Nurse Home Visitor Program Billing Manual
- Targeted Case Management Guidance
- Documentation in Member Records
- General Billing Information
- Enrollment and Participation
- Procedure/HCPCS Codes Overview
- NHVP Procedure/Diagnosis Coding
- CMS 1500 Paper Claim Instructional Reference Table
- Timely Filing
- Nurse Home Visitor Program Revisions Log
Return to Billing Manuals Web Page
The Nurse Home Visitor Program (NHVP) is a program available to first-time pregnant women or women whose first child is less than one (1) month old and who are at or below 200% of the Federal Poverty Level. ("First-time" is defined as no previous live birth, Health First Colorado (Colorado's Medicaid program) only reimburses for services for Health First Colorado-eligible members.) Participating sites must be certified by the Colorado Department of Human Services (CDHS) as NHVP providers.
Reimbursement for targeted case management (TCM) services is available through this program when provided to Health First Colorado-eligible women who are pregnant with their first child (or have had no previous live birth), and the mother and child up to the child's 2nd birthday.
Nurse Home Visitor Program providers must be enrolled as Health First Colorado providers in order to receive Health First Colorado reimbursement for TCM activities. Reimbursement is provided on a fee-for-service (FFS) basis. Fee-for-service reimbursement for TCM services provided by an NHVP provider is also available for members enrolled in a managed care program. Providers should refer to the Code of Colorado Regulations, Program Rules (10 CCR 2505-10), for specific information regarding NHVP services.
Targeted Case Management Guidance
Targeted Case Management (TCM) includes four (4) core activities:
- Assessment of the first-time pregnant woman and her first child's needs for health, mental health, social services, education, housing, childcare and related services
- Development of care plans to obtain the needed services
- Referral to resources to obtain the needed services, including medical providers who provide care to a first-time pregnant woman and her first child
- Routine monitoring and follow-up visits with the women where progress in obtaining the needed services is monitored, problem-solving assistance is provided and the care plans are revised to reflect the woman's and child's current needs
It is not necessary to provide all four (4) components at every visit. However, in order to bill for TCM, at least one (1) of the components must be provided to or on behalf of the member. The "member," in the context of this billing manual, refers to the Health First Colorado enrollee to whom or on behalf of whom the TCM is being provided. (For example, in the context of this billing manual, if/when the mother becomes ineligible for Health First Colorado, she is no longer a "member.")
Examples of TCM include:
- Discussions with providers, school counselors, etc. about assessments, progress, referrals
- Discussions with member's (mom or baby) family members about progress of the member, etc. (member can be present or not)
- Communication with the mother about meeting the needs of the child
- Time spent finding/researching appropriate referrals for a member based on assessments
Examples of services that are not TCM:
- Direct care/services
- Education
- Driving to visits
- Transporting the member
- Case conferencing with other Nurse Home Visitors/supervisors not directly involved with the member
- Billing activities and data entry
- Time spent charting
When billing TCM for the mother using the mother's Health First Colorado ID, the TCM services provided must be directly related to the assessment of the mother's needs, development of the mother's care plan, referrals to resources that will aid in meeting the needs of the mother, or routine monitoring and follow-up of the mother's progress in meeting her needs and achieving her goals.
When billing TCM for the child using the child's ID, the TCM services provided must be directly related to the assessment of the child's needs, development of the child's care plan, referrals to resources that will aid in meeting the needs of the child, or routine monitoring and follow-up of the family's progress in meeting the identified needs of the child.
Documentation in Member Records
Every claim for TCM reimbursement must be supported by clear evidence in the member's record/chart. In order for TCM reimbursement to be claimed for any given member, date, or unit amount, corresponding evidence must exist in the member's record.
Elements that should be easily identifiable by an external reviewer include:
- Evidence that at least one (1) component of TCM was provided,
- The Health First Colorado member to whom or on behalf of whom the TCM was provided (If the claim is billed using the child's Health First Colorado ID, the child's name must be evident on the record.),
- The specific dates of service on which the TCM was rendered, and
- The amount of time spent providing TCM (either an actual notation of time or a description of services comprehensive enough that time spent providing TCM could be accurately estimated).
The notations in the chart should support the number of units billed. For instance, if two (2) units of TCM are billed but the only notation in the chart reads, "Referred member to WIC," that notation does not necessarily support the number of units billed. A more complete reference that may more fully support the number of billed units could be, "Spoke with member about quantity and variety of food in household, assessed member for adequate nutrition standards, referred member to WIC to meet nutrition needs."
