Home and Community-Based Services Billing Manual: Children's Home and Community-Based Services (CHCBS), Children with Complex Health Needs (CwCHN)
- Case Management Agency Responsibilities
- Claim Submission
- Prior Authorization Requests (PARs)
- Denver Regional Pricing
- Children's Home and Community-Based Services (CHCBS)
- Home and Community-Based Services for Children with Complex Health Needs (CwCHN)
- Paper Claim Reference Table
- Timely Filing
- HCBS-CHCBS and CwCHN Specialty Manuals Revisions Log
Return to Billing Manuals Web Page
Home and Community Based Services (HCBS) Waiver programs provide additional Health First Colorado (Colorado's Medicaid program) benefits to specific populations who meet special eligibility criteria.
Level of care determinations are made annually by Case Management Agencies contracted by the Department to provide case management for eligible and enrolled Health First Colorado Members. Eligible Members must meet financial, medical and program criteria to access services under a waiver. The applicant must be at risk of transition to a Nursing Facility (NF), hospital or Intermediate Care Facility for Individuals with an Intellectual Disability (ICF/IID). In order to access waiver benefits, Members must be willing to receive services in their homes or communities. A Member who receives services through a waiver is also eligible for all basic Health First Colorado-covered services except nursing facility and long-term hospital care. When a Member chooses to receive services under a waiver, the services must be provided by certified Health First Colorado Providers or by a Health First Colorado contracting Managed Care Organization (MCO).
Applicants may apply for more than one (1) waiver but may only receive services through one (1) waiver at a time.
The New Children’s Waiver for Complex Health Needs (CWCHN):
Alongside the implementation of Community First Choice (CFC), The Department of Health Care Policy and Financing (HCPF) took the opportunity to streamline the waiver programs available for medically complex children in Colorado and expanded services options for these children.
On July 1, 2025, the Children with Life Limiting Illness (CLLI) Waiver was merged with the Children’s Home and Community Based Services (CHCBS) Waiver and was renamed as the Children with Complex Health Needs (CwCHN) Waiver. This change ensures existing CHCBS members have continued access to HCBS and Health First Colorado services while also expanding benefits and streamlining services for medically fragile children. The services available in the CwCHN Waiver include all services currently available in CLLI.
The eligibility criteria for the CwCHN Waiver was expanded to include both the CLLI and CHCBS Waiver populations. Children must be under 19 years of age and meet a level of care equivalent to a nursing facility or hospital. To meet a hospital level of care, children must be determined by a licensed medical professional to be medically complex or have a life-limiting illness.
All eligible and enrolled CLLI Members experienced a waiver name change to CwCHN July 1, 2025. Between July 1, 2025, and June 30, 2026, all eligible and enrolled CHCBS Members will be transitioned to the CwCHN waiver at the time of their Continued Stay Review (CSR). This manual reflects the services available to eligible and enrolled Members for the CHCBS and CwCHN Waivers based on their CSR date, through June 30, 2026. The CHCBS Waiver will remain open throughout the transition year to allow for CHCBS members to gradually transition to the new CwCHN waiver on their CSR date. There will be no new CHCBS enrollments as of July 1, 2025. CHCBS will sunset July 1, 2026.
Case Management Agency Responsibilities
Contracted Case Management Agencies are delegated administrative authority over HCBS waivers.
Contracted Case Management Agencies responsibilities include, but are not limited to:
- Informing Members and/or legal guardians of the eligibility process.
- Developing the appropriate Prior Approval and/or Cost Containment Record Form of services and projected costs for approval.
- Submitting a copy of the Prior Authorization and/or Cost Containment document to the authorizing agent. Refer to Appendix D located on the Billing Manuals web page under the Appendices drop-down for a list of authorizing agents.
- Assessing the Member's health and social needs.
- Arranging for face-to-face contact with the Member.
- Monitoring and evaluating services.
- Reassessing each Member annually or upon a change in condition.
Claim Submission
Submission of claims for services rendered must not be duplicative. Provider Agencies cannot be reimbursed for delivering the same service to the same Member on the same day at the same time; whether such services are billed on the same claim, or on multiple/different claims. Additionally, Provider Agencies are barred from billing services that share or have overlapping service definitions, but are described by different procedure codes, on the same day, to the same Member. Collectively referred to as duplicate claims, reimbursement for such claims requires clear documentation of the necessity of the service, and that there was not duplicative service delivery.
