Psychiatric Residential Treatment Facility and Out-of-state High Intensity Residential Treatment (OHIRT) Provider Billing Manual
- General Policies
- Child Welfare Placements in In-State Psychiatric Residential Treatment Facilities Fact Sheet
- Psychiatric Residential Treatment Facilities (PRTFs)
- Out-of-state High Intensity Residential Treatment (OHIRT) Provider
- Billing Information
- Critical Incident and Serious Occurrence Reporting
- Prior Authorization and Utilization Management (UM) Requirements
- UB-04 Paper Claim Reference Table
- Timely Filing
- Institutional Provider Certification
- PRTF/OHIRT Revisions Log
Return to Billing Manuals Web Page
General Policies
- Health First Colorado (Colorado's Medicaid program) members have their behavioral health services paid for by Regional Accountable Entities (RAEs). Regional Accountable entities are managed care entities responsible for covering behavioral health benefits for nearly all Health First Colorado members.
- Refer to Program Rule 8.212 for details about the RAE program, including policy which exempts Health First Colorado members from RAE coverage. Only a small percentage of members meeting very specific criteria will be exempt. Member exemption is determined by the Department of Health Care Policy & Financing (the Department).
- Residential services for children or youth in the custody of the Colorado Department of Human Services -Division of Child Welfare or Division of Youth Services are among the members exempted from RAE coverage by Program Rule 8.212.
- Visit the Department's Regional Accountable Entity web page for details about RAE coverage.
- To verify if a Health First Colorado member's behavioral health services are covered by an RAE, providers must perform a member eligibility query in the Provider Web Portal. Each RAE may have its own similar tool for providers to query member eligibility. Both tools are valid for checking member eligibility.
- The member eligibility query will display whether the RAE is responsible for covering the member's services. If the member is covered by the RAE, all claims for covered behavioral health services must be sent to the RAE for payment.
- All behavioral health providers must be enrolled with Health First Colorado and contracted with the RAE. Providers must contact the RAE which serves their region to begin the enrollment process. Visit the Department's Regional Accountable Entity web page for details.
- Providers who are denied RAE enrollment may not bill Gainwell fee-for-service (FFS) as an alternative reimbursement route. If the provider is denied RAE enrollment, this means that they may not treat Health First Colorado members for services covered by the RAE.
- Providers who are denied RAE enrollment may still render and be reimbursed for services not covered by the RAE.
- Providers must reference the State Behavioral Health Services Billing Manual for a list of RAE-covered services and conditions.
- Billing information included below is only applicable to services rendered to children or youth in the custody of the Colorado Department of Human Services - Division of Child Welfare or Division of Youth Services, who are not covered by the RAE.
Psychiatric Residential Treatment Facilities (PRTFs)
Providers must be enrolled as a Health First Colorado provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to the Health First Colorado
Providers should refer to the Code of Colorado Regulations, Program Rules (10 C.C.R. 2505-10), for specific information when providing psychiatric residential treatment.
Out-of-state High Intensity Residential Treatment (OHIRT) Provider
Providers must be enrolled as a Health First Colorado provider in order to:
- Treat a Health First Colorado member
- Submit claims for payment to the Health First Colorado
Out-of-state High Intensity Residential Treatment (OHIRT) Providers provide comprehensive mental health treatment to children and adolescents (youth) who, due to behavioral health concerns, or severe emotional disturbance, need treatment that can most effectively be provided in a residential treatment facility. OHIRT services are provided under the direction of a physician.
Providers should refer to the Code of Colorado Regulations, Program Rules (10 C.C.R. 2505-10), for specific information when providing OHIRT treatment.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for general billing information. Health First Colorado benefits are provided through Psychiatric Residential Treatment Facilities (PRTFs) and Out-of-state High Intensity Residential Treatment (OHIRT) Providers to enrolled members who reside in the facility on a per-diem basis.
PRTF/OHIRT Benefits
PRTFs and OHIRTs are responsible for providing clinical services to members residing in their facilities.
The following code can be billed for services provided in a PRTF/OHIRT:
| Code | Description |
| 0911 | Treatment in a PRTF, per diem (1 unit per day) |
The PRTF/OHIRT rate is inclusive of all services provided to the child in the facility, by facility staff, as part of the child’s Plan of Care. Services provided outside the facility or by non-facility staff are billed separately as fee-for-service (FFS). Examples of FFS claims that may be billed separately may include Dental or Vision services.
The Residential Provider Billing and Policy slides are available online.