Targeted Case Management services provided to or on behalf of the mother should be billed using the mother's Health First Colorado ID and the notations in the chart should support that the services were provided to or on behalf of the mother. Targeted Case Management services provided to or on behalf of the child should be billed using the child's Health First Colorado ID and evidence in the chart should support that the services were provided to or on behalf of the child. Services provided to or on behalf of the mother after she is no longer eligible for Health First Colorado are not billable to Health First Colorado and may not be billed using the child's Health First Colorado ID. For every claim submitted using the child's Health First Colorado ID, evidence in the chart supporting this claim and unit amount should specifically describe TCM services provided to or on behalf of the child.
Even if span billing is used, there must be evidence in the member's chart of specific services and specific dates of service. Refer to the Span Billing section below.
General Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page for general billing information.
Enrollment and Participation
Participating providers must be certified by the CDHS as NHVP providers. Nurse Home Visitor Program providers must meet established program training requirements, program protocols, program management information systems requirements, and program evaluation requirements for research-based model programs that have demonstrated significant reductions in infant behavioral impairments, the number of reported incidents of child abuse and neglect, the number of subsequent pregnancies, receipt of public assistance and criminal activity.
All NHVP services must be provided by a registered nurse. Nurse home visitors must be licensed as professional nurses pursuant to Article 38 of Title 12, C.R.S., or accredited by another state or voluntary agency that the state board of nursing has identified by rule pursuant to Section 12-38-108(1)(a), C.R.S., as one (1) whose accreditation may be accepted in lieu of board approval. Nurse supervisors are required to be nurses with Master's degrees in nursing or public health, unless the implementing entity can demonstrate that such a person is either unavailable within the community or an appropriately qualified nurse without a Master's degree is available.
The rendering nurses must be enrolled as Health First Colorado providers, and the rendering nurses' NPI must be affiliated with the billing provider under which the NHVP claims are submitted.
Procedure/HCPCS Codes Overview
The codes used for submitting claims for services provided to Health First Colorado members represent services that are approved by the Centers for Medicare & Medicaid Services (CMS) and services that may be provided by an enrolled Health First Colorado provider.
The Healthcare Common Procedural Coding System (HCPCS) is divided into two (2) principal subsystems, referred to as level I and level II of the HCPCS.
Level I of the HCPCS is comprised of Current Procedural Terminology (CPT), a numeric coding system maintained by the American Medical Association (AMA).
The CPT is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other health care professionals.
Level II of the HCPCS is a standardized coding system that is used primarily to identify products, supplies, and services not included in the CPT codes, such as ambulance services and durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) when used outside a physician's office. Level II codes are also referred to as alpha-numeric codes because they consist of a single alphabetical letter followed by four (4) numeric digits, while CPT codes are identified using five (5) numeric digits.
NHVP Procedure/Diagnosis Coding
NHVP Procedure Coding
Target Case Management services may be provided to, or on behalf of, the woman during the prenatal period and through the month of the first child's second birthday during any month in which the woman is Health First Colorado-eligible. Targeted Case Management services provided to, or on behalf of, the woman must be billed on a separate claim from TCM services provided to, or on behalf of, the child. The following procedure code may be billed for TCM services provided to, or on behalf of, the woman:
| Code | Description | Prior Authorization |
| G9006 | Coordinated care fee, home monitoring | No PA |
Targeted Case Management services may be provided to, or on behalf of, the child through the month of his/her second birthday during any month in which the child is Health First Colorado-eligible. Targeted Case Management services provided to, or on behalf of, the child must be billed on a separate claim from TCM services provided to, or on behalf of, the woman. The following procedure code may be billed for TCM services provided to, or on behalf of, the child:
| Code | Description | Prior Authorization |
| T1017 | Targeted case management, each 15 minutes | No PA |
Modifiers
All claims for TCM services provided through NHVP must include one (1) of the procedure codes listed above plus the HD modifier, signifying that the services are part of a pregnant/parenting women's program. Claims submitted without this modifier will be denied.
Maximum Allowable Units of Service
Reimbursement for TCM provided through NHVP is made on a per-unit basis, where one (1) unit is equal to fifteen (15) minutes. A maximum of fifteen (15) units of service will be reimbursed in any calendar month per mother/child couple. The maximum 15 units per calendar month may be divided between the mother and child if both are Health First Colorado-eligible in the same month.
