- Targeted Case Management Transition Coordination (TCM-TC)
- Allowable Targeted Case Management (Transition) Activities
- Documenting Targeted Case Management- Transition Coordination
- Targeted Case Management – Transition Coordination Procedure Code Table
- Targeted Case Management – Transition Coordination Paper Claim Reference Table
- Timely Filing
- Targeted Case Management – Transition Services Specialty Manuals Revisions Log
Return to Billing Manuals Web Page
Targeted Case Management Transition Coordination (TCM-TC)
Targeted Case Management-Transition Coordination (TCM-TC) is an optional Health First Colorado (Colorado's Medicaid program) benefit available to eligible Health First Colorado members. Targeted Case Management (TCM) Services are provided by enrolled Transition Coordination Agencies. Billing must be performed with Agencies' Provider Type 11 enrollment. Providers can contact the Department's fiscal agent if they are unsure of which Provider ID to use.
The benefit provides transition coordination support to eligible members wishing to transition into community settings from institutional settings. The benefit includes comprehensive assessment for transition, community risk assessment, development of a transition plan, referral, and monitoring/follow-up activities.
Member Eligibility
Members are only eligible for the TCM-TC if they meet the following criteria:
- Determined financially eligible for Health First Colorado
- Determined eligible for a Home and Community Based Services (HCBS) waiver by Single Entry Point (SEP) agency or Community Centered Board (CCB); or
- Reside in a Nursing Facility or Intermediate Care Facility for Members with Intellectual Disabilities (ICF-IID) or Regional Center
- Have expressed interest in moving to a community-based setting
- Be 18 years of age or older
Allowable Targeted Case Management (Transition) Activities
Billable Activities: Overview
The five (5) areas listed below are the general areas for which providers are allowed to bill.
- Assessment: accurate evaluation of a participant's strengths, needs, preferences, supports and desired outcomes.
- Service Planning: developing a specific care plan that enables a member to meet member goals.
- Referral: provision of information to help participants choose qualified providers and plan to assure providers follow the service plan.
- Monitoring and Remediation: ensuring participants get authorized services and that services meet member needs and goal. Resolution of problems when something goes wrong as well as anticipate the potential for problems.
- Other Transition Coordination: Advocate for services in the service plan.
Billable Activities: Definitions and Sample Tasks
Facilitation of Transition Options Team process to complete a comprehensive community needs and risk assessment and periodic reassessment of member needs to determine the need for community-based supports and services.
Assessment - Sample Tasks
- Gathering information from a member regarding his/her needs, preferences and concerns related to community living;
- Identifying the member's community living goals in community living;
- Gathering information from other sources such as family members, medical providers, and/or social workers to form a complete community needs assessment of the member; and
- Completing related documentation.
- Facilitate transition options team meetings and discussions to complete community needs and risk assessments
- Obtain and review any relevant and/or required information needed for the completion of the community needs and risk assessments
- Reassess risk mitigation needs based on new information, change in condition or the occurrence of an incident related to identified risk factor.
Development (and periodic revision) of Transition and Risk Mitigation Plans:
- Based on the information collected through member's comprehensive assessment, which includes Transition Options Team members
- Addresses a member's needs, preferences, risks factors and community living goals in a person-centered way;
- Addresses all needs, preferences and risk factors identified in the Community Needs Assessment and Risk Mitigation Plan;
- Identifies all services, community resources and housing components the member needs to function in the community and to prevent institutionalization or risk incidents,
- Identifies a course of action to respond to the assessed needs, preferences and risks of the member;
- Identifies risks to the member's health, welfare, and safety and mitigation strategies to address these needs.
- Provide the level of assistance needed by each member to complete create a transition budget.
- Work with the Transition Options Team to develop an alternative plan to address a need or preference if a provider is not available for a required service or support.
Service and Support Coordination
Coordination of the non-Health First Colorado services and supports being provided as identified in the Transition Plan and the Risk Mitigation Plan to ensure continuity of service and support provision.
Service Planning/Coordination Sample Tasks
- Complete, as needed, housing voucher application, including assistance to obtain necessary documents.
- Collaborate, as needed, with housing navigation services to obtain a voucher and locate housing.
