Backdating a New Enrollment Application
Providers are able to request an enrollment effective date up to ten (10) months prior to the current date. This only applies to providers starting a new enrollment application and providers resuming an application that is still in process.
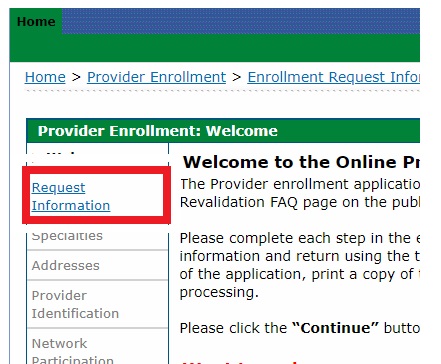
- Access the Provider Enrollment Portal.
- Acknowledge the Welcome panel by clicking Continue.
Click the Request Information link.
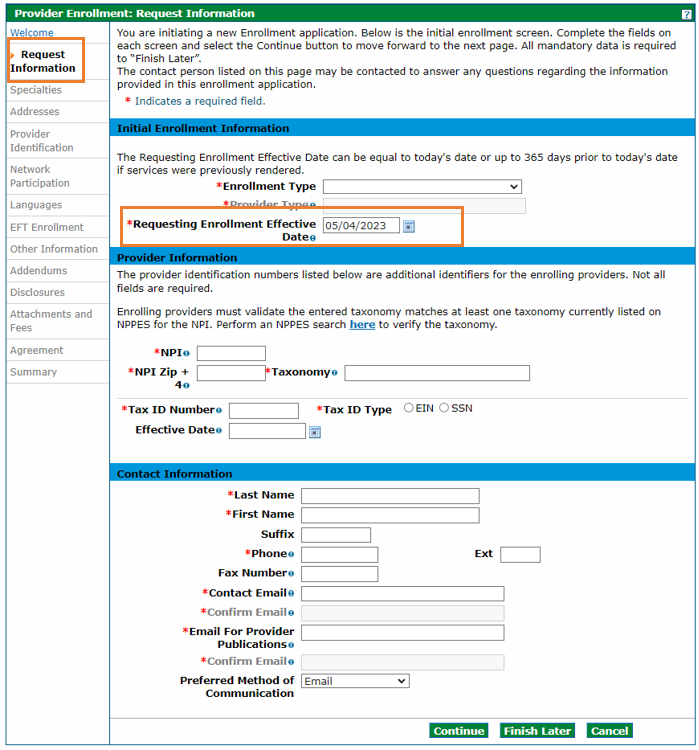
For providers starting a new enrollment application, the Requesting Enrollment Effective Date field automatically defaults to the current date for new enrollment applications. Providers may enter a backdate up to ten (10) months prior to the current date in this field.
For providers resuming an enrollment application that is still in process, the Requesting Enrollment Effective Date field will be populated with the date entered when the application was last saved. That date must be within ten (10) months prior to the current date.
Providers should complete the remainder of the enrollment application and submit it. If the enrollment and backdate request are approved, the provider will receive a Welcome Letter which will contain the provider’s backdated contract effective date.
Need More Help?
Visit the Provider Enrollment web page to find more resources on enrollment.