The maximum 15 units of service may be provided in the home/off-site setting, in the office, or a combination of both home/off-site and office.
Time spent on TCM should be rounded to the nearest whole unit. For example, if 5 minutes of TCM are provided, no units may be billed. If 10 minutes of TCM are provided, 1 unit may be billed. If 23 minutes of TCM are provided, 2 units may be billed.
Place of Service
TCM Services in the Home or Off-Site Setting
Each NHVP provider agency has an agency-specific reimbursement rate for TCM services provided in the member's home or other off-site setting (such as the member's school, work, or any other location to which the nurse home visitor must travel). This agency-specific reimbursement rate includes a calculation to account for mileage costs. All TCM services provided at a location other than the NHVP provider office must be billed using Place of Service Code 12 (Home).
TCM Services in the Office Setting
All NHVP provider agencies are reimbursed the same rate for TCM services provided to, or on behalf of, the woman and/or the child when those services take place at the NHVP provider offices. All TCM services that take place at the office must be billed using a Place of Service Code other than 12, signifying that the services were rendered in a setting that did not require the nurse home visitor to travel. Alternative Place of Service Codes include but are not limited to 11 (Office), 50 (Federally Qualified Health Center - FQHC), and 72 (Rural Health Center - RHC).
Home/Off-Site TCM and Office TCM Provided on the Same Date of Service or Span*
If Home/Off-Site TCM and Office TCM are provided to a member on the same date of service or span, two (2)-line items must be used, each with the appropriate Place of Service code. Modifier HD should be used on both line items. Additionally, Modifier 76 ("Repeat procedure or service") must be used as the second modifier on the second line item. If Modifier 76 is not used on the second line item, the second line item will be denied as a duplicate. When the claim is processed, the MMIS suspects that a service is being duplicated when it identifies two (2)-line items with the same date of service or span and with the same procedure code, regardless of the difference in the place of service. Modifier 76 must be used on the second line item to signal that it is indeed a separate service from the first line item.
Example:
| Home and Office TCM on Same Date | Line 1 | Line 2 |
| 2 units of Home TCM on 10/6/16 1 unit of Office TCM on 10/6/16 | From Date:10/6/16 To Date: 10/6/16 Place of Service: 12 Units: 2 Modifier(s): HD | From Date: 10/6/16 To Date: 10/6/16 Place of Service: 11 Units: 1 Modifier(s): HD + 76 |
Refer to the Span Billing section below for more information on span billing.
NHVP Diagnosis Coding
Diagnosis codes that are appropriate for this program include but are not limited to the following:
| Member Description and Stage | Line 1 | Line 2 |
|---|---|---|
| Pregnant Women | Z34.00 | Encounter for supervision of normal first pregnancy, unspecified trimester |
| Z34.01 | Encounter for supervision of normal first pregnancy, first trimester | |
| Z34.02 | Encounter for supervision of normal first pregnancy, second trimester | |
| Z34.03 | Encounter for supervision of normal first pregnancy, third trimester | |
| Z34.80 | Encounter for supervision of other normal pregnancy, unspecified trimester | |
| Z34.81 | Encounter for supervision of other normal pregnancy, first trimester | |
| Z34.82 | Encounter for supervision of other normal pregnancy, second trimester | |
| Z34.83 | Encounter for supervision of other normal pregnancy, third trimester | |
| Z34.90 | Encounter for supervision of normal pregnancy, unspecified, unspecified trimester | |
| Z34.91 | Encounter for supervision of normal pregnancy, unspecified, first trimester | |
| Z34.92 | Encounter for supervision of normal pregnancy, unspecified, second trimester | |
| Z34.93 | Encounter for supervision of normal pregnancy, unspecified, third trimester | |
| O09.00 | Supervision of pregnancy with history of infertility, unspecified trimester | |
| O09.01 | Supervision of pregnancy with history of infertility, first trimester | |
| O09.02 | Supervision of pregnancy with history of infertility, second trimester | |
| O09.03 | Supervision of pregnancy with history of infertility, third trimester | |
| O09.10 | Supervision of pregnancy with history of ectopic or molar pregnancy, unspecified trimester | |
| O09.11 | Supervision of pregnancy with history of ectopic or molar pregnancy, first trimester | |
| O09.12 | Supervision of pregnancy with history of ectopic or molar pregnancy, second trimester | |
| O09.13 | Supervision of pregnancy with history of ectopic or molar pregnancy, third trimester | |
| O09.291 | Supervision of pregnancy with other poor reproductive or obstetric history, first trimester | |
| O09.40 | Supervision of pregnancy with grand multiparity, unspecified trimester | |
| O09.41 | Supervision of pregnancy with grand multiparity, first trimester | |
| O09.42 | Supervision of pregnancy with grand multiparity, second trimester | |
| O09.43 | Supervision of pregnancy with grand multiparity, third trimester | |
| Mother from Delivery through ~2-3 Months Postpartum | Z39.2 | Encounter for routine postpartum follow-up |
| Mother After ~2-3 Months Postpartum to Child's 2nd Birthday | Z02.9 | Encounter for administrative examinations, unspecified |
| Child - Infancy through 2nd Birthday | Z76.2 | Encounter for health supervision and care of other healthy infant and child |
Billing for Members with Commercial Insurance and Health First Colorado
Targeted case management services provided under the NHVP are exempt from commercial billing requirements. This means that when a member has both commercial insurance and Health First Colorado, NHVP providers are not required to submit claims to commercial payers prior to billing Health First Colorado.