- Coordinate with property managers regarding housing issues
- Create a transition budget with member.
- Facilitate a community-based living arrangement.
- Coordinate any medication, home modification and/or durable medical equipment needs with the nursing facility prior to discharge to ensure that all components of transition plan are in place prior to a discharge.
- Assist member in preparing for discharge, including being present on day of discharge
- Obtain required documents necessary for voucher application and/or housing applications
- Communication with HCBS case managers, RAE Coordinators, behavioral health case managers regarding service delivery and concerns.
- Inter-agency contact/coordination.
- Coordination when member is hospitalized or re-institutionalized.
- Facilitating communication between Transition Options Team members and agencies
- Coordinate with case managers for transfers between programs, agencies and service areas (e.g., discharge to another service area and/or conclusion of TC participation).
- Respond and provide follow-up to issues identified by member and/or support system and help to provide resolution.
- Conduct service brokering for non-Health First Colorado services to determine if the identified necessary supports and services are available at the frequency needed.
- Ensure continuity of care by preparing member for disenrollment from transition coordination and arrange other community resources as needed to maintain successful community living 90 days prior to transition coordination disenrollment.
Risk Mitigation Plan Review:
- Periodic utilization reviews to assure that services, supports and prevention strategies are adequate and being delivered in accordance with Risk Mitigation Plan.
- Revisions to Risk Mitigation Plan as needed.
- Inter-disciplinary meetings to coordinate services/supports and make changes as needed.
Discharge Planning:
- Assist member to prepare for discharge and to be present on day of discharge.
- Coordinate discharge planning with member, nursing facility social worker, HCBS CM, family, landlord, housing voucher administrator and community providers.
- Coordination of all components of the transition plan prior to discharge.
Advocate for Services Identified in the Service Plan
- Provide counsel and support to the person receiving services and other appropriate parties as necessary to prepare them for entry, transfer or termination from a program
- Provide information on Medicaid State Plan benefits
- Contact with member’s family members or informal supports to assist member with accessing community-based supports.
- Advocate for the member’s preferences regarding community living options/resources
- Promote of member’s self-advocacy
- Promote person-centered practices
Determination of the Number of Units to Bill
Apply the following guidelines when determining the number of units (unit = 15 minutes) to record for billing purposes:
- Activities performed that are less than 15 minutes are billed at one (1) unit when the activity has a specifically defined and purposeful outcome, i.e., telephone contact with a member for scheduling a meeting.
- Activities that involve indirect contacts (e.g., documentation, mailing/distribution, BUS entry) are to be considered in the units appropriate to the primary transition coordination activity whenever possible. For example, if 25 minutes (2 units) is spent to write a letter, but five minutes was spent to mail the letter on the following day, an additional unit is not billed. The entire activity is billed as two (2) indirect contact units.
- Activities that include services to more than one member (e.g. Transition Coordination meetings with case managers where several different members may be discussed) should be estimated as time/unit per member. For example, if one (1) hour (4 units) is spent discussing four (4) members during a meeting, one (1) unit per person is billed. Typically, the total billed units should not exceed the total amount of time spent. In this example, four (4) units for each of the four (4) members will exceed the amount of time spent by that case manager by 3 hours.
- Typically, the number of units billed by a transition coordinator in a given time should not exceed the total amount of time worked. For example, a Transition Coordinator who works eight (8) hours a day should not exceed 32 units of billable activities in that day.
- Since a unit is defined as 1-15 minutes of transition coordination activity, there may be situations when the number of units billed exceeds the number of units worked per day or per activity. For example, a Transition Coordinator may perform a monitoring visit at a group home for four members totaling 1 hour. Since the minimum unit that can be billed per member is one unit, the transition coordinator may bill one unit for each of the four members.
- The primary intent of a TC service should always be related to the assessment of the member needs, preferences and goals or the development, implementation, amendment, coordination, or monitoring of the member’s status and goal attainment and implementation of the Transition Plan and Risk Mitigation Plan.
Documenting Targeted Case Management- Transition Coordination
Non-Reimbursable Targeted Case Management Activities
Activities that may be a Transition Coordinator’s responsibility but are not billable as TC activities. The list of activities below is not an exhaustive list.