Refer to the service definitions on the Colorado Code of Regulations website to identify if claims are duplicative. Refer to the provider specialty code enrollment requirements on the HCBS Provider Specialty Code List web page to identify services that must be provided by an individual provider. Provider Agencies may only bill for services approved in the Members’ service plans.
In any instance in which duplicate billings result in Medicaid reimbursement, a recovery shall be made by the Department against the Provider Agency.
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for general billing information, including claim submission information.
Prior Authorization Requests (PARs)
Unless otherwise noted, all HCBS services require prior approval before they can be reimbursed by Health First Colorado. Contracted Case Management Agencies complete the Prior Approval and/or Cost Containment requests for their specific programs according to instructions published in the regulations for the Department.
Providers may contact the Contracted Case Management Agency for the status of the PAR or inquire electronically through the Health First Colorado Provider Web Portal.
Approval of prior authorization does not guarantee Health First Colorado payment and does not serve as a timely filing waiver. Prior authorization only assures that the approved service is a medical necessity and is considered a benefit of Health First Colorado. All claims, including those for prior authorized services, must meet eligibility and claim submission requirements (e.g., timely filing, provider information completed appropriately, required attachments included, etc.) before payment can be made. Provider Agencies are reminded to check Member eligibility prior to rendering services.
Prior approvals must be completed thoroughly and accurately. If an error is noted on an approved request, it should be brought to the attention of the Member's Case Manager for corrections. Procedure codes, quantities, etc., may be changed or entered by the Member's Case Manager.
The authorizing agent or Contracted Case Management Agency is responsible for timely submission and distribution of copies of approvals to Provider Agencies and providers contracted to provide services.
Denver Regional Pricing
Certain HCBS delivered to members while they are within the City and County of Denver are eligible for higher rates. Information relative to these services, and guidance on the applicability of these rates to certain services, can be found in the Denver Minimum Wage Pricing Appendix, on the Department’s billing manual page under “HCBS”.
Children's Home and Community-Based Services (CHCBS)
The HCBS-CHCBS waiver program is for medically fragile children who are at risk of institutionalization in a hospital or skilled nursing facility and would not otherwise qualify for Health First Colorado services due to parental income and/or resources. All state plan Health First Colorado benefits are provided to children birth through age 17. The children must meet the established minimum criteria for hospital or skilled nursing facility level of care. Members that meet program eligibility requirements receive an annual long-term care certification by their Contracted Case Management Agency Case Manager.
CHCBS Procedure Code Table
Provider Agencies may bill the following procedure codes for HCBS-CHCBS services.
In-Home Support Services (IHSS)
IHSS within the CHCBS waiver is limited to health maintenance activities, which include support for activities of daily living. Additionally, IHSS providers must provide core independent living skills.
Specialty 656: HCBS-CHCBS Procedure Code Table
| Description | Procedure Code | Modifiers | Units |
|---|---|---|---|
| Health Maintenance Activities – Outside Denver County | H0038 | U5 | 1 unit = 15 minutes |
Wellness Education Benefit (WEB)
The WEB is designed to reduce the need for a higher level of care by offering educational materials that provide Members and their families with actionable tools that can be used to prevent the progression of a disability, increase community engagement, combat isolation and improve awareness of Health First Colorado services.
Specialty 683: HCBS-CHCBS Procedure Code Table
Wellness Education Benefit (WEB)
| Description | Procedure Code | Modifiers | Units |
|---|---|---|---|
| Wellness Education Benefit | 98960 | U5 | 1 unit per month |
Home and Community-Based Services for Children with Complex Health Needs (CwCHN)
The Children with Complex Health Needs (CwCHN) Waiver is for medically complex children from birth through age 19 who meet either a nursing facility or hospital level of care. Level of care determinations are conducted annually by Contracted Case Management Agencies. Services include Bereavement Counseling, Expressive Therapy (Art, Play and Music), Massage Therapy, Palliative/Supportive Care (Care Coordination and Pain and Symptom Management), Respite Care and Therapeutic Life Limiting Illness Support Services. Members that are enrolled in the waiver also have access to all state plan Health First Colorado benefits, including curative care.