Span Billing
Span billing is an alternative method for billing NHVP services. Span billing is a method of billing for one (1) service provided to the same member over a period of time as one (1) line item, rather than billing each encounter separately with individual dates of service. For instance, if TCM was provided to the same member on three (3) different dates of service, a span of dates can be entered in the "From Date" field and the "To Date" field on one (1) line item, rather than billing three (3)-line items for each separate date of service.
Examples:
| Span Scenario 1 | Line 1 | Line 2 |
| 4 units of Home TCM on 10/2/16 5 units of Home TCM on 10/23/16 No Office TCM provided | From Date: 10/1/16 or 10/2/16 To Date: 10/23/16 or 10/31/16 Place of Service: 12 Units: 9 Modifier(s): HD | |
| Span Scenario 2 | Line 1 | Line 2 |
| 2 units of Home TCM on 10/6/16 1 unit of Office TCM on 10/6/16 3 units of Home TCM on 10/16/16 2 units of Office TCM on 10/21/16 | From Date:10/1/13 or 10/6/16 To Date: 10/21/13 or 10/31/16 Place of Service: 12 Units: 5 Modifier(s): HD | From Date: 10/1/16 or 10/6/16 To Date: 10/21/16 or 10/31/16 Place of Service: 11 Units: 3 Modifier(s): HD + 76 |
The span "From Date" and the span "To Date" should be within the same month (10/1/16 - 10/31/16, not 10/15/16 - 11/15/16).
No other claims for that member for that service with dates of service within the span can be processed once the span claim has been submitted. If additional units of the service need to be billed during the span dates after the original span claim has been submitted, the original span claim must be adjusted to add the units. A new claim with the additional units cannot be processed.
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional, and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's Health First Colorado seven (7)-digit Health First Colorado ID number as it appears on the Health First Colorado identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two (2) digits for the month, two digits for the date, and two digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Patient's Relationship to Insured | Conditional | Complete if the member is covered by a commercial health insurance policy. Place an "X" in the box that identifies the member's relationship to the policyholder. | ||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured's last name, first name and middle initial. | ||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one (1) or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's policy number as it appears on the ID card. Only complete if field 4 is completed. | ||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured's birth date using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the insured. | ||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Conditional | Complete if information is known. Enter the date of illness, injury or pregnancy, (date of the last menstrual period) using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070114 for July 1, 2014. Enter the applicable qualifier to identify which date is being reported. 