adjustments
- Drug Claims Paid
- Inpatient Claim Adjustments
- Inpatient Claims Paid
- Outpatient Claim Adjustments
- Outpatient Claims Paid
- Medicare Crossover Institutional Claim Adjustments
- Medicare Crossover Institutional Claims Denied
- Medicare Crossover Institutional Claims Paid
- Medicare Crossover Professional Service Claim Adjustments
- Medicare Crossover Professional Service Claims Paid
Co-pay appears on the RA as "COPAY" for the following RA types:
- Remittance Advice - Medicare Crossover Professional Service Claims Denied
- Remittance Advice - Medicare Crossover Professional Service Claims In Process
Co-pay appears on the RA as "COPAY AMOUNT" for the following RA types:
- Remittance Advice - Outpatient Claims Denied
Using a Comma-Separated Values (CSV) File
The RA is available for download as PDF and CSV file formats. Downloadable CSV- formatted RAs allow users the benefits of building a customized RA specific to their use and saving the file to their computer. The CSV file on a provider's Web Portal appears as linear text separated by commas until it is downloaded into a compatible software program. Once downloaded, the file may be saved to a user's computer and the data manipulated, as desired.
To access the CSV file, providers should select the "Search Payment History" option from the left side of the provider's Web Portal home page. From the Search Payment History page providers can search for a given payment. The RA CSV file is listed for each payment returned in the search. The provider can click on the icon under the RA Copy (Delimited) column to download the CSV file.
Formats include:
- Microsoft Office Excel
- Microsoft Office Access
- OpenOffice 2.2.1 -- free software program available
Free spreadsheet applications can be found at:
- Google Docs
- ZDNet
- Other software applications may be available
Need More Help?
Please visit the Quick Guides web page to find all the Provider Web Portal Quick Guides.