Sample Non-billable Activities
- Aggregation and analysis of customer satisfaction or complaint logs and data
- Transition coordination activities when member is incarcerated (i.e., in jail)
- Transition activities related to receiving/enrollment from another TCA
- TCA staff meetings
- TC training/professional development
- Assisting a member with needs covered in room and board expense, e.g., minor home repairs.
- Recreational events e.g., agency functions when no TC activity is performed
- Providing transportation to a member, (e.g., medical dental, therapy appointments, etc.)
- Fund raising activities of the agency
- Providing a service that is an identified HCBS benefit, other funded service, or natural support (unfunded service).
- TC billing related activities
Targeted Case Management – Transition Coordination Procedure Code Table
Providers may bill procedure codes for Targeted Case Management – Transition Coordination as follows:
| Targeted Case Management- Transition Services | |||
|---|---|---|---|
| Description | Procedure Code | Modifier(s) | Unit Designation |
| Targeted Case Management – Transition Coordination | T1017 | UB | 15 Minutes – the use of the modifier here is required and is not solely for identification purposes. |
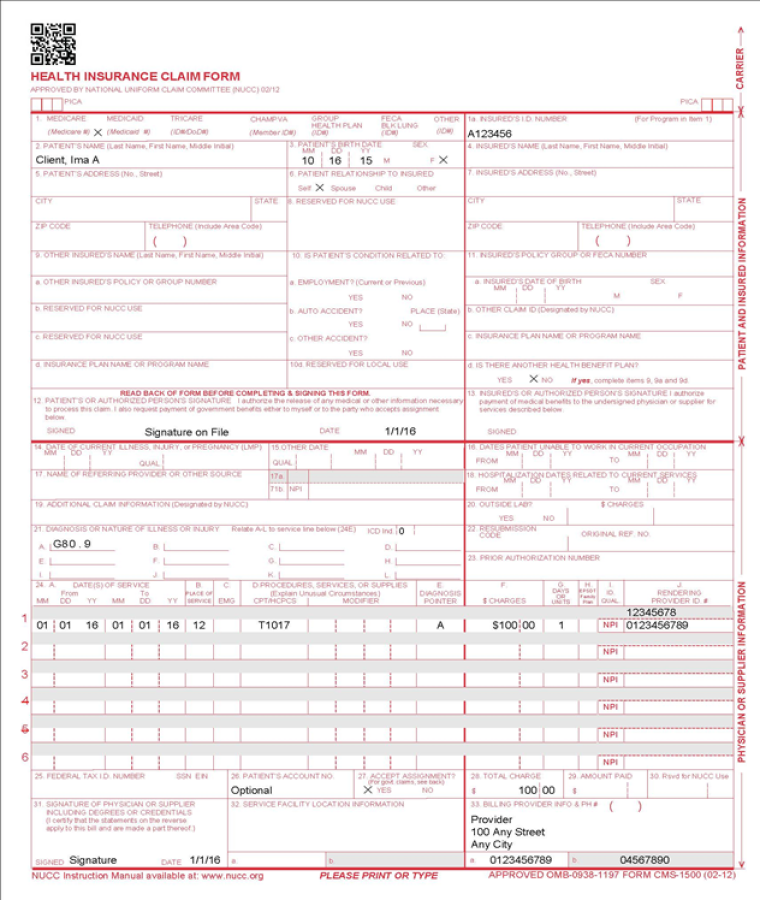
Targeted Case Management – Transition Coordination Claim Reference Table
The following paper form reference table describes required fields for the paper CMS 1500 claim form for Targeted Case Management – Transition Coordination claims.