Critical Incident and Serious Occurrence Reporting
PRTFs and OHIRTs are required to submit all critical incident reports that involve Health First Colorado (Colorado’s Medicaid program) members to the Department. This requirement does not replace or supersede any existing reporting requirements for other state agencies or departments.
All critical incidents, as defined in the Colorado Department of Human Services (CDHS) rule at 12 C.C.R. 2509-8: 7.701.2, must be reported to the Department for Health First Colorado members only, with non-member information being anonymized.
CDHS rule at 12 C.C.R. 2509-8: 7.701.2 states that critical incidents include death, abuse and neglect, injury, illness and emergency response. See the rule text for further details and explanation.
Providers must follow all critical incident reporting and timing requirements as described in CDHS rule at 12 C.C.R. 2509-8: 7.701.52 when reporting to the Department. CDHS rule at 12 C.C.R. 2509-8: 7.701.52 states that critical incidents must be reported within 24 hours, excluding weekends and holidays, of the occurrence of a critical incident at the facility or within 24 hours of a child’s return to the facility.
PRTFs and OHIRTs must report “serious occurrences,” as defined under 42 C.F.R. § 483.374, regardless of the individual’s Health First Colorado status. The federal regulations state that serious occurrences that must be reported include a resident’s death, a serious injury to a resident and a resident’s suicide attempt.
Staff must report any serious occurrence involving a resident to both the State Medicaid agency and the State-designated Protection and Advocacy system by no later than close of business the next business day after a serious occurrence. The report must include the name of the resident involved in the serious occurrence, a description of the occurrence and the name, street address and telephone number of the facility.
Critical Incidents and Serious Occurrences must be submitted to the Department via the Residential Childcare Provider Critical Incident Information Form.
Back to Top
Prior Authorization and Utilization Management (UM) Requirements
PRTF and OHIRT services must be provided and billed only by a licensed and certified PRTF or OHIRT provider.
OHIRTs outside of Colorado must work with the Department to submit for a prior authorization and continuing stay authorizations for services for members.
PRTF and OHIRT services are subject to UM approval. UM and Enhanced Standardized Assessment (ESA) requirements are located in Operational Memo OM 25-032.
UB-04 Paper Claim Reference Table
The information in the following table provides instructions for completing form locators (FL) as they appear on the paper UB-04 claim form. Instructions for completing the UB-04 claim form are based on the current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data form locators on the UB-04 have the same attributes (specifications) for Health First Colorado as those indicated in the NUBC UB-04 Reference Manual.
All code values listed in the NUBC UB-04 Reference Manual for each form locator may not be used for submitting paper claims to Health First Colorado. The appropriate code values listed in this manual must be used when billing Health First Colorado.
The UB-04 Institutional Certification Form, located on the Provider Forms web page under the Claim Forms and Attachments drop-down menu, must be completed and attached to all claims submitted on the paper UB-04. Completed UB-04 paper Health First Colorado claims, including hardcopy Medicare claims, should be mailed to the correct fiscal agent address listed in Appendix A - Colorado Department of Health Care Policy & Financing, located on the Billing Manuals web page under the Appendices drop-down.
Do not submit "continuation" claims. Each claim form has a set number of billing lines available for completion. Do not crowd more lines on the form.
Billing lines in excess of the designated number are not processed or acknowledged. Claims with more than one (1) page may be submitted through the Provider Web Portal.
Bill with a date span (From and To dates of service) only if the service was provided every consecutive day within the span. The From and To dates must be in the same month.
The Paper Claim Reference Table below lists the required, optional and/or conditional form locators for submitting the paper UB-04 claim form to Health First Colorado for nursing facility services.