HCBS-CwCHN Procedure Code Table
Provider Agencies may bill the following procedure codes for HCBS-CLLI services:
HCBS-CwCHN Procedure Code Table
| Description | Procedure Code | Modifiers | Place of Service | Units |
|---|---|---|---|---|
| Specialty 645: Expressive Therapy-Art/Play | ||||
| Art and Play Therapy | H2032 | UD, HA | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Art and Play Therapy - Group | H2032 | UD, HA, HQ | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Specialty 646: Expressive Therapy- Music Therapy | ||||
| Music Therapy | H2032 | UD | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Music Therapy - Group | H2032 | UD, HQ | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Specialty 613: Massage Therapy | ||||
| Massage Therapy | 97124 | UD | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Specialty 614: Palliative/Supportive Care | ||||
| Care Coordination | G9012 | UD | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Pain and Symptom Management | S9123 | UD | 11 - Office 12 - Home 34 - Hospice | 1 unit = 1 hour |
| Specialty 616: Respite (Unskilled) | ||||
| Respite Care - Unskilled (4 hours or less) - Outside Denver County | S5150 | UD | 12 - Home | 1 unit = 15 minutes |
| Respite Care - Unskilled (4 hours or more) - Outside Denver County | S5151 | UD | 12 - Home | 1 unit = 1 day |
| Respite Care – Camp (Group, Overnight) - Outside Denver County | T2037 | UD | 1 unit = 1 day | |
| Specialty 615: Respite (Skilled) | ||||
| Respite Care - CNA (4 hours or less) | T1005 | UD | 12 - Home | 1 unit = 15 minutes |
| Respite Care - CNA (4 hours or more) | S9125 | UD | 12 - Home | 1 unit = 1 day |
| Respite Care - Skilled RN, LPN (4 hours or less) | T1005 | UD, TD | 12 - Home | 1 unit = 15 minutes |
| Respite Care - Skilled RN, LPN (4 hours or more) | S9125 | UD, TD | 12 - Home | 1 unit = 1 day |
| Specialty 617: Therapy and Counseling | ||||
| Bereavement Counseling | S0257 | UD, HK | 11 - Office 12 - Home | 1 unit = lump sum |
| Therapeutic Life Limiting Illness Support - Individual | S0257 | UD | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Therapeutic Life Limiting Illness Support - Family | S0257 | UD, HR | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Therapeutic Life Limiting Illness Support - Group | S0257 | UD, HQ | 11 - Office 12 - Home | 1 unit = 15 minutes |
| Specialty 683: Wellness Education Benefit (WEB) | ||||
| Wellness Education Benefit | 98960 | UD | 1 unit per month | |
Service Limitations
Reimbursement for HCBS-CwCHN Therapeutic Life Limiting Illness Support services (S0257 with any "UD" modifier) shall be limited to 98 hours per annual certification. Reimbursement for HCBS-CwCHN respite care services (T1005, S9125, S5150 and S5151) shall be limited to 30 days (unique dates of service) per annual certification. Reimbursement for HCBS-CwCHN respite care services (T1005, S9125, S5150 and S5151) shall not be duplicated at the same time of service as state plan Home Health or Palliative/Supportive Care services (S9123) and shall be denied. Expressive Therapy (H2032 - Art, Play and Music) is limited to 39 hours per annual certification. Massage Therapy (97124) is limited to 24 hours per annual certification.