431 - Onset of Current Symptoms or Illness 484 - Last Menstrual Period | ||||||||||||||||||||||||||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 17b. NPI of Referring Physician | Required | Required in accordance with Program Rule 8.125.8.A | ||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Conditional | Complete if all laboratory work was referred to and performed by an outside laboratory. If this box is checked, no payment will be made to the physician for lab services. Do not complete this field if any laboratory work was performed in the office. Practitioners may not request payment for services performed by an independent or hospital laboratory. | ||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the member's diagnosis/condition. Enter applicable ICD-10 indicator. | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010119 for January 1, 2019.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes. All TCM services that are provided at a location other than the NHVP provider office must be billed with Place of Service Code: 11 - Office 50 - Federally Qualified Health Center 72 - Rural Health Clinic | ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not required | |||||||||||||||||||||||||||||||||||||
| 24D. | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually. HCPCS Level II Codes The current Medicare coding publication (for Medicare crossover claims only). Only approved codes from the current CPT or HCPCS publications will be accepted. NHVP TCM services provided to, or on behalf of the woman: G9006 - Coordinated care fee, home monitoring TCM services provided to, or on behalf of the child: T1017 - Targeted case management, each 15 minutes | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Required | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. HD - Pregnant/Parenting Women's Program This signifies that the service is part of a pregnant/parenting women's program. | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. NHVP One (1) unit equals 15 minutes of TCM. In any given calendar month, the maximum number of reimbursable units is 150 for the mother/child couple. The 15 units may be split between the woman and the child in any given calendar month that both are Medicaid-eligible. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Conditional | EPSDT (shaded area) For Early and Periodic Screening, Diagnosis and Treatment related services, enter the response in the shaded portion of the field as follows: AV - Available- Not Used S2 - Under Treatment ST - New Service Requested NU - Not Used Family Planning (unshaded area) If the service is Family Planning, enter "Y" for YES or "N" for NO in the bottom, unshaded area of the field. | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Example: 070116 for July 1, 2016. | ||||||||||||||||||||||||||||||||||||
| 32. Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name, address and ZIP code of the individual or business where the member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
Child - Single Date of Service - Home TCM
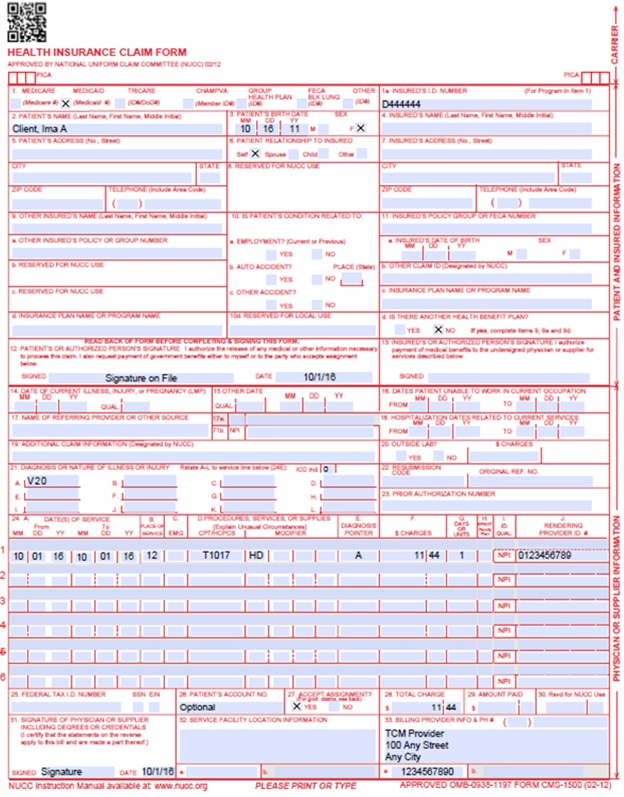
Example Only - TCM Rates with Place of Service "12" are provider-specific.
Pregnant Woman - Single Date of Service - Home TCM and Office TCM on Same Date
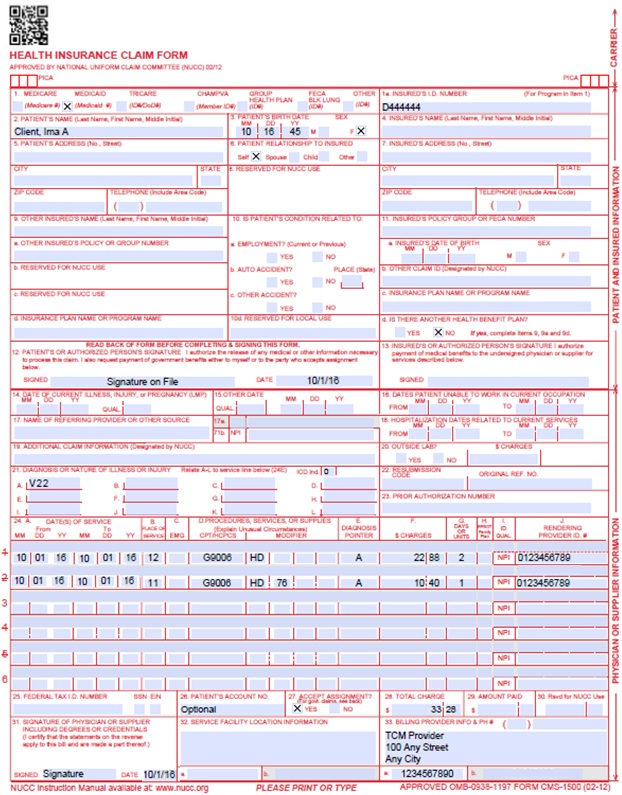
Example Only - TCM Rates with Place of Service "12" are provider-specific.
