Invest in Tools & Technology
The Need
The HCBS system is complex with a number of technology systems and an enormous data infrastructure. To adequately prepare for the future, these systems need continual maintenance and updates. The tools and technologies the Department uses not only impact our administrative functions, but each is integral to our providers’ ability to perform their contractual obligations and to provide care to our members.
In addition, technological advancement is necessary to support our members and their families who rely on our systems to access services, seek resources, and gauge provider quality. For these reasons, the Department proposes a package of investments to elevate our current suite of tools and technology and to develop new and emerging systems that will prepare us for the future.
Initiative 6.01 - Home Health/PDN Acuity Tool
Read a more in-depth summary of this project's outcomes
Initiative 6.02 - Specialty Search in Provider Specialty Tool
Read a more in-depth summary of this project's outcomes
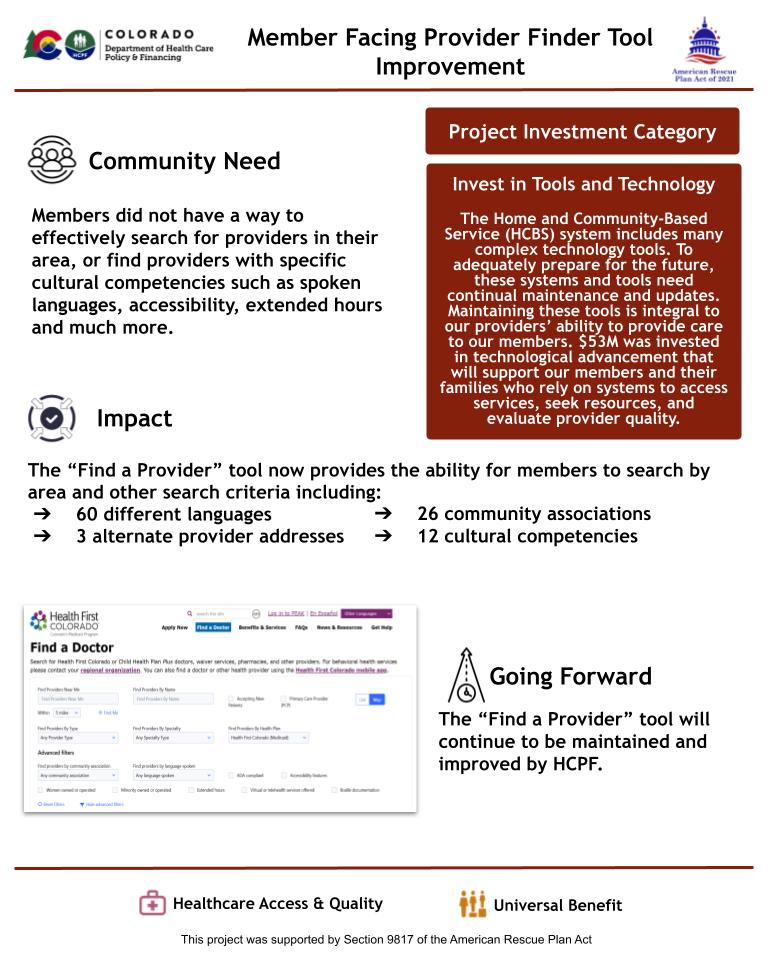
Initiative 6.03 - Member Facing Provider Finder Tool Improvement
Read a more in-depth summary of this project's outcomes
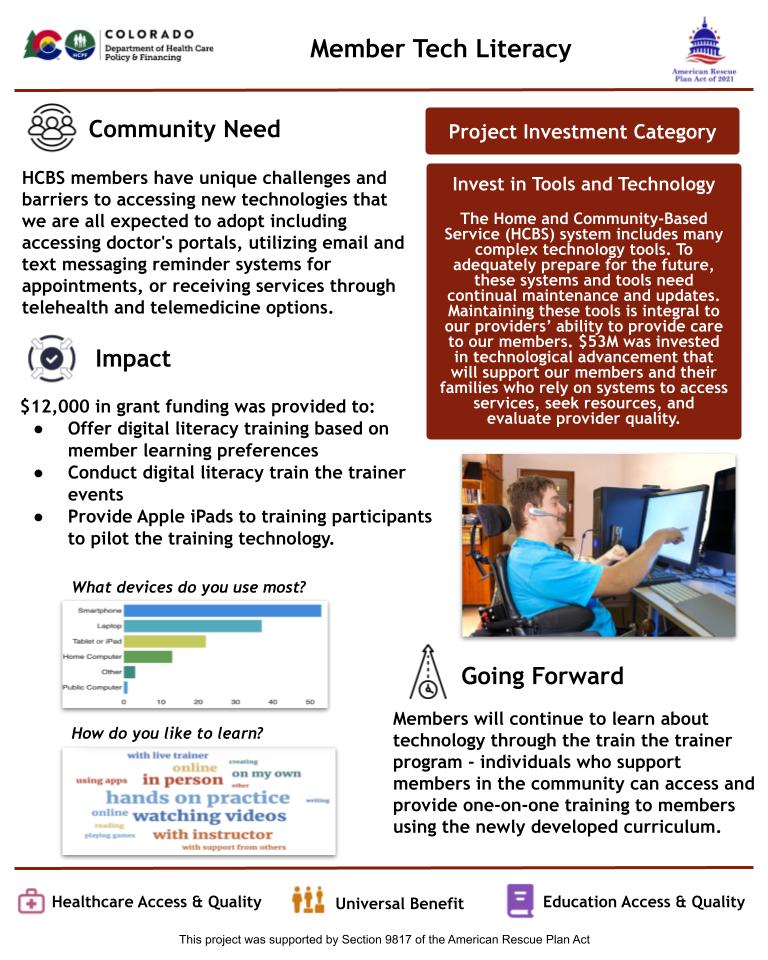
Initiative 6.05 - Member Tech Literacy
Read a more in-depth summary of this project's outcomes
Initiative 6.06 - HCBS Provider Digital Transformation
Read a more in-depth summary of this project's outcomes
Initiative 6.08 - Care & Case Management System
Read a more in-depth summary of this project's outcomes
Initiative 6.09 - Updates to Salesforce Database
Read a more in-depth summary of this project's outcomes
Initiative 6.11 - Centers of Excellence in Pain
Read a more in-depth summary of this project's outcomes
Initiative 6.12 - Systems Infrastructure for Social Determinants of Health
Read a more in-depth summary of this project's outcomes

Initiative 6.13 - Connect CMAs to ADT Data
Read a more in-depth summary of this project's outcomes
Initiative 6.14 - Data Sharing with the State Unit on Aging
Read a more in-depth summary of this project's outcomes

Initiative 6.15 - Interface with Trails
Read a more in-depth summary of this project's outcomes