Ensuring Full Continuum SUD Benefits
Substance Use Disorder Services
The Department of Health Care Policy and Financing (the Department) is committed to better health outcomes for the whole person by offering a full range of healthcare services for Health First Colorado (Colorado’s Medicaid program) members. Health First Colorado members get physical health and dental services and are also eligible for behavioral health services, which include substance use disorder (SUD) treatment. Behavioral health services including SUD treatment are available to all members without the need for a referral or copay. Health First Colorado members can find SUD benefit information in the member handbook. Providers looking for more information about offering SUD services can go to the SUD provider page.
The current SUD benefit ensures a full continuum of care as outlined by The American Society of Addiction Medicine (ASAM). ASAM establishes guidelines for what services are available at each level of care. It’s also a uniformed approach to identifying the most appropriate level of care for a member based on their individual needs. The ASAM criteria is a nationally recognized, evidence-based system that guides clinicians with matching patient needs to specific levels of care.
Colorado uses ASAM Criteria to determine Level of Care placement for members. Office of Behavioral Health provider licensing rules align with the ASAM criteria descriptions of each level of care.
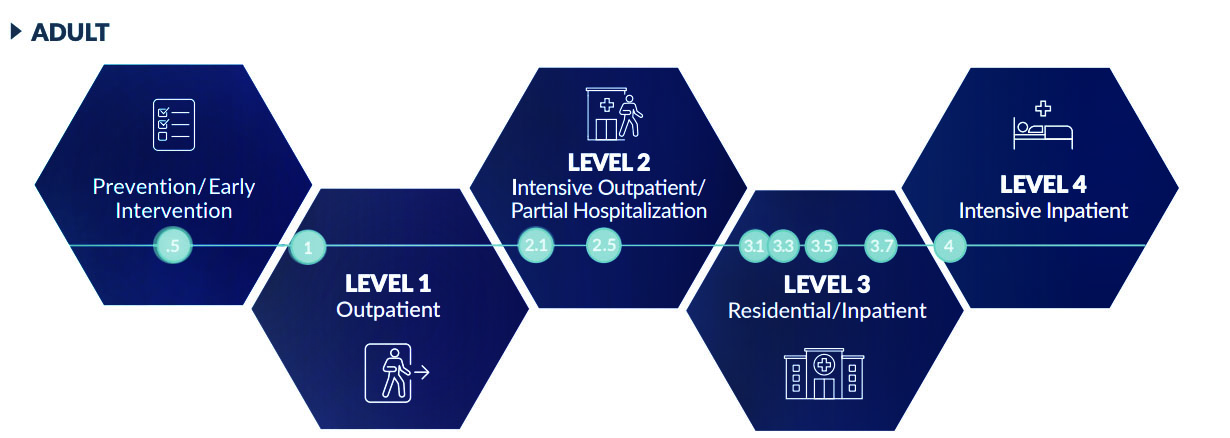
| Level of Care | Description |
|---|---|
| Prevention | .5 Early Intervention |
| Level 1 | 1 Outpatient Services |
| Level 2 | 2.1 Intensive Outpatient Services 2.5 Partial Hospitalization Services |
| Level 3 | 3.1 Clinically Managed Low-Intensity Services 3.3 Clinically Managed Population Specific High-Intensity Residential Services 3.5 Clinically Managed High-Intensity Residential Services 3.7 Medically Monitored Intensive Inpatient Services |
| Level 4 | 4 Medically Managed Intensive Inpatient Services |
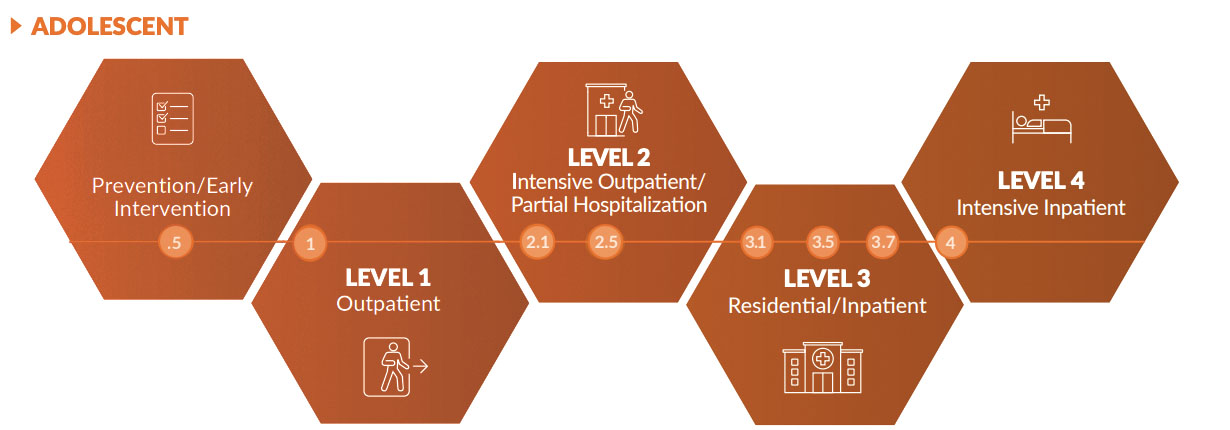