| CMS Field Number and Label | Field is: | Instructions | ||||||||||||
| Invoice/Pat Acct Number | Optional | Enter the information that identifies the patient or claim in the provider’s billing system. Submitted information appears on the Provider Claim Report. Up to 12 characters: letters, numbers or hyphens | ||||||||||||
| Invoice/Pat Acct Number | Optional | Enter the information that identifies the patient or claim in the provider’s billing system. Submitted information appears on the Provider Claim Report. Up to 12 characters: letters, numbers or hyphens | ||||||||||||
| Special Program Code | Optional | 2 digits | ||||||||||||
| 1a. Insured's ID Number | Required | Enter the member's seven-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. | ||||||||||||
| 2. Patient's Name | Required | Enter the member's last name, first name, and middle initial. | ||||||||||||
| 3. Patient's Date of Birth/Sex | Required | Enter the member's birth date using two digits for the month, two digits for the date, and two digits for the year. Example: 070114 for July 1, 2014. Place an "X" in the appropriate box to indicate the sex of the member. | ||||||||||||
| 4. Insured's Name | Conditional | Complete if the member is covered by a Medicare health insurance policy. Enter the insured’s full last name, first name, and middle initial. If the insured used a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. | ||||||||||||
| 5. Patient's Address | Not Required | |||||||||||||
| 6. Patient Relationship to Insured | Conditional | Complete if the member is covered by a commercial health care insurance policy. | ||||||||||||
| 7. Insured's Address | Not Required | |||||||||||||
| 8. Reserved for NUCC Use | Not Required | |||||||||||||
| 9. Other Insured's Name | Conditional | If field 11d is marked "YES", enter the insured’s last name, first name and middle initial. | ||||||||||||
| 9a. Other Insured's Policy or Group Number | Conditional | If field 11d is marked "YES", enter the policy or group number. | ||||||||||||
| 9b. Reserved for NUCC Use | ||||||||||||||
| 9c. Reserved for NUCC Use | ||||||||||||||
| 9d. Insurance Plan or Program Name | Conditional | If field 11D is marked "YES", enter the insurance plan or program name. | ||||||||||||
| 10a-c. Is patient's condition related to? | Conditional | When appropriate, place an "X" in the correct box to indicate whether one or more of the services described in field 24 are for a condition or injury that occurred on the job, as a result of an auto accident or other. | ||||||||||||
| 10d. Reserved for Local Use | ||||||||||||||
| 11. Insured's Policy, Group or FECA Number | Conditional | |||||||||||||
| 11a. Insured's Date of Birth, Sex | Not Required | Complete if the member is covered by a Medicare health insurance policy. Enter the insured’s birth date using two digits for the month, two digits for the date and two digits for the year. Example: 070114 for July 1, 2014. Place an “X" in the appropriate box to indicate the sex of the insured. | ||||||||||||
| 11b. Other Claim ID | Not Required | |||||||||||||
| 11c. Insurance Plan Name or Program Name | Not Required | |||||||||||||
| 11d. Is there another Health Benefit Plan? | Conditional | When appropriate, place an "X" in the correct box. If marked "YES", complete 9, 9a and 9d. | ||||||||||||
| 12. Patient's or Authorized Person's signature | Required | Enter "Signature on File", "SOF", or legal signature. If there is no signature on file, leave blank or enter "No Signature on File". Enter the date the claim form was signed. | ||||||||||||
| 13. Insured's or Authorized Person's Signature | Not Required | |||||||||||||
| 14. Date of Current Illness Injury or Pregnancy | Not Required | |||||||||||||
| 15. Other Date Not | Not Required | |||||||||||||
| 16. Date Patient Unable to Work in Current Occupation | Not Required | |||||||||||||
| 17. Name of Referring Physician | Conditional | |||||||||||||
| 17b. NPI of Referring Physician | Conditional | |||||||||||||
| 18. Hospitalization Dates Related to Current Service | Not Required | |||||||||||||
| 19. Additional Claim Information | Conditional | When applicable, enter the words "TRANSPORT CERT" to certify that you have a transportation certificate or trip sheet on file for this service. | ||||||||||||
| 20. Outside Lab? $ Charges | Not Required | |||||||||||||
| 21. Diagnosis or Nature of Illness or Injury | Required | Enter at least one but no more than twelve diagnosis codes based on the member’s diagnosis/condition. Enter applicable ICD-10 indicator. NEMT Enter diagnosis code R68.89. | ||||||||||||
| 22. Medicaid Resubmission Code | Conditional | List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code in the left- hand side of the field. 7 - Replacement of prior claim 8 - Void/Cancel of prior claim This field is not intended for use for original claim submissions. | ||||||||||||
| 23. Prior Authorization | Not Required | |||||||||||||
| 24. Claim Line Detail | Information | The paper claim form allows entry of up to six detailed billing lines. Fields 24A through 24J apply to each billed line. Do not enter more than six lines of information on the paper claim. If more than six lines of information are entered, the additional lines will not be entered for processing. Each claim form must be fully completed (totaled). Do not file continuation claims (e.g., Page 1 of 2). | ||||||||||||
| 24A. Dates of Service | Required | The field accommodates the entry of two dates: a "From" date of services and a "To" date of service. Enter the date of service using two digits for the month, two digits for the date and two digits for the year. Example: 010116 for January 1, 2016.