Paper Claim Reference Table
The following paper form reference table gives required and/or conditional fields for the paper CMS 1500 claim form for HCBS-CHCBS and CwCHN claims:
| CMS Field Number and Label | Field is? | Instructions | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Insurance Type | Required | Place an "X" in the box marked as Medicaid. | ||||||||||||||||||||||||||||||||||||
| 1a. Insured's ID Number | Required | Enter the Member's Health First Colorado seven (7)-digit ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||||||||||||||||||||||||||
| 2. Patient's Name | Required | Enter the Member's last name, first name, and middle initial. | ||||||||||||||||||||||||||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the Member's birth date using two (2) digits for the month, two (2) digits for the date, and two (2) digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the Member. | ||||||||||||||||||||||||||||||||||||
| 4. Insured's Name | Not required | |||||||||||||||||||||||||||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 6. Client Relationship to Insured | Not Required | |||||||||||||||||||||||||||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||||||||||||||||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||||||||||||||||||||||||||
| 9. Other Insured's Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 9a. Other Insured's Policy or Group Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 9d. Insurance Plan or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 10a-c. Is patient's condition related to? | Not Required | |||||||||||||||||||||||||||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||||||||||||||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | |||||||||||||||||||||||||||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||||||||||||||||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||||||||||||||||||||||||||
| 11d. Is there another Health Benefit Plan? | Not Required | |||||||||||||||||||||||||||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||||||||||||||||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||||||||||||||||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||||||||||||||||||||||||||
| 15. Other Date | Not Required | |||||||||||||||||||||||||||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||||||||||||||||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||||||||||||||||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||||||||||||||||||||||||||
| 19. Additional Claim Information | Conditional | |||||||||||||||||||||||||||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||||||||||||||||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one (1) but no more than 12 diagnosis codes based on the Member's diagnosis/condition. Enter applicable ICD-10 indicator. HCBS CHCBS and CwCHN may use R69 | ||||||||||||||||||||||||||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||||||||||||||||||||||||||
| 23. Prior Authorization | Not Required | HCBS Leave blank | ||||||||||||||||||||||||||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six (6) detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six (6) lines of information on the paper claim. If more than six (6) lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||||||||||||||||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two (2) dates: a "From" date of services and a "To" date of service. Enter the date of service using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 010116 for January 1, 2016.