| Level of Care | Description |
|---|---|
| Prevention | .5 Early Intervention |
| Level 1 | 1 Outpatient Services |
| Level 2 | 2.1 Intensive Outpatient Services 2.5 Partial Hospitalization Services |
| Level 3 | 3.1 Clinically Managed Low-Intensity Services 3.5 Clinically Managed High-Intensity Residential Services 3.7 Medically Monitored Intensive Inpatient Services |
| Level 4 | 4 Medically Managed Intensive Inpatient Services |
Services ranging from screening and harm reduction to outpatient, intensive outpatient and medication-assisted treatment services to withdrawal management (also known as) "detox" to both residential and hospital inpatient services, are all available treatment options for members. Providers work to find the right level of care that meets the member’s specific needs.
SUD Residential Care in Colorado
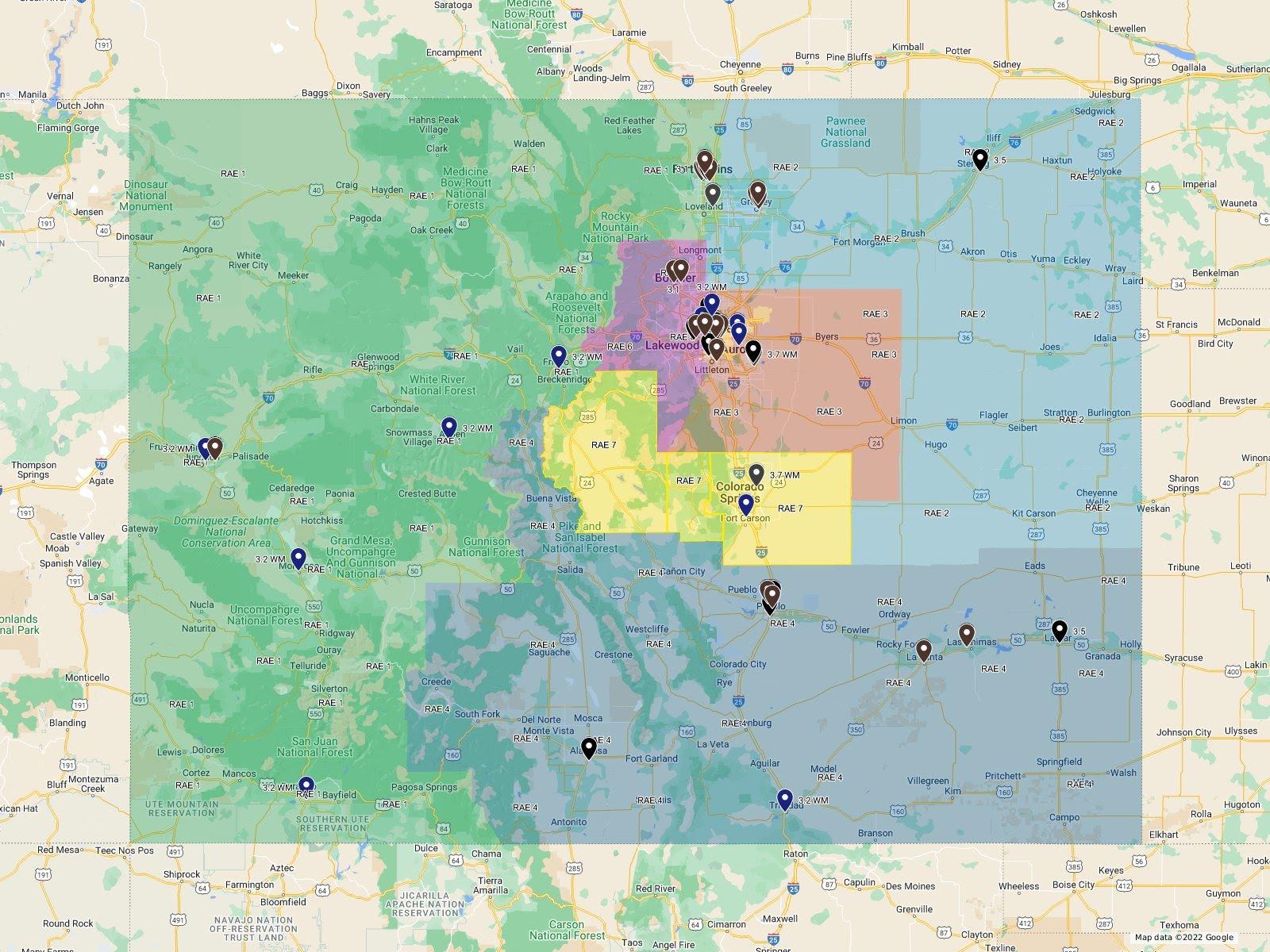
Providers are included on the SUD Residential Services Map searchable by level of ASAM care or region, they meet the following criteria:
- Licensed to provide care at a specific ASAM level and
- Enrolled as Health First Providers at that ASAM level
- The Department maintains a full list of SUD providers enrolled in Health First Colorado and contracted with the MCEs.
In addition, the map includes information about which MCEs a provider is contracted with to provide services to members from that region.
Take Note/Learn More
Register for 2026 Quarterly SUD Provider Forums
The Quarterly SUD Provider Forum is open to providers and other stakeholders to learn about changes and updates to policies, service delivery, and billing in the SUD continuum of care. The forum is also an opportunity for interested parties to ask questions and raise concerns. Suggestions for presentations and topics are accepted by email submission to hcpf_sudbenefits@state.co.us.
Meetings are held on the first Wednesday of the quarter from 2:00 - 3:00pm. You can choose to register for any or all dates below using the registration page. SUD Provider Forum Agenda.
2025 Quarterly SUD Provider Forum Dates:
- January 7, 2026 | SUD Provider Benefit Forum Follow-Up Notes Jan 2026
- April 1, 2026
- July 1, 2026
- October 7, 2026
Questions for HCPF about the SUD benefit? Join our monthly SUD Office Hours!
HCPF hosts monthly SUD Office Hours on the first Wednesday of the month from 2-3pm (when there is no SUD Provider Forum) to answer questions from providers regarding the SUD benefit. There is no structured presentation during Office Hours so please only register if you have a question and list your question on the Zoom registration form.
Transplant Patients with SUD Diagnosis – Protocol for SUD Treatment
Patients who are transplant recipients with an SUD diagnosis should receive comprehensive SUD treatment services in accordance with ASAM continuum of care guidelines. HCPF, in collaboration with MCEs, has developed an SUD treatment protocol for transplant recipients providing guidance regarding expectations for continuum of care SUD services for these members. The member’s MCE (RAE or MCO) is responsible to coordinate care when notified by a transplant team of the need for these services.
State Legislative Requirements and Reporting
SUD Utilization Management Reports produced in accordance with SB 21-137 for demonstration years 1 and 2 of the SUD of the expanded SUD benefit have been archived. Please contact the SUD benefit team by SUD benefits email if you need a copy of the reports from demonstration years 1 and 2.
SUD Utilization Management Report Demonstration Year 3 Annual Report
You can find the other Demonstration Year 3 reports on the Regulatory Resource Center Webpage.
Resources
- ASAM Criteria and Utilization Management Training
- Colorado Crisis Services
- Primary Prevention | Overdose Prevention Strategy
- US Department of Health and Human Services Overdose Prevention Strategy | ASPE
- Colorado Department of Law Opioid Crisis Response Project
- Learn More About The Recovery Cards Project
- Find Behavioral Health Help
- SUD Services Overview & FAQ
Stay Informed
We encourage you to sign up for SUD Benefits updates.
Ask a question or make a suggestion: hcpf_sudbenefits@state.co.us