| Form Locator and Labels | Completion Format | Instructions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Billing Provider Name, Address, Telephone Number | Text | Required
Abbreviate the state using standard post office abbreviations. Enter the telephone number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. Pay-to Name, Address, City, State | Text | Required only if different from FL 1. If the Pay-to Name and Address is the same as the reported Billing Provider, the Pay-to Name and Address must not be sent.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3a. Patient Control Number | Up to 20 characters: Letters, numbers or hyphens | Optional Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3b. Medical Record Number | 17 digits | Optional Enter the number assigned to the member to assist in retrieval of medical records. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. Type of Bill | 3 digits | Required
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. Federal Tax Number | Digits | Required Federal Tax Number must match the one associated with the provider’s enrolled NPI number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. Statement covers period From/Through | From:6 digits MMDDYY Through: 6 digits MMDDYY | Required Each date of service must be billed on a separate line. Refer to FL 45. On paper split an entire month into 2 claims. This form locator must reflect the beginning and ending dates of service. "From" date is the actual start date of services. "From" date cannot be prior to the start date reported on the initial prior authorization, if applicable, or is the first date of an interim bill. "Through" date is the actual discharge date, or final date of an interim bill. "From" and "Through" dates cannot exceed a calendar month (e.g., bill 01/15/10 thru 01/31/10 and 02/01/10 thru 02/15/10, not 01/15/10 thru 02/15/10). Dates must match the prior authorization if applicable. If member is admitted and discharged the same date, that date must appear in both fields. Detail dates of service must be within the "Statement Covers Period" dates. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8a. Patient Identifier | Text | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8b. Patient Name | Up to 25 characters, letters and spaces | Required Enter the member's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9a. Patient Address - Street | Characters Letters and numbers | Required Enter the member's street/post office box as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9b. Patient Address - City | Text | Required Enter the member's city as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9c. Patient Address - State | Text | Required Enter the member's state as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9d. Patient Address - ZIP | Digits | Required Enter the member's zip code as determined at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9e. Patient Address - Country Code | Digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10. Birthdate | 8 digits (MMDDCCYY) | Required Enter the member's birthdate using two (2) digits for the month, two (2) digits for the date, and four (4) digits for the year (MMDDCCYY format). Example: 01012010 for January 1, 2010. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. Patient Sex | 1 letter | Required Enter an M (male) or F (female) to indicate the member's sex. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. Admission Date | 6 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. Admission Hour | 6 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. Admission Type | 1 digit | Required Enter the following to identify the admission priority: 3 - Elective The member's condition permits adequate time to schedule the availability of accommodations. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. Source of Admission | 1 digit | Required Enter the appropriate code. (To be used in conjunction with FL 14, Admission Type.) 8 - Court/Law Enforcement 9 - Information not available | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. Discharge Hour | 2 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. Patient Discharge Status | 2 digits | Required
Claims with Member Status of 30, 31 or 32 will pay for each day billed on the detail lines, including the through date of service shown at the header. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18-28. Conditions Codes | 2 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. Accident State | 2 digits | Optional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31 - 34. Occurrence Code/Date | 2 digits and 6 digits | Not Required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35-36. Occurrence Span Code From/ Through | Digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38. Responsible Party Name/Address | None | Leave blank | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39 - 41. Value Codes and Amounts | 2 characters and up to 9 digits | Conditional
For Rancho Coma Score bill with appropriate diagnosis for head injury. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 42. Revenue Code | 4 digits | Required Enter the revenue code 0911. A revenue code must appear only once per date of service. If more than one (1) of the same service is provided on the same day, combine the units and charges on one (1) line accordingly. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 43. Revenue code Description | Text | Required Enter the revenue code description or abbreviated description. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 44. HCPCS/Rates/ HIPPS Rate Codes | 5 digits | Not required | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 45. Service Date | 6 digits | For span bills only Enter the date of service using MMDDYY format for each detail line completed. Each date of service must fall within the date span entered in the "Statement Covers Period" field (FL 6). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 46. Service Units | 3 digits | Required Enter a unit value on each line completed. Use whole numbers only. Do not enter fractions or decimals and do not show a decimal point followed by a 0 to designate whole numbers (e.g., Do not enter 1.0 to signify one [1] unit). For span bills, the units of service reflect only those visits, miles or treatments provided on dates of service in FL 45. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 47. Total Charges | 9 digits | Required Enter the total charge for each line item. Calculate the total charge as the number of units multiplied by the unit charge. Do not subtract Medicare or third-party payments from line charge entries. Do not enter negative amounts. A grand total on line 23 is required for all charges. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 48. Non-covered Charges | Up to 9 digits | Conditional Enter incurred charges that are not payable by the Health First Colorado. Non-covered charges must be entered in both FL 47 (Total Charges) and FL 48 (Non-Covered Charges.) Each column requires a grand total. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 50. Payer Name | 1 letter and text | Enter the payment source code followed by name of each payer organization from which the provider might expect payment. At least one (1) line must indicate Health First Colorado. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 51. Health Plan ID | 8 digits | Required Enter the provider's Health Plan ID for each payer name. Enter the eight (8)-digit Health First Colorado provider number assigned to the billing provider. Payment is made to the enrolled provider or agency that is assigned this number. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 52. Release of Information | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 53. Assignment of Benefits | N/A | Submitted information is not entered into the claim processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 54. Prior Payments | Up to 9 digits | Inpatient - Conditional Complete when there are Medicare or third-party payments. Enter third party and/or Medicare payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 55. Estimated Amount Due | Up to 9 digits | Conditional Complete when there are Medicare or third-party payments. Enter the net amount due from Health First Colorado after provider has received other third party, Medicare or member liability amount. Medicare Crossovers Enter the sum of the Medicare coinsurance plus Medicare deductible less third-party payments and member payments. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 56. National Provider Identifier (NPI) | 10 digits | Required Enter the billing provider's 10-digit National Provider Identifier (NPI). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 57. Other Provider ID | Optional Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 58. Insured's Name | Up to 30 characters | Required Enter the member's name on the Health First Colorado line. Other Insurance/Medicare Complete additional lines when there is third party coverage. Enter the policyholder's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 60. Insured's Unique ID | Up to 20 characters | Required Enter the insured's unique identification number assigned by the payer organization exactly as it appears on the health insurance card. Include letter prefixes or suffixes shown on the card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 61. Insurance Group Name | 14 letters | Conditional Complete when there is third party coverage. Enter the name of the group or plan providing the insurance to the insured exactly as it appears on the health insurance card. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 62. Insurance Group Number | 17 digits | Conditional Complete when there is third party coverage. Enter the identification number, control number, or code assigned by the carrier or fund administrator identifying the group under which the individual is carried. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 63. Treatment Authorization Code | Up to 18 characters | Conditional Complete when the service requires a PAR. Enter the authorization number in this FL if a PAR is required and has been approved for services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 64. Document Control Number | None | Conditional | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 65. Employer Name | Text | Conditional Complete when there is third party coverage. Enter the name of the employer that provides health care coverage for the individual identified in FL 58 (Insured Name). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 66. Diagnosis Version Qualifier | Submitted information is not entered into the claim processing system. Enter applicable ICD indicator to identify which version of ICD codes is being reported. 0ICD-10-CM (DOS 10/1/15 and after) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67. Principal Diagnosis Code | Up to 6 digits | Required Enter the exact ICD-10-CM diagnosis code describing the principal diagnosis that exists at the time of admission or develops subsequently and affects the length of stay. Do not add extra zeros to the diagnosis code. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 67A. - 67Q. - Other Diagnosis | 6 digits | Optional Enter the exact ICD-10-CM diagnosis code corresponding to additional conditions that co-exist at the time of admission or develop subsequently and which effect the treatment received or the length of stay. Do not add extra zeros to the diagnosis code. Enter applicable ICD indicator to identify which version of ICD codes is being reported. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 69. Admitting Diagnosis Code | 6 digits | Required Enter the ICD-10-CM diagnosis code as stated by the physician at the time of admission. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 70. Patient Reason Diagnosis | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 71. PPS Code | Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 72. External Cause of Injury code (E-Code) | 6 digits | Optional Enter the ICD-10-CM diagnosis code for the external cause of an injury, poisoning, or adverse effect. This code must begin with an "E". | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74. Principal Procedure Code/Date | 7 characters and 6 digits | Conditional Enter the ICD-10-CM procedure code for the principal procedure performed during this billing period and the date on which procedure was performed. Enter the date using MMDDYY format. Apply the following criteria to determine the principle procedure: The principal procedure is not performed for diagnostic or exploratory purposes. This code is related to definitive treatment, and The principal procedure is most related to the primary diagnosis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 74A. Other Procedure Code/Date | 7 characters and 6 digits | Conditional Complete when there are additional significant procedure codes. Enter the ICD-10-CM procedure codes identifying all significant procedures other than the principle procedure and the dates on which the procedures were performed. Report those that are most important for the episode of care and specifically any therapeutic procedures closely related to the principle diagnosis. Enter the date using MMDDYY format. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 76. Attending NPI - Required | NPI - 10 digits | Health First Colorado ID Required NPI - Enter the 10-digit NPI number assigned to the physician having primary responsibility for the member's medical care and treatment. This number is obtained from the physician and cannot be a clinic or group number. (If the attending physician is not enrolled in the Health First Colorado or if the member leaves the ER before being seen by a physician, the hospital may enter their individual numbers.) Hospitals and FQHCs may enter the member's regular physician's 10- digit NPI in the Attending Physician ID form locator if the locum tenens physician is not enrolled in the Health First Colorado. QUAL - Enter "1D" for Health First Colorado Enter the attending physician's last and first name. This form locator must be completed for all services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 77. Operating NPI | Optional Submitted information is not entered into the claim processing system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 78 - 79. Other ID | NPI - 10 digits | Conditional Complete when attending physician is not the PCP or to identify additional physicians. Ordering, Prescribing, or Referring NPI - when applicable NPI - Enter up to two (2) 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attending physician is not the PCP or if a clinic is a PCP agent, enter the PCP NPI number as the referring physician. The name of the Health First Colorado member's PCP appears on the eligibility verification. Review either for eligibility or PCP. Health First Colorado does not require that the PCP number appear more than once on each claim submitted. The attending physician's last and first name are optional. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 80. Remarks | Text | Enter specific additional information necessary to process the claim or fulfill reporting requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 81. Code - QUAL/CODE/VALUE (a-d) | Qualifier: 2 digits Taxonomy Code: 10 digits | Optional Complete both the qualifier and the taxonomy code for the billing provider in field 81CC-a. Field 81CC-a must be billed with qualifier B3 for the taxonomy code to be captured in the claims processing system. If B3 is missing, no taxonomy code will be captured in the claims processing system. Only one (1) taxonomy code can be captured from field 81CC. If more than one (1) taxonomy code is provided, only the first instance of B3 and taxonomy code will be captured in the claims processing system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
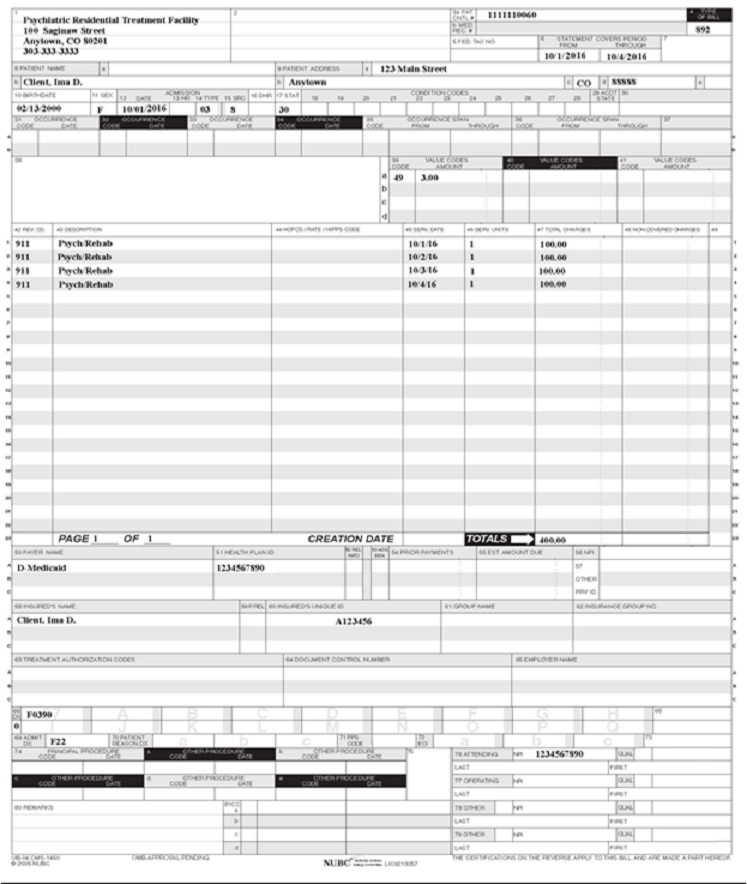
PRTF/OHIRT Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down menu for more information on timely filing policy, including the resubmission rules for denied claims.
Institutional Provider Certification
The Institutional Certification Form is located on the Provider Forms web page under the Claim Forms and Attachments drop-down.
This document is an addendum to the UB-04 claim form and is required per 42 C.F.R. 445.18 (a)(1-2) to be attached to paper claims submitted on the UB-04.
PRTF/OHIRT Revisions Log
| Revision Date | Section/Action | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 2/27/2016 | Updates based on the Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on the Colorado iC Stage II Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on the Colorado iC Stage II Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 3/13/2017 | Updated the Type of Bill section in the Paper Claims Table to reflect the NUBC manual | HCPF |
| 5/26/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 6/15/2018 | Updated timely filing information and removed references to LBOD, removed general billing information already available in the General Provider Information manual | DXC |
| 6/13/2019 | Updated Appendices' links and verbiage. | DXC |
| 12/9/2019 | Converted to web page. | HCPF |
| 8/7/2020 | Updated item 81 of the Paper Claim Reference Table for taxonomy code billing | DXC |
| 4/22/2022 | Update PRTF policies and language edits | HCPF |
| 4/7/2023 | Added link to Provider webinar and slides | HCPF |
| 12/7/2023 | Update claim instructions, added RAE links, typo cleanup | HCPF |
| 4/4/2025 | Added links to Critical Incident and Serious Occurrence Reporting section. | HCPF |
| 10/23/2025 | Updated title of document. Critical Incident and Serious Occurrence Reporting. Add UM info. Add OHIRT | HCPF |