or
Span dates of service
Practitioner claims must be consecutive days. | ||||||||||||||||||||||||||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||||||||||||||||||||||||||
| 24C. EMG | Not Required | |||||||||||||||||||||||||||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. HCBS Refer to the CHCBS or CwCHN procedure code tables. | ||||||||||||||||||||||||||||||||||||
| 24D. Modifier | Required | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four (4) modifiers may be entered when using the paper claim form. Refer to the CHCBS or CwCHN procedure code tables. | ||||||||||||||||||||||||||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one (1) diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of four (4) characters in the unshaded area. | ||||||||||||||||||||||||||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one (1) procedure from the same group is billed, special multiple pricing rules apply. The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one (1) procedure from the same grouping is performed. Submitted charges cannot be more than charges made to non-Health First Colorado-covered individuals for the same service. Do not deduct Health First Colorado co-pay or commercial insurance payments from the usual and customary charges. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | Required | Enter the number of services provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||||||||||||||||||||||||||
| 24G. Days or Units | General Instructions | A unit represents the number of times the described procedure or service was rendered. Except as instructed in this manual or in Health First Colorado bulletins, the billed unit must correspond to procedure code descriptions. The following examples show the relationship between the procedure description and the entry of units. Home and Community-Based Services Combine units of services for a single procedure code for the billed time period on one (1) detail line. Dates of service do not have to be reported separately. Example: If forty units of personal care services were provided on various days throughout the month of January, bill the personal care procedure code with a From Date of 01/03/XX and a To Date of 01/31/XX and 40 units. | ||||||||||||||||||||||||||||||||||||
| 24H. EPSDT/Family Plan | Not Required | EPSDT shaded area) Not Required Family Planning (unshaded area) Not Required | ||||||||||||||||||||||||||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||||||||||||||||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI of the Health First Colorado provider number assigned to the individual who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||||||||||||||||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||||||||||||||||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the Member or claim in the Provider Agency's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||||||||||||||||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the Provider Agency agrees to accept assignment under the terms of the payer's program. | ||||||||||||||||||||||||||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||||||||||||||||||||||||||