Single Date of Service Enter the six-digit date of service in the "From" field. | ||||||||||||
| 24B. Place of Service | Required | Enter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
| ||||||||||||
| 24C. EMG | Conditional | Enter a "N" or leave blank for NO in the bottom, unshaded area of the field to indicate the service was non-emergent medical transportation. | ||||||||||||
| 24D. Procedures, Services, or Supplies | Required | Enter the HCPCS procedure code that specifically describes the service for which payment is requested. Only approved codes from the current CPT or HCPCS publications will be accepted. | ||||||||||||
| 24D. Modifier | Not Required | Enter the appropriate procedure-related modifier that applies to the billed service. Up to four modifiers may be entered when using the paper claim form. NEMT Only A0110 may require a modifier (see Transportation HCPCS codes). | ||||||||||||
| 24E. Diagnosis Pointer | Required | Enter the diagnosis code reference letter (A-L) that relates the date of service and the procedures performed to the primary diagnosis. At least one diagnosis code reference letter must be entered. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. This field allows for the entry of 4 characters in the unshaded area. | ||||||||||||
| 24F. $ Charges | Required | Enter the usual and customary charge for the service represented by the procedure code on the detail line. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service. Do not deduct Health First Colorado co- payment or commercial insurance payments from the usual and customary charges. | ||||||||||||
| 24G. Days or Units | Required | Enter the number of units provided for each procedure code. Enter whole numbers only- do not enter fractions or decimals. | ||||||||||||
| 24H. EPSDT/Family Plan | Not Required | |||||||||||||
| 24I. ID Qualifier | Not Required | |||||||||||||
| 24J. Rendering Provider ID # | Required | In the shaded portion of the field, enter the NPI or Provider ID of the Health First Colorado provider who actually performed or rendered the billed service. This number cannot be assigned to a group or clinic. | ||||||||||||
| 25. Federal Tax ID Number | Not Required | |||||||||||||
| 26. Patient's Account Number | Optional | Enter information that identifies the member or claim in the provider's billing system. Submitted information appears on the Remittance Advice (RA). | ||||||||||||
| 27. Accept Assignment? | Required | The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer’s program. | ||||||||||||
| 28. Total Charge | Required | Enter the sum of all charges listed in field 24F. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||
| 29. Amount Paid | Conditional | Enter the total amount paid by Medicare or any other commercial health insurance that has made payment on the billed services. Do not use commas when reporting dollar amounts. Enter 00 in the cents area if the amount is a whole number. | ||||||||||||
| 30. Rsvd for NUCC Use | ||||||||||||||
| 31. Signature of Physician or Supplier Including Degrees or Credentials | Required | Each claim must bear the signature of the enrolled provider or the signature of a registered authorized agent. Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two digits for the month, two digits for the date and two digits for the year. Example: 070116 for July 1, 2016. | ||||||||||||
| 32. 32- Service Facility Location Information 32a- NPI Number 32b- Other ID # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | ||||||||||||
| 33. Billing Provider Info & Ph # | Required | Enter the name of the individual or organization that will receive payment for the billed services in the following format: 1st Line Name 2nd Line Address 3rd Line City, State and ZIP Code | ||||||||||||
| 33a- NPI Number | Required | |||||||||||||
| 33b- Other ID # | If the Provider Type is not able to obtain an NPI, enter the eight-digit Health First Colorado provider number of the individual or organization. | |||||||||||||
Targeted Case Management – Transition Coordination Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the Appendices drop-down for more information on timely filing policy, including the resubmission rules for denied claims.
Targeted Case Management – Transition Services Specialty Manuals Revisions Log
| Revision Date | Addition/Changes | Made by |
| 9/4/2020 | Manual Created | HCPF |