Pregnant Woman - Span Dates of Service - Home TCM and Office TCM during Same Span
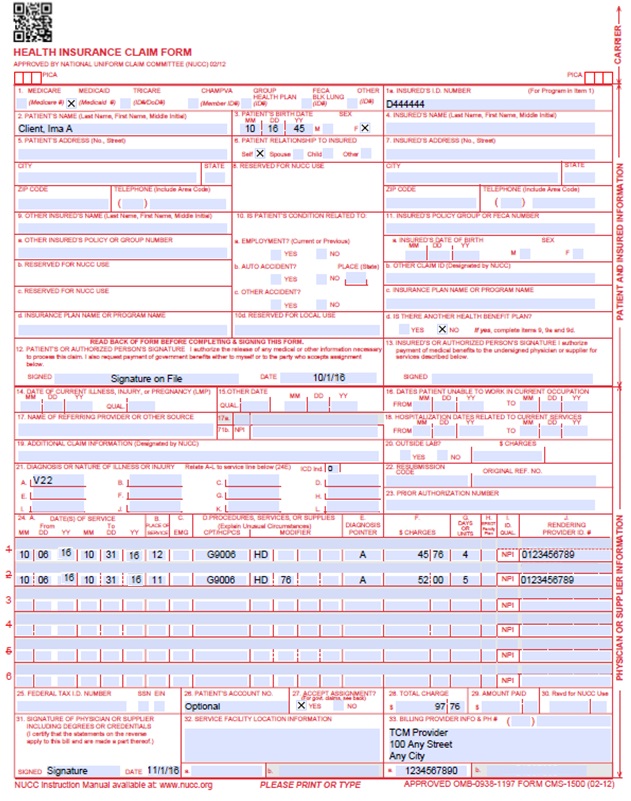
Example Only - TCM Rates with Place of Service "12" are provider-specific.
Mother after 2-3 Months Postpartum - Single Date of Service - Home TCM
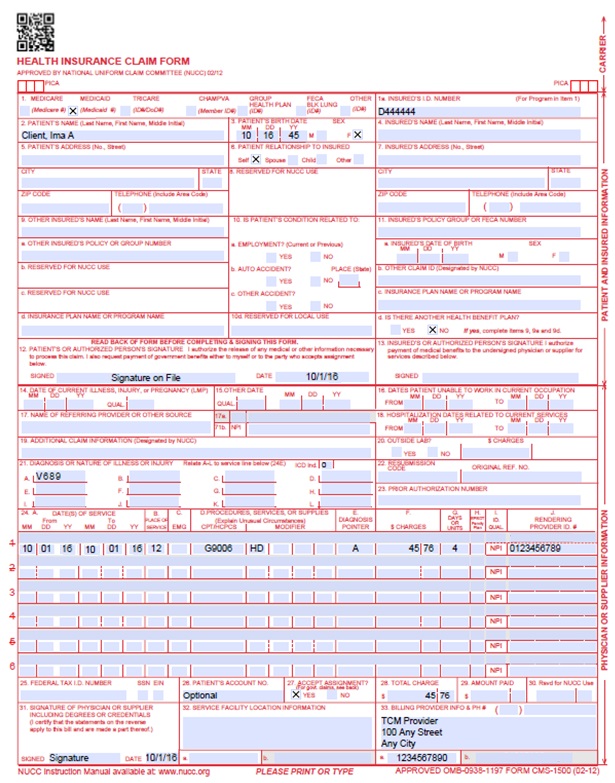
Example Only - TCM Rates with Place of Service "12" are provider-specific.
Timely Filing
Refer to the General Provider Information Manual available on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
NHVP Revision Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016. Please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 5/22/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 6/22/2018 | Updated billing and timely to point to General Manual | HCPF |
| 12/21/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 1/13/2020 | Conversion to web page | HCPF |
| 9/14/2020 | Added Line to Box 32 under the CMS 1500 Paper Claim Reference Table | HCPF |