| 29. Amount Paid | Not Required | |||||||||||||||||||||||||||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||||||||||||||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled Provider Agency or the signature of a registered authorized agent. Each claim must have the date the enrolled Provider Agency or registered authorized agent signed the claim form. Enter the date the claim was signed using two (2) digits for the month, two (2) digits for the date and two (2) digits for the year. Example: 070124 for July 1, 2024. | ||||||||||||||||||||||||||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Conditional | Enter the name, address and ZIP code of the individual or business where the Member was seen or service was performed in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | ||||||||||||||||||||||||||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||||||||||||||||||||||||||
| 33a- NPI Number | Required | |||||||||||||||||||||||||||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight (8)-digit Health First Colorado provider number of the individual or organization. | |||||||||||||||||||||||||||||||||||||
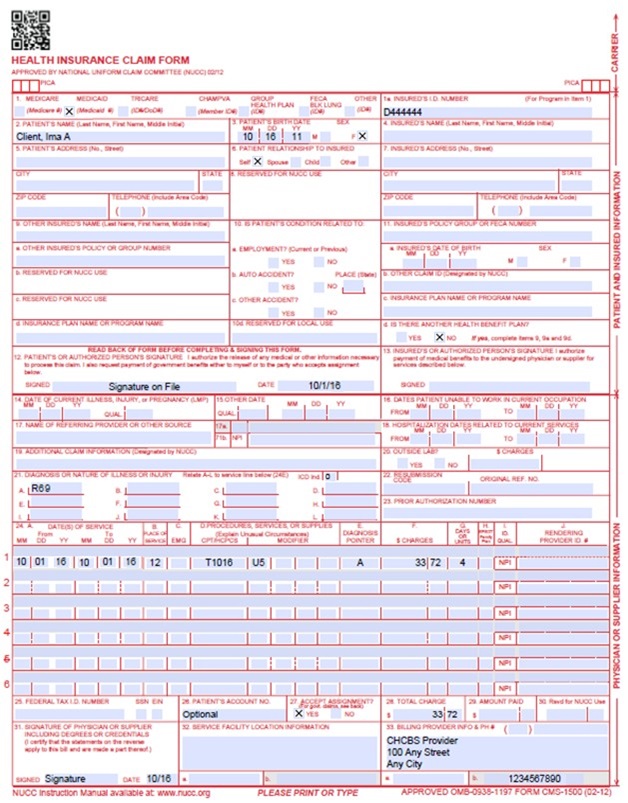
CMS 1500 CHCBS Claim Example
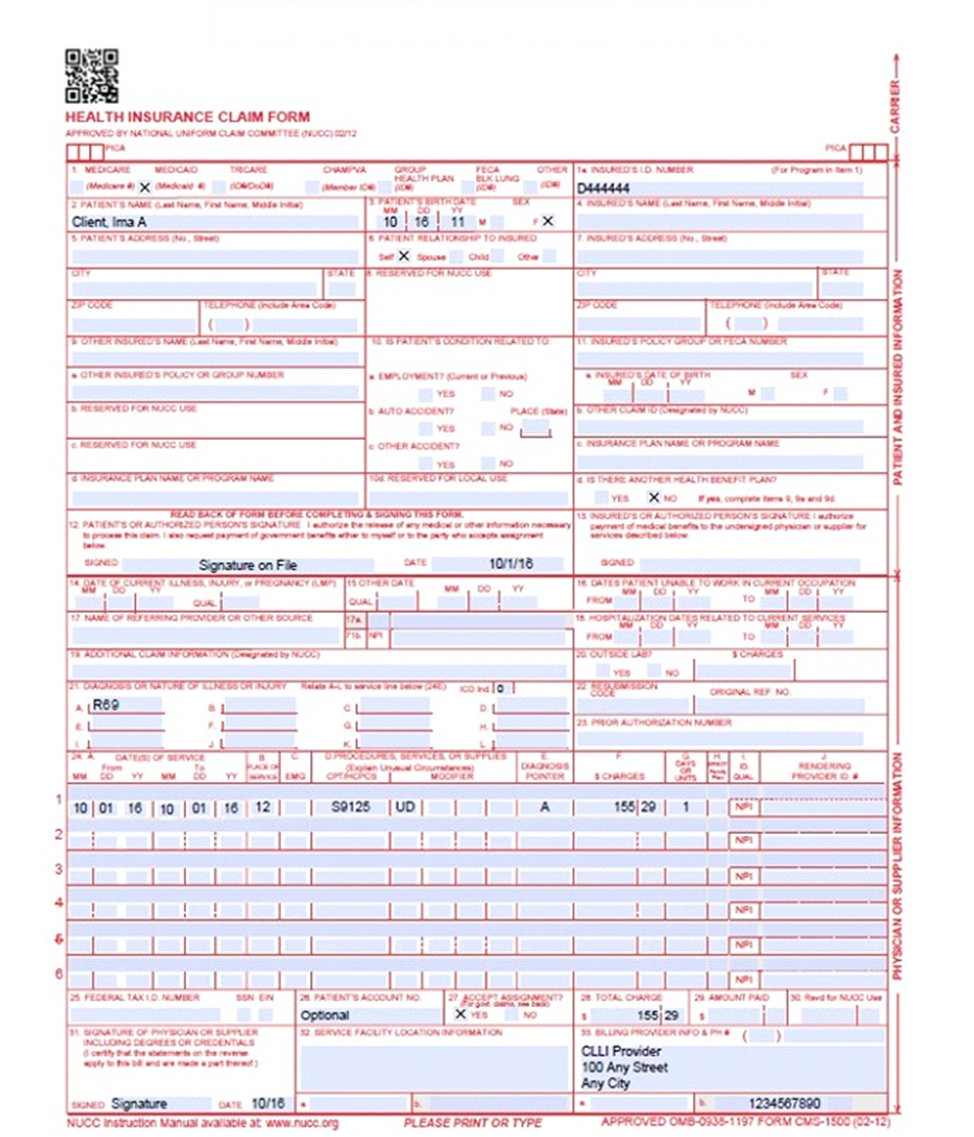
CMS 1500 HCBS-CwCHN Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
HCBS-CHCBS and CwCHN Specialty Manuals Revisions Log
| Revision Date | Addition/Changes | Made by |
|---|---|---|
| 12/1/2016 | Manual revised for interChange implementation. For manual revisions prior to 12/01/2016, please refer to Archive. | HPE (now DXC) |
| 12/27/2016 | Updates based on Colorado iC Stage II Provider Billing Manuals Comment Log v0_2.xlsx | HPE (now DXC) |
| 1/10/2017 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_3.xlsx | HPE (now DXC) |
| 1/19/2017 | Updates based on Colorado iC Stage II Provider Billing Manual Comment Log v0_4.xlsx | HPE (now DXC) |
| 1/26/2017 | Updates based on Department 1/20/2017 approval email | HPE (now DXC) |
| 2/10/2017 | Removed all references to Special Program Codes | HCPF |
| 3/13/2017 | Changed Modifier code from UL to U2 | HCPF |
| 5/26/2017 | Updates based on Fiscal Agent name change from HPE to DXC | DXC |
| 6/15/2018 | Updated timely filing information and removed references to LBOD, removed general billing information already available in the General Provider Information manual | DXC |
| 6/27/2018 | Updated ToC, minor edits, added link to general manual for claim submission info, updated Timely Filing | HCPF |
| 12/20/2018 | Clarification to signature requirements | HCPF |
| 3/18/2019 | Clarification to signature requirements | HCPF |
| 7/2/2019 | Updated Appendices' links and verbiage | DXC |
| 3/9/2020 | Converted to web page, removed CWA sections as waiver discontinued 7/2018 | HCPF |
| 3/24/2020 | Removed CWA references other than stating when the program was discontinued, removed outdated images. | HCPF |
| 9/14/2020 | Added Line to Box 32 under the Paper Claim Reference Table | HCPF |
| 10/31/2022 | Added Specialty Number | HCPF |
| 4/3/2023 | Updated AWS URL Links | HCPF |
| 4/25/2024 | Added new Denver County codes, CHCBS WEB service, and completed corrections | HCPF |
| 6/22/2024 | Removed case management services pursuant to Case Management Redesign. | HCPF |
| 7/19/2024 | Added duplicative claim language to Claims Submission | HCPF |
| 12/19/24 | Updated codes, added reference to Denver Regional Pricing Appendix. | HCPF |
| 04/02/2025 | Added WEB Benefit to CLLI. | HCPF |
| 07/01/2025 | Revised manual to reflect retitling of the Children with Life Limiting Illness Waiver (CLLI) effective June 30, 2025. | HCPF |